Abstract
Alopecia areata (AA) lifetime incidence is around 2%, with many patients first experiencing symptoms during childhood. However, ritlecitinib is the only FDA-approved treatment for pediatric patients 12 years and older. This review outlines reported topical, injectable, and oral treatment options for pediatric patients with AA. Clinical studies were obtained via a PubMed search using the following search terms: alopecia areata, areata, universalis, or totalis and medication, therapy, treatment, drug, or management. Only studies with pediatric patients were included in this review. Commonly used therapies, including corticosteroids, methotrexate, and minoxidil, newer promising medications, such as Janus kinase inhibitors, and less frequently used topical and systemic treatments are included. A summary of the drug development pipeline and ongoing interventional clinical trials with pediatric patients is provided. Treatments demonstrate variable efficacy, and many patients require combination therapy for maximal response. More robust clinical data is needed for many of the medications reviewed in order to provide better care for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Topical, injectable, and systemic corticosteroids are often used as first-line treatment for children with alopecia areata (AA), but many patients will require long-term combination therapies to maintain remission. |
Novel Janus kinase inhibitors demonstrate safety and efficacy in pediatric patients with AA, but additional data is needed to improve access. |
1 Introduction
Alopecia areata (AA) is a non-scarring autoimmune disorder that causes hair loss. This hair loss can be (i) partial or patchy alopecia areata, (ii) complete loss of hair on the scalp (alopecia totalis), or (iii) complete loss of hair over the entire body (alopecia universalis).
According to the Rochester Epidemiology Project, AA prevalence is around 0.2% and the lifetime incidence of AA is estimated at approximately 2%. Females may be affected at slightly higher rates than males, with the mean age of diagnosis being 36.2 years and 31.5 years, respectively [1]. Pediatric patients are affected at higher rates with peak prevalence at 6 years of age and normally distributed [2,3,4,5].
AA most commonly presents as acute, well-demarcated, usually asymptomatic, patchy hair loss on the scalp. Exclamation point hairs should be evident in areas of active loss and broken hairs may be seen on trichoscopy. Some patients (10–20%) may also have nail findings, including pitting, brittleness, ridging, and red lunulae [6]. AA severity can be evaluated using the severity of alopecia tool (SALT). A SALT score is determined by the percentage of hair loss on the scalp, with a higher score corresponding with more severe disease [7,8,9].
Through downregulation of major histocompatibility complexes (MHC) and upregulation of immunosuppressive molecules in the hair follicle, immune responses are dampened. This downregulation is thought to be disrupted in AA, leading to an influx of primarily CD8+ T cells and an increase in interferon (IFN)-γ [10]. The Janus kinase pathways are one type of inflammatory pathway that are upregulated in AA and are a target of medical treatment [6]. The local inflammation at the hair follicle results in degeneration of the follicle during the anagen phase and early entry into the catagen phase. However, the stem cells are typically spared, so regrowth is usually possible [10].
In June 2022, the first systemic therapy, baricitinib, a Janus kinase inhibitor, was approved for use in AA in adults [11]. In June 2023, the FDA approved ritlecitinib for the treatment of AA in children aged 12 years and older. At the time of submission, ritlecitinib is the only FDA-approved treatment for AA in children [12]. This manuscript is a review of published treatment options for the treatment of AA in children and adolescents.
2 Literature Approach
The following search terms were applied in PubMed: alopecia areata, areata, universalis, or totalis and medication, therapy, treatment, drug, or management. Studies were included if pediatric patients were included. Review articles were excluded. A total of 128 primary research articles are included in this review (Supplementary Table 1, see electronic supplementary material [ESM]). ClinicalTrials.gov was reviewed and studies in the recruiting or not yet recruiting phase as of June 11, 2023 that include pediatric patients are also included in this report. Of the 58 studies listed on ClinicalTrials.gov that included pediatric patients, 11 are included below.
3 Treatment
3.1 Topical and Localized Treatments
3.1.1 Corticosteroids
Because AA is caused by overactivation of the immune system and immune attack on hair follicles, corticosteroids work by dampening the immune response and follicular damage, halting the active phase of AA and allowing for a normal hair cycle and regrowth.
Topical corticosteroids are considered first-line therapy for pediatric alopecia areata [13]. A randomized controlled trial in a pediatric population published in 2014 demonstrated better efficacy of clobetasol propionate 0.05% compared with hydrocortisone 1% [14]. Topical corticosteroids have minimal side effects but may cause localized skin atrophy, so are typically tapered with regrowth or discontinued if there is no evidence of improvement [15]. This approach is commonly used as current first-line therapy for pediatric patients [16]. Clobetasol propionate 0.05%, or other topical corticosteroid equivalent, is typically applied daily for at least 12 weeks and up to 6 months [14,15,16].
Intralesional triamcinolone acetonide is commonly used in AA and may be more effective in those with patchy hair loss compared with those with totalis or universalis. Intralesional triamcinolone allows for perifollicular injection and higher localized concentration of the corticosteroid. Concentrations of 2.5–10 mg/mL of triamcinolone acetonide are utilized, but because of potential localized subcutaneous atrophy, it is recommended to dilute the concentration of triamcinolone acetonide to between 2.5 and 5 mg/mL. Needle phobia and pain may limit intralesional medication use, especially in pediatric patients. Sixty percent of participants had adequate response in a study with 10 pediatric and adult patients with minimal side effects, including skin atrophy. An earlier study of 84 pediatric and adult patients also demonstrated this finding [17, 18]. This approach is commonly used when topical steroids fail to have the desired clinical response and patients can tolerate injections.
3.1.2 Minoxidil
Minoxidil is a vasodilator and is thought to promote, prolong, and maintain the anagen phase of hair follicles [19]. Minoxidil is used for hair loss due a variety of causes, including AA [19]. Both topical and oral formulations are used off label in pediatrics. One study evaluated intradermal minoxidil in 100 patches in 20 adult and pediatric patients, which demonstrated quicker regrowth compared with spontaneous regrowth and similar efficacy to microneedling [20]. Two placebo-controlled studies conducted in the 1980s consisting of 60 total patients aged 6–85 years, one case series of three pediatric patients, and two pediatric case reports showed improved hair regrowth in patients treated with topical 3% minoxidil, which is not an approved formulation, compared with placebo or no treatment, but cosmetically acceptable response was noted in a minority of treated patients. Side effects included hypertrichosis, palpitations, and pruritus [21,22,23,24,25]. This approach is commonly used, and patients typically are prescribed 2–5% minoxidil to apply daily in combination with other topical or systemic therapies [16]. Patients may continue topical minoxidil indefinitely if there is benefit and any side effects are not present or minimal.
3.1.3 JAK Inhibitors
First-generation JAK inhibitors, such as ruxolitinib and tofacitinib, may be used off label topically for patients with AA. Topical ruxolitinib is a JAK1 and JAK2 inhibitor that is currently FDA approved for both atopic dermatitis and vitiligo for patients at least 12 years of age [26]. A case report of a girl in her late teens demonstrated complete eyebrow regrowth on the right side and significant regrowth on the left with 10% scalp regrowth after 12 weeks of 0.6% ruxolitinib cream [27]. A case series of six patients aged 3–17 years evaluated topical ruxolitinib and tofacitinib; four participants had some regrowth [28]. A study of 11 patients aged 4–16 years using topical tofacitinib 2% demonstrated significant SALT score improvement in eight patients, but cosmetically acceptable improvement in only three [29]. Due to the FDA approval of systemic use of this medication category, this approach is sometimes used, especially when topical or intralesional corticosteroids fail to have significant desired clinical response.
3.1.4 Platelet-Rich Plasma
Platelet-rich plasma (PRP) is not only rich in platelets, but also various growth factors and cytokines and is thought to both prevent cell death and promote cell proliferation [10]. In a 2022 study comparing intralesional PRP and intralesional triamcinolone in 60 adult and pediatric patients, PRP was less effective [30]. A placebo-controlled study compared topical 5% minoxidil and injected PRP in patients aged 10–40 years. This study showed improved response with both topical minoxidil and PRP and noted earlier response and less vellus and dystrophic hair in those treated with PRP compared with minoxidil and placebo [31]. This approach is not commonly used in pediatric patients.
3.1.5 Phosphodiesterase Inhibitors
Sildenafil is a phosphodiesterase type 5 (PDE5) inhibitor with potential to stimulate hair growth [32]. An open-label pilot study of eight pediatric subjects evaluating sildenafil cream applied twice daily for 3 months showed minimal benefit: vellus hair growth was seen in two and terminal hair growth was seen in a third patient, which was attributed to spontaneous regression instead of treatment [33]. This approach is not commonly used.
3.1.6 Prostaglandin Analogs
Two case reports of patients with AA and a study of 71 patients with eyelash loss due to different reasons explored use of bimatoprost, a prostaglandin analog. Both case reports demonstrated significant regrowth: one in scalp patches in a 9-year-old girl and the other in eyelashes in a 16-year-old girl (eyelashes subsequently fell out with discontinuation of bimatoprost drops in the one eye). The randomized controlled study of 71 patients, aged 5–17 years, compared bimatoprost 0.03% and vehicle and concluded bimatoprost was helpful for eyelash regrowth in patients without a medical condition, but not for those whose eyelash loss was attributed to AA or chemotherapy [34,35,36].
Similar to bimatoprost, latanoprost is a prostaglandin analog that may be beneficial in eyelash/eyebrow alopecia and localized alopecia areata. One pediatric case report and three studies consisting of 50, 54, and 100 adult and pediatric patients evaluated topical latanoprost, which showed better therapeutic outcomes compared with placebo. Latanoprost is likely less effective than betamethasone but is safer with fewer side effects when compared with betamethasone [37,38,39,40].
A case report described a 12-year-old with AA and vitiligo experiencing almost complete regrowth of eyebrows/eyelashes after 2 months of treatment with prostaglandin E2 drops [41]. This approach is not commonly used.
3.1.7 Squaric Acid Dibutylester
Squaric acid dibutylester (SADBE) induces allergic contact dermatitis and thus alters the local immune response, potentially allowing for hair regrowth in AA [42]. Three case series demonstrated moderate efficacy when used in patients with recalcitrant disease. Approximately 40% of pediatric patients responded to SADBE in two separate studies (13/33 and 5/13) [43, 44]. In another study, patients were sensitized with 2% SADBE and then received maintenance therapy of 0.001–0.200% to have continued mild allergic contact dermatitis [45]. Side effects of contact dermatitis (rash, blisters, and pruritus) are expected in this treatment option and can be difficult to predict, manage, and tolerate. This approach is not commonly used unless clinics have access to the medication and experienced providers. Exposure of medical personnel to SADBE may also cause allergic contact dermatitis.
3.1.8 Diphencyprone
While the mechanism of action of diphencyprone, or diphenylcyclopropenone, is not completely understood but likely similar to SADBE, it is used as a contact sensitizing agent in the treatment of AA. Regrowth success varies across retrospective studies from 14% to 33% of participants with complete regrowth, with higher success rates for moderate hair regrowth. Nine retrospective studies are included, for a total of 160 pediatric patients across four reviews and 146 pediatric and adult patients across five reviews. Around a fifth of patients had sensitization reactions and other localized skin reactions akin to SADBE, including pruritus, erythema, vesiculation, scaling, and dyspigmentation, and several had associated lymphadenopathy [46,47,48,49,50,51,52,53,54]. This approach is not commonly used unless clinics have access to the medication and experienced providers; it may also cause allergic contact dermatitis in providers and their staff.
3.1.9 Anthralin
Anthralin inhibits granulocytes and keratinocyte proliferation and reports have demonstrated mixed results with anthralin use in AA. A 2017 case series of 30 pediatric patients reported complete regrowth in 33% and partial regrowth in 37% of patients at 1 year [55]. A 2018 case series of 37 patients showed complete regrowth and at least 50% regrowth in 32% and 68%, respectively. Of those with partial regrowth, 64% relapsed. Skin irritation caused four patients to discontinue treatment [56]. A case study also demonstrated regrowth on the side where anthralin was applied [57]. Skin irritation and dyspigmentation can limit patients’ tolerance of this topical medication. While historically used more when the medication was easier to obtain, this approach is not currently commonly used.
3.1.10 Imiquimod
Imiquimod is FDA approved in the treatment of basal cell carcinomas and anogenital warts in adults and appeared to be a possible adjunctive treatment option in one case report and a case series including nine pediatric patients who displayed improved regrowth when treated with imiquimod in combination with diphenylcyclopropenone [26, 58, 59]. Imiquimod reduces the immune response by binding to toll-like receptors on immune cells, including macrophages and monocytes [60]. This approach is not commonly used.
3.1.11 Bexarotene
A phase I/II study of 42 patients evaluated topical bexarotene 1% gel for 24 weeks. One pediatric patient participated in this study and demonstrated moderate regrowth [61]. This approach is not commonly used.
3.1.12 Cryotherapy
Liquid nitrogen may be a minimally invasive treatment option for recalcitrant AA. In a retrospective review of 353 adult and pediatric patients, 61% of patients had regrowth after 3 months of treatment [62]. A case series of 11 patients treated with two 15-second freeze thaw cycles included three pediatric patients and reported regrowth of > 75% in two of the pediatric patients at 8 weeks, with continued response at 16 weeks [63]. Side effects included mild pain and pruritus. This approach is not commonly used.
3.1.13 Phototherapy
Narrowband UVB can be an effective treatment in psoriasis, but in a retrospective review of six pediatric patients with AA, significant response was not elucidated [64]. This approach is not commonly used.
3.1.14 Laser
Three studies examined the utility of a 308-nm excimer laser in treating AA in pediatric patients. Two studies revealed higher effectiveness of the laser in scalp lesions compared with patches elsewhere on the body. However, about one fifth of those who experienced regrowth relapsed 6 months after final treatment. A total of 14 pediatric patients were evaluated across three studies and all studies consisted of 24 laser sessions per patient [65,66,67]. This approach is not commonly used.
3.1.15 Botulinum toxins
A study that included three pediatric cases of AA was unable to show improvement following three sessions of intralesional 10 U botulinum toxin injections [68]. This approach is not commonly used.
3.2 Systemic Treatments
3.2.1 Corticosteroids
Oral and intravenous corticosteroids are commonly used for treating AA when topical approaches have limited response and/or active progression of AA is occurring. Due to side effects associated with prolonged systemic steroid use, high-dose pulsed administration is commonly used [69]. Relapse rates are high following pulsed dosing, so combination therapy or continued low-dose systemic therapy may be needed for continued remission. One study reported a 62% response rate with high-dose corticosteroids followed by maintenance on low-dose corticosteroids. However, all patients had weight gain and almost a fourth of patients experienced mild acne [70]. Other studies, including those in which patients only received pulsed high-dose steroids, demonstrated similar side effect profiles. High-dose pulsed steroid protocols may range from 8 mg/kg to 30 mg/kg IV methylprednisolone, or other steroid equivalents, typically for 1–3 consecutive days monthly [71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91]. Many providers will limit the number of pulses in order to minimize potential side effects.
3.2.2 Methotrexate
Methotrexate is an immunomodulatory drug used in a plethora of inflammatory and autoimmune conditions with approved doses of 7.5–25 mg weekly [26]. Multiple studies have demonstrated its safety in pediatric AA patients and also shown efficacy. Short-term efficacy ranged from 38% to 66% across multiple studies evaluating methotrexate as monotherapy. Regular laboratory monitoring is necessary [92,93,94,95]. This approach is commonly used in combination with systemic steroids when systemic steroids alone fail to have the desired clinical effect and/or there is recurrence of AA while attempting to wean or discontinue systemic steroids. Response may not be seen until about 16 weeks of treatment, compared with 8–12 weeks for other inflammatory conditions [96].
3.2.3 Minoxidil
Oral minoxidil is becoming more frequently prescribed for different types of alopecia, including AA. One study in 1987 evaluated oral versus topical minoxidil in AA patients aged 13–65 years and demonstrated better efficacy of oral minoxidil 5 mg twice daily compared with topical. However, a majority of patients still had inadequate response [97]. A 2021 retrospective review of 1404 patients aged 8–86 years further demonstrated minoxidil safety, with only 1.7% discontinuing treatment as a result of side effects (i.e., hypertrichosis most commonly, as well as lightheadedness, fluid retention, tachycardia, headache, periorbital edema, and insomnia) [98].
3.2.4 JAK Inhibitors
JAKs are Janus kinase enzymes that form dimers and phosphorylate signal transducer and activator transcription (STAT) proteins. This activates gene transcription that modulates and upregulates the immune response and is a key pathway in the pathogenesis of AA [99]. This category of medication is quickly becoming the mainstay of treatment in adult AA and patients 12 years of age and older with severe disease or disease with significant impact on quality of life.
Ritlecitinib is a JAK3/TEC kinase inhibitor recently approved by the FDA for AA in patients 12 years of age and older, rheumatoid arthritis, vitiligo, Crohn’s disease, and ulcerative colitis [26]. JAK3-specific inhibitors may provide a better safety profile as JAK3 is expressed in hematopoietic cells, compared with JAK1 which is expressed in many different cell types [100]. Inhibiting TEC may increase efficacy through more targeted lymphocyte inhibition [101]. A randomized, double-blind, phase IIb–III study with 718 patients aged 12 years and older has shown that ritlecitinib is a well-tolerated and effective drug for AA. As with all oral JAKs, regular laboratory monitoring is necessary [102]. Short-term side effects reported include headache, acne, and upper respiratory infections [103]. Other more serious potential safety concerns include serious infections, malignancy and lymphoproliferative disorders, thromboembolic events, hypersensitivity reactions, and laboratory abnormalities (i.e., decrease in lymphocyte and platelet counts and increase in creatine phosphokinase and liver enzymes) [26].
Baricitinib is a reversible JAK1 and JAK2 selective inhibitor that is indicated for the treatment of adult rheumatoid arthritis and alopecia areata. Baricitinib is approved by the FDA for adults with AA [26]. A case report demonstrated tolerance and efficacy in a 17-year-old pediatric patient [104].
Tofacitinib is a JAK1 and JAK3 inhibitor with FDA indications for rheumatoid arthritis, psoriatic arthritis, ulcerative colitis, and polyarticular course juvenile idiopathic arthritis [26]. Multiple case series and case reports have reported on the efficacy of tofacitinib treatment for pediatric patients with AA. In these studies, most patients received 5 mg twice daily, except for two studies; one patient received 4 mg twice daily in one study and another study included patients aged 4 years and 5 years who received 2.5 mg four times daily. Across these reports, over 85% of patients had regrowth, with significant or complete regrowth in the majority of those patients. Tofacitinib was also effective in treating eyelashes and eyebrows in affected patients. No serious adverse events were recorded in any reports, which included 68 pediatric patients. A retrospective study of 14 patients treated with tofacitinib demonstrated significant SALT score improvement in nine patients [105,106,107,108,109,110,111,112,113,114,115,116]. A pediatric patient in a case series had 0% improvement after 4 months of tofacitinib therapy 10 mg twice daily but had a 91% SALT score improvement after being treated with ruxolitinib 10 mg twice daily at the end of 10 months [117].
3.2.5 Biologics
Dupilumab is an interleukin (IL)-4 and IL-13 inhibitor indicated in several allergic conditions, including atopic dermatitis, asthma, chronic rhinosinusitis and nasal polyposis, and eosinophilic esophagitis. IL-4 and IL-13 upregulate other inflammatory cytokines and immunoglobulin E. In practice, since dupilumab is approved in patients as young as 6 months with atopic dermatitis, it is frequently used for patients with both AA and atopic dermatitis [26]. Sixteen pediatric patients received subcutaneous dupilumab 300 mg every 2 weeks. A sub-analysis was done of the six patients with active AA at the time of drug initiation; four demonstrated clinical improvement [118]. This medication is used extensively in pediatric patients with atopic dermatitis and has increasing evidence that it may improve AA in patients with both conditions.
Ustekinumab is an IL-12 and IL-23 inhibitor approved by the FDA for adolescent and adult patients with plaque psoriasis and adults with psoriatic arthritis and Crohn’s disease [19]. Inhibition of these pathways suppresses inflammatory cytokines associated with T-cell and natural killer cell activation [119]. A case series of three pediatric patients demonstrated hair growth in all patients with ustekinumab 90 mg [120]. This medication is not commonly used in AA patients.
Lastly, an anti-IFN-γ given to patients aged 6–15 years as a 1-mL injection twice daily for 5 days had the following results: eight out of nine patients with patchy hair loss had regrowth within 6 months and three out of five and two out of five with complete hair loss demonstrated terminal hair growth and vellus hair growth, respectively [121]. This medication is not commonly used in AA patients.
3.2.6 Phosphodiesterase Inhibitors
One study that included a single pediatric patient investigated the utility of apremilast, a PDE4 inhibitor, in AA and did not show any improvement in SALT scores in the pediatric patient or any of the eight adult patients [122].
3.2.7 Calcineurin Inhibitors
Cyclosporine is a calcineurin inhibitor prescribed for a variety of autoimmune conditions. In combination with corticosteroid use, cyclosporine 250–400 mg with subsequent tapering is effective in promoting hair regrowth in patients with AA. A case report of a patient with Down syndrome demonstrated excellent clinical response to this therapy combination. However, in one trial with 46 patients, of which 12 were pediatric patients, side effects were seen in over half of patients, including GI disturbance, edema, acneiform eruption, weight gain, hypertrichosis, and menstrual abnormality. This led to discontinuation of treatment in three patients. In addition, regular laboratory monitoring is necessary [123, 124]. This medication is not commonly used for AA.
Tacrolimus has been attempted for AA treatment [125]. Two case series (with 2/11 pediatric patients and 3/12 pediatric patients) and a case report demonstrated that the calcineurin inhibitor tacrolimus (topical) is ineffective in treating AA [126,127,128]. However, hair growth with sustained response for 2 years was seen in one case report of a pediatric patient when used alongside high-dose pulse methylprednisolone [129].
3.2.8 COX Inhibitors
The mechanism of action of sulfasalazine is also not fully understood but is an immunomodulatory drug approved by the FDA for inflammatory conditions such as rheumatoid arthritis, polyarticular juvenile idiopathic arthritis, and ulcerative colitis. Sulfasalazine elicited response in 56–68% of 71 adult and pediatric AA patients across three studies. With discontinuation of sulfasalazine, almost half of patients subsequently relapsed [130,131,132]. This medication is not commonly used for AA.
3.2.9 Hydroxychloroquine
Hydroxychloroquine exhibits immunomodulatory effects and is used in several autoimmune and inflammatory conditions and is approved by the FDA for lupus erythematosus and rheumatoid arthritis [26]. In a 2018 study of nine pediatric patients with AA treated with hydroxychloroquine, five improved by 6 months. Side effects observed during the course of treatment included GI intolerance and headaches [133]. This medication is not commonly used for AA.
3.2.10 Phototherapy
Photochemotherapy is a type of treatment consisting of psoralens, a photosensitizing agent, followed by ultraviolet radiation with ultraviolet A, also known as PUVA. Photochemotherapy is utilized in several dermatological conditions. Patients with AA responded to some extent (modest to excellent responses recorded) to PUVA in multiple studies, but frequently relapsed following discontinuation of treatment. Some patients experience mild irritation and scaling with this treatment. Intensified UV light exposure in pediatric patients has both immediate (patients must be protected from UV light for 24 hours after psoralen exposure) and long-term implications (photoaging, photocarcinogenesis) [134,135,136,137,138,139]. This therapy is not commonly used for AA.
3.2.11 Intravenous Immunoglobulin
A case report of an 8-year-old girl in 1999 exhibited a patient with significant hair regrowth after a second treatment of intravenous immunoglobulin. Dosing continued at 400 mg/kg every 4 weeks [140]. This treatment is not commonly used for AA.
3.2.12 Psychoimmunotherapy
Many patients with AA experience anxiety and depression related to their disease. A 1991 study with six adult and five pediatric patients evaluated the impact of psychoimmunotherapy on disease activity. Three of the five patients improved following psychoimmunotherapy, which highlights the importance of stress and mental well-being in maximizing therapeutic outcomes [141].
3.3 Combination and Comparative Studies
3.3.1 Methotrexate, Minoxidil, Corticosteroids
One study of 50 adult and pediatric patients compared methotrexate and minoxidil gel, with both demonstrating minimal efficacy [142]. Response rates improved when methotrexate was combined with corticosteroids in three other studies including 77 adult and pediatric patients. Only one study reported increased liver function enzymes in a single patient taking oral methotrexate [143,144,145]. The addition of topical 2% minoxidil to a prednisone taper improved rates of relapse in 32 adult and pediatric patients [146]. A case report of a pediatric patient with Down syndrome and AA demonstrated response to oral betamethasone and topical minoxidil lotion [147]. If patients do not qualify or tolerate oral JAK inhibitors, oral weekly methotrexate combined with topical, intralesional, and/or systemic corticosteroids is commonly used for extensive and recalcitrant AA.
3.3.2 COX Inhibitors
The mechanism of action of mesalazine is not completely understood but is thought to dampen the inflammatory response through multiple pathways. A case series of five patients, aged 2–17 years, revealed terminal hair regrowth in all subjects. However, mesalazine was not used as monotherapy in all patients but in conjunction with oral or topical corticosteroids or topical minoxidil in some [148].
One study demonstrated SALT score improvement in all three pediatric patients when another COX inhibitor, sulfasalazine, was used as an adjuvant to oral corticosteroids [131]. This approach is not commonly used for AA.
3.3.3 Anthralin
One case report compared anthralin and corticosteroids; only the half head treated with topical corticosteroids demonstrated regrowth [57]. In a retrospective study that included 37 pediatric patients, 68% had greater than 50% regrowth, but a majority of patients had subsequent relapse. However, participants in this study were continued on previous therapies [56]. A recent pediatric case report also evaluated the combination of leflunomide and anthralin and reported hair regrowth following treatment with this combination [149].
A 2010 prospective study with 80 pediatric and adult patients compared topical corticosteroids, tretinoin, anthralin paste, and placebo. 70% of patients in the corticosteroid group had regrowth, 55% in the tretinoin group, 35% in the anthralin paste group, and 20% in the placebo group had regrowth. 100% of participants in the anthralin group had hyperpigmentation and some also experienced mild irritation [150]. Tretinoin is thought to block selected inflammatory pathways through binding of retinoic acid receptors [151]. These approaches are not commonly used for AA.
3.3.4 Trichloroacetic Acid, Phenol
A 2021 study compared trichloroacetic acid (TCA) 35% and phenol 88%. Twenty adult and pediatric patients treated two patches with either TCA or phenol. Results showed both treatments were therapeutic, but TCA was superior to phenol. In addition, patients experienced more discomfort with phenol than TCA. No patients with regrowth had relapsed by their 6-month post-treatment follow up [152]. This approach is not commonly used for AA.
3.3.5 Phototherapy, Zinc
Some have postulated that zinc may be beneficial in treating AA [153]. In a 2015 case report, a 16-year-old took zinc 30 mg/day orally and began PUVA treatments 9 months later, with 55 sessions. Hair regrew 2 months into PUVA treatments, and the patient relapsed 4 months after discontinuing zinc and 4 weeks after stopping PUVA [154]. While zinc deficiency can cause hair loss, it is unclear if zinc improved this patient’s response to PUVA and therapeutic outcome. This approach is not commonly used for AA.
3.3.6 Laser
A case report demonstrated complete regrowth in a 5-year-old with topical khellin applied 45 minutes prior to excimer lamp irradiation twice weekly for 3 months. This patient did not show signs of relapse at a 1-year follow up [155]. This approach is not commonly used for AA.
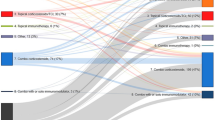
3.4 Ongoing Clinical Trials
Multiple JAK inhibitors are currently undergoing clinical trials that include pediatric patients. A variety of other topical, intralesional, and systemic therapies are also undergoing clinical trials. Table 1 summarizes the current and upcoming treatment landscape for treating pediatric patients with AA [156].
4 Conclusion
A variety of topical and systemic medications are used off label in pediatric AA. However, only one has been approved by the FDA (ritlecitinib) for pediatric patients (12 years and older). Most treatments demonstrate modest efficacy and combination therapy is often needed for patients with AA. Without larger controlled studies, it is difficult to accurately determine the true efficacy of many therapeutic agents reported in pediatric AA management. Furthermore, many patients relapse within months of discontinuing treatment in the above studies. The percentage of patients that ultimately experience relapse is not completely elucidated in these studies due to length of follow up.
The most evidence for first line therapy for pediatric patients with alopecia areata is corticosteroids. A randomized, controlled trial demonstrated the efficacy and safety of topical clobetasol propionate 0.05%, so this should be used as first line as it may benefit the patient and has minimal side effects [14]. Intralesional triamcinolone may be used if topical therapy fails to produce the desired results and/or the patient can tolerate injections [17, 18]. Due to side effects, systemic corticosteroids are less frequently used, but the use of high-dose pulse corticosteroids may be utilized to maximize response and minimize side effects, as demonstrated by multiple case series and retrospective reviews [69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91].
Several treatments may be combined with corticosteroid therapies. The use of topical and oral minoxidil is supported by several case reports, case series, and a 1987 clinical trial [19,20,21,22,23,24,25, 97, 98]. More reports exist for topical minoxidil compared with oral for pediatric patients with AA. Oral methotrexate may also be added if steroids do not have the desired effect. Several retrospective studies and a long-term follow-up of a cohort study demonstrated its benefit and safety in pediatric patients [92,93,94,95,96]. The strength of evidence for a variety of other topical and systemic therapies is lower and primarily consists of retrospective studies and case series, but they may be considered for specific patients.
The most promising treatment appears to be JAK inhibitors, but additional clinical information is needed to demonstrate safety and efficacy in the pediatric population, thereby improving access to care for these patients. In addition, JAK inhibitors and other biologics are a more expensive treatment option compared with corticosteroids, minoxidil, and methotrexate. Earlier access to effective treatment is thought to be important as response may wane the longer patients go without hair growth. Multiple clinical trials investigating JAK inhibitors are currently ongoing and include pediatric patients, so this hopefully predicts better access to treatments and improved outcomes for patients in the future.
References
Mirzoyev SA, Schrum AG, Davis MDP, Torgerson RR. Lifetime incidence risk of alopecia areata estimated at 2.1% by Rochester Epidemiology Project, 1990–2009. J Invest Dermatol. 2014;134(4):1141–2. https://doi.org/10.1038/jid.2013.464. (Epub 2013 Nov 11).
Kyriakis KP, Paltatzidou K, Kosma E, Sofouri E, Tadros A, Rachioti E. Alopecia areata prevalence by gender and age. J Eur Acad Dermatol Venereol. 2009;23(5):572–3. https://doi.org/10.1111/j.1468-3083.2008.02956.x. (Epub 2008 Sep 3).
McKenzie PL, Maltenfort M, Bruckner AL, Gupta D, Harfmann KL, Hyde P, Forrest CB, Castelo-Soccio L. Evaluation of the prevalence and incidence of pediatric alopecia areata using electronic health record data. JAMA Dermatol. 2022;158(5):547–51. https://doi.org/10.1001/jamadermatol.2022.0351.
Ali NS, Tollefson MM, Lohse CM, Torgerson RR. Incidence and comorbidities of pediatric alopecia areata: a retrospective matched cohort study using the Rochester Epidemiology Project. J Am Acad Dermatol. 2022;87(2):427–9. https://doi.org/10.1016/j.jaad.2021.08.050. (Epub 2021 Sep 4).
Caldwell CC, Saikaly SK, Dellavalle RP, Solomon JA. Prevalence of pediatric alopecia areata among 572,617 dermatology patients. J Am Acad Dermatol. 2017;77(5):980–1. https://doi.org/10.1016/j.jaad.2017.06.035.
Strazzulla LC, Wang EHC, Avila L, Lo Sicco K, Brinster N, Christiano AM, Shapiro J. Alopecia areata: disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018;78(1):1–12. https://doi.org/10.1016/j.jaad.2017.04.1141.
Olsen E, Hordinsky M, McDonald-Hull S, Price V, Roberts J, Shapiro J, Stenn K. Alopecia areata investigational assessment guidelines. National Alopecia Areata Foundation. J Am Acad Dermatol. 1999;40(2 Pt 1):242–6. https://doi.org/10.1016/s0190-9622(99)70195-7.
Olsen EA, Hordinsky MK, Price VH, Roberts JL, Shapiro J, Canfield D, Duvic M, King LE Jr, McMichael AJ, Randall VA, Turner ML, Sperling L, Whiting DA, Norris D; National Alopecia Areata Foundation. Alopecia areata investigational assessment guidelines—Part II. National Alopecia Areata Foundation. J Am Acad Dermatol. 2004;51(3):440–7. https://doi.org/10.1016/j.jaad.2003.09.032.
Olsen EA, Hordinsky MK, Price VH, Roberts JL, Shapiro J, Canfield D, Duvic M, King LE Jr, McMichael AJ, Randall VA, Turner ML, Sperling L, Whiting DA, Norris D. Severity of Alopecia Tool (SALT) scoring tool.
Zhou C, Li X, Wang C, Zhang J. Alopecia areata: an update on etiopathogenesis, diagnosis, and management. Clin Rev Allergy Immunol. 2021;61(3):403–23. https://doi.org/10.1007/s12016-021-08883-0. (Epub 2021 Aug 17).
Commissioner, O. of the. 2022. FDA approves first systemic treatment for alopecia areata. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-systemic-treatment-alopecia-areata. Accessed 12 Sept 2023.
Highlights of prescribing information. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/215830s000lbl.pdf. Accessed 4 Sept 2024.
Barton VR, Toussi A, Awasthi S, Kiuru M. Treatment of pediatric alopecia areata: a systematic review. J Am Acad Dermatol. 2022;86(6):1318–34. https://doi.org/10.1016/j.jaad.2021.04.077. (Epub 2021 Apr 30).
Lenane P, Macarthur C, Parkin PC, et al. Clobetasol propionate, 0.05%, vs hydrocortisone, 1%, for alopecia areata in children: a randomized clinical trial. JAMA Dermatol. 2014;150(1):47–50.
Montes LF. Topical halcinonide in alopecia areata and in alopecia totalis. J Cutan Pathol. 1977;4(2):47–50.
Meah N, Wall D, York K, Bhoyrul B, Bokhari L, Sigall DA, Bergfeld WF, Betz RC, Blume-Peytavi U, Callender V, Chitreddy V, Combalia A, Cotsarelis G, Craiglow B, Donovan J, Eisman S, Farrant P, Green J, Grimalt R, Harries M, Hordinsky M, Irvine AD, Itami S, Jolliffe V, King B, Lee WS, McMichael A, Messenger A, Mirmirani P, Olsen E, Orlow SJ, Piraccini BM, Rakowska A, Reygagne P, Roberts JL, Rudnicka L, Shapiro J, Sharma P, Tosti A, Vogt A, Wade M, Yip L, Zlotogorski A, Sinclair R. The Alopecia Areata Consensus of Experts (ACE) study: Results of an international expert opinion on treatments for alopecia areata. J Am Acad Dermatol. 2020;83(1):123–30. https://doi.org/10.1016/j.jaad.2020.03.004. (Epub 2020 Mar 9).
Chang KH, Rojhirunsakool S, Goldberg LJ. Treatment of severe alopecia areata with intralesional steroid injections. J Drugs Dermatol. 2009;8(10):909–12.
Abell E, Munro DD. Intralesional treatment of alopecia areata with triamcinolone acetonide by jet injector. Br J Dermatol. 1973;88(1):55–9.
Suchonwanit P, Thammarucha S, Leerunyakul K. Minoxidil and its use in hair disorders: a review. Drug Des Devel Ther. 2019;13:2777–86. https://doi.org/10.2147/DDDT.S214907. (Erratum in: Drug Des Devel Ther. 2020 Feb 10;14:575).
Abdallah MAE, Shareef R, Soltan MY. Efficacy of intradermal minoxidil 5% injections for treatment of patchy non-severe alopecia areata. J Dermatol Treat. 2022;33(2):1126–9.
Fenton DA, Wilkinson JD. Topical minoxidil in the treatment of alopecia areata. Br Med J (Clin Res Ed). 1983;287(6398):1015–7.
Price VH. Double-blind, placebo-controlled evaluation of topical minoxidil in extensive alopecia areata. J Am Acad Dermatol. 1987;16(3 Pt 2):730–6.
Georgala S, Befon A, Maniatopoulou E, Georgala C. Topical use of minoxidil in children and systemic side effects. Dermatology. 2007;214(1):101–2.
Rai AK. Minoxidil-induced hypertrichosis in a child with alopecia areata. Indian Dermatol Online J. 2017;8(2):147–8.
Weiss VC, West DP, Mueller CE. Topical minoxidil in alopecia areata. J Am Acad Dermatol. 1981;5(2):224–6.
Center for Drug Evaluation and Research. (n.d.). DRUGS@FDA data files. U.S. Food and Drug Administration. https://www.fda.gov/drugs/drug-approvals-and-databases/drugsfda-data-files. Accessed 12 Sept 2023.
Craiglow BG, Tavares D, King BA. Topical ruxolitinib for the treatment of alopecia universalis. JAMA Dermatol. 2016;152(4):490–1.
Bayart CB, DeNiro KL, Brichta L, Craiglow BG, Sidbury R. Topical Janus kinase inhibitors for the treatment of pediatric alopecia areata. J Am Acad Dermatol. 2017;77(1):167–70.
Putterman E, Castelo-Soccio L. Topical 2% tofacitinib for children with alopecia areata, alopecia totalis, and alopecia universalis. J Am Acad Dermatol. 2018;78(6):1207-1209.e1.
Khan FA, Hussain M, Khan BM, et al. Comparative study between intralesional injection of platelet rich plasma and intra lesional triamcinolone for the treatment of alopecia areata. J Ayub Med Coll Abbottabad. 2022;34(4):762–5.
El Taieb MA, Ibrahim H, Nada EA, Seif A-DM. Platelets rich plasma versus minoxidil 5% in treatment of alopecia areata: a trichoscopic evaluation. Dermatol Ther. 2017. https://doi.org/10.1111/dth.12437. (Epub 2016 Oct 28).
Choi HI, Kang BM, Jang J, Hwang ST, Kwon O. Novel effect of sildenafil on hair growth. Biochem Biophys Res Commun. 2018;505(3):685–91. https://doi.org/10.1016/j.bbrc.2018.09.164. (Epub 2018 Oct 3).
Sarifakioglu E, Degim IT, Gorpelioglu C. Determination of the sildenafil effect on alopecia areata in childhood: An open-pilot comparison study. J Dermatol Treat. 2006;17(4):235–7.
Borchert M, Bruce S, Wirta D, et al. An evaluation of the safety and efficacy of bimatoprost for eyelash growth in pediatric subjects. Clin Ophthalmol. 2016;10:419–29 (Published 2016 Mar 10).
Zaheri S, Hughes B. Successful use of bimatoprost in the treatment of alopecia of the eyelashes. Clin Exp Dermatol. 2010;35(4):e161–2.
Li AW, Antaya RJ. Successful treatment of pediatric alopecia areata of the scalp using topical bimatoprost. Pediatr Dermatol. 2016;33(5):e282–3.
Mehta JS, Raman J, Gupta N, Thoung D. Cutaneous latanoprost in the treatment of alopecia areata. Eye (Lond). 2003;17(3):444–6.
Bhat S, Handa S, De D. A randomized comparative study of the efficacy of topical latanoprost versus topical betamethasone diproprionate lotion in the treatment of localized alopecia areata. Indian J Dermatol Venereol Leprol. 2021;87(1):42–8.
Coronel-Pérez IM, Rodríguez-Rey EM, Camacho-Martínez FM. Latanoprost in the treatment of eyelash alopecia in alopecia areata universalis. J Eur Acad Dermatol Venereol. 2010;24(4):481–5.
El-Ashmawy AA, El-Maadawy IH, El-Maghraby GM. Efficacy of topical latanoprost versus minoxidil and betamethasone valerate on the treatment of alopecia areata. J Dermatolog Treat. 2018;29(1):55–64.
Yadav S, Dogra S, Kaur I. An unusual anatomical colocalization of alopecia areata and vitiligo in a child, and improvement during treatment with topical prostaglandin E2. Clin Exp Dermatol. 2009;34(8):e1010–1.
Hill ND, Bunata K, Hebert AA. Treatment of alopecia areata with squaric acid dibutylester. Clin Dermatol. 2015;33(3):300–4.
Giannetti A, Orecchia G. Clinical experience on the treatment of alopecia areata with squaric acid dibutyl ester. Dermatologica. 1983;167(5):280–2.
Tosti A, Guidetti MS, Bardazzi F, Misciali C. Long-term results of topical immunotherapy in children with alopecia totalis or alopecia universalis. J Am Acad Dermatol. 1996;35(2 Pt 1):199–201.
Pardasani AG, Turner E, McMichael AJ. Squaric acid dibutylester: indications for use and efficacy in alopecia areata. Arch Dermatol. 2001;137(7):970–2.
Salsberg JM, Donovan J. The safety and efficacy of diphencyprone for the treatment of alopecia areata in children. Arch Dermatol. 2012;148(9):1084–5.
Schuttelaar ML, Hamstra JJ, Plinck EP, et al. Alopecia areata in children: treatment with diphencyprone. Br J Dermatol. 1996;135(4):581–5.
Hull SM, Pepall L, Cunliffe WJ. Alopecia areata in children: response to treatment with diphencyprone. Br J Dermatol. 1991;125(2):164–8.
Orecchia G, Rabbiosi G. Treatment of alopecia areata with diphencyprone. Dermatologica. 1985;171(3):193–6.
Luk NM, Chiu LS, Lee KC, et al. Efficacy and safety of diphenylcyclopropenone among Chinese patients with steroid resistant and extensive alopecia areata. J Eur Acad Dermatol Venereol. 2013;27(3):e400–5.
Singh G, Okade R, Naik C, Dayanand CD. Diphenylcyclopropenone immunotherapy in ophiasis. Indian J Dermatol Venereol Leprol. 2007;73(6):432–3.
Sotiriadis D, Patsatsi A, Lazaridou E, Kastanis A, Vakirlis E, Chrysomallis F. Topical immunotherapy with diphenylcyclopropenone in the treatment of chronic extensive alopecia areata. Clin Exp Dermatol. 2007;32(1):48–51.
Orecchia G, Malagoli P. Topical immunotherapy in children with alopecia areata. J Invest Dermatol. 1995;104(5 Suppl):35S-36S.
Durdu M, Özcan D, Baba M, Seçkin D. Efficacy and safety of diphenylcyclopropenone alone or in combination with anthralin in the treatment of chronic extensive alopecia areata: a retrospective case series. J Am Acad Dermatol. 2015;72(4):640–50.
Özdemir M, Balevi A. Bilateral half-head comparison of 1% anthralin ointment in children with alopecia areata. Pediatr Dermatol. 2017;34(2):128–32.
Wu SZ, Wang S, Ratnaparkhi R, Bergfeld WF. Treatment of pediatric alopecia areata with anthralin: a retrospective study of 37 patients. Pediatr Dermatol. 2018;35(6):817–20.
Torchia D, Schachner LA. Bilateral treatment for alopecia areata. Pediatr Dermatol. 2010;27(4):415–6.
Letada PR, Sparling JD, Norwood C. Imiquimod in the treatment of alopecia universalis. Cutis. 2007;79(2):138–40.
Wasyłyszyn T, Borowska K. Possible advantage of imiquimod and diphenylcyclopropenone combined treatment versus diphenylcyclopropenone alone: an observational study of nonresponder patients with alopecia areata. Austral J Dermatol. 2017;58(3):219–23.
Bubna AK. Imiquimod - its role in the treatment of cutaneous malignancies. Indian J Pharmacol. 2015;47(4):354–9. https://doi.org/10.4103/0253-7613.161249.
Talpur R, Vu J, Bassett R, Stevens V, Duvic M. Phase I/II randomized bilateral half-head comparison of topical bexarotene 1% gel for alopecia areata. J Am Acad Dermatol. 2009;61(4):592.e1-592.e5929.
Jun M, Lee NR, Lee WS. Efficacy and safety of superficial cryotherapy for alopecia areata: A retrospective, comprehensive review of 353 cases over 22 years [published correction appears in J Dermatol. 2017 Aug;44(8):985]. J Dermatol. 2017;44(4):386–93.
Zawar VP, Karad GM. Liquid nitrogen cryotherapy in recalcitrant alopecia areata: a study of 11 patients. Int J Trichol. 2016;8(1):15–20.
Jury CS, McHenry P, Burden AD, Lever R, Bilsland D. Narrowband ultraviolet B (UVB) phototherapy in children. Clin Exp Dermatol. 2006;31(2):196–9.
Al-Mutairi N. 308-nm excimer laser for the treatment of alopecia areata in children. Pediatr Dermatol. 2009;26(5):547–50.
Al-Mutairi N. 308-nm excimer laser for the treatment of alopecia areata. Dermatol Surg. 2007;33(12):1483–7.
Zakaria W, Passeron T, Ostovari N, Lacour JP, Ortonne JP. 308-nm excimer laser therapy in alopecia areata. J Am Acad Dermatol. 2004;51(5):837–8.
Cho HR, Lew BL, Lew H, Sim WY. Treatment effects of intradermal botulinum toxin type A injection on alopecia areata. Dermatol Surg. 2010;36(Suppl 4):2175–81.
Gallaga NM, Carrillo B, Good A, Munoz-Gonzalez A, Ross L. Pediatric pulse dose corticosteroid therapy dosing and administration in the treatment of alopecia areata: a review of literature. Pediatr Dermatol. 2023;40(2):276–81. https://doi.org/10.1111/pde.15209. (Epub 2022 Dec 2).
Jahn-Bassler K, Bauer WM, Karlhofer F, Vossen MG, Stingl G. Sequential high- and low-dose systemic corticosteroid therapy for severe childhood alopecia areata. J Dtsch Dermatol Ges. 2017;15(1):42–7.
Lalosevic J, Gajic-Veljic M, Bonaci-Nikolic B, Nikolic M. Combined oral pulse and topical corticosteroid therapy for severe alopecia areata in children: a long-term follow-up study. Dermatol Ther. 2015;28(5):309–17.
Chong JH, Taïeb A, Morice-Picard F, Dutkiewicz AS, Léauté-Labrèze C, Boralevi F. High-dose pulsed corticosteroid therapy combined with methotrexate for severe alopecia areata of childhood. J Eur Acad Dermatol Venereol. 2017;31(11):e476–7.
Seiter S, Ugurel S, Tilgen W, Reinhold U. High-dose pulse corticosteroid therapy in the treatment of severe alopecia areata. Dermatology. 2001;202(3):230–4.
Unger WP, Schemmer RJ. Corticosteroids in the treatment of alopecia totalis. Systemic effects. Arch Dermatol. 1978;114(10):1486–90.
Sharma VK, Gupta S. Twice weekly 5 mg dexamethasone oral pulse in the treatment of extensive alopecia areata. J Dermatol. 1999;26(9):562–5.
Smith A, Trüeb RM, Theiler M, Hauser V, Weibel L. High relapse rates despite early intervention with intravenous methylprednisolone pulse therapy for severe childhood alopecia areata. Pediatr Dermatol. 2015;32(4):481–7.
Senila SC, Danescu SA, Ungureanu L, Candrea E, Cosgarea RM. Intravenous methylprednisolone pulse therapy in severe alopecia areata. Indian J Dermatol Venereol Leprol. 2015;81(1):95.
Hubiche T, Léauté-Labrèze C, Taïeb A, Boralevi F. Poor long term outcome of severe alopecia areata in children treated with high dose pulse corticosteroid therapy. Br J Dermatol. 2008;158(5):1136–7.
Bin Saif GA. Oral mega pulse methylprednisolone in alopecia universalis. Saudi Med J. 2006;27(5):717–20.
Friedli A, Labarthe MP, Engelhardt E, Feldmann R, Salomon D, Saurat JH. Pulse methylprednisolone therapy for severe alopecia areata: an open prospective study of 45 patients. J Am Acad Dermatol. 1998;39(4 Pt 1):597–602.
Kiesch N, Stene JJ, Goens J, Vanhooteghem O, Song M. Pulse steroid therapy for children’s severe alopecia areata? Dermatology. 1997;194(4):395–7.
Perriard-Wolfensberger J, Pasche-Koo F, Mainetti C, Labarthe MP, Salomon D, Saurat JH. Pulse of methylprednisolone in alopecia areata. Dermatology. 1993;187(4):282–5.
Kar BR, Handa S, Dogra S, Kumar B. Placebo-controlled oral pulse prednisolone therapy in alopecia areata. J Am Acad Dermatol. 2005;52(2):287–90.
Efentaki P, Altenburg A, Haerting J, Zouboulis CC. Medium-dose prednisolone pulse therapy in alopecia areata. Dermatoendocrinol. 2009;1(6):310–3.
Sharma VK, Muralidhar S. Treatment of widespread alopecia areata in young patients with monthly oral corticosteroid pulse. Pediatr Dermatol. 1998;15(4):313–7.
Winter RJ, Kern F, Blizzard RM. Prednisone therapy for alopecia areata. A follow-up report. Arch Dermatol. 1976;112(11):1549–52.
Friedland R, Tal R, Lapidoth M, Zvulunov A, Ben AD. Pulse corticosteroid therapy for alopecia areata in children: a retrospective study. Dermatology. 2013;227(1):37–44.
Yoshimasu T, Kanazawa N, Yamamoto Y, Furukawa F. Multiple courses of pulse corticosteroid therapy for alopecia areata. J Dermatol. 2016;43(9):1075–7.
Alabdulkareem AS, Abahussein AA, Okoro A. Severe alopecia areata treated with systemic corticosteroids. Int J Dermatol. 1998;37(8):622–4.
Seo J, Lee YI, Hwang S, Zheng Z, Kim DY. Intramuscular triamcinolone acetonide: an undervalued option for refractory alopecia areata. J Dermatol. 2017;44(2):173–9.
Michalowski R, Kuczyńska L. Long-term intramuscular triamcinolone-acetonide therapy in alopecia areata totalis and universalis. Arch Dermatol Res. 1978;261(1):73–6.
Royer M, Bodemer C, Vabres P, et al. Efficacy and tolerability of methotrexate in severe childhood alopecia areata. Br J Dermatol. 2011;165(2):407–10.
Lucas P, Bodemer C, Barbarot S, Vabres P, Royer M, Mazereeuw-Hautier J. Methotrexate in severe childhood alopecia areata: long-term follow-up. Acta Derm Venereol. 2016;96(1):102–3.
Landis ET, Pichardo-Geisinger RO. Methotrexate for the treatment of pediatric alopecia areata. J Dermatol Treat. 2018;29(2):145–8.
Batalla A, Flórez Á, Abalde T, Vázquez-Veiga H. Methotrexate in alopecia areata: a report of three cases. Int J Trichol. 2016;8(4):188–90.
Siegfried EC, Arkin LM, Chiu YE, Hebert AA, Callen JP, Castelo-Soccio L, Co DO, Cordoro KM, Curran ML, Dalrymple AM, Flohr C, Gordon KB, Hanna D, Irvine AD, Kim S, Kirkorian AY, Lara-Corrales I, Lindstrom J, Paller AS, Reyes M, Begolka WS, Tom WL, Van Voorhees AS, Vleugels RA, Lee LW, Davies OMT, Brandling-Bennett HA. Methotrexate for inflammatory skin disease in pediatric patients: consensus treatment guidelines. Pediatr Dermatol. 2023;40(5):789–808. https://doi.org/10.1111/pde.15327. (Epub 2023 Jun 14).
Fiedler-Weiss VC, Rumsfield J, Buys CM, West DP, Wendrow A. Evaluation of oral minoxidil in the treatment of alopecia areata. Arch Dermatol. 1987;123(11):1488–90.
Vañó-Galván S, Pirmez R, Hermosa-Gelbard A, Moreno-Arrones ÓM, Saceda-Corralo D, Rodrigues-Barata R, Jimenez-Cauhe J, Koh WL, Poa JE, Jerjen R, Trindade de Carvalho L, John JM, Salas-Callo CI, Vincenzi C, Yin L, Lo-Sicco K, Waskiel-Burnat A, Starace M, Zamorano JL, Jaén-Olasolo P, Piraccini BM, Rudnicka L, Shapiro J, Tosti A, Sinclair R, Bhoyrul B. Safety of low-dose oral minoxidil for hair loss: a multicenter study of 1404 patients. J Am Acad Dermatol. 2021;84(6):1644-1651. https://doi.org/10.1016/j.jaad.2021.02.054. Epub 2021 Feb 24.
Ahmad A, Zaheer M, Balis FJ. Baricitinib—StatPearls—NCBI Bookshelf. Baricitinib. 2022. https://www.ncbi.nlm.nih.gov/books/NBK572064/. Accessed 12 Sept 2023.
Ramírez-Marín HA, Tosti A. Evaluating the therapeutic potential of ritlecitinib for the treatment of alopecia areata. Drug Des Dev Ther. 2022;16:363–74. https://doi.org/10.2147/dddt.s334727.
Zarrin AA, Bao K, Lupardus P, Vucic D. Kinase inhibition in autoimmunity and inflammation. Nat Rev Drug Discov. 2021;20(1):39–63. https://doi.org/10.1038/s41573-020-0082-8. (Epub 2020 Oct 19).
King B, Zhang X, Harcha WG, et al. Efficacy and safety of ritlecitinib in adults and adolescents with alopecia areata: a randomised, double-blind, multicentre, phase 2b-3 trial [published correction appears in Lancet. 2023 Jun 10;401(10392):1928]. Lancet. 2023;401(10387):1518–29.
Hordinsky M, Hebert AA, Gooderham M, Kwon O, Murashkin N, Fang H, Harada K, Law E, Wajsbrot D, Takiya L, Zwillich SH, Wolk R, Tran H. Efficacy and safety of ritlecitinib in adolescents with alopecia areata: Results from the ALLEGRO phase 2b/3 randomized, double-blind, placebo-controlled trial. Pediatr Dermatol. 2023. https://doi.org/10.1111/pde.15378. (Epub ahead of print).
Jabbari A, Dai Z, Xing L, et al. Reversal of alopecia areata following treatment with the JAK1/2 Inhibitor baricitinib. EBioMedicine. 2015;2(4):351–5 (Published 2015 Feb 26).
Craiglow BG, Liu LY, King BA. Tofacitinib for the treatment of alopecia areata and variants in adolescents. J Am Acad Dermatol. 2017;76(1):29–32.
Castelo-Soccio L. Experience with oral tofacitinib in 8 adolescent patients with alopecia universalis. J Am Acad Dermatol. 2017;76(4):754–5.
Kibbie J, Kines K, Norris D, Dunnick CA. Oral tofacitinib for the treatment of alopecia areata in pediatric patients. Pediatr Dermatol. 2022;39(1):31–4.
Craiglow BG, King BA. Tofacitinib for the treatment of alopecia areata in preadolescent children. J Am Acad Dermatol. 2019;80(2):568–70.
Dai YX, Chen CC. Tofacitinib therapy for children with severe alopecia areata. J Am Acad Dermatol. 2019;80(4):1164–6.
Brown L, Skopit S. An excellent response to tofacitinib in a pediatric alopecia patient: a case report and review. J Drugs Dermatol. 2018;17(8):914–7.
Patel NU, Oussedik E, Grammenos A, Pichardo-Geisinger R. A case report highlighting the effective treatment of alopecia universalis with tofacitinib in an adolescent and adult patient. J Cutan Med Surg. 2018;22(4):439–42.
Liu LY, King BA. Response to tofacitinib therapy of eyebrows and eyelashes in alopecia areata. J Am Acad Dermatol. 2019;80(6):1778–9.
Berbert Ferreira R, Ferreira SB, Scheinberg MA. An excellent response to tofacitinib in a Brazilian adolescent patient with alopecia areata: a case report and a review of the literature. Clin Case Rep. 2019;7(12):2539–42 (Published 2019 Nov 21).
Dincer Rota D, Emeksiz MAC, Erdogan FG, Yildirim D. Experience with oral tofacitinib in severe alopecia areata with different clinical responses. J Cosmet Dermatol. 2021;20(9):3026–33.
Jerjen R, Meah N, de Carvalho LT, Wall D, Eisman S, Sinclair R. Treatment of alopecia areata in pre-adolescent children with oral tofacitinib: a retrospective study. Pediatr Dermatol. 2021;38(1):103–8.
Akdogan N, Ersoy-Evans S, Doğan S, Atakan N. Experience with oral tofacitinib in two adolescents and seven adults with alopecia areata. Dermatol Ther. 2019;32(6): e13118.
Liu LY, King BA. Ruxolitinib for the treatment of severe alopecia areata. J Am Acad Dermatol. 2019;80(2):566–8.
McKenzie PL, Castelo-Soccio L. Dupilumab therapy for alopecia areata in pediatric patients with concomitant atopic dermatitis. J Am Acad Dermatol. 2021;84(6):1691–4.
Benson JM, Peritt D, Scallon BJ, Heavner GA, Shealy DJ, Giles-Komar JM, Mascelli MA. Discovery and mechanism of ustekinumab. MAbs. 2011;3(6):535–45. https://doi.org/10.4161/mabs.3.6.17815.
Aleisa A, Lim Y, Gordon S, et al. Response to ustekinumab in three pediatric patients with alopecia areata. Pediatr Dermatol. 2019;36(1):e44–5.
Skurkovich S, Korotky NG, Sharova NM, Skurkovich B. Treatment of alopecia areata with anti-interferon-gamma antibodies. J Investig Dermatol Symp Proc. 2005;10(3):283–4.
Liu LY, King BA. Lack of efficacy of apremilast in 9 patients with severe alopecia areata. J Am Acad Dermatol. 2017;77(4):773–4.
Kim BJ, Min SU, Park KY, et al. Combination therapy of cyclosporine and methylprednisolone on severe alopecia areata. J Dermatolog Treat. 2008;19(4):216–20.
Gensure RC. Clinical response to combined therapy of cyclosporine and prednisone. J Investig Dermatol Symp Proc. 2013;16(1):S58.
Farhangian ME, McMichael AJ, Huang KE, Feldman SR. Treatment of alopecia areata in the United States: a retrospective cross-sectional study. J Drugs Dermatol. 2015;14(9):1012–4.
Price VH, Willey A, Chen BK. Topical tacrolimus in alopecia areata. J Am Acad Dermatol. 2005;52(1):138–9.
Thiers BH. Topical tacrolimus: treatment failure in a patient with alopecia areata. Arch Dermatol. 2000;136(1):124.
Jung KE, Gye JW, Park MK, Park BC. Comparison of the topical FK506 and clobetasol propionate as first-line therapy in the treatment of early alopecia areata. Int J Dermatol. 2017;56(12):1487–8.
Sauerbrey A. Successful immunsuppression in childhood alopecia areata. Klin Padiatr. 2011;223(4):244–5.
Rashidi T, Mahd AA. Treatment of persistent alopecia areata with sulfasalazine. Int J Dermatol. 2008;47(8):850–2.
Bakar O, Gurbuz O. Is there a role for sulfasalazine in the treatment of alopecia areata? J Am Acad Dermatol. 2007;57(4):703–6.
Aghaei S. An uncontrolled, open label study of sulfasalazine in severe alopecia areata. Indian J Dermatol Venereol Leprol. 2008;74(6):611–3.
Yun D, Silverberg NB, Stein SL. Alopecia areata treated with hydroxychloroquine: a retrospective study of nine pediatric cases. Pediatr Dermatol. 2018;35(3):361–5.
Mitchell AJ, Douglass MC. Topical photochemotherapy for alopecia areata. J Am Acad Dermatol. 1985;12(4):644–9.
Majumdar B, De A, Ghosh S, et al. “Turban PUVAsol:” a simple, novel, effective, and safe treatment option for advanced and refractory cases of alopecia areata. Int J Trichol. 2018;10(3):124–8.
Yoon TY, Kim YG. Infant alopecia universalis: role of topical PUVA (psoralen ultraviolet A) radiation. Int J Dermatol. 2005;44(12):1065–7.
Claudy AL, Gagnaire D. PUVA treatment of alopecia areata. Arch Dermatol. 1983;119(12):975–8.
El-Mofty M, Rasheed H, El-Eishy N, et al. A clinical and immunological study of phototoxic regimen of ultraviolet A for treatment of alopecia areata: a randomized controlled clinical trial. J Dermatol Treat. 2019;30(6):582–7.
Amer MA, El Garf A. Photochemotherapy and alopecia areata. Int J Dermatol. 1983;22(4):245–6.
Boonyaleepun S, Boonyaleepun C, Schlactus JL. Effect of IVIG on the hair regrowth in a common variable immune deficiency patient with alopecia universalis. Asian Pac J Allergy Immunol. 1999;17(1):59–62.
Teshima H, Sogawa H, Mizobe K, Kuroki N, Nakagawa T. Application of psychoimmunotherapy in patients with alopecia universalis. Psychother Psychosom. 1991;56(4):235–41.
Toma DM, Atallah RB, Eldahshan RM. Comparative study between topical methotrexate 1% gel and minoxidil 5% gel in the treatment of localized alopecia areata. Dermatol Ther. 2022;35(9): e15696.
Anuset D, Perceau G, Bernard P, Reguiai Z. Efficacy and safety of methotrexate combined with low- to moderate-dose corticosteroids for severe alopecia areata. Dermatology. 2016;232(2):242–8.
Hammerschmidt M, Mulinari BF. Efficacy and safety of methotrexate in alopecia areata. An Bras Dermatol. 2014;89(5):729–34.
Droitcourt C, Milpied B, Ezzedine K, et al. Interest of high-dose pulse corticosteroid therapy combined with methotrexate for severe alopecia areata: a retrospective case series. Dermatology. 2012;224(4):369–73.
Olsen EA, Carson SC, Turney EA. Systemic steroids with or without 2% topical minoxidil in the treatment of alopecia areata. Arch Dermatol. 1992;128(11):1467–73.
Sethuraman G, Malhotra AK, Sharma VK. Alopecia universalis in Down syndrome: response to therapy. Indian J Dermatol Venereol Leprol. 2006;72(6):454–5.
Kiszewski AE, Bevilaqua M, De Abreu LB. Mesalazine in the treatment of extensive alopecia areata: a new therapeutic option? Int J Trichology. 2018;10(3):99–102.
Sardana K, Gupta A, Gautam RK. Recalcitrant alopecia areata responsive to leflunomide and anthralin-Potentially undiscovered JAK/STAT inhibitors? Pediatr Dermatol. 2018;35(6):856–8.
Das S, Ghorami RC, Chatterjee T, Banerjee G. Comparative assessment of topical steroids, topical tretenoin (0.05%) and dithranol paste in alopecia areata. Indian J Dermatol. 2010;55(2):148–9.
Yoham AL, Casadesus D. Tretinoin—StatPearls—NCBI Bookshelf. 2023. https://www.ncbi.nlm.nih.gov/books/NBK557478/. Accessed 12 Sept 2023.
Mahgoub D, Mohye Eldeen R, Saadi D, El-Samanoudy S, Ibrahim S. Clinical and trichoscopic evaluation of trichloroacetic acid 35% vs phenol 88% peels in treatment of alopecia areata. J Cosmet Dermatol. 2021;20(1):143–9.
Camacho FM, García-Hernández MJ. Zinc aspartate, biotin, and clobetasol propionate in the treatment of alopecia areata in childhood. Pediatr Dermatol. 1999;16(4):336–8.
Lux-Battistelli C. Combination therapy with zinc gluconate and PUVA for alopecia areata totalis: an adjunctive but crucial role of zinc supplementation. Dermatol Ther. 2015;28(4):235–8.
Fenniche S, Hammami H, Zaouak A. Association of khellin and 308-nm excimer lamp in the treatment of severe alopecia areata in a child. J Cosmet Laser Ther. 2018;20(3):156–8.
Clinical Trials. National Library of Medicine. http://www.clinicaltrials.gov. Accessed 12 Sept 2023.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this manuscript.
Conflicts of interest
None.
Availability of data and material
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Author contributions
LLW contributed to the design and drafting of the manuscript. DSM contributed to the conception and revision of the manuscript. DBM and ELN contributed to the design and revision of the work. All authors approved the final version of the manuscript and agree to be accountable for the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Westerkam, L.L., McShane, D.B., Nieman, E.L. et al. Treatment Options for Alopecia Areata in Children and Adolescents. Pediatr Drugs 26, 245–257 (2024). https://doi.org/10.1007/s40272-024-00620-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-024-00620-2