Abstract
Introduction
There are several barriers to conducting medication management in nursing homes. Our project aimed to develop an algorithm that guides and supports pharmacists to perform this clinical service.
Methods
Phase I of the project examined the practitioner and patient perspectives on the medication process in nursing homes. The mixed methods approach consisted of interviews with qualitative content analysis and a quantitative questionnaire. Phase IIa scoped existing research and comprised a three-stepped systematic review. It was registered in the International Prospective Register of Systematic Reviews (CRD42017065002). Results of the first two steps were assessed for quality. Phase IIb was performed as a Delphi survey. The developed algorithm was tested in nursing homes. The primary endpoint was the number and type of detected drug-related problems. The study was conducted between June 2016 and December 2018 (Deutsches-Register-Klinischer-Studien-ID: DRKS00010995).
Results
Interviews were held with 21 healthcare practitioners and six patients. Frequent and relevant aspects of the medication process in nursing homes were identified. The systematic reviews included 28 reviews, 12 interventional studies and 1450 non-interventional studies. As a result of the Delphi survey, two new aspects were added. Testing of the drafted algorithm was done in 73 nursing home residents. A mean of 6.3 drug-related problems were detected. Sample cases were executed in a mean time of 21 min by community pharmacists.
Conclusions
The developed and consented algorithm can guide pharmacists in conducting medication management in a timely and effective manner. It might serve as a facilitator to improve collaboration and quality of medication in nursing home residents.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Medication management is beneficial for nursing home residents but is rarely conducted in this setting in Germany. |
The AMBER project developed an algorithm that can guide pharmacists in conducting medication management for nursing home residents. |
Implementation of this tool into standard care can foster medication safety in a population that might not have independent access to all facets of healthcare services. |
1 Introduction
Residents of nursing homes are a vulnerable patient group when it comes to drug therapy [1,2,3]. Aging, multimorbidity, polymedication and physiologic changes, like a declining renal function, lead to increased risks [4,5,6,7,8]. Drug therapy is usually applied by the facility nurses, resulting in a high level of heteronomy and dependance. Several studies have demonstrated positive effects of comprehensive medication management (CMM) or medication review (MR), delivered by community pharmacies, for the general population and in nursing home care [9,10,11,12]. CMM is defined by the Patient-Centered Primary Care Collaborative (PCPCC) as “the standard of care that ensures each patient’s medications are individually assessed to determine that each medication is appropriate for the patient, effective for the medical condition, safe given the comorbidities and other medications being taken, and able to be taken by the patient as intended” [13]. It is delivered in collaboration with other providers to optimize patient outcomes [14]. Depending on the jurisdiction, pharmacies have certain obligations associated with the drug supply of nursing home residents [15]. Drug-therapy optimization in this specific setting requires an emphasis on interprofessional collaboration, as nurses are usually first to realize changes in a patient’s health condition [16, 17]. A systematic review by Kwak et al. found that CMM in nursing homes can be cost effective if it is performed by an interprofessional team [18]. Potential barriers to implementing CMM in nursing homes are, among others, lack of time and inadequate reimbursement [19]. In Australia, MR in nursing homes is remunerated but pharmacists stated that more funding was required to achieve a team-based intervention [20]. Internationally, clinical services, education and clinical skills are implemented to different extents among pharmacists [21]. Structured guidance can lead to a higher quality level of services. The TIMER® tool, as an example, was developed to support pharmacists in conducting CMM in Texas [22]. It differs from safety tools, like lists for identifying potentially inappropriate medication (PIM), by covering aspects of therapy optimization as well as safety aspects. Examples of PIM lists are the Beers criteria or the EU(7) PIM list [23, 24]. Potential shortages of labor force and time in pharmacies and nursing home facilities are problems that need to be taken into account when exploring potential solutions to promote CMM in this specific setting [25,26,27].
1.1 Aims
The AMBER project aimed to develop an algorithm that can provide guidance for pharmacists conducting CMM in nursing homes. It should address the most relevant and frequent aspects of therapy and safety in the medication process and be highly feasible and time saving for all participants.
2 Methods
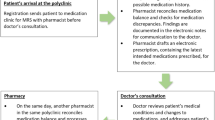
To reach a high validity, several individual studies were coordinated in four major study phases (Fig. 1):
-
Phase I: the practitioner’s and patient`s perspective. Interviews and questionnaires on the medication process in nursing homes were held with patients, nurses, physicians and pharmacists.
-
Phase IIa: considering prior research. A three-stepped systematic review was done on different aspects of the medication process in nursing homes.
-
Phase IIb: experts’ position. Based on the results of phase I and IIa, a Delphi survey was conducted.
-
Phase III: clinical testing. The refined algorithm and resulting tool was tested in nursing homes. Additional analyses on feasibility were done.
Study phases (according to the study protocol [28]) and timeline
2.1 Ethics
The interventional study followed the principles of the Declaration of Helsinki [29]. Informed consent was obtained from all study participants or their legal attorney. The regional ethics committee of the Medical Association of Westphalia-Lippe and the University of Muenster approved the study (registration number 2017-350-f-S). The study was registered at the German Clinical Trials Register (DRKS-ID: DRKS00010995). The study protocol has been published previously [28].
2.2 Phase I: Interviews with Healthcare Practitioners and Patients
Twelve randomly chosen nursing homes in Muenster, Germany were asked to join the study. Interview participants were recruited from the included nursing homes as a convenience sample, aiming for a total of ≥ 20 interviews with similar numbers per group of patients, pharmacists, physicians and nurses. Healthcare professionals were required to have > 1 year of working experience in nursing home facilities to be included.
Practitioner interviews and questionnaires were conducted following a mixed methods approach, which combined qualitative and quantitative aspects. Interviews featured open questions to get feedback on uncertainties, goals and problems in the medication process. The specifically developed questionnaire on experiences, standards and expectations on problems, risks and goals in the medication process consisted of 51 aspects, which were rated regarding frequency and relevance. These aspects could be allocated to the domains of general challenges in the medication process, patient goals, barriers in communication, medical goals and pharmaceutical aspects (see Electronic Supplementary Material [ESM] 1). Questions were designed to cover the medication process in nursing homes from the beginning (initialization of prescription) to the end (therapeutic monitoring). Insight into the medication process was gained from discussion rounds with a geriatrician, a general practitioner, a geriatric pharmacist and a nurse. Qualitative content analysis was done according to Mayring, engaging the software MAXQDA (version 12, VERBI software GmBH, Germany) [30]. The frequency of the coded categories was counted. Each of the 51 aspects was rated on a five-point Likert scale on frequency and relevance. A combined index was formed by adding the rating for frequency to the rating for relevance and dividing it by two. Aspects, rated and calculated in this way by > 50% of the participants with an index of ≥ 3, were considered as meaningful and were considered for the first draft of the algorithm. For nursing home residents, a reduced questionnaire with 24 questions on relevance only was developed, with respect to limited resilience and concentration. Questionnaires and interviews were performed from June 1, 2016 to December 31, 2016.
2.3 Phase IIa: Systematic Reviews
A systematic review was conducted following the patient, intervention, comparison and outcome (PICO) framework and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (ESM 2, Table 1). It was divided into three consecutive steps, as each step required an individual search strategy and method. The following databases were searched: MEDLINE/PCM (via PubMed), PsycINFO (via EBSCOhost), CDSR (via Cochrane Library), CINAHL (via EBSCOhost), International Pharmaceutical Abstracts (via EBSCOhost) and NHSEED/DARE (via CRD). The review was registered in the International Prospective Register of Systematic Reviews (PROSPERO, registration number CRD42017065002) [31]. CITAVI© Software 5.7.1.0 (Swiss Academic Software GmbH, Waedenswil, Switzerland) was engaged for data management and for removing duplications. In addition, duplications were removed by hand. Studies were excluded during screening and full-text assessment if they were not written in English or German, did not provide any results (e.g. study protocols), were not related to the medication process, and if they were letters, comments, author’s views and congress or seminar papers. Retrieved titles and abstracts were extracted by one reviewer (SE). Two reviewers analyzed the studies for inclusion in the review (SE, OR). Discrepancies were resolved by discussion. Extraction was done on the number of studies included (for step 1), the number of participants, the study design, the review question, the intervention (steps 1 and 2) and the findings (SE).
Step 1 focused on available reviews, systematic reviews and meta analyses on medication-related interventions in nursing homes. The methodological quality of the reviews was assessed using the ‘Assessment of Multiple SysTemAtic Reviews’ (AMSTAR) checklist (SE, OR) [32, 33]. The objective of step 2 of the systematic review was to find more recent interventional studies on medication-related interventions in nursing homes that were not covered by step 1. The quality of the retrieved studies was assessed with the ‘template for intervention description and replication’ (TIDieR) checklist [34]. Step three comprised under-reported problems in nursing homes, reported by non-interventional studies, like observational trials, qualitative research and guidelines on problems in the medication process in nursing homes.
A narrative synthesis was done for all three steps in accordance with a guidance paper by Popay et al. [35]. Only studies that had been completed and published at the time of the review were included. The searches were conducted from March 2017 onwards and included studies from 2000 or later. The full search strategies and the detailed timelines are provided in ESM 3. Authors of included studies were not contacted for provision of further data.
2.4 Phase IIb: Preliminary Algorithm and Delphi Survey
A preliminary algorithm was developed by comparing the results of the interviews to the results of the systematic reviews. Aspects of the algorithm were summarized to statements and included in an international Delphi survey. Participants in the Delphi survey were pharmacists and researchers with experience in patient and nursing home care. They were recruited for participation as members of the Pharmaceutical Care Network Europe (PCNE). Rating of the aspects was done with a 5-point Likert scale, with 1 meaning no agreement and 5 expressing full agreement. The survey consisted of additional text fields for comments and a final open question. It was distributed via the web-based software SurveyMonkey® (San Mateo, CA, USA). Consensus was defined as an agreement of ≥ 70% (rating 4 or 5) and a median of ≥ 3 on the Likert scale. For the second Delphi round, additional and modified aspects retrieved from the comments in round one were presented to the expert panel. The Delphi survey took place from July 1, 2017 to December 31, 2017. Results were used to approve, modify or supplement the steps of the algorithm.
2.5 Phase III: Testing and Validation
The modified and refined algorithm was tested in nursing homes. The study protocol followed the ‘Standard Protocol Items: Recommendations for Interventional Trials’ SPIRIT 2013 statement [36, 37] and conformed to the ‘Manual for the Design of Non-Drug Trials in Primary Care’ by Joos et al. [38]. The aim of the test was to get an impression of the effectiveness, feasibility and acceptance of the algorithm for conducting CMM in nursing homes. A single-armed prospective study was planned. Detection of drug-related problems (DRPs) was determined as the endpoint of the intervention. The study was conducted over 12 months from January 1, 2018 to December 31, 2018 in nursing homes in North Rhine-Westphalia, Germany. Inclusion criteria were
-
age ≥ 65 years;
-
resident of a nursing home facility;
-
multimorbidity, defined as two or more chronic diseases [39];
-
polymedication with five or more systemically available drugs;
-
informed consent to participate in the study by the resident or legal attorney.
Participation in another clinical study was defined as an exclusion criterion.
2.5.1 Intervention
After recruitment of the nursing homes, all residents were screened for inclusion criteria and asked to give informed consent. The general practitioners responsible for the included patients were contacted by the lead researcher (SE). Patient data were retrieved from the documentation system of the nursing homes and from the physicians. Further information was gathered from a patient interview and from the nurses. Based on the available information, an algorithm-based CMM was conducted (SE). Results of the algorithm-based CMM were documented and a SOAP note (acronym for a clinical communication form consisting of information on subjective, objective, assessment and plan) was handed to the physician and to the nurse. A case discussion was offered [40]. The SOAP notes contained the detected aspects, suggestions to resolve them and references to the therapy. The CMM was done in accordance with the PCPCC and American College of Clinical Pharmacy (ACCP) definitions [13, 14]. Number and type of DRPs were analyzed descriptively. Otherwise, standards of care remained unchanged throughout the study phase. Power was calculated with a two-sided Wilcoxon signed-rank test with a significance level of 0.05, and yielded in 75 patients. The details are described in the study protocol [16].
Convenience, feasibility and reproducibility was tested by five pharmacists, who analyzed nine randomly chosen patient cases with an electronic tool (SurveyMonkey®), which was based on the algorithm. The pharmacists were in charge of providing medication to one or more nursing homes but did not conduct CMM on a regular basis. They were selected by the study authors as a convenience sample.
2.5.2 Endpoints
The primary endpoint of the study was the number of detected DRPs according to the ‘PCNE Classification V 8.01’ via algorithm [41]. Secondary outcomes were acceptance of the CMM by physicians and nurses, the discrepancy in DRPs between the algorithm-based CMM and the comprehensive CMM and the feasibility (time spent conducting an algorithm-guided CMM per case, open feedback question). All patients from the participating nursing homes were screened for inclusion and exclusion criteria. Patient data collected were name and study number, age and gender, medication, diagnoses, vital signs and laboratory data. Data were managed with Microsoft® Excel® Software version 1912, (Microsoft, Redmond, Washington, USA) and SPSS version 20.0 Inc. (IBM, Chicago, Illinois, USA). All data was anonymized for further evaluation. Results were analyzed descriptively. For the Likert-scale questions and the Delphi survey, average, median, the coefficient of variation and consensus estimates were calculated. As endpoints for feasibility testing, time was measured and feedback was collected by asking for comments. In addition to the algorithm-based CMM, an unguided CMM was done for the same patients to the best of the ability of the researchers (SE, OR) to compare both approaches regarding the number of detected DRPs.
3 Results
3.1 Phase I: Practitioner Interviews and Questionnaires
A total of 27 interviews and questionnaires were held on frequent and relevant aspects of the medication process in nursing homes. They consisted of seven encounters with physicians, seven encounters with pharmacists, seven encounters with nurses and six encounters with patients. Baselines characteristics of the interviewees are summarized in ESM 4, Table 1. The results of the quantitative analysis on frequent and relevant aspects of the medication process in nursing homes differed considerably between the three professions. Interviewees did not respond to all 51 questions. Hence, for the group of pharmacists, only 36 aspects could be analyzed (physicians 50, nurses 49). Polymedication, cognitive impairment, blood pressure and blood sugar control were mentioned by more than one group as meaningful. Reliable pain management was rated as important by all groups. Detailed results of relevant and frequent problems, which were rated with a combined Likert-scale index ≥ 3, are shown in ESM 4, Table 2. The qualitative content analysis of the interviews showed that the largest barriers in the medication process were located in the field of communication. In particular, the communication between physicians and nurses was described as challenging. Missing background information upon handling the drugs was an aspect mentioned by all professions. Summarized results of the qualitative content analysis are described in ESM 4, Table 3.
3.2 Phase IIa: Systematic Review
The three-stepped review covered former reviews (step 1), recent interventional studies published after these systematic reviews (step 2) and non-interventional studies (step 3). Figure 2 shows the study flow for searching, screening and selecting the studies within the three steps of the systematic review.
3.2.1 Systematic Review Step 1
Various reviews demonstrated an improvement of drug-related endpoints by medication-related interventions in nursing homes. However, the impact on endpoints like costs, hospitalization or adverse reactions was uncertain [9, 42, 43]. Not all included reviews met the AMSTAR criteria but the methodological quality of most reviews was very high. Interventions should be collaborative and feasible for daily practice, as the settings of the efficacy studies were not always comparable to standard care. In summary, the majority of the reviews found positive effects or MR in nursing homes on increasing safety and quality of the medication, whereas outcomes on all other endpoints were weaker. Step 1 did not add any new aspects to the algorithm but supported the findings from phase I. Table 1 displays the extracted results of the included reviews.
3.2.2 Systematic Review Step 2
In the second systematic review, 12 interventional studies on the medication process in nursing homes were examined. Combined, the studies indicated that a collaborative approach was superior to one-sided efforts. Similar results were found for longitudinal care, which tended to show much better results than unique interventions. PIMs, psychotropic medication, anticholinergic drugs, proton-pump inhibitors as well as crushing drugs were aspects found to be more likely to cause problems in nursing homes. Special attention should be given to transferring the SOAP note with the results of the CMM to the physician, as many suggestions did not reach the general practitioner’s attention and showed limited acceptance (summarized study extraction in ESM 5, Table 1). The emphasis on PIMs and interprofessional communication was included in the algorithm.
3.2.3 Systematic Review Step 3
The systematic review of non-interventional studies included 1450 studies. As expected, the study designs were heterogeneous. There was no assessment of bias performed but, for most aspects, there were studies of obviously higher and lower quality. As there were a high number of studies, they were clustered by medication, indication and complaints. Most studies were dealing with problems caused by antibiotic therapy (n = 300), antipsychotics (n = 99) and PIMs (n = 84). Pain was the complaint mentioned most frequently (n = 116). These aspects were considered for the algorithm. The number of studies for all clusters is displayed in ESM 6, Table 1. Some studies were allocated to multiple clusters, as they were dealing with more than one relevant aspect. In these cases, all the main findings of the studies were included. As they were of non-interventional design, they were usually identifying or describing potentially harmful or problematic aspects of the medication process in nursing home care.
3.3 Phase IIb: Preliminary Aspects and Delphi Survey
Based on the practitioner and patient interviews and the three-stepped systematic review, preliminary aspects for the algorithm were identified and expressed as statements. The survey was sent to 23 international experts, who were members of the PCNE. With 15 responders from 10 countries, the response rate was 65%. All participants were senior researchers (average age 53.8 years) with experience in patient care research of > 15 years. For five statements, an agreement of > 70% was achieved in round 1. The average rating was > 3 (on a scale of 1–5) and the coefficient of variance was ≤ 0.3. Nine experts provided further information on what they feel should be included in an MR in nursing homes. Table 2 shows the results of the Delphi survey round 1.
Based on the results of round 1 of the Delphi survey, two new and two modified statements were presented to the experts in the second round. All experts who participated in round 1 were also asked to participate in round 2. Ten experts responded. Statements and results of round 2 are shown in Table 3.
Due to the high agreement and the small coefficient of variance (0.09–0.22), all new or modified aspects were included so that an algorithm for CMM in nursing homes could be created (Fig. 3).
3.4 Phase III: Practice Testing
The developed algorithm was tested in clinical practice. Recruitment was successful for seven nursing homes. One nursing home dropped out later, as financial harms were suspected from further participation in the study. All contacted nursing homes expressed very limited time and staff capacities. In the remaining six nursing homes, 153 residents or their legal attorneys were contacted and 73 residents gave consent for participation in the study (47.7 %). Even though nurses appreciated the presence of pharmacists, provision of patient data by the nurses was difficult due to the stated massive work overload. Physicians were asked for collaboration in person, via telephone, fax and mail. Despite a data privacy declaration from the patient being provided in all cases and a legal obligation to deliver the patient history was in effect, the patient history was rarely transmitted. However, the medication and some additional data could be collected for all 73 patients from the documentation system of the nursing homes. The average age of the patients was 80.0 years and they were predominantly female (64.4%). Patients used an average of 8.5 drugs for chronic conditions, 3.1 ‘as-needed’ drugs and 0.2 drugs for acute conditions.
The algorithm-based CMM detected 459 DRPs in the 73 residents, an average of 6.3 DRPs per resident. According to the PCNE classification system, most DRPs detected were related to adverse drug events (n = 269), untreated symptoms or indications (n = 124), an effect of the drug treatment that was not optimal (n = 40) and unnecessary drug treatment (n = 21). The steps of the algorithm showed different efficacy in detecting DRPs: in step one, for all patients for whom more than one source of medication lists was available (n = 38), one or more discrepancies in the medication plans was seen. Assessing the patients’ chief complaints found 22 DRPs, clinical parameters 58 DRPs, splitting/crushing drugs 33 DRPs, drug–drug or drug–food interactions 75 DRPs, antibiotics 3 DRPs, PIMs 143 DRPs, indications without a drug 94 DRPs, drugs without indication 31 DRPs (total of 459 DRPs).
To get a first impression of the integrity of these results and as a safety precaution, ten randomly drawn cases were controlled with a comprehensive MR by the authors to the best of their ability. For these ten cases, the algorithm-based CMM revealed an average of 6.7 DRPs, compared with 8.2 DRPs by the most intensive CMM (Δ 1.5 DRP). All of the additionally found DRPs were of a potential nature and could be allocated to an optimization of the therapy regarding guidelines. They were not related to patient safety.
Feasibility of the algorithm was tested with five community pharmacists on nine randomly drawn pseudonymized cases. Pharmacists spent an average of 21:08 min (median of 15:53 min, range 6:38–40:19 min) applying the algorithm to the patient case. Pharmacists consistently stated that the tool was helpful, feasible and time saving and that they wouldn’t have considered all these aspects without this guidance. Screening for PIMs with the Eu(7)-PIM list was described as the most time-consuming step. The pharmacists mentioned that an automatically generated SOAP note would help them to save even more time.
4 Discussion
Based on practitioner interviews, systematic reviews, a Delphi survey and clinical testing, an algorithm was developed that could provide guidance on conducting CMM in nursing homes. Practitioner and patient interviews gave a first impression on important and relevant aspects in the medication process. As each interviewed group mentioned different aspects, a valuable and differentiated picture was formed at this stage. The three-stepped systematic review added the perspective of previous research. It provided the new aspect of antibiotic therapy to the algorithm, and confirmed the results of phase I, as PIMs, anticholinergic drugs, crushing drugs, and pain were described as relevant aspects in nursing homes. Step 1 found a high plausibility that CMM in nursing homes were effective and added feasibility and an emphasis on collaboration to the algorithm. The Delphi survey incorporated expertise and complemented the algorithm with two new aspects. Modifications were suggested. Based on this comprehensive approach, a refined algorithm and resulting ten-stepped tool was developed. A first clinical testing in 73 cases revealed that the algorithm reliably detected the majority of DRPs in an acceptable timeframe of 21 min.
In light of existing literature, the mean number of 6.3 detected DRPs seems reasonable. Pharmacists found a mean of 5.1 DRPs per patient in a nursing home study by Halvorsen et al. [70], a mean of 4.1 DRPs in a study by Vinks et al. [71] and a mean of 3.5 DRPs in a study by Finkers et al. [72]. The pattern of detected DRPs with many adverse drug reactions notably differed from a recent study in German nursing homes, in which pharmacists found a mean of only 1.6 DRPs per patient, predominately drug–drug interactions [73]. This difference in the number and the kind of detected DRPs might indicate that the algorithm can assist pharmacists to expand their scope when conducing a CMM. As the step of optimizing antibiotic therapy found DRPs in only three cases, it may be considered acceptable to skip this step after further clinical testing with similar results.
The timespan of 21 min for conducting an MR with the new algorithm seems appropriate. However, this time did not include the collection of data, nor writing a SOAP note. As a qualitative result of the study, it was observed that collaboration was appreciated by most nurses. Ironically, their perceived work overload was the biggest barrier for implementation of the CMM which, most probably, could help them save time. The limited concerns of the general practitioners might have been due to the remote personal relationship with the pharmacists, an effect that was seen in other nursing home studies previously [74, 75].
4.1 Limitations
The developed algorithm results from a project with a number of methodological strengths. Patients, practitioners, research and experts contributed to find the most frequent and relevant aspects for CMM in nursing home residents. A limitation was the selection of the participants for the interviews, the Delphi survey and the clinical testing, which followed defined criteria but was partly a convenience sample, partly depending on personal relations. The three-stepped systematic review was done with great accuracy; the high number of non-interventional studies, however, did not allow a quality assessment in this step. Clinical testing faced the challenges of a work overload of the nurses and the limited commitment of some physicians. Both barriers may persist in standard care after implementation of the algorithm. On the other hand, this hassle can make collaborative CMM in nursing homes even more important as growing collaboration might lead to mutual understanding. However, CMM might end up being well-meant but poorly executed under these circumstances. Clinical and feasibility testing were performed with a small number of participants and yielded in preliminary data only. Comparison between the algorithm-detected DRPs and DRPs detected by a comprehensive CMM was limited to a few cases. The number of detected DRPs, as an endpoint to compare the algorithm-guided approach with an unguided approach, does not reflect all aspects of the CMM. Relevance of the DRPs was not clearly defined. Furthermore, results were not approved by a multidisciplinary panel. The developed algorithm needs further testing and robust validation; it might need to be adjusted over time. Even though international experts contributed to shape the algorithm, it is unclear whether it can be transferred to other jurisdictions. Likewise, some nursing homes will require altered approaches to meet specific demands.
5 Conclusions
The multi-level AMBER project developed a consented ten-stepped algorithm that can guide pharmacists in conducting CMM in nursing home residents in a timely and efficient manner. It might serve as a facilitator to improve the quality of medication in this highly vulnerable patient group. The algorithm might be especially helpful for pharmacists who have limited experience or are new to CMM in this particular setting. The observed work overload in nursing homes on the one hand makes CMM even more important, and on the other hand needs creative solutions and robust relations to be implemented successfully.
References
O’Sullivan DP, O’Mahony D, Parsons C, Hughes C, Murphy K, Patterson S, Byrne S. A prevalence study of potentially inappropriate prescribing in Irish long-term care residents. Drugs Aging. 2013;30:39–49. https://doi.org/10.1007/s40266-012-0039-7.
Shah SM, Im C, Harris T, DeWilde S, Cook DG. Quality of prescribing in care homes and the community in England and Wales. Br J Gen Pract. 2012;62:e329–36. https://doi.org/10.3399/bjgp12X641447.
Morin L, Laroche M-L, Texier G, Johnell K. Prevalence of potentially inappropriate medication use in older adults living in nursing homes: a systematic review. J Am Med Dir Assoc. 2016;17(862):e1-9. https://doi.org/10.1016/j.jamda.2016.06.011.
Lattanzio F, Landi F, Bustacchini S, Abbatecola AM, Corica F, Pranno L, Corsonello A. Geriatric conditions and the risk of adverse drug reactions in older adults: a review. Drug Saf. 2012;35(Suppl 1):55–61. https://doi.org/10.1007/BF03319103.
Cherubini A, Corsonello A, Lattanzio F. Polypharmacy in nursing home residents: what is the way forward? J Am Med Dir Assoc. 2016;17:4–6. https://doi.org/10.1016/j.jamda.2015.07.008.
Hutchison LC, O’Brien CE. Changes in pharmacokinetics and pharmacodynamics in the elderly patient. J Pharm Pract. 2007;20:4–12. https://doi.org/10.1177/0897190007304657.
Jones SA, Bhandari S. The prevalence of potentially inappropriate medication prescribing in elderly patients with chronic kidney disease. Postgrad Med J. 2013;89:247–50. https://doi.org/10.1136/postgradmedj-2012-130889.
Hubbard RE, O’Mahony MS, Woodhouse KW. Medication prescribing in frail older people. Eur J Clin Pharmacol. 2013;69:319–26. https://doi.org/10.1007/s00228-012-1387-2.
Alldred DP, Kennedy M-C, Hughes C, Chen TF, Miller P. Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev. 2016;2:CD009095. https://doi.org/10.1002/14651858.CD009095.pub3.
Chisholm-Burns MA, Kim Lee J, Spivey CA, Slack M, Herrier RN, Hall-Lipsy E, et al. US pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48:923–33. https://doi.org/10.1097/MLR.0b013e3181e57962.
Doucette WR, McDonough RP, Klepser D, McCarthy R. Comprehensive medication therapy management: identifying and resolving drug-related issues in a community pharmacy. Clin Ther. 2005;27:1104–11.
Koberlein-Neu J, Mennemann H, Hamacher S, Waltering I, Jaehde U, Schaffert C, Rose O. Interprofessional medication management in patients with multiple morbidities. Dtsch Arztebl Int. 2016;113:741–8. https://doi.org/10.3238/arztebl.2016.0741.
Patient-Centered Primary Care Collaborative (PCPCC). The Patient-Centered Medical Home. 2012. https://www.pcpcc.org/sites/default/files/media/medmanagement.pdf. Accessed 28 Sept 2020.
American College of Clinical Pharmacy. Comprehensive medication management in team-based care. https://www.accp.com/docs/positions/misc/CMM%20Brief.pdf. Accessed 28 Sept 2020.
Chia HS, Ho JA, Lim BD. Pharmacist review and its impact on Singapore nursing homes. Singap Med J. 2015;56:493–501. https://doi.org/10.11622/smedj.2015133.
Gulla C, Flo E, Kjome RLS, Husebo BS. Implementing a novel strategy for interprofessional medication review using collegial mentoring and systematic clinical evaluation in nursing homes (COSMOS). BMC Geriatr. 2019;19:130. https://doi.org/10.1186/s12877-019-1139-6.
Holland R, Battersby J, Harvey I, Lenaghan E, Smith J, Hay L. Systematic review of multidisciplinary interventions in heart failure (structured abstract). Heart. 2005;91:899–906.
Kwak A, Moon YJ, Song Y-K, Yun H-Y, Kim K. Economic impact of pharmacist-participated medication management for elderly patients in nursing homes: a systematic review. Int J Environ Res Public Health. 2019. https://doi.org/10.3390/ijerph16162955.
Wouters H, Foster JM, Ensink A, O’Donnell LK, Zuidema SU, Boersma F, Taxis K. Barriers and facilitators of conducting medication reviews in nursing home residents: a qualitative study. Front Pharmacol. 2019;10:1026. https://doi.org/10.3389/fphar.2019.01026.
Disalvo D, Luckett T, Bennett A, Davidson P, Agar M. Pharmacists’ perspectives on medication reviews for long-term care residents with advanced dementia: a qualitative study. Int J Clin Pharm. 2019;41:950–62. https://doi.org/10.1007/s11096-019-00821-7.
Rose O, Derendorf H, Erzkamp S, Fujita K, Hartl A, Hoti K, et al. Development of clinical pharmacy services in Australia, Austria, Belgium, Bosnia-Herzegovina, Canada, Germany, Japan, Kosovo, Switzerland, the Netherlands, Thailand, USA and correlation with educational standards, level of research, and implementation practices. Int J Clin Pharmacol Ther. 2018;56:518–30. https://doi.org/10.5414/CP203264.
Lee SS, Schwemm AK, Reist J, Cantrell M, Andreski M, Doucette WR, et al. Pharmacists’ and pharmacy students’ ability to identify drug-related problems using TIMER (Tool to Improve Medications in the Elderly via Review). Am J Pharm Educ. 2009;73:52.
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67:674–94. https://doi.org/10.1111/jgs.15767.
Renom-Guiteras A, Meyer G, Thürmann PA. The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol. 2015;71:861–75. https://doi.org/10.1007/s00228-015-1860-9.
Bates I, John C, Bruno A, Fu P, Aliabadi S. An analysis of the global pharmacy workforce capacity. Hum Resour Health. 2016;14:61. https://doi.org/10.1186/s12960-016-0158-z.
Chan ZCY, Tam WS, Lung MKY, Wong WY, Chau CW. A systematic literature review of nurse shortage and the intention to leave. J Nurs Manag. 2013;21:605–13. https://doi.org/10.1111/j.1365-2834.2012.01437.x.
Thompson W, Hogel M, Li Y, Thavorn K, O’Donnell D, McCarthy L, et al. Effect of a proton pump inhibitor deprescribing guideline on drug usage and costs in long-term care. J Am Med Dir Assoc. 2016;17(673):e1-4. https://doi.org/10.1016/j.jamda.2016.04.020.
Erzkamp S, Rose O. Development and evaluation of an algorithm-based tool for medication management in nursing homes: the AMBER study protocol. BMJ Open. 2018;8:e019398. https://doi.org/10.1136/bmjopen-2017-019398.
World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4. https://doi.org/10.1001/jama.2013.281053.
Mayring P. Qualitative Inhaltsanalyse: Grundlagen und Techniken. 12th ed. Weinheim: Beltz; 2015.
Erzkamp S, Köberlein-Neu J, Rose O. A review on relevant aspects of a medication review in nursing homes. 2017. https://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017065002. Accessed 12 June 2017.
Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. https://doi.org/10.1186/1471-2288-7-10.
Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62:1013–20. https://doi.org/10.1016/j.jclinepi.2008.10.009.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. https://doi.org/10.1136/bmj.g1687.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Developing guidance on the conduct of narrative synthesis in systematic reviews. J Epidemiol Community Health. 2005;59(Suppl 1):A7.
Chan A-W, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158:200–7. https://doi.org/10.7326/0003-4819-158-3-201302050-00583.
Chan A-W, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586.
Joos S, Bleidorn J, Haasenritter J, Hummers-Pradier E, Peters-Klimm F, Gagyor I. Manual for the design of non-drug trials in primary care, taking account of good clinical practice (GCP) criteria. Z Evid Fortbild Qual Gesundhwes. 2013;107:87–92. https://doi.org/10.1016/j.zefq.2012.12.019.
Johnston MC, Crilly M, Black C, Prescott GJ, Mercer SW. Defining and measuring multimorbidity: a systematic review of systematic reviews. Eur J Public Health. 2019;29:182–9. https://doi.org/10.1093/eurpub/cky098.
American College of Clinical Pharmacy. Standards of practice for clinical pharmacists. Pharmacotherapy. 2014;34:794–7. https://doi.org/10.1002/phar.1438.
Pharmaceutical Care Network Europe. Classification for drug related problems version 8.01. https://www.pcne.org/upload/files/215_PCNE_classification_V8-01.pdf. Accessed 18 Aug 2016.
Hughes CM, Lapane KL. Pharmacy interventions on prescribing in nursing homes: from evidence to practice. Ther Adv Drug Saf. 2011;2:103–12. https://doi.org/10.1177/2042098611406167.
Thiruchelvam K, Hasan SS, Wong PS, Kairuz T. Residential aged care medication review to improve the quality of medication use: a systematic review. J Am Med Dir Assoc. 2017;18:87.e1-87.e14. https://doi.org/10.1016/j.jamda.2016.10.004.
Chhabra PT, Rattinger GB, Dutcher SK, Hare ME, Zuckerman IH, et al. Medication reconciliation during the transition to and from long-term care settings: a systematic review. Res Soc Admiss Pharm. 2012;8:60–75.
Church J, Goodall S, Norman R, Haas M. An economic evaluation of community and residential aged care falls prevention strategies in NSW. N S W Public Health Bull. 2011;22:60–8. https://doi.org/10.1071/NB10051.
Clegg A, Siddiqi N, Heaven A, Young J, Holt R. Interventions for preventing delirium in older people in institutional long-term care. Cochrane Database Syst Rev. 2014.
da Silva DT, Santos AP, Aguiar PM, da Silva WB, de Lyra DP Jr. Analysis of research quality regarding pharmaceutical intervention in elderly residents of long-term care facilities: a systematic review. J Am Geriatr Soc. 2010;58:1404–6. https://doi.org/10.1111/j.1532-5415.2010.02932.x
Fleming A, Browne J, Byrne S. The effect of interventions to reduce potentially inappropriate antibiotic prescribing in long-term care facilities: a systematic review of randomised controlled trials. Drugs Aging. 2013;30:401–8. https://doi.org/10.1007/s40266-013-0066-z.
Forsetlund L, Eike MC, Gjerberg E, Vist GE. Effect of interventions to reduce potentially inappropriate use of drugs in nursing homes: a systematic review of randomised controlled trials. BMC Geriatr. 2011;11:16. https://doi.org/10.1186/1471-2318-11-16.
Hanlon JT, Lindblad CI, Gray SL. Can clinical pharmacy services have a positive impact on drug-related problems and health outcomes in community-based older adults? Am J Geriatr Pharmacother. 2004;2:3–13. https://doi.org/10.1016/S1543-5946(04)90002-5.
Kroger E, Wilchesky M, Marcotte M, Voyer P, Morin M, Champoux N, et al. Medication use among nursing home residents with severe dementia: identifying categories of appropriateness and elements of a successful intervention. J Am Med Dir Assoc. 2015;16(629):e1-17. https://doi.org/10.1016/j.jamda.2015.04.002.
LaMantia MA, Scheunemann LP, Viera AJ, Busby-Whitehead J, Hanson LC. Interventions to improve transitional care between nursing homes and hospitals: a systematic review. J Am Geriatr Soc. 2010;58:777–82. https://doi.org/10.1111/j.1532-5415.2010.02776.x.
Lehnbom EC, Stewart MJ, Manias E, Westbrook JI. Impact of medication reconciliation and review on clinical outcomes. Ann Pharmacother. 2014;48:1298–312. https://doi.org/10.1177/1060028014543485.
Loganathan M, Singh S, Franklin BD, Bottle A, Majeed A. Interventions to optimise prescribing in care homes: systematic review. Age Ageing. 2011;40:150–62. https://doi.org/10.1093/ageing/afq161.
Marasinghe KM. Computerised clinical decision support systems to improve medication safety in long-term care homes: a systematic review. BMJ Open. 2015;5:e006539. https://doi.org/10.1136/bmjopen-2014-006539.
Marcum ZA, Handler SM, Wright R, Hanlon JT. Interventions to improve suboptimal prescribing in nursing homes: A narrative review. Am J Geriatr Pharmacother. 2010;8:183–200. https://doi.org/10.1016/j.amjopharm.2010.05.004.
Neyens JC, van Haastregt JC, Dijcks BP, Martens M, van den Heuvel WJ, de Witte LP, Schols JM. Effectiveness and implementation aspects of interventions for preventing falls in elderly people in long-term care facilities: a systematic review of RCTs. J Am Med Dir Assoc. 2011;12:410–25. https://doi.org/10.1016/j.jamda.2010.07.018.
Nishtala PS, McLachlan AJ, Bell JS, Chen TF. Psychotropic prescribing in long-term care facilities: impact of medication reviews and educational interventions. Am J Geriatr Psychiatry. 2008;16:621–32. https://doi.org/10.1097/JGP.0b013e31817c6abe.
Oliver D, Connelly JB, Victor CR, Shaw FE, Whitehead A, Genc Y, et al. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2007;334:82. https://doi.org/10.1136/bmj.39049.706493.55.
Parsons C, Alldred D, Daiello L, Hughes C. Prescribing for older people in nursing homes: strategies to improve prescribing and medicines use in nursing homes. Int J Older People Nurs. 2011;6:55–62. https://doi.org/10.1111/j.1748-3743.2010.00263.x.
Phillips JL, West PA, Davidson PM, Agar M. Does case conferencing for people with advanced dementia living in nursing homes improve care outcomes: evidence from an integrative review? Int J Nurs Stud. 2013;50:1122–35. https://doi.org/10.1016/j.ijnurstu.2012.11.001.
Spinewine A, Fialova D, Byrne S. The role of the pharmacist in optimizing pharmacotherapy in older people. Drugs Aging. 2012;29:495–510. https://doi.org/10.2165/11631720-000000000-00000.
Stubbs B, Denkinger MD, Brefka S, Dallmeier D. What works to prevent falls in older adults dwelling in long term care facilities and hospitals? An umbrella review of meta-analyses of randomised controlled trials. Maturitas. 2015;81:335–42. https://doi.org/10.1016/j.maturitas.2015.03.026.
Thompson Coon J, Abbott R, Rogers M, Whear R, Pearson S, Lang I, et al. Interventions to reduce inappropriate prescribing of antipsychotic medications in people with dementia resident in care homes: a systematic review. J Am Med Dir Assoc. 2014;15:706–18. https://doi.org/10.1016/j.jamda.2014.06.012.
Verrue CLR, Petrovic M, Mehuys E, Remon JP, Vander SR. Pharmacists’ interventions for optimization of medication use in nursing homes: a systematic review. Drugs Aging. 2009;26:37–49.
Vu MQ, Weintraub N, Rubenstein LZ. Falls in the nursing home: are they preventable? J Am Med Dir Assoc. 2004;5:401–6. https://doi.org/10.1097/01.JAM.0000144553.45330.AD.
Wallerstedt SM, Kindblom JM, Nylen K, Samuelsson O, Strandell A. Medication reviews for nursing home residents to reduce mortality and hospitalization: systematic review and meta-analysis. Br J Clin Pharmacol. 2014;78:488–97. https://doi.org/10.1111/bcp.12351.
Wilson NM, March LM, Sambrook PN, Hilmer SN. Medication safety in residential aged-care facilities: a perspective. Ther Adv Drug Saf. 2010;1:11–20. https://doi.org/10.1177/2042098610381418.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44:213–8. https://doi.org/10.1093/ageing/afu145.
Halvorsen KH, Ruths S, Granas AG, Viktil KK. Multidisciplinary intervention to identify and resolve drug-related problems in Norwegian nursing homes. Scand J Prim Health Care. 2010;28:82–8. https://doi.org/10.3109/02813431003765455.
Vinks THAM, Egberts TCG, de Lange TM, de Koning FHP. Pharmacist-based medication review reduces potential drug-related problems in the elderly: the SMOG controlled trial. Drugs Aging. 2009;26:123–33. https://doi.org/10.2165/0002512-200926020-00004.
Finkers F, Maring JG, Boersma F, Taxis K. Study of medication reviews to identify drug-related problems of polypharmacy patients in the Dutch nursing home setting. J Clin Pharm Ther. 2007;32:469–76. https://doi.org/10.1111/j.1365-2710.2007.00849.x.
Bitter K, Pehe C, Krüger M, Heuer G, Quinke R, Jaehde U. Pharmacist-led medication reviews for geriatric residents in German long-term care facilities. BMC Geriatr. 2019;19:39. https://doi.org/10.1186/s12877-019-1052-z.
Roberts MS, Stokes JA, King MA, Lynne TA, Purdie DM, Glasziou PP, et al. Outcomes of a randomized controlled trial of a clinical pharmacy intervention in 52 nursing homes. Br J Clin Pharmacol. 2001;51:257–65.
Levenson SA, Saffel DA. The consultant pharmacist and the physician in the nursing home: roles, relationships, and a recipe for success. J Am Med Dir Assoc. 2007;8:55–64. https://doi.org/10.1016/j.jamda.2006.11.002.
Acknowledgements
The AMBER project needs to thank the participating nursing homes, patients, pharmacists, physicians and nurses, without whom it would not have been possible. The authors would like to thank Dr. Sebastian Baum, Dr. Dolf Hage, Dr. Heinz Giesen, Laura Kerschke, M.Sc., Prof. Dr. Hugo Mennemann and Dr. Udo Puteanus for their valuable contributions, and the Apothekerstiftung Westfalen-Lippe for funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The AMBER project was supported by the Apothekerstiftung Westfalen-Lippe. There was no involvement of the funding party in the study and its outcomes.
Conflict of interest
Juliane Koeberlein-Neu, Susanne Erzkamp and Olaf Rose declare that they have no competing interests and received no financial support for the conduct of this study.
Ethics approval
The regional ethics committee of the Medical Association of Westphalia-Lippe and the University of Muenster approved the study (registration number 2017-350-f-S). The study was registered at the German Clinical Trials Register (DRKS-ID: DRKS00010995).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
All authors consent to publication of this paper.
Availability of data and material (data transparency)
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics
The study was registered in the German Clinical Trials Register (DRKS-ID: DRKS00010995, August 23, 2017). The review was registered in the International Prospective Register of Systematic Reviews (PROSPERO, registration number CRD42017065002, May 5, 2017). Ethics approval by the Medical Association of Westphalia-Lippe and the University of Muenster (registration number 2017-350-f-S). The study protocol was published previously (Erzkamp S, Rose O. Development and evaluation of an algorithm-based tool for Medication Management in nursing homes: The AMBER study protocol. BMJ Open 2018;8(4):e019398).
Author contributions
SE and OR initiated the project; SE, JKN and OR were responsible for design and methodology; SE carried out the interviews, systematic reviews and Delphi survey with support from OR where needed; OR took the lead in writing the manuscript; all authors read, discussed and approved the manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
40264_2020_1016_MOESM1_ESM.pdf
Supplementary file 1: Questionnaires. Supplementary file 2: PRISMA-P checklist. Supplementary file 3: Search strategies. Supplementary file 4: Baselines of the interviewees and results of the interviews. Supplementary file 5: Summarized results of the interventional studies (systematic review step 2). Supplementary file 6: Indications and number of studies on non-interventional records (systematic review step 3) (PDF 2242 kb)
Rights and permissions
About this article
Cite this article
Erzkamp, S., Köberlein-Neu, J. & Rose, O. An Algorithm for Comprehensive Medication Management in Nursing Homes: Results of the AMBER Project. Drug Saf 44, 313–325 (2021). https://doi.org/10.1007/s40264-020-01016-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-020-01016-0