Abstract
Background
Potentially inappropriate prescribing (PIP) is commonly seen amongst the older population in all clinical settings, as indicated by several prevalence studies in several countries. Quantitative work such as this confirms that this is a global public health problem likely to grow in tandem with ageing of the global population. However, less attention has been focused on why it is happening and how it can be prevented.
Objective
The objective of this paper is to synthesise qualitative studies that explore PIP in older patients, in an effort to understand why it happens from a prescriber’s perspective and to generate a new theory to guide future interventional studies aimed at minimising it in older people. To date, there is no published systematic synthesis of this type.
Methods
Papers were deemed suitable for inclusion if they used qualitative methods, explored some area of PIP in patients over 65 years of age, were published in English and had available published abstracts. Four databases were systematically searched for papers published up to the end of April 2013: PubMed, Embase, CINAHL and Web of Knowledge. No date restrictions were applied. Key words searched were: Qualitative AND (Inappropriate* OR Appropriate* OR Safe) AND (Elderly OR Aged OR Geriatric* OR Old*) AND Prescri*. Reference lists were then searched for other suitable papers. Critical Appraisal Skills Programme criteria were used to assess quality. Meta-ethnography was used to synthesise the papers.
Results
Out of 624 papers identified, seven papers were deemed relevant. Four key concepts were identified as being causal factors in PIP: (1) the need to please the patient, (2) feeling of being forced to prescribe, (3) tension between prescribing experience and prescribing guidelines and (4) prescriber fear. These were re-interpreted in a line of argument synthesis indicating that some doctors have self-perceived restrictions with regard to prescribing appropriately because of a combination of factors, rather than any one dominant factor.
Conclusion
Prevention of PIP may be favourably influenced by addressing the key interactive determinants of inappropriate prescribing behaviour.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Qualitative work in the field of potentially inappropriate prescribing in older patients has never before been synthesised. |
This meta-synthesis indicates that doctors often have self-perceived restrictions leading to a sense of powerlessness to prescribe appropriately because of a combination of factors. |
Possible methods for empowering doctors to prescribe appropriately include educational interventions and improved communication between levels of care. |
1 Introduction
Potentially inappropriate prescribing (PIP) is commonly seen amongst the older population. There are various factors that make this group more susceptible to PIP, principally multiple co-morbidities and related polypharmacy [1, 2]. PIP includes both prescribing of potentially inappropriate medications (PIMs), i.e. introducing a medication that poses more risk than benefit when a safer alternative is available, as well as potential prescribing omissions (PPOs) [2–6], i.e. the omission of medications that would benefit the patient. In primary care, recent studies show that 20–40 % of older patients have experienced PIP [1–3]. The prevalence of PIP in these patients is 33–58 % in the hospital setting [4, 5] and rates of 44–70 % have been reported in long-term care facilities [6]. The common consequences of PIP are adverse drug reactions, adverse drug events, hospitalisation and inefficient use of resources [7–9].
Quantitative data such as these have highlighted the issue and attracted attention. However, very little attention has been focused on why it is happening. This paper aims to synthesise qualitative studies that explore PIP in older patients, using a meta-ethnographic approach, as developed by Noblit and Hare [10], in an effort to understand the psychological and behavioural basis of PIP applied to older people and to generate a new theory to guide future intervention studies aimed at PIP prevention. The few qualitative studies in the published literature have never previously been analysed in a meta-synthesis such as this before. Application of qualitative research methods in a variety of healthcare research domains [11] has provided important insights and understanding with relevance to clinical practice.
As with a meta-analysis of data from quantitative studies, a meta-synthesis of qualitative studies involves a recognised methodology for combining the themes from several studies. However, unlike a meta-analysis, a qualitative synthesis aims to interpret the thematic findings from the original studies so as to be able to generate a new all-encompassing theory not previously identified [11–14]. To do this, we chose a technique called meta-ethnography [10] for this meta-synthesis, which has been used to good effect in healthcare research [11, 14–16].
2 Methods
We used the seven-step model of meta-ethnography (Fig. 1), i.e.
In step 1, we agreed a clear statement of the specific research question.
In step 2, we developed a search strategy to identify suitable articles. Four databases were systematically searched for papers published up to the end of April 2013 (no start date was specified): PubMed, Embase, CINAHL and Web of Knowledge. The following terms were used: Qualitative AND (Inappropriate* OR Appropriat* OR Safe) AND (Elderly OR Aged OR Geriatric* OR Old*) AND Prescri*. We then searched the reference lists of papers located for other suitable papers that should be included in the meta-synthesis.
Papers were deemed suitable for inclusion if they used qualitative methods, explored some area of PIP in patients over 65 years of age, were published in English and had available published abstracts. Two researchers (SC and AF) then read articles that were deemed potentially relevant after the abstract review. Articles meeting inclusion criteria were included in the final review.
The quality of the final papers was assessed by two researchers using the Critical Appraisal Skills Programme (CASP). The CASP tool assesses qualitative papers on the basis of the results presented, the validity of the results and the potential implications of the results locally. The authors decided to use the CASP methodology as it has been used to good effect previously in healthcare research studies [11, 13, 15, 17]. The purpose of using the CASP was not to eliminate published papers, but rather to make sure the papers we used were of high quality, and to ensure low-quality papers were not contributing to our final synthesis.
Step 3 involved reading the studies. The terms first-order, second-order and third-order constructs relate to the different levels of interpretation within a meta-synthesis. First-order constructs relate to the raw data in the empirical studies, i.e. the original participants’ interpretations of a certain experience. Second-order constructs are the common themes/categories that the original authors identified amongst these participants and used as their results/findings. Third-order constructs are the new interpretations that those performing the synthesis must identify by compiling all the second-order constructs from the selected studies, translating them into each other to determine if in fact they concur in terms of thematic content, and then reinterpreting them to generate new theory. The papers were read carefully by two researchers. The key findings from each paper, as presented by the authors, were listed as the second-order constructs.
In step 4, we determined how the studies were related to each other by listing key concepts that represented the whole data set.
In step 5, we translated the papers into each other. There are numerous forms of final synthesis within meta-ethnography, the choice of which depends on how the papers are related to each other [10]. As it became apparent that concepts from one study would encompass others, if not all the other studies, the authors used ‘reciprocal translation’ followed by a ‘line of argument’ synthesis. Each key concept was compared across the published papers, to determine what each paper stated about that concept. In this way, the papers were translated into one another.
Step 6 involved examining what each paper stated about each concept, and reinterpreting these to produce third-order constructs, linked together in a final ‘line of argument’ synthesis. The aim of a ‘line of argument’ is to create a coherent theme that may explain what all the studies have reported in one holistic theme, taking into account the fact that each study may have explored different aspects of the phenomenon [18].
Finally, in step 7, we expressed the results of the synthesis in tables, figures and text. We used the ENTREQ (Enhancing transparency in reporting the synthesis of qualitative research) [19] statement, a framework for reporting the synthesis of qualitative health research, to guide how we reported the results.
3 Results
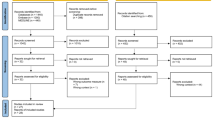
The search of the electronic databases identified 864 papers, leaving 624 after duplicates were removed (Fig. 2). After a title and abstract review, a further 576 were removed: 348 did not use qualitative methods, 176 did not involve PIP, 44 did not deal with patients over 65 years and eight had no abstracts available. Sixteen full papers were retrieved for review. Of these, ten were eliminated because they did not use qualitative methods. One additional paper was identified from the references list of another paper and included. This left seven papers for inclusion in the final synthesis (Table 1).
All seven papers were of high quality when assessed using the CASP criteria; all of the papers met most of the criteria for inclusion in the analysis. Common weaknesses were ‘reflexivity’ (the awareness of the researcher’s contribution to the construction of meanings throughout the research process), which none of the papers mentioned, ‘data collection’ (none of the papers justified methods chosen or discussed saturation of data) and ‘statement of findings’ (the vast majority of papers did not apply triangulation).
3.1 Reciprocal Translation
Four key concepts that reflected the findings in the seven papers were identified from the meta-synthesis as being contributory factors to PIP: (1) desire to please the patient, (2) feeling of being forced to prescribe, (3) tension between experience and guidelines and (4) prescriber fear. The reciprocal translation and final synthesis are presented below. Each of these thematic concepts is described in greater detail. Excerpts consisting of original quotes from participants (first-order constructs) as well as authors’ findings (second-order constructs), from the original papers are presented in Table 2 along with third-order interpretations to illustrate how the four themes were identified.
3.1.1 Please the Patient
In the majority of papers, there was a clear underlying theme of ‘wanting to please the patient’. This usually meant prescribing outside the guidelines but as Dickinson et al. [20] stated in their paper exploring inappropriate long-term prescribing of antidepressants, ‘… in many circumstances it is easier to follow the path of least resistance and let them (i.e. PIP decisions) be…’. This was a common viewpoint expressed by the doctors they interviewed. They noted that patients were happy with their antidepressants and as a result doctors were generally satisfied with the pharmacotherapy. They also observed that the doctors recognised the problem of prescribing medication even though the problem may be social rather than psychiatric in nature. However, because of some patients’ resistance to non-pharmacological treatments, they proceeded with prescribing the medication anyway.
Agarwal et al. [21] refers to this resistance from patients’ in their study of general practitioners’ (GPs’) approach to insulin prescribing in older patients. When asked why insulin is often under-prescribed in this population, the consensus was that ‘GPs felt older patients would be less receptive to medication regimen changes’. Spitz et al. [22] looked at underuse of opioids in older patients for non-cancer pain. In this study, the patient was also a common barrier to appropriate prescribing here, apparently as a result of older patients’ reluctance to consider opioid analgesia for this category of pain. The physician participants in this study also commented that this resistance acted as a barrier to prescribing these medications to future patients.
The concept of prescribing to please the patient was most evident in the paper by Cook et al. [23] who explored prescribers’ attitudes to prescribing benzodiazepines for older adults. These medications should only be used for brief periods in older patients and for symptomatic relief only [24, 25]. The participants in this study spoke of the problems they experienced in the past trying to wean patients off benzodiazepines and how this affected their future prescribing patterns. The participants again spoke of ‘the path of least resistance’ and how much quicker and easier it is just to prescribe what the patient wants, rather than spend significant amounts of time trying to persuade patients that a different approach to managing insomnia and anxiety would be preferable. They furthermore identified the possibility of the patients switching to another physician as a reason for inappropriate prescribing. This was also reported by Damestoy et al. [26], who studied physicians’ perspectives on prescribing psychotropic medication for older patients. The participants described how otherwise quiet and timid patients became aggressive and demanding when their anxiolytic use was questioned.
3.1.2 Forced to Prescribe
One consequence of this need to please the patient was that prescribers often felt they were forced into prescribing, or not prescribing medications, in a manner they knew did not adhere to guidelines. This concept could therefore have been integrated into the previous one; however, we consider it should stand alone, as there were several factors leading prescribers to feeling forced to prescribe, other than the need to please the patient, e.g. poor quality of treatment resources. Wood-Mitchell et al. [27] explored prescribing of medications for dementia in older patients. They observed that many of the prescribers felt they were seeing too many referred patients owing to a lack of support services for these patients. According to many prescribers, there was too much reliance on medication as a quick and ‘easy’ treatment for these patients and the development of non-pharmacological treatments was deployed less frequently as a result. Additionally, the quality-of-care settings were important in the prescribers’ decision process. Low-quality care staff training and ‘under-stimulating environments’ were thought to result in challenging behaviours in patients with dementia. These low-quality care facilities are then unable to cope with disturbed patient behaviour and are more likely to refer the patients for assessment with a view to pharmacotherapy for their disturbed behaviour. The physician prescribers then feel they have no choice but to prescribe owing to the lack of services already mentioned.
Agarwal et al. [21] also reported this lack of confidence amongst prescribers in some long-term care settings. In relation to not prescribing insulin, GPs knowledge of some care facilities hindered them from starting a patient on insulin because of the doctor’s lack of confidence in the support the patient would receive in care. Lack of alternatives was another factor leading to physicians feeling forced to prescribe something. Damestoy et al. [26] described how doctors felt that non-pharmacological treatments were insufficient for conditions such as anxiety, indicating that many doctors ‘considered them to be ineffective (and that) … psychotherapeutic approaches were doomed to failure’. This was echoed by Wood-Mitchell et al. [27], and again by Dickinson et al. [20], indicating long waiting lists for cognitive behavioural therapy. Damestoy et al. [26] also identified a feeling of isolation amongst prescribers, once again forcing them to prescribe in some situations where they realize that psychotropic medications are not appropriate. This theme of ‘isolation’ was also picked up by Spitz et al. [22] reporting that doctors desired more peer support to enable them to prescribe appropriately. Looking at these studies, it can be seen that prescribers know what is right, but feel unable to follow through.
3.1.3 Experience vs. Guidelines
In all but one of the papers, it was clear that prescribers were well aware of the potentially inappropriate nature of some of their prescribing. They were, for the most part, aware of the treatment guidelines and they all agreed as to what the best practice was. However, in general, they varied greatly in their actual practice. They perceived a significant problem in implementing these guidelines in real life. The end result was reversion to previous practices, and what they were familiar with. Lack of evidence supporting some guidelines also influenced prescribers in favour of their own experience as reported by Woods-Mitchell et al. [27]. Conversely, Agarwal et al. [21] reported that a prescriber’s lack of experience can have a similar effect in relation to under-prescribing of insulin.
Cook et al. [23] found that many prescribers considered that guidelines were ‘out of touch with real-world problems’ and that past experience had taught them to avoid changing drug therapy to avoid a perceived higher risk of misadventure. Damestoy et al. [26] reported that many of the physicians interviewed prescribed as they did because they did not often see adverse effects. Spitz et al. [22] used focus groups with prescribers to elucidate why opioids were underused in non-cancer pain in older people. They found that doctors were aware that opioids have a role in non-cancer pain, but felt the evidence base was insufficient to support this role. They also expressed their desire for evidence-based tools for calculating doses. Dickinson et al. [20] showed that in relation to long-term prescribing of antidepressants, GPs did not see much of a problem, as they have not seen any evidence to indicate serious harm to older patients.
3.1.4 Fear
The final concept evident across the papers reviewed was fear. It manifested itself in a number of different ways but in all cases it was clear that it was a contributing factor to PIP. For instance, Agarwal et al. [21] reported that doctors felt a sense of fear toward older patients in general owing to their frailty and co-morbidities. Consequently, they perceived more potential to do harm. They also observed a fear of the unknown amongst several GPs, e.g. most admitted to inexperience using insulin in older patients and found the prospect of initiating it anxiety provoking, such that they would avoid prescribing it even if guidelines recommended it. Dickinson et al. [20] also identified fear as a central theme amongst GPs in relation to PIP. Doctors described reluctance to stopping a medication that has been taken for a long time by a patient to avoid worry, and spoke of not wishing to disrupt patients’ clinical stability. With this fear of medication change and an apparent lack of fear of adverse effects (also reported), these authors concluded that there was no incentive for change. Fear of causing harm was the overwhelming barrier identified in the study by Spitz et al. [22]. Prescribers described genuine fear of prescribing opioids for older patients, and worry regarding the possible serious adverse effects. Sometimes these fears arose from previous bad experiences with prescribing opioids in older patients. In other cases, this fear was more to do with avoidance of the guilt that would ensue if a patient was to have an adverse drug event because of the drug. Spinewine et al. observed a different type of fear in their study looking at appropriateness of medicines in general in older patients [28]. Prescribers they interviewed described a fear of offending other doctors, including specialist doctors and GPs. If, for example, a doctor noticed something potentially inappropriate on a patient’s prescription, but if that patient was under the care of a specialist, they would be less likely to intervene. Similarly, when transferring information between levels of care, e.g. from hospital to primary care, it was noted that the amount of information could be limited because of fear of causing offence to patients’ GPs.
3.2 Line of Argument Synthesis
Looking at the four key concepts that emerged from the papers, we concluded that the literature actually indicates that, in many situations, prescribers suffer from ‘self-perceived restrictions’ leading to a sense of powerlessness to prescribe appropriately for older patients. This forces them to rely on what they know and have done before, which leads to the PIP that has been identified [4–8].
4 Discussion
Although the published literature abounds with papers describing the prevalence of PIP in various clinical settings and the link between PIP and multi-morbidity/polypharmacy in older people, there is a lack of scientific enquiry into the prescriber-based reasons that underpin PIP. This meta-synthesis has, for the first time, identified a cluster of reasons physicians feel may perpetuate PIP in older people. These reasons include (1) the need to please the patient, (2) feeling forced to prescribe, (3) tension between prescribing experience and prescribing guidelines and (3) prescriber fear. Ultimately, these factors in combination militate against safe and effective prescribing in older people.
To date, there is a lack of proven interventions that reliably counteract PIP in older patients. A recent review by O’Connor et al. [5] points toward four areas of intervention to counteract PIP in this population, namely comprehensive geriatric assessment, medication use review, prescriber education/audit/feedback and computerised prescriber order entry with clinical decision support. However, the evidence to support routine implementation of any of these interventions to prevent PIP in multi-morbid older patients is weak. Prescriber education interventions to prevent PIP in particular drug classes have been shown to work, e.g. antibiotics, opioid analgesics and antipsychotics [5]. However, interventions to guide prescribers away from PIP in the broad sense are lacking. Rather surprisingly, researchers have given relatively little attention to the prescriber as a prime target for attenuating PIP in the high-risk, older, multi-morbid population.
Whilst there may be other prescriber factors to consider other than the four prime reasons that predispose physicians to poor prescribing practices identified in this study, nevertheless, our findings provide an evidence-based platform for the design of more effective interventions as a means of PIP prevention in older populations. Whatever interventions are developed in the future, they must be able to empower physicians to prescribe in such a way as to improve adherence to guidelines, avoid feelings of being forced to prescribe inappropriately to please patients and fear of countermanding other physicians prescriptions.
The global expansion of the frail older population demands an improved level of education in geriatric pharmacology at the undergraduate and postgraduate level. Specifically, this will involve electronic education programmes that include self-testing and feedback. Importantly, recent discourse on prescriber ‘non-technical skills’ has cast new light on a previously neglected aspect of prescriber behaviour [29]. These ‘non-technical skills’ encompass communication, team-working/leadership, error awareness, risk assessment and situational awareness. This skill set must be incorporated into any prescriber education programme to enhance its efficacy. A model for the delivery of such an intervention has been suggested [29].
4.1 Limitations
Although we systematically searched for suitable papers, qualitative papers are often difficult to find because of ambiguous titles.
Meta-ethnography, while a useful tool for this type of research, is not an objective technique and is open to differing interpretations between different researchers.
Four of the seven papers included in this review concerned the prescribing of psychiatric medications. Mediators of PIP may differ between psychiatry and general medicine. Similarly, the mediators of the different forms of PIP (PIMs and PPOs) may differ. PIMs and PPOs were not separated for individual analysis in this paper.
5 Conclusion
PIP in older patients is a result of many factors, including patient-, prescriber- and system-level barriers. As a result, prescribers feel unable to prescribe in an appropriate manner. Possible remedies for this could include better communication, more comprehensive education and system-level interventions to enable prescribers to re-acquire this power. The problem is not a lack of guidelines, it is an abundance of barriers to implementing these guidelines, which need to be systematically removed.
References
Ryan C, O’Mahony D, Kennedy J, et al. Potentially inappropriate prescribing in an Irish elderly population in primary care. Br J Clin Pharmacol. 2009;68(6):936–47.
Dunn RL, Harrison D, Ripley TL. The Beers criteria as an outpatient screening tool for potentially inappropriate medications. Consult Pharm. 2011;26(10):754–63.
Spiker EC, Emptage RE, Giannamore MR, et al. Potential adverse drug events in an indigent and homeless geriatric population. Ann Pharmacother. 2001;35(10):1166–72.
Gallagher P, Lang PO, Cherubini A, et al. Prevalence of potentially inappropriate prescribing in an acutely ill population of older patients admitted to six European hospitals. Eur J Clin Pharmacol. 2011;67(11):1175–88.
O’Connor MN, Gallagher P, O’Mahony D. Inappropriate prescribing: criteria, detection and prevention. Drugs Aging. 2012;29(6):437–52.
O’Sullivan DP, O’Mahony D, Parsons C, et al. A prevalence study of potentially inappropriate prescribing in Irish long-term care residents. Drugs Aging. 2013;30(1):39–49.
Lund BC, Carnahan RM, Egge JA, et al. Inappropriate prescribing predicts adverse drug events in older adults. Ann Pharmacother. 2010;44(6):957–63.
Chrischilles EA, VanGilder R, Wright K, et al. Inappropriate medication use as a risk factor for self-reported adverse drug. J Am Geriatr Soc. 2009;57(6):1000–6.
Passarelli MC, Jacob-Filho W, Figueras A. Adverse drug reactions in an elderly hospitalised population: inappropriate prescription is a leading cause. Drugs Aging. 2005;22(9):767–77.
Noblit GW, Hare RD. Meta-ethnography: synthesising qualitative studies. New York: Sage; 1988.
Campbell R, Pound P, Pope C, et al. Evaluating meta-ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care. Soc Sci Med. 2003;56(4):671–84.
Campbell R, Pound P, Morgan M, et al. Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess. 2011;15(43):1–164.
Atkins S, Lewin S, Smith H, et al. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol. 2008;16(8):21.
Malpass A, Shaw A, Sharp D, et al. “Medication career” or “moral career”? The two sides of managing antidepressants: a meta-ethnography of patients’ experience of antidepressants. Soc Sci Med. 2009;68(1):154–68.
Pound P, Britten N, Morgan M, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med. 2005;61(1):133–55.
Britten N, Campbell R, Pope C, et al. Using meta ethnography to synthesise qualitative research: a worked example. J Health Serv Res Policy. 2002;7(4):209–15.
Teixeira Rodrigues A, Roque F, Falcao A, et al. Understanding physician antibiotic prescribing behaviour: a systematic review of qualitative studies. Int J Antimicrob Agents. 2013;41(3):203–12.
Thorne S, Jensen L, Kearney MH, et al. Qualitative metasynthesis: reflections on methodological orientation and idealogical agenda. Qual Health Res. 2004;14(10):1342–65.
Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;27(12):181.
Dickinson R, Knapp P, House AO, et al. Long-term prescribing of antidepressants in the older population: a qualitative study. Br J Gen Pract. 2010;60(573):257–9.
Agarwal G, Nair K, Cosby J, et al. GPs’ approach to insulin prescribing in older patients: a qualitative study. Br J Gen Pract. 2008;58(553):569–75.
Spitz A, Moore AA, Papaleontiou M, et al. Primary care providers’ perspective on prescribing opioids to older adults with chronic non-cancer pain: a qualitative study. BMC Geriatr. 2011;14(11):35.
Cook JM, Marshall R, Masci C, et al. Physicians’ perspectives on prescribing benzodiazepines for older adults: a qualitative study. J Gen Intern Med. 2007;22(3):303–7.
Salzman C, The APA. Task Force report on benzodiazepine dependence, toxicity, and abuse. Am J Psychiatry. 1991;148(2):151–2.
Consensus conference. Drugs and insomnia: the use of medications to promote sleep. JAMA. 1984;251(18):2410–4.
Damestoy N, Collin J, Lalande R. Prescribing psychotropic medication for elderly patients: some physicians’ perspectives. CMAJ. 1999;161(2):143–5.
Wood-Mitchell A, James IA, Waterworth A, et al. Factors influencing the prescribing of medications by old age psychiatrists for behavioural and psychological symptoms of dementia: a qualitative study. Age Ageing. 2008;37(5):547–52.
Spinewine A, Swine C, Dhillon S, et al. Appropriateness of use of medicines in elderly inpatients: qualitative study. BMJ. 2005;331(7522):935–8.
Gordon M. Non-technical skills training to enhance patient safety. Clin Teach. 2013;10(3):170–5.
Acknowledgments
The authors would like to acknowledge the Health Research Board of Ireland for funding this research (Grant no. HRA_HSR/2010/14). The manuscript does not contain clinical studies or patient data.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cullinan, S., O’Mahony, D., Fleming, A. et al. A Meta-Synthesis of Potentially Inappropriate Prescribing in Older Patients. Drugs Aging 31, 631–638 (2014). https://doi.org/10.1007/s40266-014-0190-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-014-0190-4