Abstract
Ganaxolone (ZTALMY®), a synthetic neuroactive steroid that acts as a positive allosteric modulator of the synaptic and extrasynaptic gamma-aminobutyric acid (GABA)A receptor, is an effective and well tolerated, orally-administered adjunct to existing antiseizure treatments in patients 2 years of age or older with cyclin-dependent kinase-like 5 (CDKL5) deficiency disorder (CDD)-associated seizures. CDD (a rare X-linked genetic disorder) is a severe developmental epileptic encephalopathy with onset in early infancy. In the randomized, double-blind, phase 3 Marigold trial, adjunctive ganaxolone significantly reduced the 28-day major motor seizure frequency from baseline compared with placebo in patients with CDD-associated refractory epilepsy. Preliminary results from the Marigold open-label extension suggest that the clinical benefits of ganaxolone in patients with CDD are maintained longer term. Ganaxolone is generally well tolerated; somnolence is the most frequent adverse reaction.
Plain Language Summary
Cyclin-dependent kinase-like 5 (CDKL5) deficiency disorder (CDD) is a rare, X-linked genetic disorder characterised by clinical features that include developmental delay and severe treatment-resistant epilepsy that begins soon after birth. Treatment of CDD is symptom based; antiseizure medications suitable for the seizure types seen in CDD are widely used, but no one agent has been associated with improved seizure control and treatment becomes less effective over time. Ganaxolone (ZTALMY®), an analog of the naturally occurring neuroactive steroid allopregnanolone, has recently been developed and is the first approved treatment for seizures associated with CDD. In the phase 3 placebo-controlled Marigold trial in patients aged 2–19 years, ganaxolone was more effective than placebo (as an addition to existing antiseizure treatment) in reducing the frequency of seizures in patients with CDD. The effectiveness of ganaxolone seems to be maintained during longer term treatment. Ganaxolone was generally well tolerated in patients with CDD; the most common adverse reaction was somnolence. Oral ganaxolone is an effective and well-tolerated adjunct to existing treatment options for patients with CDD-associated seizures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Digital Features for this Adis Drug Q&A can be found at https://doi.org/10.6084/m9.figshare.21737315. |
A selective, high-affinity positive allosteric modulator of synaptic and extrasynaptic GABAA receptors |
Administered orally three times daily with food |
More effective than placebo (as an adjunct to existing antiseizure treatment) in reducing the frequency of major motor seizures; efficacy appears to be maintained during longer term treatment |
Generally well tolerated; somnolence is the most frequent adverse reaction |
What is the rationale for using ganaxolone in the treatment of seizures associated with cyclin-dependent kinase-like 5 deficiency disorder (CDD)?
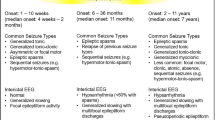
Cyclin-dependent kinase-like 5 (CDKL5) deficiency disorder (CDD), a rare X-linked disorder resulting from pathogenic (or likely pathogenic) CDKL5 variants, is a severe developmental epileptic encephalopathy with onset in early infancy [1]. CDD has a prevalence of 1 in 40,000–60,000 births (making it one of the more common forms of genetic epilepsy) and is characterized by a range of clinical features, including developmental delay and severe, treatment-refractory epilepsy beginning soon after birth [1,2,3,4]. Data from the International CDKL5 Disorder database indicates that more than half of individuals with CDD have 1–5 seizures/day on average and 15% have > 5 seizures/day [1]. Treatment of CDD is predominantly empirical and symptom based. Although epilepsy in this patient population is highly refractory, antiseizure medications appropriate for epilepsy with focal and generalized seizure types seen in CDD are widely used, but no one agent has been associated with improved seizure control and treatment becomes less effective over time [1, 3, 4]. There is therefore a need for better treatments for this drug-resistant epilepsy of early childhood [5].
In patients with epilepsy, seizures generally occur because of an imbalance between neuronal excitation and inhibition associated with a failure of inhibitory neurotransmission [6]. A large body of evidence has linked epilepsy with dysfunction of gamma-aminobutyric acid (GABA)A receptor inhibition; thus, the GABAA receptor is a significant target of antiseizure drugs [6]. Activation of synaptic GABAA receptors results in a rapid, phasic inhibition of synaptic activity, while activation of extrasynaptic GABAA receptors results in a persistent, tonic inhibition [7]. Even though synaptic GABAA receptors are downregulated in prolonged seizures, agents that have activity at the retained extrasynaptic GABAA receptors can achieve sustained anticonvulsant effects and consequently be suitable for treating refractory epilepsy [8]. Ganaxolone (ZTALMY®) [9], an analog of the naturally occurring neuroactive steroid allopregnanolone, is a selective, high-affinity positive allosteric modulator of both synaptic and extrasynaptic GABAA receptors [2, 8,9,10,11] and may therefore have potential for seizure improvements in patients with CDD.
For whom is ganaxolone indicated?
Ganaxolone is indicated for the treatment of seizures associated with CDD in patients 2 years of age and older [9]. Table 1 provides a summary of the prescribing information for ganaxolone as approved in the USA, and Table 2 presents various warnings and precautions that relate to the use of ganaxolone. Consult prescribing information for further details.
What are the pharmacological properties of ganaxolone?
Ganaxolone is the 3β-methylated synthetic analog of allopregnanolone; the 3β-methyl substitution renders the drug orally bioavailable. After absorption, ganaxolone does not convert back to a metabolite with activity at the nuclear progesterone receptor [10]. While the exact mechanism by which ganaxolone prevents seizures in patients with CDD is unknown, its anticonvulsant effects are thought to result from positive allosteric modulation of the GABAA receptor in the central nervous system [9]. The anticonvulsive activity of ganaxolone has been shown in animal epilepsy models [10,11,12,13,14]; tolerance to ganaxolone did not develop with chronic administration of the drug in an animal model of epilepsy [14]. The treatment effect of ganaxolone as an adjunct was shown intially in a small cohort of patients with CDD (n = 7; aged 2.6–16.5 years) in a phase 2a trial [15, 16]. Ganaxolone dosages up to 63 mg/kg/day reduced the 28-day seizure frequency at 26 weeks by a median 44.4% relative to baseline [15, 17], and continued to be effective in the four patients who entered a 12-month open-label extension [16, 17].
Peak plasma concentrations (Cmax) of ganaxolone are achieved 2–3 h after oral administration; exposure (Cmax and AUC) is increased when administered with a high-fat meal (3- and 2-fold, respectively, vs fasted state), and ganaxolone should be administered with food. Ganaxolone is highly protein-bound (≈ 99%) in serum. Ganaxolone is metabolized by CYP3A4/5, CYP2B6, CYP2C19 and CYP2D6 and undergoes hepatic clearance. The terminal half-life of ganaxolone is 34 h. Ganaxolone is primarily excreted in faeces (55% of total radioactivity recovered in faeces and 18% in urine after a single oral 300 mg dose of [14C]-ganaxolone in healthy subjects). In vitro, ganaxolone is not an inhibitor or inducer of CYP isozymes (including CYP1A2, CYP2B6 or CYP3A4/5) or an inhibitor or substrate of transporters at clinically relevant concentrations [9].
Coadministration of ganaxolone with rifampin, a strong inducer of CYP2C19 and CYP3A4 and a moderate inducer of CYP2B6, decreased ganaxolone exposure (Cmax by 57% and and AUC by 68%) in healthy subjects. Concomitant use of ganaxolone with strong or moderate CYP3A4 inducers should be therefore avoided (Table 2); if this is not possible, the ganaxolone dosage should be increased, but should not exceed the maximum recommended dosage. There is potential for clinically relevant drug interactions to occur if enzyme-inducing antiepileptic drugs are initiated or dosages are increased in patients who are on a stable ganaxolone dosage, and the ganaxolone dosage may need to be increased (Table 2). Changes in ganaxolone exposure when coadministered with a strong CYP3A4 inhibitor in healthy subjects were minimal, and changes in ganaxolone exposures when coadministered with strong, moderate or weak CYP3A4 inhibitors are not expected to be clinically significant. Ganaxolone had no clinically relevant effects on exposures of a sensitive CYP3A4 substrate in healthy subjects [9].
What is the efficacy of ganaxolone in the treatment of seizures associated with CDD?
Adjunctive treatment with ganaxolone is effective in reducing the frequency of refractory CDD-associated seizures, based on results of the randomized, double-blind, placebo-controlled, global phase 3 Marigold trial [17] and preliminary data from the open-label Marigold extension [18]. Treatment with ganxaolone was significantly more effective than placebo in reducing the 28-day frequency of major motor seizures from baseline in patients with CDD in the placebo-controlled period of Marigold [17].
Eligible trial participants were:
-
aged 2–21 years;
-
had a molecularly confirmed CDKL5 variant (including mosaic variant) that was pathogenic/likely to be pathogenic;
-
a history of seizures that were inadequately controlled by ≥ 2 previous treatment regimens; and
-
had ≥ 16 major motor seizures [i.e. bilateral tonic (sustained motor activity for ≥ 3 s), generalized tonic-clonic, bilateral clonic, atonic, focal to bilateral tonic-clonic] per 28 days in each 4-week period of an 8-week historical period prior to screening [17].
A stable (≥ 1 month) treatment regimen of up to 4 concomitant antiseizure medications was permitted, as was consistent treatment with nonpharmacological treatment regimens in the 3 months prior to screening [17]. Apart from one patient, ganaxolone recipients were receiving other antiseizure treatments [9].
The 8-week historical eligibility period was followed by a 6-week prospective period in which baseline data were collected. Mean patient age was 6.8 years (range 2–19 years) and most participants were female (79%) [9, 17]. Patients were then randomized to receive ganaxolone or placebo three times daily with food as adjunctive therapy to existing antiseizure medications in a 17-week double-blind treatment period. Oral ganaxolone (50 mg/mL) or matching placebo solution was titrated for 4 weeks up to a maximum dose of 63 mg/kg/day (for patients weighing ≤ 28 kg) or 1800 mg/day (for patients weighing > 28 kg), which was followed by 13 weeks of maintenance treatment [17]. On completion of the double-blind period, patients could enter an open-label extension in which all patients received adjunctive ganaxolone (placebo recipients were switched to ganaxolone titrated over 4 weeks, followed by maintenance treatment). The maximum daily dose of ganaxolone permitted was 63 mg/kg/day (in those weighing ≤ 28 kg) and 1800 mg/day (in those weighing > 28 kg) taken in three divided doses [17, 18].
The primary endpoint was the percentage change in major motor seizure frequency (expressed as a 28-day median value) from the 6-week baseline period to the end of the 17-week double-blind period of the trial. The median 28-day major motor seizure frequency in the 6-week baseline period was 54.0 in the ganaxolone group and 49.2 in the placebo group [Hodges-Lehmann estimate of median difference of 12.0 (95% CI −8.4 to 32.7)]. Patients had previously received a median of 7 antiseizure medications (range 4–10) and were on a median of 2 concomitant antiseizure medications (range 1–4; most frequently used were valproate, levetiracetam, clobazam and vigabatrin) during the trial. At the end of the 4-week dose titration period, 40 of 50 ganaxolone recipients and 42 of 51 placebo recipients had reached their target dose [17].
Ganaxolone was more effective than placebo in reducing major motor seizure frequency from baseline during the 17-week double-blind treatment period of the Marigold trial (Table 3). The median percentage change in 28-day major motor seizure frequency from baseline period to week 17 of the double-blind period was significantly greater with ganaxolone than placebo (primary endpoint; Table 3); the median 28-day major motor seizure frequency during the 17-week double-blind period was 45.0 in the ganaxolone arm compared with 55.5 in the placebo arm [17]. A reduction in major motor seizure frequency of ≥ 50% from the baseline period to week 17 of the double-blind period was seen in 12 of 49 ganaxolone recipients and 5 of 51 placebo recipients (Table 3); however, the between-group difference was not statistically significant and further statistical testing for subsequent endpoints was not conducted, according to the pre-specified hierarchical testing procedure [17]. The median percentage change from baseline in 28-day major motor seizure frequency during the titration period (weeks 1–4 of treatment) [−35.1% vs −13.9% (Hodges–Lehmann estimate of median difference −18.7%; 95% CI −34.8 to −1.8)] and during the maintenance period (weeks 5–17) [−29.4% vs −6.5% (Hodges–Lehmann estimate of median difference −29.3%; 95% CI −51.5 to −8.9)] was numerically higher in the ganaxolone group compared with placebo, as was the median percentage change from baseline in 28-day seizure frequency for all seizure types combined [−19.1% vs −8.9% (Hodges–Lehmann estimate of median difference −17.4%; 95% CI −36.4 to 0.3)]. No patient in the trial had seizure freedom (reduction in seizure frequency of 100%) [17].
While a numerically higher proportion of patients in the ganaxolone arm than in the placebo arm were rated as minimally improved or better on the Clinical Global Impression of Improvement (CGI-I) caregiver- and clinician-administered scales, the Caregiver Global Impression of Change in Seizure Intensity/Duration (CGI-CSID) scale, Caregiver Global Impression of Change in Attention (CGI-CA) scale and the Caregiver Global Impression of Change (CGI-C) scales (Table 3), the odds ratios for the CGI-CA and CGI-C scales indicate that there were no differences between the two treatment arms and due to the hierarchical testing procedure no conclusions regarding statistical significance can be drawn [17].
Are the benefits of ganaxolone sustained longer term?
The clinical benefits of ganaxolone in patients with CDD are maintained longer term, according to preliminary results after 12 months’ treatment with ganaxolone in the open-label extension of the Marigold trial (n = 88) [18]. The median percentage change in 28-day major motor seizure frequency from baseline was −30.1% at 8 months (n = 38) and −46.5% at 12 months (n = 22) in patients who had been treated with ganaxolone throughout the study and −33.3% (n = 34) and −53.8% (n = 26), respectively in placebo recipients who had switched to ganaxolone. The median 28-day major motor seizure frequency in the 6-week baseline period in extension study participants was 50.6. The majority of patients showed improvements (minimally improved or better) in both caregiver and clinician CGI-I ratings at week 34 in the extension study [18].
What is the tolerability profile of ganaxolone?
Ganaxolone was generally well tolerated in patients with CDD-associated refractory epilepsy in the Marigold trial [9, 17, 18]. In the placebo-controlled period, similar proportions of ganaxolone and placebo recipients experienced a treatment-emergent adverse event [TEAE] (86% vs 88%); the most common TEAEs that occurred in ≥ 10% of ganaxolone recipients and more frequently with ganaxolone than placebo were somnolence (36% vs 16%), pyrexia (18% vs 8%) and upper respiratory tract infection (10% vs 6%). Treatment related AEs occurred more frequently with ganaxolone than placebo (70% vs 43%) [17]; those occurring in ≥ 5% of ganaxolone recipients and more frequently than with placebo were somnolence (34% vs 6%), constipation (6% vs 0%), salivary hypersecretion (6% vs 2%) and sedation (6% vs 4%). Serious TEAEs, TEAEs leading to dose reduction/interruption and TEAEs leading to treatment discontinuation occurred in 12%, 22% and 4% of ganaxolone recipients and 10%, 16% and 8% of placebo recipients [17].
The most frequent adverse reactions leading to dose reduction/interruption in the ganaxolone arm were somnolence (10%) and sedation (2%) and those leading to treatment discontinuation were somnolence and seizure (1 patient) and seizure (1 patient) [9]. There were no TEAEs leading to death in either treatment arm, nor were there clinically significant findings related to clinical laboratory tests, electrocardiography, vital signs, and physical, neurological or developmental evaluations [17].
The type and incidence of adverse events reported with ganaxolone in the open-label extension of the Marigold trial were consistent with those seen in the placebo-controlled period and no new safety signals were observed. The most frequently reported adverse events leading to ganaxolone discontinuation were seizures (3.4%) and somnolence (2.3%) [18].
What is the current clinical position of ganaxolone in the treatment of seizures associated with CDD?
Oral ganaxolone is an effective and well tolerated adjunct to existing antiseizure treatments in patients aged 2 years and older with seizures associated with CDD and has potential as a new treatment in the management of CDD-associated refractory epilepsy. Based on clinical trial data, adjunctive ganaxolone significantly reduced the frequency of major motor seizures from baseline compared with placebo in patients with CDD-associated refractory epilepsy [17]. Although the reduction in seizure frequency was relatively modest, such an improvement is considered clinically relevant, given the severity of the seizures associated with CDD [5]. Of note, patients in the Marigold trial had a high baseline seizure burden despite ongoing treatment with antiseizure medications and had previously been treated with a median seven antiseizure medications at baseline [17]. Preliminary results after ≥ 8 months’ treatment in the open-label extension of Marigold suggest that the clinical benefits of ganaxolone in patients with CDD are maintained longer term [18]; final results of the extension study are awaited with interest. Ganaxolone was generally well tolerated in the Marigold trial; similar proportions of ganaxolone and placebo recipients experienced serious TEAEs or TEAEs requiring dose reduction/interruptions and few ganaxolone recipients discontinued treatment as a result of TEAEs [17, 18].
Expert opinion indicates that when managing epilepsy in CDD, seizure control should be approached in the context of the broader neurodevelopmental disorder and quality of life priorities and wherever possible antiseizure regimens should aim to minimize complex drug-drug interactions and tolerability issues [1, 3, 4]. Clobazam, topiramate, steroids, valproate, levetiracetam, vigabatrin and lamotrigine have been identified by clinicians and caregivers as being antiseizure treatments of benefit [1, 3], but no particular agent stands out as effective in CDD-associated seizures and often multiple agents are required [1, 3, 19].
Formerly, treatment guidelines for the management of CDD were not available and evidence-based data from academic medical centres on the clinical management of these patients was limited to treatments for epilepsy [1]; no strong evidence was available for any specific treatment intervention in this patient population [20]. More recently, ganaxolone has been recommended as an option for epilepsy associated with CDD (dependent on local regulatory approval), if clinically indicated, by the International Consensus Recommendations for the assessment and management of individuals with CDD [20]. Ganaxolone is the first approved treatment for seizures associated with CDD in patients 2 years of age or older and the first treatment specifically approved for CDD [19].
References
Leonard H, Downs J, Benke TA, et al. CDKL5 deficiency disorder: clinical features, diagnosis, and management. Lancet Neurol. 2022;21(6):563–76.
Cerne R, Lippa A, Poe MM, et al. GABAkines—advances in the discovery, development, and commercialization of positive allosteric modulators of GABAA receptors. Pharmacol Ther. 2022;234: 108035.
Olson HE, Daniels CI, Haviland I, et al. Current neurologic treatment and emerging therapies in CDKL5 deficiency disorder. J Neurodev Disord. 2021;13(1):1–11.
Hong W, Haviland I, Pestana-Knight E, et al. CDKL5 deficiency disorder-related epilepsy: a review of current and emerging treatment. CNS Drugs. 2022;36(6):591–604.
Gill D. A potential new treatment for CDKL5 deficiency disorder. Lancet Neurol. 2022;21(5):394–5.
Greenfield LJ Jr. Molecular mechanisms of antiseizure drug activity at GABAA receptors. Seizure. 2013;22(8):589–600.
Lattanzi S, Riva A, Striano P. Ganaxolone treatment for epilepsy patients: from pharmacology to place in therapy. Expert Rev Neurother. 2021;21(11):1317–32.
Younus I, Reddy DS. A resurging boom in new drugs for epilepsy and brain disorders. Expert Rev Clin Pharmacol. 2018;11(1):27–45.
Marinus Pharmaceuticals Inc. ZTALMY® (ganaxolone): US prescribing information. 2022. https://marinuspharma.com/. Accessed 5 Dec 2022.
Marinus Pharmaceuticals Inc. Ganaxolone: mechanism of action and pharmacology [poster]. 2020. https://marinuspharma.com/wp-content/uploads/2020/12/1_AES2020_GNX-Mechanism-of-Action.pdf. Accessed 5 Dec 2022.
Carter RB, Wood PL, Wieland S, et al. Characterization of the anticonvulsant properties of ganaxolone (CCD 1042; 3α-hydroxy-3β-methyl-5α-pregnan-20-one), a selective, high-affinity, steroid modulator of the γ-aminobutyric acidA receptor. J Pharmacol Exp Ther. 1997;280(3):1284–95.
Gasior M, Ungard JT, Beekman M, et al. Acute and chronic effects of the synthetic neuroactive steroid, ganaxolone, against the convulsive and lethal effects of pentylenetetrazol in seizure-kindled mice: comparison with diazepam and valproate. Neuropharmacology. 2000;39(7):1184–96.
Liptáková S, Velísek L, Velísková J, et al. Effect of ganaxolone on flurothyl seizures in developing rats. Epilepsia. 2000;41(7):788–93.
Reddy DS, Rogawski MA. Chronic treatment with the neuroactive steroid ganaxolone in the rat induces anticonvulsant tolerance to diazepam but not to itself. J Pharmacol Exp Ther. 2000;295(3):1241–8.
Marinus Pharmaceuticals Inc. Ganaxalone in CDKL5 deficiency disorder: open-label phase 2a results and ongoing pivotal phase 3 study design [poster]. 2018. https://marinuspharma.com/wp-content/uploads/2020/09/AES2018_CDKL5-Ph2-and-Ph3-Design.pdf. Accessed 5 Dec 2022.
Specchio N, Masuoka L, Aimetti A, et al. Long-term, durable seizure frequency reduction in children with CDKL5 Deficiency Disorder (CDD) treated with ganaxolone [abstract no. 3.283 plus poster]. In: 72nd Annual Meeting of the American Epilepsy Society. 2018.
Pestana Knight EM, Amin S, Bahi-Buisson N, et al. Safety and efficacy of ganaxolone in patients with CDKL5 deficiency disorder: results from the double-blind phase of a randomised, placebo-controlled, phase 3 trial. Lancet Neurol. 2022;21(5):417–27.
Olson H, Valappil AN, Rybak E, et al. Extended duration safety and efficacy of adjunctive ganaxolone treatment in patients with CDKL5 deficiency disorder: 8-month minimum open-label extension follow-up [abstract no. 2.217 plus poster]. In: 75th Annual Meeting of the American Epilepsy Society. 2021.
National Organization for Rare Disorders Inc. CDKL5 deficiency disorder. 2020. https://rarediseases.org/rare-diseases/cdkl5/. Accessed 5 Dec 2022.
Amin S, Monaghan M, Aledo-Serrano A, et al. International Consensus Recommendations for the assessment and management of individuals with CDKL5 deficiency disorder. Front Neurol. 2022;13: 874695.
Acknowledgements
The manuscript was reviewed by: Y. Prashar, Department of Pharmacology, Rayat Institute of Pharmacy, Punjab, India; A. Strzelczyk, Epilepsy Center Frankfurt Rhine-Main, Department of Neurology, University Hospital Frankfurt, Frankfurt am Main, Germany. During the peer review process, Marinus Pharmaceuticals, Inc., the marketing authorization holder of ganaxolone, was also offered an opportunity to provide a scientific accuracy review of their data. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and conflict of interest
S.J. Keam is a contracted employee of Adis International Ltd/Springer Nature and declares no relevant conflicts of interest. Z.T. Al-Salama, a salaried employee of Adis International Ltd/Springer Nature and an editor of Drugs & Therapy Perspectives, was not involved in any publishing decisions for the manuscript and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent for publication, Availability of data and material, Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keam, S.J., Al-Salama, Z.T. Ganaxolone in seizures associated with cyclin-dependent kinase-like 5 deficiency disorder: a profile of its use in the USA. Drugs Ther Perspect 39, 81–88 (2023). https://doi.org/10.1007/s40267-022-00976-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-022-00976-w