Abstract
Duvelisib (Copiktra™) is a small-molecule inhibitor of phosphatidylinositol-3 kinase that has been developed as an oral treatment for various cancer indications. In September 2018, duvelisib received its first global approval in the USA for the treatment of adult patients with relapsed or refractory chronic lymphocytic leukaemia (CLL)/small lymphocytic lymphoma (SLL) after at least two prior therapies. Duvelisib was also granted accelerated approval in the USA for the treatment of adult patients with relapsed or refractory follicular lymphoma (FL) after at least two prior systemic therapies. Clinical development for various haematological malignancies is ongoing worldwide, as well as preclinical development for solid tumours in the USA. This article summarizes the milestones in the development of duvelisib leading to these first approvals for CLL/SLL and FL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Duvelisib (Copiktra™) is a first-in-class, small-molecule, selective dual inhibitor of the δ and γ isoforms of phosphatidylinositol-3 kinase (PI3K). It is being developed by Verastem Oncology (under license from Infinity Pharmaceuticals) as an oral treatment for various cancer indications. PI3K signalling is involved in the activation, proliferation and survival of B and T cells [1]. While the α and β isoforms of PI3K are widely expressed, the γ and δ isoforms are exclusively expressed in haematopoietic cells [2]. Duvelisib inhibits the PI3K-δ isoform, which is necessary for cell proliferation and survival, and the PI3K-γ isoform, which modulates cytokine signalling and pro-inflammatory responses from the tumour microenvironment [2].
Duvelisib received its first global approval on 24 September 2018, in the USA, for the treatment of adult patients with relapsed or refractory chronic lymphocytic leukaemia (CLL)/small lymphocytic lymphoma (SLL) after at least two prior therapies [3, 4]. The drug has also been granted accelerated approval in the USA for the treatment of adult patients with relapsed or refractory follicular lymphoma (FL) after at least two prior systemic therapies [3, 4]; continued approval for this indication may be contingent upon verification of clinical benefit in confirmatory trials [4]. The recommended dosage of duvelisib for all indications is 25 mg administered orally twice daily, with or without food [4].
Duvelisib is in phase III clinical development for relapsed or refractory CLL and FL worldwide, as well as phase I/II development as first-line therapy for FL. Phase I–III development is ongoing in various countries for the treatment of non-Hodgkin’s lymphoma (NHL) and T-cell lymphoma. Duvelisib is also undergoing preclinical development in the USA for the treatment of solid tumours.
1.1 Company Agreements
Duvelisib was originated by Intellikine (owned by Takeda). In July 2010, Infinity Pharmaceuticals obtained global development and commercialisation rights to Intellikine’s portfolio of PI3K inhibitors, including duvelisib [5]. This agreement with Millennium (Takeda Oncology Company and Takeda Pharmaceutical Company Limited) was amended in December 2012. Under the terms of the agreement, Infinity retained worldwide rights to duvelisib and any future PI3K-δ or -γ products, and Millennium remained entitled to receive milestone and royalty payments on future worldwide sales [6]. In March 2015, Infinity exercised its option to buy out all future royalty obligations due to Takeda in oncology indications, eliminating the future obligation to pay Takeda royalties based on global sales of duvelisib [7]. In November 2016, Infinity granted exclusive rights to Verastem (now Verastem Oncology) for the development and commercialisation of duvelisib worldwide. Under the terms of the agreement, Verastem will pay Infinity up to $US28 million in milestone payments, along with royalties on net sales [8].

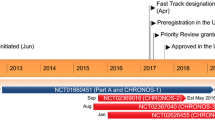
Key milestones in the development of duvelisib for the treatment of relapsed/refractory CLL/SLL and FL. CLL chronic lymphocytic leukaemia, FL follicular lymphoma, iNHL indolent non-Hodgkin’s lymphoma, NDA New Drug Application, SLL small lymphocytic lymphoma
In June 2018, Verastem Oncology and Yakult Honsha entered into an exclusive licensing agreement for the development and commercialisation of duvelisib for the treatment, prevention or diagnosis of all oncology indications in Japan [9]. Verastem Oncology signed an exclusive licensing agreement with CSPC Pharmaceutical Group in September 2018 for the development and commercialisation of duvelisib for all oncology indications in China [10].
1.2 Patent Information
Intellikine and Infinity Pharmaceuticals hold US patents covering duvelisib and related compounds which will expire between 2029 and 2032. The company also has pending patent applications worldwide relating to its PI3K programme which, if approved, are expected to expire between 2029 and 2036. Both the issued and pending patent applications have been licensed to Verastem.
2 Scientific Summary
2.1 Pharmacodynamics
Duvelisib inhibits PI3K-δ and -γ isoforms expressed in normal and malignant B cells [4]. It is 10 times more selective for PI3K-δ than for PI3K-γ (IC50 values 1028 and 96 nM) [2].
Duvelisib induces rapid inhibition of phosphorylated AKT (pAKT, a downstream marker of PI3K signalling) [11,12,13,14,15] and reduces serum levels of various chemokines and cytokines [11,12,13,14,15,16].

Chemical structure of duvelisib
In vitro, duvelisib potently killed 3 of 4 T-cell lymphoma lines with constitutive phosphorylation of AKT (pAKT, a downstream marker for PI3K inhibition) versus 0 of 7 cell lines lacking pAKT [11]. Consistent with these results, duvelisib induced apoptosis in B-cell receptor-mediated (and/or stromal co-cultured [13]) CLL lymphocytes, with minimal cytotoxicity against normal B cells [13, 14]. However, the drug was partially cytotoxic to normal T cells and natural killer cells [14]. Duvelisib induced approximately twofold more cell death than the PI3K-δ inhibitor idelalisib or the pan-PI3K inhibitor copanlisib [11].
In addition, duvelisib inhibited CLL cell chemotaxis toward the chemokine CXCL12 and reduced CLL cell migration beneath marrow stromal cells (pseudoemperipolesis) in vitro, suggesting that the drug interferes with the migrating and homing capabilities of CLL cells [13]. The activity of duvelisib was associated with mitigation of AKT, BAD, ERK and S6 activity downstream of the B-cell receptor signalling cascade [13].
In a patient-derived xenograft model of peripheral T-cell lymphoma, treatment with duvelisib shifted polarization of tumour-associated macrophages away from the tumour-promoting/immunosuppressive M2 phenotype toward the immune-stimulatory/pro-inflammatory M1 phenotype [11]. In patients, such a shift could promote an immunostimulatory environment that activates effector T cells [11].
2.2 Pharmacokinetics
Duvelisib is rapidly absorbed following a single oral dose [12]. A dose-proportional increase in plasma exposure is seen with duvelisib 8–75 mg twice daily (i.e. 0.3–3 times the recommended dosage) [4]. Following administration of duvelisib 25 mg twice daily, at steady-state, the geometric mean peak plasma concentration (Cmax) of duvelisib was 1.5 μg/mL and the area under the concentration-time curve (AUC) was 7.9 μg·h/mL; Cmax was reached in 1–2 h (Tmax). Duvelisib has an absolute bioavailability of 42% following administration of a single 25 mg dose. Duvelisib can be administered with or without food [4]. Administration of a single dose of duvelisib with a high-fat meal in volunteers delayed median Tmax from 1 to 3 h, but did not appreciably affect overall exposure [17].
The steady-state geometric mean apparent volume of distribution of duvelisib is 28.5 L, and the drug is 98% bound to plasma proteins [4]. The mean blood-to-plasma ratio is 0.5. Duvelisib metabolism is primarily mediated by CYP3A4. Following a single 25 mg dose of radiolabelled duvelisib, 79% of the radioactivity was excreted in the faeces (11% as unchanged drug) and 14% was excreted in the urine (< 1% as unchanged drug). The geometric mean terminal elimination half-life of duvelisib is 4.7 h. In patients with lymphoma or leukaemia, the steady-state geometric mean apparent systemic clearance is 4.2 L/h [4].
Age (18–90 years), sex, race, bodyweight (40–154 kg), renal impairment (creatinine clearance 23–80 mL/min) and hepatic impairment (Child Pugh class A, B and C) had no clinically meaningful effects on the pharmacokinetics of duvelisib [4].
Co-administration of duvelisib with strong CYP3A4 inducers (e.g. rifampicin) should be avoided since co-administration may decrease duvelisib exposure and efficacy [4]. Co-administration of duvelisib with strong CYP3A4 inhibitors (e.g. ketoconazole) may increase the risk of toxicity due to increased duvelisib exposure. Therefore, the dosage of duvelisib should be reduced to 15 mg twice daily when co-administered with a strong CYP3A4 inhibitor. Co-administration of duvelisib with sensitive CYP3A4 substrates (e.g. midazolam) may increase the exposure of the CYP3A4 sensitive drugs, resulting in an increased risk of toxicity with these drugs. Dose modification is recommended, and patients should be monitored for signs of toxicity. In vitro, duvelisib is a substrate of P-glycoprotein and BCRP. Duvelisib does not inhibit OAT1, OAT3, OCT1, OCT2, OATP1B1, OATP1B3, BCRP or P-glycoprotein [4].
2.3 Therapeutic Trials
2.3.1 Monotherapy
The efficacy of oral duvelisib monotherapy in patients with relapsed/refractory CLL/SLL was demonstrated in the randomized, open-label, multicentre, phase III DUO trial (NCT02004522) [18]. Patients were randomized to receive duvelisib monotherapy (n = 160) or ofatumumab monotherapy (n = 159). Patients in the duvelisib group received 25 mg twice daily in 28-day cycles except for the first cycle (21 days) to align with administration of ofatumumab infusions. Duvelisib was administered for up to 18 cycles, until disease progression or unacceptable toxicity. Ofatumumab was administered according to the approved product labelling (maximum of 12 doses within 7 cycles). Duvelisib significantly prolonged progression-free survival (PFS) versus ofatumumab as assessed by independent review committee (IRC) [13.3 vs. 9.9 months; hazard ratio (HR) 0.40; p < 0.0001; primary endpoint]. Similar results were seen for investigator-assessed PFS (17.6 vs. 9.7 months; HR 0.40; p < 0.0001). The estimated probability of being progression-free at 6 and 12 months was 78 and 60% with duvelisib versus 72 and 39% with ofatumumab. The beneficial effects of duvelisib on PFS were observed in multiple predefined CLL/SLL subgroups, including patients with high-risk cytogenetic markers. Duvelisib was also associated with a significantly higher overall response rate (ORR) versus ofatumumab (74 vs. 45%; p < 0.0001), particularly in the lymph node disease compartment (85 vs. 16%; p < 0.0001). Median overall survival (OS) was not reached in either treatment group; the 12-month probability of survival was 86% for both duvelisib and ofatumumab [18].
The US approval of duvelisib was based on a sub-analysis of patients from the overall DUO population with at least two prior lines of therapy (n = 196) [4]. In this sub-population, median PFS as assessed by IRC was 16.4 months with duvelisib versus 9.1 months with ofatumumab. The ORR as assessed by IRC was 78% in the duvelisib group compared with 39% in the ofatumumab group; all responses were partial responses [4].
In the DUO crossover extension study (NCT02049515), duvelisib monotherapy was associated with robust and durable responses in 89 CLL/SLL patients with progressive disease following ofatumumab treatment in the DUO trial [19]. All patients received duvelisib 25 mg twice daily until disease progression, death, intolerance or study withdrawal. The ORR was 73% on duvelisib compared with 28% on prior ofatumumab. Median PFS as assessed by IRC was 15 months on duvelisib compared with 9 months on prior ofatumumab [19].
The efficacy of oral duvelisib monotherapy in patients with relapsed/refractory indolent NHL was demonstrated in the single-arm, open-label, phase II DYNAMO trial (NCT01882803) [20]. All patients received duvelisib 25 mg twice daily in 28-day cycles until disease progression or unacceptable tolerability. The ORR as assessed by IRC was 46% (primary endpoint); all responses were partial responses. Across disease subtypes, the ORR was 41% in patients with FL (n = 83), 68% in patients with SLL (n = 28) and 33% in patients with marginal zone lymphoma (n = 18). Overall, the median time to response was 1.9 months and the median duration of response was 9.9 months. Median PFS was 8.4 months and the estimated probability of being progression-free at 6 months was 60%. Median OS was 18.4 months and the estimated probability of survival at 12 months was 74% [20].
Oral duvelisib monotherapy demonstrated clinical activity in an open-label, phase I trial in patients with relapsed/refractory advanced haematological malignancies (NCT01476657) [12]. In the dose-escalation phase (n = 31), patients received duvelisib 8–100 mg twice daily. In the expansion phase (n = 179), patients with indolent NHL, CLL or T-cell lymphoma received duvelisib 25 or 75 mg twice daily. Clinical responses were seen across a range of doses and disease subtypes, with investigator-assessed ORRs of 58% in patients with indolent NHL (n = 31), 56% in patients with CLL/SLL (n = 55), 50% in patients with peripheral T-cell lymphoma (n = 16) and 32% in patients with cutaneous T-cell lymphoma (n = 19). The median time to response was ≈ 1.8 months [12].
2.3.2 Combination Therapy
The efficacy of duvelisib in combination with fludarabine, cyclophosphamide and rituximab (FCR) as first-line therapy in younger patients (≤ 65 years) with CLL has been evaluated in a phase Ib/II trial (NCT02158091) [21]. Patients received duvelisib 25 mg once daily (n = 6) or 25 mg twice daily (n = 26), with the addition of FCR on day 8. Up to 6 cycles of FCR were administered, followed by maintenance therapy with duvelisib for up to 2 years. A total of 29/32 patients were evaluable for post-FCR response. The ORR was 97%; 28% of patients achieved a CR or CR with incomplete haematological recovery (CRi) and 69% achieved a partial response. The best rate of minimal residual disease negativity (MRD) negativity in the bone marrow was 81%. The rate of CR/CRi with MRD in the bone marrow (primary endpoint) was 28%. PFS and OS at 2 years were both 97% [21].
A phase I trial has investigated the efficacy of duvelisib in combination with bendamustine, rituximab or bendamustine plus rituximab in patients with relapsed/refractory lymphoma or CLL (NCT01871675) [22]. A total of 38/48 patients were evaluable for response, with an ORR of 74% [8% complete response (CR), 66% partial response, 16% stable disease and 10% progressive disease]. Median PFS was 13.7 months. Median OS was not reached, but the 15-month probability of survival was 82% [22].
2.4 Adverse Events
2.4.1 Monotherapy
Oral duvelisib monotherapy had a manageable tolerability profile in patients with relapsed/refractory CLL/SLL in the phase III DUO trial (NCT02004522) [18]. The most frequently reported haematological adverse events (AEs) were neutropenia (33% with duvelisib vs. 21% with ofatumumab), anaemia (23 vs. 10%) and thrombocytopenia (15 vs. 6%). The most common non-haematological AEs were diarrhoea (51%), pyrexia (29%), nausea (23%) and cough (21%) with duvelisib, and infusion-related reactions (19%), cough (14%), diarrhoea (12%), rash (12%) and fatigue (12%) with ofatumumab. Severe (grade ≥ 3) immune-related toxicities in the duvelisib group included colitis (12%), pneumonitis (3%), increased ALT (3%) and increased AST (3%); most of these were managed with dose interruptions and/or steroids. In both treatment groups, pneumonia was the most frequently reported serious AE (15% with duvelisib vs. 3% with ofatumumab). Four patients in the duvelisib group experienced fatal drug-related AEs, including pneumonia (n = 2), sepsis (n = 1) and general health deterioration (n = 1) [18]. In the DUO crossover extension study (NCT02049515), the safety profile of duvelisib was manageable and consistent with that observed in the DUO trial [19].
Duvelisib monotherapy had a generally acceptable tolerability profile in patients with relapsed/refractory indolent NHL in the phase II DYNAMO trial (NCT01882803) [20]. The most frequently reported AEs were neutropenia (28%), diarrhoea (15%) and thrombocytopenia (13%). Most AEs were mild or moderate in severity. Dose interruptions or reductions due to AEs occurred in 63% of patients, and 17% of patients discontinued treatment because of AEs. Four patients experienced fatal duvelisib-related AEs, including drug reaction with eosinophilia and systemic symptoms (DRESS), toxic epidermal necrolysis (TEN), suspected viral infection and septic shock [20].
The US prescribing information contains a boxed warning regarding the potential of duvelisib to cause fatal and/or serious toxicities: infections (including Pneumocystis jirovecii pneumonia), diarrhoea or colitis, cutaneous reactions (including DRESS and TEN) and pneumonitis [4]. Other AEs of special interest with duvelisib were hepatotoxicity and neutropenia. Local prescribing information should be consulted for details of the management of these disorders. Duvelisib has the potential to cause foetal harm if administered to a pregnant woman. Also, based on findings in animals, duvelisib may affect fertility in males [4].
2.4.2 Combination Therapy
The safety profile of duvelisib in combination with either obinutuzumab or rituximab in patients with previously untreated FL in the phase Ib/II CONTEMPO trial (NCT02391545) was in line with the safety profile of duvelisib as monotherapy [23]. No dose-limiting toxicities (DLTs) were observed with duvelisib plus rituximab. However, one duvelisib plus obinutuzumab recipient experienced a DLT (grade 3 elevated lipase) during the first cycle [23].
In another phase Ib/II trial, duvelisib demonstrated an acceptable safety profile when administered in combination with FCR as first-line therapy in patients with CLL (NCT02158091) [21]. The only DLT was grade 3 febrile neutropenia with duvelisib 25 mg once daily. The most frequently reported AEs were nausea (72%), thrombocytopenia (69%), neutropenia (56%), diarrhoea (47%), anaemia (34%), anorexia (34%) and vomiting (28%). Serious AEs included transaminitis (n = 9), febrile neutropenia (n = 7), pneumonia (n = 6), colitis (n = 2), pruritus (n = 1) and cytomegalovirus infection (n = 1) [21].
The tolerability profile of duvelisib in combination with bendamustine, rituximab or bendamustine plus rituximab in patients with relapsed/refractory lymphoma or CLL in a phase I trial (NCT01871675) was generally similar to that of duvelisib alone [22]. When duvelisib 75 mg twice daily was administered with rituximab 375 mg/m2 weekly for two 28-day cycles ± bendamustine 70 or 90 mg/m2 on days 1 and 2 of the first 6 cycles, no DLTs were observed. However, one patient who received duvelisib 50 mg twice daily plus bendamustine 120 mg/m2 on days 1 and 2 of the first 6 cycles developed DLTs (febrile neutropenia, neutropenia, thrombocytopenia and hepatotoxicity). Two patients in the duvelisib plus rituximab group experienced fatal AEs that were potentially related to treatment (cardiac arrest and pneumonia) [22].
2.5 Ongoing Clinical Trials
Several phase I and/or II trials evaluating the safety and/or efficacy of duvelisib, alone or in combination with other antineoplastics, are currently underway. These include:
-
The phase II PRIMO trial (NCT03372057) is evaluating the efficacy and safety of duvelisib monotherapy in up to 120 adult patients with relapsed/refractory peripheral T-cell lymphoma. The primary endpoint is ORR and the secondary endpoints include duration of response and PFS [24];
-
A phase II trial (NCT02711852) is evaluating the long-term safety and efficacy of duvelisib in 500 patients with haematological malignancies who have participated in a previous duvelisib trial;
-
A phase I/II trial (NCT03534323) is evaluating the efficacy of duvelisib in combination with venetoclax in 47 patients with relapsed/refractory CLL or SLL;
-
A phase I trial (NCT02783625) is evaluating the efficacy of duvelisib in combination with either romidepsin or bortezomib in 88 patients with relapsed/refractory T-cell lymphoma. The primary endpoint is the maximum tolerated dose and the secondary endpoint is ORR.
3 Current Status
Duvelisib received its first global approval on 24 September 2018 in the USA for the treatment of adult patients with relapsed or refractory CLL/SLL after at least two prior therapies. Duvelisib was also granted accelerated approval in the USA for the treatment of adult patients with relapsed or refractory FL after at least two prior systemic therapies.
References
Winkler DG, Faia KL, DiNitto JP, et al. PI3K-δ and PI3K-γ inhibition by IPI-145 abrogates immune responses and suppresses activity in autoimmune and inflammatory disease models. Chem Biol. 2013;20(11):1364–74.
Vangapandu HV, Jain N, Gandhi V. Duvelisib: a phosphoinositide-3 kinase delta/gamma inhibitor for chronic lymphocytic leukemia. Expert Opin Investig Drugs. 2017;26(5):625–32.
US FDA. Duvelisib (COPIKTRA, Verastem, Inc.) for adult patients with relapsed or refractory chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL); 2018. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm621503.htm. Accessed 10 Oct 2018.
Verastem Inc. Copiktra (duvelisib), capsules for oral use: US prescribing information; 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/211155s000lbl.pdf. Accessed 10 Oct 2018.
Infinity Pharmaceuticals Inc. Infinity and Intellikine enter agreement to develop oral therapies targeting PI3 kinase delta, gamma [media release]; 8 Jul 2010. http://globenewswire.com/news-release/2010/07/08/424597/195928/en/Infinity-and-Intellikine-Enter-Agreement-to-Develop-Oral-Therapies-Targeting-PI3-Kinase-Delta-Gamma.
Infinity Pharmaceuticals Inc. Infinity amends PI3K-delta, gamma agreement with Millennium [media release]; 24 Dec 2012. https://www.businesswire.com/news/home/20121224005109/en/Infinity-Amends-PI3K-DeltaGamma-Agreement-Millennium.
Infinity Pharmaceuticals. Infinity exercises option to buy out all future royalty obligations to Takeda for duvelisib sales in oncology [media release]; 31 Mar 2015. http://investors.infi.com/news-releases/news-release-details/infinity-exercises-option-buy-out-all-future-royalty-obligations.
Verastem. Verastem licenses duvelisib from Infinity Pharmaceuticals [media release]; 2 Nov 2016. http://investor.verastem.com/phoenix.zhtml?c=250749&p=irol-newsArticle&ID=2218384.
Verastem Oncology. Verastem Oncology and Yakult Honsha Co., Ltd. sign exclusive license agreement for the development and commercialization of duvelisib in Japan [media release]; 5 June 2018. http://investor.verastem.com/phoenix.zhtml?c=250749&p=irol-newsArticle&ID=2353165.
Verastem Inc. CSPC Pharmaceutical Group Limited and Verastem Oncology sign exclusive license agreement for the development and commercialization of COPIKTRA™ (duvelisib) in China [media release]; 25 Sep 2018. http://investor.verastem.com/phoenix.zhtml?c=250749&p=irol-newsArticle&ID=2368922.
Horwitz SM, Koch R, Porcu P, et al. Activity of the PI3K-δ, γ inhibitor duvelisib in a phase 1 trial and preclinical models of T-cell lymphoma. Blood. 2018;131(8):888–98.
Flinn IW, O’Brien S, Kahl B, et al. Duvelisib, a novel oral dual inhibitor of PI3K-δ, γ, is clinically active in advanced hematologic malignancies. Blood. 2018;131(8):877–87.
Balakrishnan K, Peluso M, Fu M, et al. The phosphoinositide-3-kinase (PI3K)-delta and gamma inhibitor, IPI-145 (duvelisib), overcomes signals from the PI3K/AKT/S6 pathway and promotes apoptosis in CLL. Leukemia. 2015;29(9):1811–22.
Dong S, Guinn D, Dubovsky JA, et al. IPI-145 antagonizes intrinsic and extrinsic survival signals in chronic lymphocytic leukemia cells. Blood. 2014;124(24):3583–6.
Pillinger G, Piddock R, Lawes M, et al. The PI3K gamma/delta inhibitor, IPI-145 (duvelisib) inhibits acute myeloid leukemia blast proliferation and adhesion [abstract no. E911]. Haematologica. 2015;100(Suppl 1):363.
Weaver DT, Sprott K, Pachter J, et al. Duvelisib inhibition of chemokines in patients with CLL (DUO study) and iNHL (DYNAMO study) [abstract no. 12048]. J Clin Oncol. 2018;36(Suppl 15).
Kharidia J, Van Iersel MP, Hartstra J, et al. The pharmacokinetics, pharmacodynamics, safety, tolerability and food effect of duvelisib, an oral, dual PI3K-δ and PI3K-γ inhibitor, in healthy human subjects [abstract no. 020]. Clin Pharmacol Drug Dev. 2016;5(Suppl 1):14–5.
Flinn IW, Hillmen P, Montillo M, et al. The phase 3 DUO trial: duvelisib versus ofatumumab in relapsed and refractory CLL/SLL. Blood. 2018. https://doi.org/10.1182/blood-2018-05-850461.
Kuss BJ, Davids MS, Hillmen P, et al. The efficacy of duvelisib monotherapy following disease progression on ofatumumab monotherapy in patients with relapsed/refractory CLL or SLL in the DUO crossover extension study [abstract no. 7533 plus poster]. J Clin Oncol. 2018;36(Suppl 15).
Flinn IW, Miller CB, Ardeshna KM, et al. DYNAMO: a phase 2 study demonstrating the clinical activity of duvelisib in patients with relapsed refractory indolent non-Hodgkin lymphoma [abstract no. 1218]. Blood 2016;128(22).
Davids M, Fisher D, Tyekucheva S, et al. A phase Ib/II study of duvelisib in combination with FCR (DFCR) for frontline therapy of younger CLL patients [abstract no. S807]. In: 23rd Congress of the European Haematology Association; 2018.
Flinn IW, Cherry M, Maris M, et al. Combination trial of duvelisib (IPI-145) with bendamustine, rituximab, or bendamustine/rituximab in patients with lymphoma or chronic lymphocytic leukemia [abstract no. 3928]. Blood. 2015;126(23).
Casulo C, Jacobsen E, Van Eygen K, et al. Preliminary safety, pharmacokinetics, and pharmacodynamics of duvelisib plus rituximab or obinutuzumab in patients with previously untreated CD20+ follicular lymphoma [abstract no. P319]. Haematologica. 2016;101((Suppl 1)):104.
Horwitz SM, Soto J, Youssoufian H. The PRIMO study: a phase 2 study of duvelisib efficacy and safety in patients with relapsed or refractory peripheral T-cell lymphoma (PTCL) [abstract no. TPS7590]. J Clin Oncol. 2018;36(Suppl 15).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflicts of interest
During the peer review process the manufacturer of duvelisib was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the author on the basis of scientific completeness and accuracy. Hannah Blair is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies to market launch and beyond.
Rights and permissions
About this article
Cite this article
Blair, H.A. Duvelisib: First Global Approval. Drugs 78, 1847–1853 (2018). https://doi.org/10.1007/s40265-018-1013-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-018-1013-4