Abstract
Background
Cumulative evidence of dementia risk in patients taking proton pump inhibitors (PPIs) is still inconclusive, probably due to a variety of study designs.
Objective
This study aimed to compare how the association between dementia risk and use of PPIs differs by different outcome and exposure definitions.
Methods
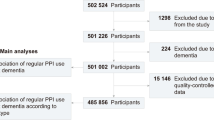
We conceptualized a target trial using claims data with 7,696,127 individuals aged 40 years or older without previous dementia or mild cognitive impairment (MCI) from the Association of Statutory Health Insurance Physicians in Bavaria. Dementia was defined as either including or excluding MCI to compare how the results alter by different outcome definitions. We used weighted Cox models to estimate the PPI initiation effect on dementia risk and weighted pooled logistic regression to assess the effect of time-varying use versus non-use during 9 years of study period, including 1 year of wash-out period (2009–2018). The median follow-up time of PPI initiators and non-initiators was 5.4 and 5.8 years, respectively. We also evaluated the association between each PPI agent (omeprazole, pantoprazole, lansoprazole, esomeprazole, and combined use) and dementia risk.
Results
A total of 105,220 (3.6%) PPI initiators and 74,697 (2.6%) non-initiators were diagnosed with dementia. Comparing PPI initiation with no initiation, the hazard ratio (HR) for dementia was 1.04 [95% confidence interval (CI) 1.03–1.05]. The HR for time-varying PPI use versus non-use was 1.85 (1.80–1.90). When MCI was included in the outcome, the number of outcomes increased to 121,922 in PPI initiators and 86,954 in non-initiators, but HRs remained similar, showing 1.04 (1.03–1.05) and 1.82 (1.77–1.86), respectively. Pantoprazole was the most frequently used PPI agent. Although the estimated HRs for the time-varying use effect of each PPI showed different ranges, all agents were associated with an increased dementia risk. A total of 105,220 (3.6%) PPI initiators and 74,697 (2.6%) non-initiators were diagnosed with dementia. Comparing PPI initiation with no initiation, the hazard ratio (HR) for dementia was 1.04 [95% confidence interval (CI) 1.03–1.05]. The HR for time-varying PPI use versus non-use was 1.85 (1.80–1.90). When MCI was included in the outcome, the number of outcomes increased to 121,922 in PPI initiators and 86,954 in non-initiators, but HRs remained similar, showing 1.04 (1.03–1.05) and 1.82 (1.77–1.86), respectively. Pantoprazole was the most frequently used PPI agent. Although the estimated HRs for the time-varying use effect of each PPI showed different ranges, all agents were associated with an increased dementia risk.A total of 105,220 (3.6%) PPI initiators and 74,697 (2.6%) non-initiators were diagnosed with dementia. Comparing PPI initiation with no initiation, the hazard ratio (HR) for dementia was 1.04 [95% confidence interval (CI) 1.03–1.05]. The HR for time-varying PPI use versus non-use was 1.85 (1.80–1.90). When MCI was included in the outcome, the number of outcomes increased to 121,922 in PPI initiators and 86,954 in non-initiators, but HRs remained similar, showing 1.04 (1.03–1.05) and 1.82 (1.77–1.86), respectively. Pantoprazole was the most frequently used PPI agent. Although the estimated HRs for the time-varying use effect of each PPI showed different ranges, all agents were associated with an increased dementia risk.A total of 105,220 (3.6%) PPI initiators and 74,697 (2.6%) non-initiators were diagnosed with dementia. Comparing PPI initiation with no initiation, the hazard ratio (HR) for dementia was 1.04 [95% confidence interval (CI) 1.03–1.05]. The HR for time-varying PPI use versus non-use was 1.85 (1.80–1.90). When MCI was included in the outcome, the number of outcomes increased to 121,922 in PPI initiators and 86,954 in non-initiators, but HRs remained similar, showing 1.04 (1.03–1.05) and 1.82 (1.77–1.86), respectively. Pantoprazole was the most frequently used PPI agent. Although the estimated HRs for the time-varying use effect of each PPI showed different ranges, all agents were associated with an increased dementia risk.A total of 105,220 (3.6%) PPI initiators and 74,697 (2.6%) non-initiators were diagnosed with dementia. Comparing PPI initiation with no initiation, the hazard ratio (HR) for dementia was 1.04 [95% confidence interval (CI) 1.03–1.05]. The HR for time-varying PPI use versus non-use was 1.85 (1.80–1.90). When MCI was included in the outcome, the number of outcomes increased to 121,922 in PPI initiators and 86,954 in non-initiators, but HRs remained similar, showing 1.04 (1.03–1.05) and 1.82 (1.77–1.86), respectively. Pantoprazole was the most frequently used PPI agent. Although the estimated HRs for the time-varying use effect of each PPI showed different ranges, all agents were associated with an increased dementia risk.A total of 105,220 (3.6%) PPI initiators and 74,697 (2.6%) non-initiators were diagnosed with dementia. Comparing PPI initiation with no initiation, the hazard ratio (HR) for dementia was 1.04 [95% confidence interval (CI) 1.03–1.05]. The HR for time-varying PPI use versus non-use was 1.85 (1.80–1.90). When MCI was included in the outcome, the number of outcomes increased to 121,922 in PPI initiators and 86,954 in non-initiators, but HRs remained similar, showing 1.04 (1.03–1.05) and 1.82 (1.77–1.86), respectively. Pantoprazole was the most frequently used PPI agent. Although the estimated HRs for the time-varying use effect of each PPI showed different ranges, all agents were associated with an increased dementia risk.A total of 105,220 (3.6%) PPI initiators and 74,697 (2.6%) non-initiators were diagnosed with dementia. Comparing PPI initiation with no initiation, the hazard ratio (HR) for dementia was 1.04 [95% confidence interval (CI) 1.03–1.05]. The HR for time-varying PPI use versus non-use was 1.85 (1.80–1.90). When MCI was included in the outcome, the number of outcomes increased to 121,922 in PPI initiators and 86,954 in non-initiators, but HRs remained similar, showing 1.04 (1.03–1.05) and 1.82 (1.77–1.86), respectively. Pantoprazole was the most frequently used PPI agent. Although the estimated HRs for the time-varying use effect of each PPI showed different ranges, all agents were associated with an increased dementia risk.A total of 105,220 (3.6%) PPI initiators and 74,697 (2.6%) non-initiators were diagnosed with dementia. Comparing PPI initiation with no initiation, the hazard ratio (HR) for dementia was 1.04 [95% confidence interval (CI) 1.03–1.05]. The HR for time-varying PPI use versus non-use was 1.85 (1.80–1.90). When MCI was included in the outcome, the number of outcomes increased to 121,922 in PPI initiators and 86,954 in non-initiators, but HRs remained similar, showing 1.04 (1.03–1.05) and 1.82 (1.77–1.86), respectively. Pantoprazole was the most frequently used PPI agent. Although the estimated HRs for the time-varying use effect of each PPI showed different ranges, all agents were associated with an increased dementia risk.A total of 105,220 (3.6%) PPI initiators and 74,697 (2.6%) non-initiators were diagnosed with dementia. Comparing PPI initiation with no initiation, the hazard ratio (HR) for dementia was 1.04 [95% confidence interval (CI) 1.03–1.05]. The HR for time-varying PPI use versus non-use was 1.85 (1.80–1.90). When MCI was included in the outcome, the number of outcomes increased to 121,922 in PPI initiators and 86,954 in non-initiators, but HRs remained similar, showing 1.04 (1.03–1.05) and 1.82 (1.77–1.86), respectively. Pantoprazole was the most frequently used PPI agent. Although the estimated HRs for the time-varying use effect of each PPI showed different ranges, all agents were associated with an increased dementia risk.
Conclusion
Our large study supports existing evidence that PPI use is related to an increased risk of dementia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Increased dementia risk by PPI use did not differ, whether or not the definition of dementia included mild cognitive impairment. |
Different PPI agents showed the different risk-increasing effect on dementia that warrants further investigation. |
While our German big data showed an increased risk of dementia with PPI use, discrepancies in dementia risk by PPI use from other studies may be due to various countries where the studies were conducted, which means different PPI use patterns. |
1 Introduction
Proton pump inhibitors (PPIs) are widely used to treat disorders of excessive gastric acid production, thanks to their well-established therapeutic effectiveness [1, 2]. Since an increased risk of dementia by PPI intake and plausible pathophysiological pathways have been reported [3, 4], a considerable number of observational studies have examined the association between PPI intake and the risk of dementia [5,6,7,8,9,10]. PPIs are among the most often used medications. Therefore, the safety of PPIs is a crucial clinical concern. However, the cumulative evidence is still inconclusive, and systematic reviews [11, 12] have pointed out a lack of well-designed research to establish reliable evidence.
Several possible reasons could have caused discrepancies in the previously performed studies. We found that dementia was differently defined in each study. In some studies, mild cognitive impairment (MCI) was also categorized as dementia [9, 13,14,15], or the outcome of interest was cognitive function scores as a continuous variable rather than a medical diagnosis of dementia [16, 18]. Interestingly, most studies that included MCI as an outcome presented no association between PPI intake and risk of dementia or even a protective effect of PPI intake on the dementia risk [9, 13,14,15, 17, 18]. Given that the overall reversion rate from MCI to normal cognition is approximately 18% depending on subject-based factors such as recovery from sickness and different diagnostic measurements for cognitive functions [19], the varying outcome definitions used in the available studies could have yielded conflicting results. In a study using claims data, the question whether dementia was diagnosed by a neurologist could also be an important issue in the context of outcome misclassification [20].
In addition, individuals who had ever received PPI treatment were included as PPI users without information on treatment adherence or period [14, 21]. Although PPI intake patterns rely on the patients’ gastric symptoms and general health status even without properly documented indication in practice [22, 23], the assessment of time-varying PPI use is lacking in previously conducted research. We recently performed an analysis of time-varying PPI use on the risk of dementia by using claims data from a German statutory health insurance [5]. To our knowledge, there is no other study that assessed the time-varying use effect of PPIs on dementia risk, which makes a comparison for results unavailable.
In this study, we describe results comparing the risk of dementia in those who were treated with PPIs by applying different outcome definitions, either solely dementia or dementia including MCI, using real-world big data from Germany. The focus was put on the assessment of the effect of time-varying PPI use on dementia risk with adjustment for time-varying confounding beyond the treatment initiation effect. We also estimated the association between the use of each PPI agent (omeprazole, pantoprazole, lansoprazole, esomeprazole, and combined use) and the incidence of dementia, and further compared the results with other studies similarly conducted but in different countries [24, 25]. In summary, the various analyses and comparisons could contribute to cumulative evidence to determine causality between PPI use and dementia and be a useful source for decisions in clinical practice.
2 Material and Methods
2.1 Data Source and Participants
In Germany, health insurance has been compulsory since 2009. It consists of two systems: the statutory health insurance (SHI) and the private health insurance sectors; most people in Bavaria (87.3%) are insured by SHI [26]. This study used administrative claims data from the KVB (German: Kassenärztliche Vereinigung Bayerns; The Bavarian Association of Statutory Health Insurance Physicians). The KVB is the largest of 17 regional associations of SHI physicians in Germany, and represents about 26,000 physicians and psychotherapists and makes sure that all SHI-insured patients (about 11 million people in Bavaria) have access to medical care any time. Additionally, the work of KVB is subject to the legal supervision of the Bavarian State Ministry of Health [27]. The anonymized dataset of claims data from all statutory health insurance companies in the Federal State of Bavaria between the calendar years 2010 and 2018 was provided. Given people with early-onset dementia are already in their 40s, all individuals aged 40 years or older with at least 1 year of continuously insured records before and after study entry were included [28].
The dataset consisted of information on patients’ year of birth, sex, codes according to the Anatomical Therapeutic Chemical Classification (ATC) of prescription medications, and diagnoses [International Classification of Diseases (ICD-10 system)]. Diagnoses were transferred quarterly by physicians, while data on reimbursable medications were acquired from pharmacies. Inpatient claims data are generally not registered by the KVB.
The present study has been approved by the ethics committee of the Medical Faculty of the Ludwig Maximilians-University Munich, Germany. Since the data were anonymized and produced for research purposes, consent from study participants was not required.
2.2 Medication Exposure and Outcomes
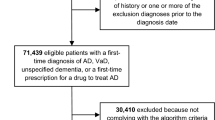
We defined an initiation of any PPI (ATC codes A02BC01-06) at baseline and non-initiation. The combined use was defined if the study subject had prescriptions for two or more PPI agents at any time during the study period. PPI use was assessed using prescriptions dispensed by community pharmacies and applying a 1-year washout period, as over-the-counter (OTC) use was unavailable in our data. The first PPI dispensing date formed the index date for each individual in the PPI initiator group. Individuals who were eligible as PPI initiators were followed-up and compared with non-initiators (Supplementary Figure S1). To minimize the selection bias in the group of non-initiators, we emulated a target trial [29]. Each participant had several trials with different enrollment points, i.e., every quarter of the year from when they became eligible to the end of study participation [30]. All person trials were pooled in the emulated trials of non-initiators. We then randomly selected non-initiators from the person trials by 1:1 matching for cohort entry time [31]. Follow-up for study outcomes started after initiation of treatment and continued until the occurrence of an outcome of interest, loss to follow-up, or the end of the study period on 31 December 2018. Because patients’ data were transferred quarterly, the upper limit of the interval (i.e., the last day of each quarter) was assigned for the end of follow-up, which corresponds to the usual method for the interval-censored data analysis [32]. The primary outcome of interest was the incidence of dementia. To ascertain the incidence of dementia, the ICD-10 codes for dementia (F00, F01, F03, F05.1, G30, G31.0, G31.1, G31.9, and F02.8+G31.82) [33] had to be found at least twice in consecutive quarters. We also included the ICD-10 code F06.7 for MCI in the outcome definition to compare how the risk of dementia alters by different outcome definitions.
2.3 Covariates
We controlled analyses for several confounders, considering direct causes of the exposure or outcome or both, which would identify a sufficient set of confounding factors [2, 34, 35], which means adjustments for covariates that are either the cause of the exposure or outcome and are not on the causal pathway to the outcome (mediators) or variables affecting the outcome only through the exposure (instrumental variables). The covariates encompass participants’ demographics (age and sex), calendar year of study entry, comorbidities, and medication use. Compared with our previous work, the approved indications of PPI were additionally controlled to minimize the unmeasured confounding. Participants’ baseline characteristics were measured in the 2-year quarters preceding cohort entry. A complete list of participants’ characteristics and a definition of covariates are provided in Supplementary Table S2.
2.4 Statistical Analysis
We used weighted Cox regression models with robust standard errors to estimate the effect of PPI initiation versus non-initiation on dementia risk. Entropy balancing was used to adjust for confounding [36, 37]. Standardized mean differences were used to examine the balance in the covariates between PPI initiators and non-initiators before and after weighting [37]. Overall exposure-specific survival was plotted as Kaplan–Meier estimates [38]. We estimated hazard ratios (HRs) with the corresponding 95% confidence intervals (CIs). To reduce the potential for reverse causality, we applied a 1-year lag window, where we censored dementia cases occurring during the first year of follow-up [39].
We used weighted pooled logistic regression models to examine the effect of time-varying PPI use on dementia risk because the status of PPI treatment varies depending on patients’ health conditions in general practice [22, 23]. This method, known as a marginal structural model, is an observational-based method and has recently often been used to analyze complex real-world data [40–42]. As we assessed baseline confounder in the 2-year quarters preceding cohort entry, we constructed a dataset consisting of follow-up intervals of 6 months for consistency. In other words, we calculated updated weights of each individual at every 6 months. Stabilized inverse probability of treatment weights were used to adjust for the time-varying confounding [37, 38]. Additionally, the inverse probability of being censored was calculated to adjust for time-varying selection bias [43]. This approach can be considered as an analysis of the continuous PPI treatment effect and is analogous to analysis in an unblinded RCT [44]. A survival curve standardized for baseline covariates and weighted for time-varying confounders was also drawn [38].
To examine whether the effect of each PPI agent (omeprazole, pantoprazole, lansoprazole, esomeprazole, and combined use) on the risk of dementia is equivalent, we further performed both analyses of each PPI agent by using the non-initiator group as a reference.
We performed several sensitivity analyses to examine the extent to which observed associations could be due to bias. As the first sensitivity analysis, we fit the same weighted Cox model and pooled logistic regression models restricting to the individuals aged 70 years or older. This restriction strategy aims to assess the risk of dementia by PPI intake altered by survival bias [39]. For the second sensitivity analysis, we repeated our analyses by defining the outcome of dementia or MCI diagnosed by a neurologist or psychiatrist due to the possible overestimation of incident dementia in the claims data [20].
Lastly, we computed an E-value, which indicates the minimum strength of an association that an unmeasured confounder would need to have to account for the observed association between PPI intake and dementia risk [45]. Analyses were performed using R (version 3.6.3).
3 Results
In our dataset of 7,696,127 individuals, 2,886,733 PPI initiators were observed. We randomly selected the same number of non-initiators. The median follow-up time of PPI initiators and non-initiators was 5.4 [interquartile range (IQR) 3.1–7.2] years and 5.8 (IQR 3.3–7.3) years, respectively. The median age of the whole study population was 58.0 (IQR 49.0–71.0) years, and 56.4% were women. We provided the baseline covariates of the study population in Table 1. PPI initiators were older and more likely to have more commodities and concomitant medication compared with non-initiators. However, both groups were well balanced on the confounders after weighting.
There were 105,220 cases of dementia in PPI initiators (3.6%) and 74,697 cases in non-initiators (2.6%) (Table 2). When MCI was also included in the outcome, 121,922 (4.2%) and 86,954 (3.0%) cases were observed in the PPI initiators and non-initiators, respectively. However, both HRs for different outcome definitions were the same (HR 1.04, 95% CI 1.03–1.05). Survival curves comparing outcome-free survival among initiators of PPIs versus non-initiators were provided (Supplementary Figure S3).
In the analysis of time-varying PPI use versus non-use that considered time-varying confounding and censoring, increased dementia risk by PPI use was observed again (HR 1.85, 95% CI 1.80–1.90). The risk of dementia, including MCI, was similar (HR 1.82, 95% CI 1.77–1.86). The survival curves standardized for baseline covariates and weighted for time-varying confounders showed that PPI use gradually increased the risk of dementia as PPI treatment period was extended (Fig. 1).
When we assessed the effect of each PPI agent on the risk of dementia (Table 3) or dementia including MCI (Table 4), we found a protective initiation effect by combined use of PPI, unlike the use of each separate type of PPI. However, the analyses for time-varying use showed that all types of PPI agents increased the risk of dementia whether MCI was included as outcome or not (Tables 3 and 4). The characteristics of initiators of each PPI agent are presented in Supplementary Table S4 with standard mean differences for PPIs and non-initiation. Individuals who received only pantoprazole treatment were 61.5% of all PPI initiators. In general, pantoprazole users took more co-medications. Only 800 PPI new users initiated and continued rabeprazole treatment. Due to the small number of users, rabeprazole was not further analyzed. Three individuals who initiated dexlansoprazole treatment were included in the group of combined use. Survival curves comparing outcome-free survival among each PPI agent user and non-initiator were consistent with these findings (Supplementary Figure S5).
In the sensitivity analysis restricted to participants aged 70 years or older, we found individuals were generally unhealthier whether they were PPI initiators or non-initiators (Supplementary Table S6) compared with the whole study population. An interesting finding is that PPI indications were less frequently observed in old PPI initiators (27.1%) compared with PPI initiators from the whole study population (28.3%). We did not find an increased dementia risk by PPI initiation in the elderly population (HR 0.99, 95% CI 0.98–1.00), and even a protective effect was observed when MCI was considered as an outcome (HR 0.94, 95% CI 0.93–0.95). However, time-varying PPI use analysis with adjustment for time-dependent variables showed an increased risk of dementia (HR 1.82, 95% CI 1.75–1.88) (Supplementary Table S7), which is comparable to the results of the main analysis. Unlike in the older population, PPI initiation and its long-term use showed risk-increasing effects in the younger population (Supplementary Table S8).
When we repeated our analyses, defining the outcome as dementia diagnosed by neurologists or psychiatrists, the total number of dementia cases decreased to 30,825, which is only 17% of the event cases in the primary analysis. However, effect estimates were similar to the HRs of the primary analysis (Supplementary Table S9). If MCI was included in the outcome, the number of events was 39,324.
The calculated E-value implicated that observed association between time-varying PPI use and dementia risk could be explained away if an unmeasured confounder has a relation with both exposure and outcome with a relative risk (RR) of 3.10 or higher. In addition, the unmeasured confounder needs to be associated with PPI initiation and dementia, with RR of at least 3.0 to shift the lower CI limit (i.e., 1.80) to the null.
4 Discussion
This research presents the first comparison of dementia risk by PPI use by applying different exposure and outcome definitions, suggesting that initiation and long-term use of PPIs increase the risk of dementia.
Since previously conducted studies have reported inconsistent results on the association between the use of PPIs and dementia risk, no consensus has been achieved yet [11, 46, 47]. Under the assumption that the inconclusive findings were due to different exposure and outcome definitions and study designs that cause bias, we aimed to compare how the results vary by the different definitions of exposure and outcome and the included study participants.
In our main analysis, in which all eligible study participants were included, we did not find a difference in the risk of dementia when the dementia was defined including MCI or not. However, the results were different by the definition of exposures. When we assessed the initiation effect of PPI treatment on the risk of dementia, a slightly increased dementia risk was observed (HR 1.04, 95% CI 1.03–1.05). In the analysis of the time-varying use effect where PPI use and time-varying covariates were assessed at 6–month intervals, we found a HR of 1.85 (95% CI 1.80–1.90) for dementia only and a HR of 1.82 (95% CI 1.77–1.86) for dementia or MCI. There was no remarkable difference in the risk by the different outcome definitions as described above.
We explored our data and found that the PPI intake pattern changed dynamically through the study period. In general, individuals who initiated PPIs at baseline did not continue the PPI intake during the whole study period. Instead, most PPI users received intermittent treatments. During the first follow-up interval, 93.5% of PPI users were those who had already initiated PPIs at baseline (Supplementary Table S10-A). The rate of PPI initiators at baseline who were also included as PPI users at each follow-up interval gradually decreased to 73.6% during the first 5 years, and it remained similar afterwards. When we assessed how many PPI users received PPIs for two consecutive follow-up intervals (i.e., 1 year), we could see that most PPI users continued their treatment from baseline until the second follow-up. From then on, it was shown that between 67.0% and 79.5% of PPI users at each interval also received PPIs for at least two consecutive follow-up intervals.
Regarding time-varying confounders, while the participants who took PPIs during the first follow-up interval were generally healthier than the PPI users at baseline (Table 1), the indications for PPI were similarly observed during the first follow-up period (28.9%) compared with baseline (28.3%). From the second follow-up, PPI users at each follow-up always had more comorbidities compared with the baseline, which is regarded as related to the survival bias. In particular, 46.2% of PPI users had PPI indications at the last follow-up, showing a more considerable rise in frequency compared with the degree of increase in other comorbidities. Concomitant medication use was already more frequent at the first follow-up interval than at baseline. Contrary to the characteristics of PPI users at each interval, the comorbidities and use of co-medications in non-users increased only slightly as more follow-up time went by (Supplementary Table S10-B).
Longitudinal studies usually aim to estimate the effect of a time-varying exposure on the outcome, and adjustment for time-varying confounding is required [43, 48]. Given that PPI intake patterns alter dynamically and confounders change over time, as shown in our dataset, we focus more on analyzing the time-varying use effect rather than the initiation effect. The control for the time-varying confounders ensures that both are neither affected by the previous treatment levels nor affect the subsequent treatment levels.
We performed further analyses to assess the effect of each PPI agent on the risk of dementia (omeprazole, pantoprazole, lansoprazole, esomeprazole, and combined use). As observed in the primary analysis, there were no remarkable differences in the risk of dementia by use of each PPI agent depending on the different outcome definitions (i.e., dementia only or dementia including MCI) (Tables 3 and 4). Interestingly, individuals who took combined types of PPIs had a lower risk of dementia in the initiation effect analysis, although the use of each single PPI agent showed an increased risk of dementia. Nevertheless, time-varying use effect analyses showed similarly increased dementia risks regardless of the type of PPI agents taken. Whereas other baseline covariates of users of combined PPI types were similar to those of other PPI type users, a distinctively high proportion of women (61.2%) was found in the combination group (Supplementary Table S4). In addition, the combined type of users had the longest median follow-up time of 6.8 (IQR 5.1–7.7) years among different PPI user groups, and it was also much longer than the median follow-up time of non-initiators (5.8 years, IQR 3.3–7.3 years). We assumed that those differences between the combined use and other PPI groups caused the difference in the results of initiation effect analysis.
Taipale et al. [24] reported no association between omeprazole, pantoprazole, rabeprazole, or esomeprazole and the risk of Alzheimer’s disease in their nested case-control study (3-year lag window applied). On the contrary, lansoprazole (HR 1.05, 95% CI 1.01–1.09) or combined use (HR 1.04, 95% CI 1.01–1.07) slightly increased the risk of Alzheimer’s disease in their study. Another nested case-control study by Imfeld et al. [25] also showed no association between pantoprazole, rabeprazole, or esomeprazole intake and Alzheimer’s disease risk. Although the authors even presented the protective effect of omeprazole, lansoprazole, or combined use on the risk of Alzheimer’s disease, they did not provide more detailed information on the characteristics of each group. Therefore, we are unable to further compare the results from those studies with our findings. In addition, those two studies examined the risk of Alzheimer’s disease, while we additionally included other common types of dementia in the analysis.
A noticeable finding was that each study described a distinctly different distribution of PPI agents in PPI users. While pantoprazole dominated in our German study, omeprazole was more frequently used in the UK [25]. Combined use occupied the most considerable proportion in Finland [24]. It has been reported that different types of PPIs are preferred country by country, probably due to various healthcare systems, drug approval processes, or pharma contracts, though no differences in therapeutic efficiency exists between the specific agents at equivalent doses [2, 49]. Previous studies have reported cholinergic dysfunction and increased amyloid beta peptide levels by PPI use as possible biological mechanisms [3, 4]. Despite such possible pathophysiological pathways of PPI use to the incidence of dementia [3, 4], no pharmacodynamic investigation was made to answer whether each PPI agent has a different impact on the risk of dementia.
We conducted a sensitivity analysis restricting to the older study population (aged 70 years or older) because the inconclusive results in the previous studies could have been induced due to survival bias. In other words, an underestimation of dementia incidence in older survivors was possible in the previous studies that included only elderly subjects [37]. No evidence of increased dementia risk by PPI use was often observed in studies in which the mean or median age of participants was high [24, 25, 50]. Meanwhile, the studies including a wider age range more often reported an increased risk of dementia by PPI use [5, 7, 51]. It has been explained in the literature that including older individuals may attenuate the effect of risk factors, or the association could even be protective [37]. As discussed in the literature, we found no association between PPI initiation and risk of dementia in our older study population (Supplementary Table S7). When the outcome was defined as dementia including MCI, PPI initiation even showed a protective effect (HR 0.94, 95% CI 0.93–0.95). However, we reported here an increased dementia risk by time-varying PPI use, although HRs became smaller compared with the HRs of the primary analysis, in which we included persons aged 40 years or older. On the contrary, a population younger than 70 years showed similar results to our primary analysis (Supplementary Table S8). Therefore, it is confirmed that there was potential for survival bias in studies including only older adults. Due to the non-availability of mortality data in our dataset, however, we could not further address the survival bias as a source of bias.
For another sensitivity analysis, we strictly defined dementia or MCI, restricting to the diagnosis made by neurologists or psychiatrists. The absolute number of outcomes decreased to 17.1% (dementia only) and 18.8% (dementia or MCI) compared with the number of outcomes in the primary analysis. Nevertheless, the HR estimates for the initiation effect and time-varying use effect were similar to those from the primary analysis (Supplementary Table S9).
In this study, we did not compare PPIs with an active comparator, which is histamine-2 receptor antagonists (H2RAs), because an active comparator should have a known safety profile concerning the outcome of interest [52, 53]. However, it has been shown that H2RAs also may increase the risk of dementia in previous studies. We discussed this issue in detail in our earlier report [5].
Despite the statistical approaches to mitigating bias in the design of non-randomized studies, there could be residual confounding. We did not adjust our models for lifestyle factors such as socioeconomic status. However, we included available ICD-10 codes for several lifestyle factors (e.g., obesity and alcohol abuse). Unlike our previous study [5], we adjusted our models for the approved indications for PPI use in this study. It is still unclear whether treatment indications for PPIs directly or indirectly affect our outcome of interest. However, a recent study discussed the relationship between the risk of dementia and gastroesophageal reflux [54]. More broadly, the association between gut–brain axis and Alzheimer’s disease has been actively discussed in past years [55, 56]. Therefore, we included indications for PPI treatment in the model to minimize unmeasured confounding and indication bias [57].
In our additional analysis to examine bias by unmeasured confounding, we obtained an E-value of 3.10, which means that an unmeasured confounder with a relationship with both PPI use and dementia risk needs an effect of at least 3.10 or RR beyond the measured confounders to revoke the observed effect estimate. We presume that each unobserved risk factor does not have greater RR than the calculated E-value. However, the observed effect estimate would become smaller if more risk factors are added in the analysis for model adjustment. Regarding the generalizability, as the population of this study was from KVB dataset, which covers 11 million people in the federal state of Bavarian in Germany, the question of if the study population represents the Bavarian population is redundant. The findings could be applicable to other regions in Germany and other countries similar to Germany in terms of lifestyles and ethnic proportions.
The study have several limitations. We had no hospitalization data. Thus, there is a possible underestimation of numbers in both exposure and outcome of interests. However, the simultaneously underestimated number of dementia diagnoses could attenuate the influence of underestimated PPI consumption.
Another limitation is that adherence data and OTC use was not available due to the nature of claims data. Since OTC data are not included, PPI users might have been categorized as non-initiator. It might cause an underestimation of the effect of PPI use. At the same time, PPIs could have been overestimated when the subjects took PPI on demand. As a result, the overall influence of exposure measurement error is expected to attenuate toward the null.
One more point to be considered is the age of study population. While previous studies have often shown older average age at dementia diagnosis, focusing on late-onset dementia [24, 58], the minimum eligible age of the population in the present study is relatively young (40 years or older). Therefore, the results might reflect both early-onset and late-onset dementia. Although there are other studies including younger individuals [51, 59], late-onset dementia is more common and frequently discussed in dementia studies [58]. Thus, a careful comparison of the results is required. Given PPIs are among the most frequently used treatment options, the safety issue is therefore an important consideration in clinical settings, and the findings of this study, together with its strengths and limitations, could be a useful source for decisions in clinical practice.
5 Conclusion
This study reports an increased risk of dementia by PPI use in the general population and also contributes to cumulative evidence by providing the comparison of results by different definitions of exposure and outcome. Therefore, physicians and patients are recommended to avoid overuse of PPIs. Given the country-specific preferences for specific PPI agents and our finding that dementia risk slightly differs by PPI agents, comparing the effect of each PPI agent on dementia risk is warranted in further studies.
References
Lassalle M, Le Tri T, Bardou M, Biour M, Kirchgesner J, Rouby F, et al. Use of proton pump inhibitors in adults in France: a nationwide drug utilization study. Eur J Clin Pharmacol. 2020;76:449–57.
Rückert-Eheberg IM, Nolde M, Ahn N, Tauscher M, Gerlach R, Güntner F, et al. Who gets prescriptions for proton pump inhibitors and why? A drug-utilization study with claims data in Bavaria, Germany, 2010–2018. Eur J Clin Pharmacol. 2021;78:657–67.
Kumar R, Kumar A, Nordberg A, Långström B, Darreh-Shori T. Proton pump inhibitors act with unprecedented potencies as inhibitors of the acetylcholine biosynthesizing enzyme-A plausible missing link for their association with incidence of dementia. Alzheimers Dement. 2020;16:1031–42.
Ortiz-Guerrero G, Amador-Munoz D, Calderon-Ospina CA, López-Fuentes D, Nava-Mesa MO. Proton pump inhibitors and dementia: physiopathological mechanisms and clinical consequences. Neural Plast. 2018;2018:5257285.
Ahn N, Nolde M, Günter A, Güntner F, Gerlach R, Tauscher M, et al. Emulating a target trial of proton pump inhibitors and dementia risk using claims data. Eur J Neurol. 2022;29(5):1335–43.
Chen LY, Lin HJ, Wu WT, Chen YC, Chen CL, Kao J, et al. Clinical use of acid suppressants and risk of dementia in the elderly: a pharmaco-epidemiological cohort study. Int J Environ Res Public Health. 2020;17:8271.
Lin H-C, Huang K-T, Lin H-L, Uang Y-S, Ho Y, Keller JJ, et al. Use of gastric acid–suppressive agents increases the risk of dementia in patients with upper gastrointestinal disease: a population-based retrospective cohort study. PLoS One. 2021;16: e0249050.
Torres-Bondia F, Dakterzada F, Galván L, Buti M, Besanson G, Gill E, et al. Proton pump inhibitors and the risk of Alzheimer’s disease and non-Alzheimer’s dementias. Sci Rep. 2020;10:21046.
Weiss A, Gingold-Belfer R, Boltin D, Beloosesky Y, Koren-Morag N, Meyerovitch J, et al. Chronic omeprazole use in the elderly is associated with decreased risk of dementia and cognitive decline. Dig Liver Dis. 2021;54:622–8.
Wu CL, Lei WY, Wang JS, Lin CE, Chen CL, Wen SH. Acid suppressants use and the risk of dementia: a population-based propensity score-matched cohort study. PLoS One. 2020;15: e0242975.
Wang H, Tian L, Yan X. No association between acid suppressant use and risk of dementia: an updated meta-analysis. Eur J Clin Pharmacol. 2022;78:375–82.
Yoon KB, Bang CS, Kim JS. Proton-pump inhibitors and the risk of dementia: a systematic review and meta-analysis. Korean J Helicobacter Up Gastrointest Res. 2021;21:135–43.
Cooksey R, Kennedy J, Dennis MS, Escott-Price V, Lyons RA, Seaborne M, et al. Proton pump inhibitors and dementia risk: evidence from a cohort study using linked routinely collected national health data in Wales, UK. PLoS One. 2020;15: e0237676.
Goldstein FC, Steenland K, Zhao L, Wharton W, Levey AI, Hajjar I. Proton pump inhibitors and risk of mild cognitive impairment and dementia. J Am Geriatr Soc. 2017;65:1969–74.
Wu B, Hu Q, Tian F, Wu F, Li Y, Xu T. A pharmacovigilance study of association between proton pump inhibitor and dementia event based on FDA adverse event reporting system data. Sci Rep. 2021;11:10709.
Herghelegiu AMP, Prada GI, Nacu R. Prolonged use of proton pump inhibitors and cognitive function in older adults. Farmacia. 2016;64:262–7.
Lochhead P, Hagan K, Joshi AD, Khalili H, Nguyen LH, Grodstein F, et al. Association between proton pump inhibitor use and cognitive function in women. Gastroenterology. 2017;153:971-9.e4.
Wod M, Hallas J, Andersen K, García Rodríguez LA, Christensen K, Gaist D. Lack of association between proton pump inhibitor use and cognitive decline. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2018;16:681–9.
Canevelli M, Grande G, Lacorte E, Quarchioni E, Cesari M, Mariani C, et al. Spontaneous reversion of mild cognitive impairment to normal cognition: a systematic review of literature and meta-analysis. J Am Med Dir Assoc. 2016;17:943–8.
Taylor DH Jr, Østbye T, Langa KM, Weir D, Plassman BL. The accuracy of Medicare claims as an epidemiological tool: the case of dementia revisited. J Alzheimers Dis. 2009;17:807–15.
Booker A, Jacob LE, Rapp M, Bohlken J, Kostev K. Risk factors for dementia diagnosis in German primary care practices. Int Psychogeriatr. 2016;28:1059–65.
Gamelas V, Salvado V, Dias L. Prescription pattern of proton pump inhibitors at hospital admission and discharge. GE Port J Gastroenterol. 2019;26:114–20.
Hayes KN, Nakhla NR, Tadrous M. Further evidence to monitor long-term proton pump inhibitor use. JAMA Netw Open. 2019;2:e1916184-e.
Taipale H, Tolppanen AM, Tiihonen M, Tanskanen A, Tiihonen J, Hartikainen S. No association between proton pump inhibitor use and risk of Alzheimer’s disease. Am J Gastroenterol. 2017;112:1802–8.
Imfeld P, Bodmer M, Jick SS, Meier CR. Proton pump inhibitor use and risk of developing Alzheimer’s disease or vascular dementia: a case-control analysis. Drug Saf. 2018;41:1387–96.
Chaibi S, Schulze Ehring F, Verband der Privaten Krankenversicherung e.V. PKV-Regionalatlas Bayern: Regionale Bedeutung der Privatversicherten für die medizinische Versorgung unter besonderer Berücksichtigung des ländlichen Raum. 2019.
The Bavarian Association of Statutory Health Insurance Physicians About Us. https://www.kvb.de/fileadmin/kvb/dokumente/UeberUns/KVB-About-us.pdf. Accessed 13 Feb 2023.
Knopman DS. Young-onset dementia—new insights for an underappreciated problem. JAMA Neurol. 2021;78(9):1055–6.
Hernan MA, Robins JM. Using big data to emulate a target trial when a randomized trial is not available. Am J Epidemiol. 2016;183:758–64.
Danaei G, Rodriguez LA, Cantero OF, Logan R, Hernan MA. Observational data for comparative effectiveness research: an emulation of randomised trials of statins and primary prevention of coronary heart disease. Stat Methods Med Res. 2013;22:70–96.
Ohneberg K, Beyersmann J, Schumacher M. Exposure density sampling: dynamic matching with respect to a time-dependent exposure. Stat Med. 2019;38:4390–403.
Panageas KS, Ben-Porat L, Dickler MN, Chapman PB, Schrag D. When you look matters: the effect of assessment schedule on progression-free survival. JNCI: J Natl Cancer Inst. 2007;99:428–32.
(ZI), Z.f.d.k.V.i.d.B.D. Demenz Zi-Kodier_Manual. 2020. https://www.zi.de/fileadmin/images/content/Kodierhilfe/Kodierrmanual_Demenz.pdf. Accessed 10 Feb 2023.
VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. 2019;34:211–9.
Budson AE, Kowall NW. The handbook of Alzheimer’s disease and other dementias. West Sussex: Blackwell Publishing Ltd; 2011.
Hainmueller J. Entropy balancing for causal effects: a multivariate reweighting method to produce balanced samples in observational studies. Polit Anal. 2012;20:25–46.
Matschinger H, Heider D, König HH. A comparison of matching and weighting methods for causal inference based on routine health insurance data, or: what to do if an RCT is impossible. Gesundheitswesen. 2020;82(S 02):s139–s50.
Cole SR, Hernán MA. Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed. 2004;75:45–9.
Weuve J, Proust-Lima C, Power MC, Gross AL, Hofer SM, Thiébaut R, et al. Guidelines for reporting methodological challenges and evaluating potential bias in dementia research. Alzheimers Dement. 2015;11:1098–109.
Belviso N, Zhang Y, Aronow HD, Wyss R, Barbour M, Kogut S, et al. Addressing posttreatment selection bias in comparative effectiveness research, using real-world data and simulation. Am J Epidemiol. 2022;191:331–40.
Tran T, Suissa S. Comparing new-user cohort designs: the example of proton pump inhibitor effectiveness in idiopathic pulmonary fibrosis. Am J Epidemiol. 2021;190:928–38.
Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11:561–70.
Mansournia MA, Etminan M, Danaei G, Kaufman JS, Collins G. Handling time varying confounding in observational research. BMJ. 2017;359: j4587.
Fewell Z, Hernán MA, Wolfe F, Tilling K, Choi H, Sterne JAC. Controlling for time-dependent confounding using marginal structural models. Stata J. 2004;4:402–20.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167:268–74.
Desai M, Nutalapati V, Srinivasan S, Fathallah J, Dasari C, Chandrasekhar VT, et al. Proton pump inhibitors do not increase the risk of dementia: a systematic review and meta-analysis of prospective studies. Dis Esophagus. 2020;33:doaa041.
Zhang Y, Liang M, Sun C, Song EJ, Cheng C, Shi T, et al. Proton pump inhibitors use and dementia risk: a meta-analysis of cohort studies. Eur J Clin Pharmacol. 2020;76:139–47.
Pazzagli L, Linder M, Zhang M, Vago E, Stang P, Myers D, et al. Methods for time-varying exposure related problems in pharmacoepidemiology: an overview. Pharmacoepidemiol Drug Saf. 2018;27:148–60.
Thomson AB. Are the orally administered proton pump inhibitors equivalent? A comparison of lansoprazole, omeprazole, pantoprazole, and rabeprazole. Curr Gastroenterol Rep. 2000;2:482–93.
Gray SL, Walker RL, Dublin S, Yu O, Aiello Bowles EJ, Anderson ML, et al. Proton pump inhibitor use and dementia risk: prospective population-based study. J Am Geriatr Soc. 2018;66:247–53.
Tai SY, Chien CY, Wu DC, Lin KD, Ho BL, Chang YH, et al. Risk of dementia from proton pump inhibitor use in Asian population: a nationwide cohort study in Taiwan. PLoS One. 2017;12: e0171006.
Yoshida K, Solomon DH, Kim SC. Active-comparator design and new-user design in observational studies. Nat Rev Rheumatol. 2015;11:437–41.
The European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP) Guide on Methodological Standards in Pharmacoepidemiology (Revision 10). https://www.encepp.eu/standards_and_guidances/documents/methodologicalGuideFullRevision10.pdf. Accessed 10 Feb 2023
Gau SY, Lai JN, Yip HT, Wu MC, Wei JC. Higher dementia risk in people with gastroesophageal reflux disease: a real-world evidence. Front Aging Neurosci. 2022;14: 830729.
Kowalski K, Mulak A. Brain-gut-microbiota axis in Alzheimer’s disease. J Neurogastroenterol Motil. 2019;25:48–60.
Saji N, Murotani K, Hisada T, Kunihiro T, Tsuduki T, Sugimoto T, et al. Relationship between dementia and gut microbiome-associated metabolites: a cross-sectional study in Japan. Sci Rep. 2020;10:8088.
Myers JA, Rassen JA, Gagne JJ, Huybrechts KF, Schneeweiss S, Rothman KJ, et al. Effects of adjusting for instrumental variables on bias and precision of effect estimates. Am J Epidemiol. 2011;174:1213–22.
Joling KJ, Janssen O, Francke AL, Verheij RA, Lissenberg-Witte BI, Visser PJ, et al. Time from diagnosis to institutionalization and death in people with dementia. Alzheimers Dement. 2020;16(4):662–71.
Park SK, Nam JH, Lee H, Chung H, Lee EK, Shin JY. Beyond uncertainty: negative findings for the association between the use of proton pump inhibitors and risk of dementia. J Gastroenterol Hepatol. 2019;34(12):2135–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the Innovation Committee at the Federal Joint Committee (Gemeinsamer Bundesausschuss, G-BA), the highest decision-making body of the joint self-government of physicians, dentists, hospitals, and health insurance funds in Germany (grant no. 01VSF18013). The funding agency played no role in the design, methods, data collections, analysis, and preparation of this article.
Competing interests
The authors declare no competing interests.
Author contributions
NA: study design, statistical analysis, interpretation of data, and writing and revising the manuscript; NW: statistical analysis, interpretation of data, and critical review of manuscript; SB: interpretation of data and critical review of manuscript; MN: interpretation of data and critical review of manuscript, RG: interpretation of data and critical review of manuscript; MT: interpretation of data and critical review of manuscript; AG: acquisition and interpretation of data and critical review of manuscript; FG: acquisition and interpretation of data and critical review of manuscript; IR: interpretation of data and critical review of manuscript; CM: study design, interpretation of data, and critical review of manuscript; JL: study design, interpretation of data, and critical review of manuscript.
Data availability statement
The data that support the findings of this study are available from the KVB (German: Kassenärztliche Vereinigung Bayerns; Association of Statutory Health Insurance Physicians of Bavaria) by contractual agreement.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ahn, N., Wawro, N., Baumeister, SE. et al. Time-Varying Use of Proton Pump Inhibitors and Cognitive Impairment and Dementia: A Real-World Analysis from Germany. Drugs Aging 40, 653–663 (2023). https://doi.org/10.1007/s40266-023-01031-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-023-01031-7