Abstract
Abiraterone acetate (Zytiga®) is an orally administered, selective inhibitor of the 17α-hydroxylase and C17,20-lyase enzymatic activities of cytochrome P450 (CYP) 17. CYP17 is required for androgen biosynthesis, with androgen receptor signalling crucial in the progression from primary to metastatic prostate cancer. Abiraterone acetate is approved in the European Union and the US, in combination with prednisone or prednisolone, for the treatment of men with metastatic castration-resistant prostate cancer (CRPC). When administered in combination with prednisone in a placebo-controlled, multinational phase III study, abiraterone acetate significantly prolonged overall survival and radiographic progression-free survival (rPFS) in men with metastatic CRPC who had previously received docetaxel. In men with metastatic CRPC who had not previously received chemotherapy participating in a placebo-controlled, multinational phase III study, there was a strong trend towards an overall survival benefit, a significant prolongation in rPFS and significant delays in clinical decline, the need for chemotherapy and the onset of pain observed. Given the nature of the therapy, the overall tolerability profile of abiraterone acetate, in combination with prednisone, was acceptable in men with metastatic CRPC. Abiraterone acetate is associated with hypokalaemia, hypertension, and fluid retention or oedema, secondary to its mechanism of action, and with cardiac adverse events and hepatotoxicity; however, in the phase III studies the incidences of the most frequently reported grade 3 or 4 adverse events of special interest were relatively low. Although the final overall survival data in men with metastatic CRPC who have not previously received chemotherapy are awaited, current evidence indicates that abiraterone acetate is a useful option for the treatment of metastatic CRPC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Converted to the active metabolite abiraterone following oral administration |
Selective inhibitor of the 17α-hydroxylase and C17,20-lyase enzymatic activities of cytochrome P450 17 |
Demonstrates a strong trend towards an overall survival benefit and prolongs radiographic progression-free survival (rPFS) in men with metastatic CRPC who have not previously received chemotherapy |
Prolongs overall survival and rPFS in men with metastatic CRPC who have previously received docetaxel |
Given the nature of the therapy, the overall tolerability profile was acceptable |
Associated in some patients with hypokalaemia, hypertension, and fluid retention or oedema, secondary to its mechanism of action, and with cardiac adverse events and hepatotoxicity |
1 Introduction
Androgen receptor signalling is crucial not only to the development of the normal prostate but also in the progression from primary to metastatic prostate cancer and, thus, represents a cogent therapeutic target [1, 2]. Although advanced prostate cancers are initially sensitive to androgen deprivation therapy (medical [e.g. luteinizing hormone-releasing hormone (LHRH) agonist or antagonist therapy] or surgical [bilateral orchiectomy] castration), disease progression despite androgen deprivation therapy (i.e. castration-resistant prostate cancer [CRPC]) eventually occurs [2–5].
A hallmark of CRPC is its continued reliance on androgen receptor signalling for tumour cell survival [1]. Evidence suggests that there are several mechanisms by which androgen receptor activation and prostate cancer growth are achieved despite the presence of low circulating testicular androgen levels, including extragonadal (adrenal and intratumoural) androgen production via upregulation of cytochrome P450 (CYP) 17 [6, 7].
More complete androgen suppression leading to desirable clinical outcomes in patients with CRPC was first observed with ketoconazole, a weak and nonspecific CYP17 inhibitor [6, 7]. However, ketoconazole induced only modest antitumour activity in a phase III study, with disease progression associated with significant elevations in androstenedione and dehydroepiandrosterone (DHEA), indicating incomplete target blockade [8, 9]. Moreover, ketoconazole’s lack of specificity resulted in the inhibition of 11β-hydroxylation and cholesterol side chain cleavage to pregnenolone and, thus, adrenal insufficiency, gastrointestinal toxicity and hepatotoxicity [7]. Abiraterone acetate was therefore developed as a selective, irreversible inhibitor of CYP17 [7] and has been shown to be both more potent and selective than ketoconazole [10].
This article reviews pharmacological, therapeutic efficacy and tolerability data relevant to the utilization of oral abiraterone acetate (Zytiga®) in the treatment of patients with metastatic CRPC.
2 Pharmacodynamic Properties
The pharmacodynamic properties of oral abiraterone acetate are well established and have been reviewed previously [11]; therefore, a brief overview is presented in this section.
Abiraterone, the active metabolite of abiraterone acetate (Sect. 3), is a selective inhibitor of CYP17 (17α-hydroxylase and C17,20-lyase), which is required for androgen biosynthesis [12, 13]. Specifically, pregnenolone and progesterone are converted to their 17α-hydroxy derivatives (by 17α-hydroxylase) and subsequently to DHEA and androstenedione (by C17,20-lyase); DHEA and androstenedione are androgens and testosterone precursors [12, 13] (Fig. 1). CYP17 is expressed in adrenal, prostatic and testicular tumour tissues [12, 13]; ex vivo, the expression of CYP17A was 16.9-fold higher (p = 0.0005) in CRPC metastases than in primary prostate tumours [14]. Preliminary data suggest that abiraterone also inhibits 3β-hydroxysteroid dehydrogenase/isomerase, which is required for 5α-dihydrotestosterone (DHT) synthesis [15].
Selected components of the androgen synthesis pathway. Adapted from Yang [11] with permission. aEnzymes inhibited by abiraterone acetate. ACTH adrenocorticotrophic hormone, DHEA dehydroepiandrosterone, DHT 5α-dihydrotestosterone
Both abiraterone and abiraterone acetate inhibit 17α-hydroxylase and C17,20-lyase activity to a greater extent than ketoconazole [11, 16]. In a study in patients with untreated prostate cancer, the half-maximal inhibitory concentrations of abiraterone against 17α-hydroxylase and C17,20-lyase were 4 and 2.9 nmol/L; the corresponding values were 18 and 17 nmol/L for abiraterone acetate and 65 and 26 for ketoconazole. The apparent inhibition constant for abiraterone was <1 nmol/L [11, 16].
Inhibition of 17α-hydroxylase reduces cortisol levels and elevates adrenocorticotrophic hormone (ACTH) levels (secondary to positive feedback mechanisms) [2, 11, 17–19] (Fig. 1). This, in turn, raises deoxycorticosterone and corticosterone levels, leading to secondary mineralocorticoid excess characterized by hypokalaemia, hypertension and fluid retention or oedema [17, 18]. In two phase I studies in patients with progressive CRPC who had not previously received chemotherapy, therapy with abiraterone acetate 250–2,000 mg once daily was associated with elevated ACTH, deoxycorticosterone and/or corticosterone levels and with mineralocorticoid-related adverse events [19, 20].
Inhibition of C17,20-lyase reduces DHEA, androstenedione and testosterone levels [18]. Abiraterone acetate suppressed serum testosterone levels to undetectable or near undetectable levels after 8 [19] or 28 [20] days’ therapy in patients with progressive CRPC, and, in combination with oral prednisone, suppressed blood and bone marrow aspirate testosterone levels to less than pg/mL levels in patients with metastatic CRPC, with this suppression sustained at progression [21]. Levels of other components of the androgen synthesis pathway, including DHEA and/or androstenedione were also reduced following therapy with abiraterone acetate [19, 20].
To address the imbalance of glucocorticoid and mineralocorticoid levels resulting from 17α-hydroxylase and C17,20-lyase inhibition, abiraterone acetate was administered concomitantly with a glucocorticoid (e.g. dexamethasone or prednisone) or a mineralocorticoid receptor agonist (e.g. eplerenone) to suppress the ACTH drive [12] in phase I [19, 20] and II [9, 22, 23] studies. All of the patients in the two multinational phase III studies [24–26] discussed in Sect. 5 received concomitant prednisone; the incidence of mineralocorticoid-related adverse events in these studies is presented in Sect. 6.2.
Testosterone and its 5α-reduced derivative DHT are the major physiological ligands that activate the androgen receptor [6, 27]. However, alternative activation pathways of the androgen receptor may confer resistance to prostate cancer therapy, including that with abiraterone acetate [28]. For instance, mutations of the androgen receptor may enable activation by other ligands (e.g. deoxycorticosterone, corticosterone), or may lead to constitutive (i.e. ligand-independent) activation [28]; in vivo, therapy with abiraterone acetate was associated with increased expression of the androgen receptor and CYP17A1 [29, 30]. Of note, limited in vitro data (available as an abstract) suggests the potential for cross resistance between the taxanes docetaxel and cabazitaxel and the novel agents abiraterone acetate and enzalutamide (MDV3100), with androgen receptor nuclear translation in Hep3B cells inhibited by 21, 34, 58 and 100 %, respectively, compared with the control (mitoxantrone) [31].
In phase I and II studies in patients with prostate cancer, therapy with abiraterone acetate 250–2,000 mg once daily demonstrated reductions in prostate-specific antigen (PSA) levels (a biomarker in patients with prostate cancer [12]) [9, 19, 20, 22, 23, 32] and/or circulating tumour cell (CTC) counts [9, 22, 23].
The QT/corrected QT interval does not appear to be affected by therapeutic dosages of oral abiraterone acetate plus prednisone in patients with metastatic CRPC [33].
3 Pharmacokinetic Properties
The pharmacokinetic properties of oral abiraterone acetate have been discussed in detail previously [11]; this section provides a brief summary.
Following oral administration, abiraterone acetate is hydrolysed to the active metabolite abiraterone, with the process believed to be mediated by unidentified esterase(s) rather than CYP enzymes [12, 13]. In clinical studies, plasma abiraterone acetate concentrations were below detectable levels (i.e. <0.2 ng/mL) in >99 % of the analysed samples [13].
In patients with metastatic CRPC, the maximum plasma concentration (Cmax) of abiraterone was reached in a median time of approximately 2 h following the oral administration of abiraterone acetate [12, 13]. Mean steady-state area under the concentration-time curve (AUC) and Cmax values for abiraterone were 1173 ng · h/mL and 226 ng/mL in patients who received abiraterone acetate 1,000 mg once daily [13]. Of note, accumulation of the drug at steady state has been observed, with an AUC value that is 2-fold higher than after a single dose of abiraterone acetate 1,000 mg [13].
The systemic exposure of abiraterone is elevated to a highly variable extent when abiraterone acetate is administered with food [12, 13]. AUC from time zero to infinity (AUC∞) and Cmax values were elevated by approximately 5- and 7-fold with a low-fat meal and by approximately 10- and 17-fold with a high fat meal. Therefore, abiraterone acetate should not be administered with food (see Sect. 7) [12, 13].
The apparent volume of distribution of abiraterone of approximately 5,630 L indicates extensive distribution to the peripheral tissues [12]; the mean apparent steady-state volume of distribution is 19,669 L [13]. Abiraterone is highly bound (>99 %) to the human plasma proteins albumin and α-1 acid glycoprotein [12, 13]. Of note, it is not yet known whether abiraterone acetate or its metabolites are distributed to semen [13].
The biotransformation of abiraterone predominately occurs in the liver and involves hydroxylation, oxidation and sulphation [12]. The two major circulating metabolites in the plasma (abiraterone sulphate and N-oxide abiraterone sulphate) are both inactive and each account for approximately 43 % of exposure [12, 13]. The formation of abiraterone sulphate and N-oxide abiraterone sulphate is mediated by sulfotransferase, and CYP3A4 and sulfotransferase, respectively [13].
The mean plasma terminal elimination half-life of abiraterone in patients with metastatic CRPC is 12 h [13]. The elimination of orally administered abiraterone acetate 1,000 mg occurs primarily via the faeces (88 and 5 % of a 14C-labelled dose was recovered via the faeces and urine), with unchanged abiraterone acetate (~55 % of the administered dose) and abiraterone (~22 %) the major compounds present in the faeces [12, 13].
3.1 Special Populations
Mild (Child–Pugh class A) hepatic impairment had minimal effects on the pharmacokinetics of abiraterone [34], thus, dosage adjustment is not required in these patients [12, 13]. Mean abiraterone Cmax, AUClast and AUC∞ values were elevated approximately 3.5-, 4.8- and 4.7-fold in patients with moderate (Child–Pugh class B; n = 8) hepatic impairment versus subjects with normal hepatic function (n = 8); the mean half-life of abiraterone was prolonged to approximately 19 h in patients with moderate hepatic impairment [34]. Therefore, caution is advised in patients with moderate hepatic impairment [12, 13], with the US prescribing information recommending a dosage reduction to 250 mg once daily for this patient population and treatment discontinuation in patients with alanine aminotransferase (ALT) and/or aspartate aminotransferase (AST) levels >5 × the upper limit of normal (ULN) or total bilirubin levels >3 × ULN [13]. Data are lacking in patients with severe hepatic impairment; therefore, the utilization of abiraterone acetate in this patient population is contraindicated in the EU [12] and not recommended in the US [13].
The systemic exposure (based on geometric mean Cmax, AUClast and AUC∞ values) of abiraterone was not elevated with a single dose of abiraterone acetate 1,000 mg in patients with end-stage renal disease requiring haemodialysis (data currently available as an abstract) [35]. Therefore, dosage adjustments are not required in patients with renal impairment [12, 13], although in the EU caution is advised in patients with severe renal impairment, owing to the lack of clinical data [12].
4 Potential Drug Interactions
Data from in vitro studies in human liver microsomes have shown that, as well as inhibiting CYP17, abiraterone is a strong inhibitor of CYP1A2, CYP2D6 and CYP2C8, and a moderate inhibitor of CYP2C9, CYP2C19 and CYP3A4/5 [13]. However, the pharmacokinetics of theophylline (a CYP1A2 substrate) were not altered when coadministered as a single 100 mg dose with abiraterone acetate 1,000 mg once daily plus oral prednisone 5 mg twice daily in patients with metastatic CRPC who had failed at least one line of chemotherapy (n = 16) [36].
The concurrent administration of abiraterone acetate 1,000 mg once daily plus prednisone 5 mg twice daily and a single dose of dextromethorphan 30 mg (a CYP2D6 substrate) to patients with metastatic CRPC who had failed gonadotropin-releasing hormone therapy and at least one line of chemotherapy approximately doubled mean dextromethorphan Cmax, AUC from time zero to 24 h (AUC24), AUClast and AUC∞ values and elevated mean AUC24, AUClast and AUC∞ values for dextrorphan, the active metabolite of dextromethorphan, by approximately 33 % [36]. Therefore, the coadministration of abiraterone acetate with CYP2D6 substrates that have a narrow therapeutic index (e.g. thioridazine) should be utilized with caution (with a dose reduction of the CYP2D6 substrate considered) [12, 13] or avoided [13].
The pretreatment of healthy volunteers with rifampicin (rifampin) 600 mg/day (a strong CYP3A4 inducer) for 6 days followed by the administration of a single dose of abiraterone acetate 1,000 mg resulted in a 55 % reduction in the mean plasma AUC∞ of abiraterone [12, 13]. Therefore, strong inducers of CYP3A4 (e.g. carbamazepine, phenobarbital and rifampicin) should be avoided unless there is no therapeutic alternative in patients receiving abiraterone acetate [12, 13]. The US prescribing information [13] indicates that if a strong CYP3A4 inducer must be coadministered with abiraterone acetate, the abiraterone acetate dosage must be adjusted during the coadministration period (see the US prescribing information for further details). In healthy volunteers, concurrent therapy with abiraterone acetate and ketoconazole (a strong CYP3A4 inhibitor) had no clinically relevant effect on the pharmacokinetics of abiraterone [12, 13].
At clinically relevant concentrations, neither abiraterone acetate nor abiraterone were substrates of p-glycoprotein (p-gp) in vitro, although abiraterone acetate inhibits p-gp [13].
5 Therapeutic Efficacy
The efficacy of oral abiraterone acetate in combination with oral prednisone has been assessed in the treatment of men with metastatic CRPC who have not previously received chemotherapy (Sect. 5.1) or who have previously received docetaxel (Sect. 5.2). Data are from fully published studies [24–26, 37–39] and abstracts [40–43], with supplementary data from the European Medicines Agency (EMA) assessment report [44], the EU summary of product characteristics (SPC) [12] and the US prescribing information [13]. In both studies, patients received oral abiraterone acetate 1,000 mg (administered as four 250 mg tablets) or placebo once daily in combination with oral prednisone 5 mg twice daily [24–26].
Almost three-quarters (73 %) of patients in the studies discussed in this section were aged ≥65 years and 30 % were aged ≥75 years [13]. No overall differences in terms of efficacy were observed between elderly and younger patients.
5.1 In Men Who Have Not Previously Received Chemotherapy
A randomized, double-blind, placebo-controlled, multinational, phase III study assessed the efficacy of abiraterone acetate in combination with prednisone in the treatment of men with metastatic CRPC who have not previously received chemotherapy [24].
Key design details for this study are summarized in Table 1. At baseline, patient demographic and disease characteristics were well balanced between the abiraterone acetate plus prednisone and placebo plus prednisone groups [24]. Overall, 76 and 24 % of patients had an Eastern Cooperative Oncology Group (ECOG) performance status score of 0 or 1 [12]. Patients were stratified by ECOG performance status score at baseline [24].
Overall survival (co-primary efficacy endpoint; investigator review) was assessed at three prespecified interim analyses conducted after 209, 333 and 434 deaths, respectively (corresponding to 27, 43 and 56 % of the prespecified total of 773 overall survival events) [13, 24, 40, 44]. The final overall survival analysis will be performed after 773 overall survival events [24].
Radiographic progression-free survival (rPFS; co-primary efficacy endpoint) was assessed at the first interim analysis conducted after 401 progression-free events (blinded independent radiological review) and at the second and third interim analyses (investigator review) [13, 24, 40, 44]. The median duration of follow-up was 22.2 months at the time of the second interim analysis [24] and 27.1 months at the time of the third interim analysis [40]. The study was unblinded after the second interim analysis on the recommendation of the data and safety monitoring committee, and placebo plus prednisone recipients were switched to abiraterone acetate plus prednisone therapy [24]. Analyses were conducted in the intent-to-treat population [24].
5.1.1 Radiographic Progression-Free Survival and Overall Survival
Combination therapy with abiraterone acetate plus prednisone significantly prolonged median rPFS relative to placebo plus prednisone at the first interim analysis in men with metastatic CRPC who have not previously received chemotherapy, reflecting a 57 % reduction in the risk of disease progression or death (Table 2) [24]. At this time, 27.5 % of abiraterone acetate plus prednisone recipients and 46.3 % of placebo plus prednisone recipients had radiographic evidence of progression or had died [12]. Median rPFS was also prolonged to a significantly greater extent with abiraterone acetate plus prednisone than placebo plus prednisone at the time of the second and third interim analyses (Table 2). At the time of the second interim analysis, 49.6 % of abiraterone acetate plus prednisone recipients and 62.0 % placebo plus prednisone recipients had radiographic evidence of progression or had died [12]. In addition, hazard ratios (HRs) significantly favoured abiraterone acetate plus prednisone over placebo plus prednisone across all patient subgroups in terms of rPFS. Of note, rPFS was positively correlated with overall survival, with an estimated correlation coefficient of 0.72 [24].
At the time of the first interim analysis, the median overall survival duration in either treatment group had not yet been reached (Table 2) [44]. At the time of the second and third interim analyses, the reduction in the risk of death associated with abiraterone acetate plus prednisone relative to placebo plus prednisone was not statistically significant (Table 2) [13, 24, 40, 44]. At the time of the respective analyses, 26.9 and 36.6 % of abiraterone acetate plus prednisone recipients and 34.3 and 43.2 % of placebo plus prednisone recipients had died [24, 44].
5.1.2 Secondary and Exploratory Endpoint Analyses
Compared with placebo plus prednisone, combination therapy with abiraterone acetate plus prednisone demonstrated significant advantages in terms of the secondary endpoints, with risk reductions ranging from 17 to 51 %, at the second [24] and third [40] interim analyses (Table 2).
Among the exploratory endpoints (see Table 1 for definitions) evaluated at the second interim assessment, the proportion of patients with a reduction of ≥50 % in the PSA level (relative risk [RR] 2.59 [95 % CI 2.19–3.05]; p < 0.001) and the proportion of patients with an objective response (RR 2.27 [95 % CI 1.59–3.25]; p < 0.001) also significantly favoured abiraterone acetate plus prednisone over placebo plus prednisone [24]. Abiraterone acetate plus prednisone also demonstrated significant advantages over placebo plus prednisone in terms of the median time to an increase in pain (HR 0.82 [95 % CI 0.67–1.00]; p = 0.049) at the second interim analysis and in the median time to a decline in functional status at the second (HR 0.78 [95 % CI 0.66–0.92]; p = 0.003) [24] and third (HR 0.79 [95 % CI 0.67–0.93]; p = 0.005) [41] interim analyses.
5.2 In Men Who Have Previously Received Docetaxel
The therapeutic efficacy of oral abiraterone acetate, in combination with oral prednisone, in men with metastatic CRPC who have previously received docetaxel has been evaluated in a randomized, double-blind, placebo-controlled, multinational, phase III study [25, 26].
Key design details for this study are summarized in Table 3. At baseline, patient demographic and disease characteristics were well balanced between the two treatment groups [25]. The majority (89 %) of patients had an ECOG performance status score of 0 or 1, with 67 % demonstrating radiographic evidence of disease progression. Prior to randomization, 70 and 30 % of patients had received one or two previous cytotoxic chemotherapy regimens [25].
Patients were stratified by ECOG performance status score at baseline, level of worst pain over the previous 24 h as assessed by the Brief Pain Inventory-Short Form (BPI-SF), number of previous chemotherapy regimens and the type of evidence of disease progression (elevation in PSA level only vs. radiographic evidence of progression with or without an elevation in the level of PSA) [25]. The median duration of treatment was 7.4 months in the abiraterone acetate plus prednisone group and 3.6 months in the placebo plus prednisone group [26]. Almost 50 % of patients continued or received (after a new skeletal-related event) concomitant bisphosphonates during the study [37].
The results presented are from the prespecified interim analysis conducted after 552 death events (median duration of follow-up of 12.8 months) [25] and from the prespecified final analysis conducted after 775 death events (97 % of the prespecified total of 797 death events) [median duration of follow-up of 20.2 months] [26]. The study was unblinded following analysis of the interim data, with placebo recipients switched to abiraterone acetate therapy if eligible [25]. The data reported are from the study period prior to the switch in therapy [26]. Analyses were conducted in the intent-to-treat population [25, 26].
5.2.1 Primary Endpoint Analyses
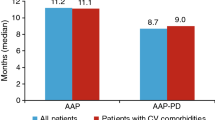
Combination therapy with abiraterone acetate plus prednisone was effective in the treatment of men with metastatic CRPC who have previously received docetaxel, with a significantly longer median overall survival (primary endpoint) in patients receiving abiraterone acetate plus prednisone than in those receiving placebo plus prednisone at both the interim [25] and final [26] analyses (Table 4). Of interest, in the final analysis, unfavourable and favourable CTC counts (i.e. ≥5 and <5) were predictive of overall survival from 4 weeks’ post-treatment, with the inclusion of CTC conversion significantly reducing the treatment effect at all time points [42]. At the time of the interim analysis, 41.8 % of abiraterone acetate plus prednisone recipients and 55.0 % of placebo plus prednisone recipients had died [25]; at the time of the final analysis, 62.9 and 68.8 % of patients had died [12].
At the final analysis, the survival benefit with abiraterone acetate plus prednisone versus placebo plus prednisone appeared to be independent of previous treatment with docetaxel, with a significantly (p < 0.05) longer median overall survival in the abiraterone acetate plus prednisone group, irrespective of the timing of docetaxel administration and the reason for the discontinuation of docetaxel [26].
According to a multivariate analysis, the effect of abiraterone acetate plus prednisone on overall survival was maintained following adjustment for stratification factors at the interim (HR 0.66 [95 % CI 0.55–0.78]; p < 0.001) [25] and final (HR 0.76 [95 % CI 0.66–0.88]; p = 0.0003) [26] analyses.
Visceral metastases are considered to be a poor prognostic factor in men with metastatic CRPC [43]. In an exploratory subgroup analysis evaluated at the time of the final analysis [43], median overall survival following therapy with abiraterone acetate plus prednisone or placebo plus prednisone was 12.9 and 8.3 months among men with visceral disease (n = 352) and 17.1 and 12.3 months among men without visceral disease (n = 843) [p < 0.0001].
5.2.2 Secondary and Other Endpoint Analyses
Abiraterone acetate plus prednisone was significantly more effective than placebo plus prednisone in prolonging median time to PSA progression, median rPFS and the proportion of patients achieving a PSA response at the interim [25] and final [26] analyses (Table 4). A significant between-group difference in favour of abiraterone acetate plus prednisone over placebo plus prednisone was also observed in the objective response rate at both timepoints (14.0 vs. 2.8 % of patients, p < 0.001 [25]; 14.8 vs. 3.3 %, p < 0.0001 [26]).
Therapy with abiraterone acetate plus prednisone was associated with significant benefits over placebo plus prednisone in terms of bone-related symptoms (patient-reported pain palliation and skeletal-related events) [12, 25, 37]. In patients with clinically significant pain at baseline, patient-reported pain intensity palliation (as assessed by the BPI-SF) was achieved in a significantly (p ≤ 0.0005) higher proportion of abiraterone acetate plus prednisone than placebo plus prednisone recipients at the time of the interim (44 vs. 27 % [patient numbers not reported]) [12, 25] and final (45 % [157 of 349 patients] vs. 29 % [47 of 163]) [37] analyses. Moreover, at the time of the final analysis, the median time to pain intensity palliation significantly favoured abiraterone acetate plus prednisone over placebo plus prednisone (5.6 vs. 13.7 months; p = 0.0018) [37]. A significantly longer median duration of pain intensity palliation was observed with abiraterone acetate plus prednisone than with placebo plus prednisone (4.2 vs. 2.1 months; p = 0.0056) [37].
An exploratory analysis suggested that abiraterone acetate plus prednisone delayed the development of skeletal-related events, with a significantly longer median time to the first skeletal-related event observed following therapy with abiraterone acetate plus prednisone than with placebo plus prednisone (25.0 vs. 20.3 p = 0.0001) [37]. Likewise, abiraterone acetate plus prednisone was associated with significant (p < 0.05) improvements in patient-reported fatigue [38] and patient-reported functional status [39].
6 Tolerability
Discussion in this section focuses on tolerability data derived from the multinational studies discussed in Sect. 5 [24–26, 40] and integrated data from the multinational studies reported in the EMA assessment report [44], the EU SPC [12] and the US prescribing information [13]. Unless otherwise stated, the median duration of follow-up in men with metastatic CRPC who had not previously received chemotherapy [24] or who have previously received docetaxel [26] was 22.2 and 20.2 months, respectively.
6.1 General Profile
Given the nature of the therapy, the tolerability profile of abiraterone acetate plus prednisone in men with metastatic CRPC was acceptable. The most frequently reported treatment-emergent adverse events (all grades) with abiraterone acetate plus prednisone in men with metastatic CRPC who have not previously received chemotherapy [24] were fatigue (39 % of patients), back pain (32 %) and arthralgia (28 %). Those occurring in men with metastatic CRPC who have previously received docetaxel were fatigue (47 % of patients), back pain (33 %) and nausea (33 %) [26]. The overall tolerability profile of abiraterone acetate in elderly patients appears to be consistent with that in younger patients [13].
Very common (≥1/10) adverse reactions following therapy with abiraterone acetate plus prednisone were hypertension, hypokalaemia, and fluid retention or oedema (see Sect. 6.2) and diarrhoea and urinary tract infection [12]. Serious treatment-emergent adverse events were reported in approximately one-third of patients in both the abiraterone acetate plus prednisone and placebo plus prednisone groups, with infections and infestations (8.9 and 5.7 % of patients) the most frequently reported serious adverse event category [44]. Serious treatment-related adverse events were experienced by approximately 10 % of patients in either treatment group [44]. Adrenal insufficiency occurred in one placebo plus prednisone recipient and no abiraterone acetate plus prednisone recipients [44]. Treatment-related adverse events led to treatment discontinuation in 5.4 % of patients in each treatment group [44].
Grade 3 or 4 treatment-emergent adverse events were reported in 55.2 % of patients receiving abiraterone acetate plus prednisone and 49.8 % of those receiving placebo plus prednisone, with anaemia, arthralgia, back pain, bone pain and fatigue the most frequent [44]. Grade 3 or 4 treatment-related adverse events were experienced by 22.8 and 17.9 % of patients receiving abiraterone acetate plus prednisone or placebo plus prednisone [44]. Treatment-related adverse events leading to death occurred in 1.0 % of abiraterone acetate plus prednisone recipients and 1.6 % of placebo plus prednisone recipients [44].
At the time of the third interim analysis in the study in men with metastatic CRPC who have not previously received chemotherapy, there were no clinically relevant increases in the incidence of various adverse events following therapy with abiraterone acetate plus prednisone compared with placebo plus prednisone (data currently available as an abstract) [45]. Treatment discontinuation because of treatment-emergent adverse events occurred in 8 and 6 % of patients in the respective treatment groups [45].
6.2 Adverse Events of Special Interest
Adverse events associated with abiraterone acetate therapy and considered of special interest include cardiac adverse events, hepatotoxicity (liver function test abnormalities), hypokalaemia, hypertension, and fluid retention or oedema [44]. Hypertension, hypokalaemia, and fluid retention or oedema appear to be related to the mechanism of action of abiraterone acetate, which promotes elevated mineralocorticoid levels as a result of CYP17 inhibition (see Sect. 2).
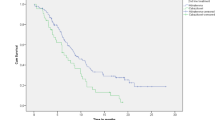
In general, the adverse events of special interest observed following therapy with abiraterone acetate plus prednisone in the two multinational studies discussed in Sect. 5 were consistent with the known tolerability profile of the agent [44]. The most frequently reported adverse events of special interest (all grades) in the multinational studies are reported in Fig. 2.
Tolerability profile of oral abiraterone acetate in combination with oral prednisone in men with metastatic castration-resistant prostate cancer (CRPC). Incidence of adverse events of special interest (grades 1–4) in two randomized, double-blind, placebo-controlled, multinational, phase III studies in men with metastatic CRPC who a have not previously received chemotherapy [24] or b have previously received docetaxel [26]. Limited supplementary data were procured from the European Medicines Agency assessment report [44]. ABI abiraterone acetate, ALT alanine aminotransferase, AST aspartate aminotransferase, PL placebo, PRE prednisone, pts patients
The most frequently reported grade 3 or 4 adverse events of special interest following combination therapy with abiraterone acetate plus prednisone or placebo plus prednisone in men with metastatic CRPC who have not previously received chemotherapy [24] were cardiac adverse events (6 vs. 3 % of patients), an elevation in the level of ALT [5 vs. <1 %] and hypertension (4 vs. 3 %). Among men with metastatic CRPC who have previously received docetaxel, grade 4 adverse events of special interest occurred in ≤1 % of patients in each treatment group [26].
An integrated analysis [12] showed that the cardiovascular adverse events following therapy with abiraterone acetate plus prednisone or placebo plus prednisone were hypertension (14.5 vs. 10.5 % of patients), atrial fibrillation (3.4 vs. 3.4 %), tachycardia (2.8 vs. 1.7 %), angina pectoris (1.9 vs. 0.9 %), cardiac failure (1.9 vs. 0.6 %) and arrhythmia (1.1 vs. 0.4 %). Among men with metastatic CRPC who have not previously received chemotherapy [44], serious cardiac adverse events were observed in 7 % of abiraterone acetate plus prednisone recipients and 3 % of placebo plus prednisone recipients, with <1.0 % of patients in both groups discontinuing therapy because of cardiac adverse events. Grade 3 or 4 treatment-emergent adverse events classified in the system order class of cardiac disorders occurred in 4 and 2 % of patients in the respective treatment groups [44]. Among men with metastatic CRPC who have previously received docetaxel, 1 % each of patients receiving abiraterone acetate plus prednisone or placebo plus prednisone died due to cardiac adverse events [26].
The laboratory findings observed following abiraterone acetate plus prednisone therapy in men with metastatic CRPC were generally consistent with those previously reported [44]. Grade 3 or 4 phosphorus abnormalities were observed in 5 % of patients receiving abiraterone acetate plus prednisone and 2 % of those receiving placebo plus prednisone. Of note, the majority of initial elevations in liver enzymes occurred within the first 3 months of abiraterone acetate plus prednisone therapy [44].
Grade 3 or 4 hepatotoxicity, consisting predominately of a reversible elevation in aminotransferase levels, was observed in 8 % of abiraterone acetate plus prednisone recipients and 3 % of placebo plus prednisone recipients with metastatic CRPC who have not previously received chemotherapy [24]. Serious hepatotoxicity was observed in 1.1 and 0.6 % of patients [44]. No patient in either treatment group died from hepatotoxicity-related adverse events [24]. In the study in men with metastatic CRPC who have previously received docetaxel, a grade 4 elevation in aminotransferase levels resulted in a protocol amendment (more frequent liver function tests during the first 12 weeks of therapy) at the time of the interim analysis [25]. However, at this timepoint, the incidence of liver-function test abnormalities were similar between the abiraterone acetate plus prednisone and placebo plus prednisone treatment groups (statistical analysis not reported). Of note, the mechanism for abiraterone hepatotoxicity is as yet unknown [44].
As expected, the mineralocorticoid adverse events of hypertension, hypokalaemia, and fluid retention or oedema (all grades) were more frequent with abiraterone acetate plus prednisone than placebo plus prednisone in patients with metastatic CRPC (Fig. 2) [24, 26]. Among men with metastatic CRPC who have not previously received chemotherapy, the mineralocorticoid adverse events were mostly grade 1 or 2 in severity [24]; serious mineralocorticoid adverse events were observed in 0.2–0.7 % of patients in each treatment group [44]. In general, mineralocorticoid adverse events were able to be successfully managed medically [12]. The coadministration of a corticosteroid reduces the incidence and severity of these adverse events (see Sect. 2) [12].
7 Dosage and Administration
Abiraterone acetate is indicated in the EU [12] as combination therapy with prednisone or prednisolone in men with asymptomatic or mildly symptomatic metastatic CRPC following the failure of androgen deprivation therapy in whom chemotherapy is not yet clinically indicated and in men with metastatic CRPC whose disease has progressed on or after docetaxel-containing chemotherapy. In the US [13], oral abiraterone acetate is indicated as combination therapy with prednisone in men with metastatic CRPC.
The recommended dosage of abiraterone acetate is 1,000 mg (four 250 mg tablets) once daily, to be administered with prednisone or prednisolone 10 mg/day [12] or prednisone 5 mg twice daily [13]. Abiraterone acetate must be consumed on an empty stomach; no food should be consumed for at least 2 h before and at least 1 h after the administration of abiraterone acetate [12, 13] (see Sect. 3).
In patients not surgically castrated, medical castration with a LHRH analogue should be continued during therapy with abiraterone acetate [12].
Serum transaminase levels should be evaluated prior to the initiation of abiraterone acetate therapy, every 2 weeks for the first 3 months, then monthly thereafter [12]. Dosage delays and/or reductions are recommended for patients who develop hepatotoxicity (ALT and/or AST levels >5 × ULN [12, 13] or total bilirubin levels >3 × ULN [13]); see the local prescribing information for further details.
As abiraterone acetate therapy may be associated with hypertension, hypokalaemia and fluid retention or oedema (see Sect. 6.2), caution is advised in patients with a history of cardiovascular disease or those with underlying medical conditions (e.g. heart failure, recent myocardial infarction or ventricular arrhythmia) that may be compromised by such adverse events [12, 13]. Patients should be monitored at least once a month for these events, which should be corrected and controlled prior to and during treatment with abiraterone acetate [12, 13].
Therapy with abiraterone acetate has been associated with myopathy, including rhabdomyolysis with renal failure [12]. Therefore, caution is recommended in patients receiving concomitant therapy with agents known to be associated with myopathy/rhabdomyolysis [12].
Local prescribing information should be consulted for detailed information, including contraindications, dose adjustments, drug interactions, monitoring requirements, precautions, and use in special patient populations.
8 Place of Abiraterone Acetate in Metastatic Castration-Resistant Prostate Cancer
CRPC is characterized by disease progression despite the persistence of castrate levels of androgens (testosterone <50 ng/dL [<1.7 nmol/L]) [4, 46]. It may present as a continuous elevation in serum PSA levels, a progression of pre-existing disease and/or the appearance of further metastases [4, 46]. Notably, it is still hormone-sensitive, retaining an androgen receptor-driven mechanism for development [2, 4, 46].
Recent evidence suggests several mechanisms by which androgen receptor activation drives prostate cancer growth despite the presence of low circulating testicular androgen levels [6, 7, 10, 17]:
-
ligand-dependent mechanisms such as androgen receptor upregulation via gene amplification or protein overexpression, and extragonadal androgen production (i.e. androgens synthesized intratumourally via the de novo route or converted from adrenal androgens) through CYP17 upregulation and;
-
ligand-independent mechanisms such as androgen receptor coactivator expression, androgen receptor mutation and androgen receptor splice variants.
The identification and understanding of these mechanisms is driving research into the development of agents for the treatment of CRPC that target the androgen receptor signalling pathway [6, 7, 10]. For instance, abiraterone acetate is a selective inhibitor of CYP17 (Sect. 2), while enzalutamide is an androgen receptor and nuclear translocation inhibitor that has also demonstrated inhibitory activity against prostate cancer cell lines harbouring androgen receptor splice variants [10]. Enzalutamide is currently approved in the EU [47] and the US [48] for the treatment of men with metastatic CRPC whose disease has progressed on or after docetaxel chemotherapy, and in a recent phase III study was associated with a significant overall survival benefit compared with placebo [49]. Several other novel agents targeting the androgen receptor (e.g. ARN509, galeterone (TOK001) and orteronel [TAK700]) are currently undergoing clinical studies [10, 50]. Data from these studies are awaited with interest.
Historically, men with prostate cancer have not been considered ideal candidates for an immunotherapy approach owing to previous data indicating the low immunogenicity of cancerous prostatic cells [50]. However, recent evidence has indicated that cancerous prostatic cells can not only stimulate an immune response, but also elude it via several biological mechanisms, including the down regulation of MHC I molecules and the secretion of soluble immunosuppressive factors (e.g. TGF-β and IL-10) [50]. Sipuleucel-T is an autologous active cellular immunotherapy designed to stimulate a T-cell response against prostatic acid phosphatase, an antigen expressed in the majority of prostate cancers, but not in non-prostate tissue [51]. It is approved in the US for the treatment of men with asymptomatic or minimally symptomatic metastatic CRPC, and in a recent phase III study was associated with a statistically significant advantage over placebo for overall survival [51].
The treatment of CRPC depends upon the metastatic status of the patient [5]. According to the US National Comprehensive Cancer Network (NCCN) guidance for the treatment of prostate cancer [5] and the European Association of Urology (EAU) guidelines for the treatment of advanced, relapsing and castration-resistant prostate cancer [52], men with CRPC with no or minimal signs of metastases should be observed [5] or treated with secondary androgen deprivation therapy (i.e. androgen deprivation therapy subsequent to medical or surgical castration) [5, 52]. Such patients may also benefit from inclusion in clinical studies [5, 52]. For men with metastatic CRPC without symptoms, therapy with abiraterone acetate or sipuleucel-T (appropriate for patients who have a good performance level [ECOG 0–1] and a ≥6 months’ life expectancy) should be considered [5]. Such patients may benefit from chemotherapy with docetaxel, secondary androgen deprivation therapy with, among others, enzalutamide, and inclusion in clinical studies [5].
For men with symptomatic metastatic CRPC, [5] docetaxel plus prednisone is recommended by both the NCCN [5] and EAU [52] guidelines, with mitoxantrone a viable therapeutic option for patients who cannot tolerate docetaxel. The NCCN guidelines further recommend radium-223 for patients with symptomatic bone metastases [5]. The combination of docetaxel and prednisone has been the standard first-line chemotherapy in CRPC since demonstrating improved survival compared with the previous standard regimen, mitoxantrone plus prednisone, in a phase III study in 2004 [53]. Although docetaxel has since been combined with various agents that have demonstrated additive or synergistic activity in preclinical studies in an effort to further improve outcomes, to date, overall survival has not been extended compared with docetaxel plus prednisone [53]. Of note, the addition of estramustine to docetaxel is not recommended as it has been shown to elevate adverse events without enhancing efficacy [5].
There is currently no consensus in the US guidelines [5] as to the best therapy following the failure of docetaxel in men with metastatic CRPC, with abiraterone acetate, cabazitaxel, enzalutamide and radium-223 all identified as potential options. Other possibilities are docetaxel rechallenge, mitoxantrone, other secondary androgen deprivation therapies, salvage chemotherapy, sipuleucel-T and participation in a clinical study [5]. The EAU guidelines [52] consider cabazitaxel as an effective treatment following docetaxel therapy, based on significantly prolonged overall survival and PFS with cabazitaxel plus prednisone versus mitoxantrone plus prednisone in a phase III study in patients with metastatic CRPC who had progressed during or after docetaxel therapy [54]. Other options include docetaxel rechallenge, mitoxantrone, molecular-targeted therapy and vinorelbine [52]. Of note, at the time of publication of the EAU guidelines [52], the role of abiraterone acetate and enzalutamide was yet to be determined, with the place of sipuleucel-T in the current treatment algorithm still under consideration. The National Institute for Health and Clinical Excellence technology appraisal guidance [55] recommends abiraterone acetate as an option for the treatment of patients with metastatic CRPC whose disease has progressed during or following one docetaxel-containing chemotherapy regimen.
In men with metastatic CRPC who had not previously received chemotherapy participating in a placebo-controlled, multinational phase III study, abiraterone acetate plus prednisone significantly prolonged median rPFS (Sect. 5.1.1). However, a significant overall survival benefit was not observed at the time of the second and third interim analyses (Sect. 5.1.1). Combination therapy with abiraterone acetate plus prednisone also demonstrated significant advantages over placebo plus prednisone in terms of the time until the initiation of opiate analgesia, the initiation of cytotoxic chemotherapy, a decline in ECOG performance status and PSA progression, and in the time to an elevation in pain and a decline in functional status (Sect. 5.1.2). Of note, in this study, placebo plus prednisone recipients could be switched to abiraterone acetate plus prednisone therapy, which may potentially affect the ability to demonstrate statistical significance between the abiraterone acetate and placebo groups in the final overall survival analysis [24].
In men with metastatic CRPC who had previously received docetaxel, combination therapy with abiraterone acetate plus prednisone was significantly more effective than placebo plus prednisone in prolonging median overall survival in a multinational, phase III study after a median follow-up of up to 20.2 months (Sect. 5.2.1). The combination of abiraterone acetate plus prednisone also resulted in a significantly longer median rPFS and time to PSA progression and a significantly higher median PSA response rate after a median follow-up of up to 20.2 months (Sect. 5.2.2). Significant benefits in bone-related symptoms (patient-reported pain palliation and skeletal-related events) were also observed with abiraterone acetate plus prednisone. Notably, the final analysis of this study was conducted after 775 death events, 97 % of the required total of 797 death events [26]. Although the investigators state that the effect of 3 % fewer death events than prespecified on the overall results is probably negligible, they indicate that because of this, the hazard ratio should be interpreted with caution [26]. Moreover, while the survival benefit observed with abiraterone acetate plus prednisone at the final analysis appears to be independent of prior treatment with docetaxel, it is worth noting that patients were not required to demonstrate disease progression following previous therapy, as toxicity with this chemotherapeutic agent may have resulted in discontinuation [12].
The study in men with metastatic CRPC who had not previously received chemotherapy [24] (see Sect. 5.1) only included patients with no or mild symptoms according to the BPI-SF and excluded patients with visceral metastases, with both pain and visceral metastases considered to be a poor prognostic factor [52]. Studies assessing the efficacy of abiraterone acetate in patients with poor prognostic factors (e.g. anaemia [haemoglobin levels <13 g/dL], bone scan progression, estramustine therapy prior to docetaxel therapy, pain and visceral metastases [52]) who had not previously received chemotherapy or who had previously received docetaxel, and head-to-head studies comparing abiraterone acetate with standard chemotherapy in both patient populations would be of interest. Although beyond the scope of this review, it is worth noting that abiraterone acetate plus prednisone, alone or in combination with other anticancer agents, including cabazitaxel, enzalutamide and trebananib (AMG386), is a current focus of interest in ongoing clinical studies in metastatic CRPC and in other indications (e.g. breast cancer). Results from these studies are awaited with interest.
Given the nature of the therapy, the overall tolerability profile of abiraterone acetate, in combination with prednisone, was acceptable in and generally consistent between men with metastatic CRPC who have not previously received chemotherapy and those who have previously received docetaxel (Sect. 6.1). The most frequently reported treatment-emergent adverse events (all grades) with abiraterone acetate plus prednisone in men with metastatic CRPC were fatigue, back pain and arthralgia. Adverse events associated with abiraterone acetate therapy and considered of special interest include cardiac adverse events, hepatotoxicity (liver function test abnormalities) and mineralocorticoid adverse events (hypokalaemia, hypertension, and fluid retention or oedema) [Sect. 6.2]. Dosage delays and/or reductions are recommended for patients who develop hepatotoxicity and caution is advised in patients with a history of cardiovascular disease or those with underlying medical conditions that may be compromised by such adverse events (Sect. 7). In general, the adverse events of special interest observed following therapy with abiraterone acetate plus prednisone in two multinational studies were consistent with the known tolerability profile of the agent (Sect. 6.2).
Currently, pharmacoeconomic data for abiraterone acetate versus other currently approved agents are limited and are based on indirect comparisons of clinical data from non-head-to-head phase III studies. Three cost-utility analyses in patients with metastatic CRPC who have previously received docetaxel predicted that abiraterone acetate plus prednisone dominates cabazitaxel plus prednisone in Brazil [56] and Sweden [57] and is cost effective relative to cabazitaxel or mitoxantrone plus prednisone at a willingness-to-pay threshold of US$100,000 in the US [58]. As with all pharmacoeconomic analyses, these preliminary cost-effectiveness analyses have limitations, including the utilization of indirect comparative data from clinical studies with differences in design and patient populations, and the results cannot be generalized to other geographical locations. Further well designed pharmacoeconomic studies are needed to help clarify the relative cost effectiveness of abiraterone acetate in the treatment of men with metastatic CRPC who have previously received docetaxel and to determine the cost effectiveness of abiraterone acetate in the treatment of men with metastatic CRPC who have not previously received chemotherapy.
In conclusion, abiraterone acetate, in combination with prednisone, is effective in the treatment of men with metastatic CRPC. Overall survival and rPFS were significantly prolonged in men with metastatic CRPC who had previously received docetaxel. In men with metastatic CRPC who had not previously received chemotherapy, there was a strong trend towards an overall survival benefit, a significant prolongation in rPFS and significant delays in clinical decline, the need for chemotherapy and the onset of pain observed. Given the nature of the therapy, the overall tolerability profile of abiraterone acetate, in combination with prednisone, was acceptable in men with metastatic CRPC. Although the final overall survival data in men with metastatic CRPC who have not previously received chemotherapy are awaited, current evidence indicates that abiraterone acetate is a useful option for the treatment of metastatic CRPC.
Data selection sources:
Relevant medical literature (including published and unpublished data) on abiraterone acetate was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) [searches last updated 4 November 2013], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Abiraterone, neoplasms, prostate cancer, prostatic.
Study selection: Studies in patients with metastatic castration-resistant prostate cancer who received abiraterone acetate. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
Bluemn EG, Nelson PS. The androgen/androgen receptor axis in prostate cancer. Curr Opin Oncol. 2012;24(3):251–7.
Massard C, Fizazi K. Targeting continued androgen receptor signaling in prostate cancer. Clin Cancer Res. 2011;17(12):3876–83.
Horwich A, Parker C, Bangma C, et al. Prostate cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21(Suppl 5):v129–33.
Hotte SJ, Saad F. Current management of castrate-resistant prostate cancer. Curr Oncol. 2010;17(Suppl 2):S72–9.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: prostate cancer (Version 4.2013). 2013. http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf (Accessed 11 Nov 2013).
Mohler JL, Titus MA, Wilson EM. Potential prostate cancer drug target: bioactivation of androstanediol by conversion to dihydrotestosterone. Clin Cancer Res. 2011;17(18):5844–9.
Schweizer MT, Antonarakis ES. Abiraterone and other novel androgen-directed strategies for the treatment of prostate cancer: a new era of hormonal therapies is born. Ther Adv Urol. 2012;4(4):167–78.
Small EJ, Halabi S, Dawson NA, et al. Antiandrogen withdrawal alone or in combination with ketoconazole in androgen-independent prostate cancer patients: a phase III trial (CALGB 9583). J Clin Oncol. 2004;22(6):1025–33.
Attard G, Reid AH, A’Hern R, et al. Selective inhibition of CYP17 with abiraterone acetate is highly active in the treatment of castration-resistant prostate cancer. J Clin Oncol. 2009;27(23):3742–8.
Tsao CK, Galsky MD, Small AC, et al. Targeting the androgen receptor signalling axis in castration-resistant prostate cancer (CRPC). BJU Int. 2012;110(11):1580–8.
Yang LP. Abiraterone acetate: in metastatic castration-resistant prostate cancer [Erratum appears in Drugs. 2012;72(2):192]. Drugs. 2011;71(15):2067–77.
European Medicines Agency. ZYTIGA 250 mg tablets: summary of product characteristics; 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002321/WC500112858.pdf (Accessed 11 Nov 2013).
Janssen Biotech Inc. ZYTIGA® (abiraterone acetate) tablets: prescribing information; 2013. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/202379s007lbl.pdf (Accessed 11 Nov 2013).
Montgomery RB, Mostaghel EA, Vessella R, et al. Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res. 2008;68(11):4447–54.
Li R, Evaul K, Sharma KK, et al. Abiraterone inhibits 3-hydroxysteroid dehydrogenase: a rationale for increasing drug exposure in castration-resistant prostate cancer. Clin Cancer Res. 2012;18(13):3571–9.
Potter GA, Barrie SE, Jarman M, et al. Novel steroidal inhibitors of human cytochrome P45017α (17α-hydroxylase-C17,20-lyase): potential agents for the treatment of prostatic cancer. J Med Chem. 1995;38(13):2463–71.
Yamaoka M, Hara T, Kusaka M. Overcoming persistent dependency on androgen signaling after progression to castration-resistant prostate cancer. Clin Cancer Res. 2010;16(17):4319–24.
Ang JE, Olmos D, de Bono JS. CYP17 blockade by abiraterone: further evidence for frequent continued hormone-dependence in castration-resistant prostate cancer. Br J Cancer. 2009;100(5):671–5.
Attard G, Reid AH, Yap TA, et al. Phase I clinical trial of a selective inhibitor of CYP17, abiraterone acetate, confirms that castration-resistant prostate cancer commonly remains hormone driven [Erratum appears in J Clin Oncol. 2012;30(15):1896]. J Clin Oncol. 2008;26(28):4563–71.
Ryan CJ, Smith MR, Fong L, et al. Phase I clinical trial of the CYP17 inhibitor abiraterone acetate demonstrating clinical activity in patients with castration-resistant prostate cancer who received prior ketoconazole therapy. J Clin Oncol. 2010;28(9):1481–8.
Efstathiou E, Titus M, Tsavachidou D, et al. Effects of abiraterone acetate on androgen signaling in castrate-resistant prostate cancer in bone. J Clin Oncol. 2012;30(6):637–43.
Reid AH, Attard G, Danila DC, et al. Significant and sustained antitumor activity in post-docetaxel, castration-resistant prostate cancer with the CYP17 inhibitor abiraterone acetate. J Clin Oncol. 2010;28(9):1489–95.
Danila DC, Morris MJ, de Bono JS, et al. Phase II multicenter study of abiraterone acetate plus prednisone therapy in patients with docetaxel-treated castration-resistant prostate cancer. J Clin Oncol. 2010;28(9):1496–501.
Ryan CJ, Smith MR, de Bono JS, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368(2):138–48.
de Bono JS, Logothetis CJ, Molina A, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364(21):1995–2005.
Fizazi K, Scher HI, Molina A, et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012;13(10):983–92.
Cai C, Balk SP. Intratumoral androgen biosynthesis in prostate cancer pathogenesis and response to therapy. Endocr Relat Cancer. 2011;18(5):R175–82.
Attard G, Reid AH, Olmos D, et al. Antitumor activity with CYP17 blockade indicates that castration-resistant prostate cancer frequently remains hormone driven. Cancer Res. 2009;69(12):4937–40.
Cai C, Chen S, Ng P, et al. Intratumoral de novo steroid synthesis activates androgen receptor in castration-resistant prostate cancer and is upregulated by treatment with CYP17A1 inhibitors. Cancer Res. 2011;71(20):6503–13.
Mostaghel EA, Marck BT, Plymate SR, et al. Resistance to CYP17A1 inhibition with abiraterone in castration-resistant prostate cancer: induction of steroidogenesis and androgen receptor splice variants. Clin Cancer Res. 2011;17(18):5913–25.
van Soest RJ, van Royen ME, de Morrée ES, et al. Effects on androgen receptor nuclear import by docetaxel, cabazitaxel, abiraterone, and enzalutamide: potential mechanism for cross-resistance in castration-resistant prostate cancer (CRPC) [abstract no. 5064]. J Clin Oncol. 2013;31(15 Suppl 1).
Ryan CJ, Shah S, Efstathiou E, et al. Phase II study of abiraterone acetate in chemotherapy-naive metastatic castration-resistant prostate cancer displaying bone flare discordant with serologic response. Clin Cancer Res. 2011;17(14):4854–61.
Tolcher AW, Chi KN, Shore ND, et al. Effect of abiraterone acetate plus prednisone on the QT interval in patients with metastatic castration-resistant prostate cancer. Cancer Chemother Pharmacol. 2012;70(2):305–13.
Marbury T, Stonerock R, Acharya M, et al. A phase 1 single-dose open-label pharmacokinetic (PK) study of abiraterone acetate (AA) in male subjects with mild or moderate hepatic impairment [abstract no. 7055]. Eur J Cancer. 2011;47:S501.
Marbury T, Stonerock R, Tran N, et al. A phase 1 single dose open-label reduced/staged pharmacokinetic (PK) and safety study of abiraterone acetate (AA) in men with impaired renal function [abstract no. 7057]. Eur J Cancer. 2011;47:S502.
Chi KN, Tolcher A, Lee P, et al. Effect of abiraterone acetate plus prednisone on the pharmacokinetics of dextromethorphan and theophylline in patients with metastatic castration-resistant prostate cancer. Cancer Chemother Pharmacol. 2013;71(1):237–44.
Logothetis CJ, Basch E, Molina A, et al. Effect of abiraterone acetate and prednisone compared with placebo and prednisone on pain control and skeletal-related events in patients with metastatic castration-resistant prostate cancer: exploratory analysis of data from the COU-AA-301 randomised trial. Lancet Oncol. 2012;13(12):1210–7.
Sternberg CN, Molina A, North S, et al. Effect of abiraterone acetate on fatigue in patients with metastatic castration-resistant prostate cancer after docetaxel chemotherapy. Ann Oncol. 2013;24(4):1017–25.
Harland S, Staffurth J, Molina A, et al. Effect of abiraterone acetate treatment on the quality of life of patients with metastatic castration-resistant prostate cancer after failure of docetaxel chemotherapy. Eur J Cancer 2013;49(17):3648–57.
Saad F, Shore ND, Van Poppel H, et al. Abiraterone acetate in metastatic castration-resistant prostate cancer patients without prior chemotherapy: interim analysis of the COU-AA-302 phase 3 trial [abstract no. 713]. J Urol. 2013;189(4 Suppl):e293.
Shore N, Ryan CJ, Mulders P, et al. The impact of abiraterone acetate therapy on patient-reported pain and functional status in chemotherapy-naïve patients with progressive, metastatic castration-resistant prostate cancer: results from an updated analysis [abstract no. 784]. J Urol. 2013;189(4 Suppl):e323.
Scher HI, Heller G, Molina A, et al. Evaluation of circulating tumor cell (CTC) enumeration as an efficacy response biomarker of overall survival (OS) in metastatic castration-resistant prostate cancer (mCRPC): planned final analysis (FA) of COU-AA-301, a randomized, double-blind, placebo-controlled, phase III study of abiraterone acetate (AA) plus low-dose prednisone (P) post docetaxel [abstract no. LBA4517]. J Clin Oncol. 2011;29(18 Suppl 2).
Goodman OB, Flaig TW, Molina A, et al. Exploratory analysis of the visceral disease (VD) patient subset in COU-AA-301, a phase III study of abiraterone acetate (AA) in metastatic castration-resistant prostate cancer (mCRPC) [abstract no. 14]. J Clin Oncol. 2013;31(Suppl 6).
European Medicines Agency. Assessment report: Zytiga (abiraterone); 2012. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Assessment_Report_-_Variation/human/002321/WC500137814.pdf (Accessed 11 Nov 2013).
Rathkopf DE, Smith MR, de Bono JS, et al. Long-term safety and efficacy analysis of abiraterone acetate (AA) plus prednisone (P) in metastatic castration-resistant prostate cancer (mCRPC) without prior chemotherapy (COU-AA-302) [abstract no. 5009]. J Clin Oncol. 2013;31(15 Suppl 1).
Heidenreich A, Bolla M, Joniau S, et al. Guidelines on prostate cancer; 2011. http://www.uroweb.org/gls/pdf/08_Prostate_Cancer.pdf (Accessed 11 Nov 2013).
European Medicines Agency. Xtandi 40 mg soft capsules: summary of product characteristics; 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002639/WC500144996.pdf (Accessed 11 Nov 2013).
Astellas Pharma US Inc. XTANDI® (enzalutamide) capsules for oral use: prescribing information; 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/203415lbl.pdf (Accessed 11 Nov 2013).
Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367(13):1187–97.
Rescigno P, Buonerba C, Bellmunt J, et al. New perspectives in the therapy of castration resistant prostate cancer. Curr Drug Targets. 2012;13(13):1676–86.
Plosker GL. Sipuleucel-T: in metastatic castration-resistant prostate cancer. Drugs. 2011;71(1):101–8.
Mottet N, Bellmunt J, Bolla M, et al. EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2011;59(4):572–83.
McKeage K. Docetaxel: a review of its use for the first-line treatment of advanced castration-resistant prostate cancer. Drugs. 2012;72(11):1559–77.
Keating GM. Cabazitaxel: a guide to its use in hormone-refractory metastatic prostate cancer. Drugs Aging. 2013;30(5):359–65.
National Institute for Health and Clinical Excellence. Abiraterone for castration-resistant metastatic prostate cancer previously treated with a docetaxel-containing regimen (NICE technology appraisal guidance 259); 2012. http://guidance.nice.org.uk/TA259/Guidance/pdf/English (Accessed 11 Nov 2013).
Pereira ML, Bahmdouni LS, Pepe C, et al. Cost-effectiveness analysis of abiraterone for the treatment of advanced prostate cancer under the Brazilian private health care system [abstract no. PCN86]. Value Health. 2012;15(7):A424–5.
Persson U, Nilsson S, Hjortsberg C, et al. Economic evaluation of abiraterone acetate as treatment for metastatic castration resistant prostate cancer after failure of docetaxel in Sweden [abstract no. PCN66]. Value Health. 2012;15(4):A219.
Wilson LS, Zhong L, Pon V, et al. Cost effectiveness analysis of new treatments for metastatic castration-resistant prostate cancer: does severity matter? [abstract no. PCN72]. Value Health. 2012;15(4):A220–1.
Scher HI, Halabi S, Tannock I, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26(7):1148–59.
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article. Changes resulting from comments received were made by the author on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: N. Agarwal, University of Utah Huntsman Cancer Institute, Salt Lake City, UT, USA; R.J. Amato, Division of Oncology, Department of Internal Medicine, Memorial Hermann Cancer Center, University of Texas Health Science Center at Houston (Medical School), Houston, TX, USA; U. Emmenegger, Division of Medical Oncology, Odette Cancer Centre, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, ON, Canada; S. Kadkol, Department of Pathology, University of Illinois at Chicago, Chicago, IL, USA; G. Di Lorenzo, Department of Molecular and Clinical Endocrinology & Oncology, University degli Studi Federico II, Naples, Italy; C. Massard, Department of Cancer Medicine, Institut Gustave Roussy, University of Paris-Sud, Villejuif, France; M. Namiki, Department of Integrative Cancer Therapy and Urology, Kanazawa University Graduate School of Medical Science, Kanazawa, Japan.
Rights and permissions
About this article
Cite this article
Hoy, S.M. Abiraterone Acetate: A Review of Its Use in Patients with Metastatic Castration-Resistant Prostate Cancer. Drugs 73, 2077–2091 (2013). https://doi.org/10.1007/s40265-013-0150-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-013-0150-z