Abstract
Introduction
Fasiglifam (TAK-875) is a G protein-coupled receptor 40 agonist that was being investigated for treatment of type 2 diabetes mellitus (T2DM). A development program was terminated late in phase III clinical trials due to liver safety concerns.
Methods
The liver safety of fasiglifam was assessed from data based on six phase II and nine phase III double-blind studies and two open-label studies with emphasis on pooled data from 15 double-blind studies from both global and Japanese development programs. Taking into consideration different daily doses of fasiglifam administered in clinical studies, the primary comparisons were between all patients exposed to fasiglifam (any dose) versus placebo, and, where applicable, versus the two active comparators, sitagliptin or glimepiride. A Liver Safety Evaluation Committee consisting of hepatologists blinded to treatment assignments evaluated hepatic adverse events (AEs) and serious AEs (SAEs) for causal relationship to study drug.
Results
The analysis included data from 9139 patients with T2DM in 15 double-blind controlled studies who received either fasiglifam (n = 5359, fasiglifam group), fasiglifam and sitagliptin (n = 123), or a comparator agent (n = 3657, non-exposed group consisting of placebo and other antidiabetic agents). Exposure to treatment for more than 1 year ranged from 249 patients in the placebo arm, to 370 patients in the glimepiride arm and 617 patients in the fasiglifam 50 mg arm. The primary focus of the analysis was on the hepatic safety of fasiglifam. The overall safety profile based on treatment-emergent AEs (TEAEs), SAEs, deaths, and withdrawal due to AEs was similar between fasiglifam and placebo (excluding liver test abnormalities). However, there was an increased incidence rate of serum alanine aminotransferase (ALT) elevations > 3 × upper limit of normal (ULN), 5 × ULN, and 10 × ULN in fasiglifam-treated patients compared with those treated with placebo or active comparators. ALT elevations > 3 × ULN for fasiglifam were 2.7% compared with 0.8 and 0.5% for the active comparators and placebo. There did not appear to be a clear dose response in incidence of ALT elevations between patients receiving 25 or 50 mg daily. The cumulative incidence of elevations in serum ALT > 3 × ULN was higher in the first 6 months of treatment with fasiglifam compared with both placebo and the active comparators, but the rate of new ALT elevations appeared to be similar across all treatment groups thereafter. No demographic or baseline patient characteristics were identified to predict elevations exceeding ALT > 3 × ULN in fasiglifam-treated patients. The pattern of liver injury with fasiglifam was hepatocellular, and there were no reports of liver-related deaths, liver failure or life-threatening liver injury. Most fasiglifam-associated ALT elevations were asymptomatic and resolved promptly upon discontinuing treatment, but in two patients the recovery was prolonged. Importantly, three important serious liver injury cases were identified among fasiglifam-treated patients; one case was adjudicated to be a clear Hy’s Law case and the two remaining cases were considered to closely approximate Hy’s Law cases.
Conclusions
Although the incidence of overall AEs, SAEs, and deaths was similar between fasiglifam and placebo, a liver signal was identified based primarily on the difference in liver chemistry values in the fasiglifam group compared with the placebo and active comparator groups. Three serious liver injuries were attributed to fasiglifam treatment. Clinical development of fasiglifam was halted due to these liver safety concerns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The incidence of alanine aminotransferase (ALT) elevations was substantially higher in fasiglifam compared with placebo and the active comparators, identifying a liver signal |
One definite Hy’s Law and two ‘near’ Hy’s Law cases were identified in fasiglifam-treated patients |
The combination of imbalance in ALT elevations with Hy’s Law cases led to the termination of the fasiglifam clinical program in late phase III development |
1 Introduction
Fasiglifam (TAK-875), a potent and highly selective agonist of G protein-coupled receptor 40 (GPR40), was developed as an adjunct to diet and exercise to improve glycemic control. GPR40 is expressed on pancreatic islet cells [1]. It is activated by long-chain free fatty acids, and consequently stimulates pancreatic β-cells to secrete insulin [2, 3] via a glucose-dependent mechanism [4, 5]. This underlying mechanism might explain the low incidence of hypoglycemia reported in previous studies evaluating fasiglifam in healthy subjects and in patients with type 2 diabetes mellitus (T2DM) [6,7,8,9,10].
As part of the clinical development program, the efficacy and safety of fasiglifam versus glimepiride or placebo were evaluated in a 12-week, phase II study in patients with T2DM from the US or Latin America [8]. In this study, fasiglifam demonstrated statistically significant improvements in glycemic control (glycosylated hemoglobin [HbA1c] levels) and fasting plasma glucose (FPG) compared with placebo. HbA1c reductions of > 1.0% were achieved with fasiglifam doses of ≥ 50 mg, which were comparable with those observed with glimepiride 4 mg. Similar results were also observed in a 52-week, phase III study of fasiglifam 25 or 50 mg as monotherapy, or in combination with basal antidiabetic therapy in Japanese patients [10]. In this study, HbA1c levels decreased from week 2 and this was maintained until the end of the 52-week period; however, the primary objective of this study was safety.
Preclinical studies revealed crystallization of TAK-875 and its primary metabolite TAK-875-glucuronide in the biliary tract of dogs observed in 9-month repeat-dose studies in dogs with 150 mg/kg TAK-875 [11]. Based on the preclinical studies demonstrating hepatotoxicity in dogs, a comprehensive liver safety monitoring plan was developed and put in place prior to the start of the global phase III studies. Although fasiglifam was generally well-tolerated in healthy subjects and patients with T2DM [8, 10, 12, 13], concerns about hepatotoxicity arose from additional global phase III studies and resulted in the decision to terminate the fasiglifam clinical development program. This article summarizes the safety findings from pooled safety data of several phase II and III studies focusing on liver safety findings. At the time clinical development was halted, a total of nine studies (four phase II and five phase III) had been completed. The complete set of studies that are included in the present discussion are summarized in electronic supplementary Table 1.
2 Methods
The analysis includes data from 9139 patients with T2DM in 15 double-blind controlled studies who received either fasiglifam (n = 5359, fasiglifam group), fasiglifam and sitagliptin (n = 123) or a comparator agent (n = 3657, non-exposed group consisting of placebo and other antidiabetic agents). The studies were double-blind, randomized, controlled trials conducted by the sponsor that included patients treated with fasiglifam between 1 day and 2.5 years. These 15 controlled studies included both a separate Japanese clinical development program (n = 4) and a global clinical program (n = 11). The studies assessed fasiglifam versus a comparator, taken as monotherapy, or as initial combination therapy with glimepiride or sitagliptin. Primary assessment was based on overall safety data and analysis of adverse events (AEs) and AEs of special interest (AESIs) based on standardized Medical Dictionary for Regulatory Activities (MedDRA) queries (SMQs), including hepatic and cardiovascular events and liver-related laboratory assessments. The primary comparisons were between all subjects exposed to fasiglifam alone versus placebo. Comparisons with the two active comparators—sitagliptin and glimepiride—were also made when possible. The analyses were primarily descriptive. The risk difference, along with its 95% confidence interval (CI), was also obtained for each markedly abnormal criterion for liver tests, as well as hepatic AEs. Additional analyses of liver safety, including assessments of type/pattern of injury pattern, severity, cumulative occurrence, and prevalence pattern over time, subgroup analyses (region, body mass index [BMI], race, duration of diabetes, responder status) and risk factors, including concomitant medications, for liver safety were also performed. Concomitant medications for inclusion in the model were identified by review of all concomitant medications with likelihood to cause liver injury based on the LIVERTOX® database (http://www.livertox.nih.gov). A logistic regression model was used to assess if certain factors predicted liver test elevation, specifically alanine aminotransferase (ALT) > 3 × upper limit of normal (ULN). In addition, a Liver Safety Evaluation Committee (LSEC) consisting of external hepatologists blinded to treatment assignments for controlled studies reviewed and adjudicated all serious liver-related AEs, potential cases of biochemical Hy’s Law [ALT or aspartate aminotransferase (AST) > 3 × ULN and total bilirubin (TBIL) > 2 × ULN], and cases with other significant liver enzyme abnormalities to assess causal relationship to study drug. Cases with significant liver enzyme abnormalities were defined in two ways. These include patients who met the protocol criteria for discontinuation of study medication based on the US FDA drug-induced liver injury guidance [14] and patients with an ALT or AST > 5 × ULN in whom the study medication was discontinued but did not meet protocol criteria for discontinuation. The LSEC adjudicated cases from both controlled studies and the Japanese open-label studies, and results are included for all cases adjudicated. The LSEC used the structured adjudication process as developed by the Drug-Induced Liver Injury Network [15]. The pattern of liver injury was assessed for each case using the R value [16], which is defined as follows: hepatocellular pattern: R = ALT > 3 × ULN and (ALT/ULN)/(ALP/ULN) ≥ 5; cholestatic pattern: R = ALP > 2 × ULN and (ALT/ULN)/(ALP/ULN) ≤ 2; and mixed pattern: R = ALT > 3 × ULN and ALP > 2 × ULN and (ALT/ULN)/(ALP/ULN) > 2 to < 5, where ALP refers to alkaline phosphatase.
All the above analyses were intended to address the liver safety of fasiglifam using currently recommended methodology [17, 18]. As part of this objective, the analysis attempted to address the following questions. Are there any Hy’s Law cases in the dataset? How are changes across different liver tests correlated, and how do those correlations differ between treatment groups? What is the time-dependent incidence of elevations of liver tests in the active treatment and comparator arms? Is there a ‘window of susceptibility’ in the active treatment arm? Are shifts from baseline different between treatment groups? Is there any evidence for a dose–response relationship? What do time profiles of individual liver tests or liver test panels look like? Are liver test changes observed during treatment transient or progressing while a patient is receiving treatment? What do time profiles look like after treatment is stopped? How does the intake of certain concomitant medications, or occurrence and/or resolution of certain AEs, relate to time profiles of liver tests? Are liver test elevations correlated with the desired therapeutic effect of the drug? Are liver test elevations associated with non-liver side effects or laboratory abnormalities? Are liver test elevations associated with pharmacokinetic parameters of the drug (if available)? To systematically address these questions, a set of standard graph templates were used and customized as required [14].
3 Results
3.1 Treatment Exposure
Table 1 summarizes the treatment breakdown across individual double-blind controlled studies. The majority of patients were in the placebo arm and the fasiglifam 25 and 50 mg arms. As noted from Table 1, certain doses were only administered in some studies. While the primary comparison will be on subjects exposed to fasiglifam versus those who were not, the focus of the safety discussion will be on the fasiglifam 25 and 50 mg doses, which were the intended doses to be marketed. Compared with placebo and fasiglifam, fewer patients were exposed to the active comparators sitagliptin and glimepiride.
The status of each study regarding completion is highlighted in electronic supplementary Fig. 1. Most of the global phase III studies were terminated before completion, whereas all the Japanese studies were completed as the clinical development program in Japan was ahead of the global clinical program. Note that the figure also includes two open-label studies (OCT-002 and OCT-003) that are not included in the pooled analysis.
Information on drug exposure, including duration of exposure and cumulative exposure in days, was generated (electronic supplementary Table 2). Due to the different study durations of the studies included in the pool of studies in the analysis and as a result of the termination of the development program, some subjects did not fully undergo all the planned study procedures. Median exposure time ranged from 170 days in the placebo arm, to 296 days in the glimepiride arm, with the median times for the other treatment arms falling in between these two extremes. Exposure to treatment for more than 1 year ranged from 249 patients in the placebo arm, to 370 patients in the glimepiride arm and 617 patients in the fasiglifam 50 mg arm.
3.2 Demographics and Baseline Characteristics
Electronic supplementary Table 3 shows a summary of the baseline demographics and baseline characteristics for patients. Some of the baseline characteristics, such as age and BMI, appeared to have higher values in the placebo arm compared with other treatments, although there were no major differences. Overall, the baseline demographics and baseline characteristics for patients are comparable across treatment groups.
3.3 Overall Safety
Overall, there were no notable differences across the cohorts in all treatment-emergent AEs (TEAEs), AEs leading to study drug withdrawal, SAEs, treatment-related AEs (TRAEs), and serious TRAEs (electronic supplementary Table 4), and there was no definitive dose–response pattern in the various considerations in the overview of AEs. There were some characteristics of the rates where the 50 mg dose exceeded that of the 25 mg dose and that of placebo, such as in the TEAEs and TRAEs leading to discontinuation. Relative to the active comparators, glimepiride had higher rates of TEAEs relative to both doses of fasiglifam as well as placebo. A slightly lower incidence of TEAEs overall was noted in the sitagliptin arm. None of the differences were statistically significant. Given the notable sample size differences across different treatment groups, these results should be interpreted with caution. There were 50 deaths (25 in the fasiglifam arm, 19 in the placebo arm, and 6 in the comparator arm), however none of the deaths were assessed as being related to liver safety.
3.4 Liver Safety: Analysis Based on Adverse Events
3.4.1 Risk Difference Plot for Hepatic Standardized MedDRA Query
Electronic supplementary Fig. 2 shows the risk plot of the hepatic AEs based on the hepatic SMQ. The risk difference between fasiglifam and both placebo and active comparators, along with its 95% CI, are presented for each AE. The left panel presents the observed number of subjects with the AE within the SMQ, along with the percentages of the total number of subjects (presented at the top) for each AE and for treatment. The middle and right panels show the 95% CIs and the point estimate for the difference comparing fasiglifam versus placebo (middle panel) and fasiglifam versus the active comparator (right panel). If the dot falls on the right of the dotted vertical line (representing no difference), then this suggests more events in fasiglifam than placebo or the active comparator (depending on the panel). CIs that include zero suggest that there is no difference at the 95% confidence level. From the middle panel, all AEs in the SMQ were higher in fasiglifam compared with placebo, other than for liver disorders, hepatic steatosis, and blood bilirubin increased. From the right panel, all AEs were the same in fasiglifam compared with the active comparator, other than for hepatic enzyme increased and hepatic function abnormal, which were higher in fasiglifam.
3.5 Liver Safety: Analysis Based on Laboratory Data
3.5.1 Evaluation of Drug-Induced Serious Hepatotoxicity (eDISH) Analysis
Figure 1 shows the evaluation of drug-induced serious hepatotoxicity (eDISH) plot for fasiglifam treatment and the comparator groups (placebo and active) based on the central laboratory data. The eDISH plot reveals that some patients in each treatment arm appear in the right upper quadrant of the eDISH plot (‘Hy’s Law quadrant’) and therefore experienced elevations in serum ALT > 3 × ULN and total serum bilirubin (TBIL) > 2 × ULN (although not necessarily at the same time). There are six potential Hy’s Law cases in fasiglifam-treated patients. Additionally, three patients all receiving fasiglifam are not included in this eDISH plot as they were patients identified from the Japanese open-label studies.
One additional fasiglifam-treated patient not represented in the eDISH plot who experienced a rise in TBIL > 2 × ULN would also qualify as a potential Hy’s Law case based on peak elevation of AST > 3 × ULN, but not ALT. In this case of a patient with obstructive jaundice, the event was adjudicated by the LSEC as being excluded.
The full laboratory and clinical data from all potential Hy’s Law cases were submitted to the LSEC for adjudication. Following adjudication, one fasiglifam case was considered to be a clear Hy’s Law case and two additional fasiglifam cases were considered to nearly meet the criteria for a Hy’s Law case. Two additional cases of concern were those in whom recovery from liver enzyme elevations was prolonged. Details of these five cases are presented later (see Sect. 3.6.5).
For the six fasiglifam-treated patients represented in the eDISH plot, the LSEC adjudicated three cases as excluded, two cases as unlikely, and one case as highly likely (see Case 1, Sect. 3.6.5). For the three cases adjudicated as excluded, diagnoses included biliary tract disease with partial duct obstruction later confirmed as pancreatic carcinoma, choledocolithiasis, and biliary tract disease with cholecystitis. For the two cases adjudicated as unlikely, the diagnoses included biliary tract disease with gallstones, and activation of chronic hepatitis b infection.
The one placebo patient in the eDISH plot had cholelithiasis, choledocholithiasis, and gallstone pancreatitis, and was adjudicated as unlikely. There were two active comparator cases in the eDISH plot. One active comparator patient had choledocholithiasis adjudicated as unlikely, while the second active comparator case was adjudicated as possible in a patient with manifestations of alcohol injury. For the three patients identified in the Japanese open-label studies not included in the eDISH plot, two of the cases were adjudicated as unlikely as a result of symptomatic cholelithiasis, while the third case in a patient with chronic hepatitis b infection and a history of gallstones was adjudicated as possible.
3.5.2 Severity of Liver Events
Electronic supplementary Fig. 3 shows the risk plot of the key liver safety-related laboratory parameters. The risk difference between fasiglifam and both placebo and active comparators, along with its 95% CI, are presented for each abnormal criterion. In general, a higher proportion of patients in the fasiglifam arm tended to experience liver test elevations at various thresholds compared with placebo or the comparator. For ALT > 3 × ULN, the ALT elevations for fasiglifam were 2.7%, compared with 0.8% and 0.5% for the active comparator and placebo, respectively. A similar trend was noted for AST. Compared with placebo or the comparator, ALT > 5 × ULN and > 10 × ULN elevations were much higher in the fasiglifam arm; the same pattern was noted for AST.
Table 2 shows liver test elevations for the fasiglifam 25 and 50 mg doses compared with placebo and comparators. The incidence of ALT elevations > 3 × ULN, > 5 × ULN, and > 10 × ULN were similar between the fasiglifam 25 and 50 mg doses. ALT elevations > 5 × ULN and > 10 × ULN were reported in 1.0 and 0.4% of patients treated with fasiglifam 25 mg, compared with 1.3 and 0.6% of patients treated with the fasiglifam 50 mg dose, respectively. The incidence of ALT > 3 × ULN and TBIL > 2 × ULN was < 0.1, 0.1, and 0.2% for placebo, fasiglifam, and active comparators, respectively. Including the additional three cases from the Japanese open-label studies increased the incidence of ALT > 3 × ULN and TBIL > 2 × ULN in fasiglifam-treated patients to 0.2%.
3.5.3 Timing of Hepatic Events
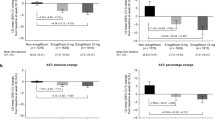
Figure 2 shows the Kaplan–Meier plot for time to ALT > 3 × ALT. The Kaplan–Meier plot was purposely truncated at 0.060 on the y axis to magnify and clearly discern the patterns in the plot. As can be seen from the y axis, the differences in the probabilities are small. The Kaplan–Meir plot shows an increased incidence in the fasiglifam arms for time-to-first-occurrence of ALT > 3 × ULN compared with placebo and active comparators (log-rank test, p < 0.0001). Most of the events in the fasiglifam treatment arms appear to occur in the first 6 months; the rate of new events then appears to fall to approximately that observed in the comparator groups. The graphical appearance of the Kaplan–Meier plot in terms of the slope is steeper between 90 and 180 days compared with the previous period of 0–90 days, while taking into account differences in the number of patients exposed in the two periods (see electronic supplementary Table 2). In addition, although the 50 mg dose appears to show higher event rates than the 25 mg dose, the two plots cross at approximately 450 days, and the log-rank test comparing 50 versus 25 mg was not significant at the 5% level.
3.5.4 Shifts in Laboratory Parameters
The shift plot suggests a more pronounced shift for ALT values from baseline to peak ALT for fasiglifam compared with placebo or active comparators (Fig. 3). Similar results are shown in electronic supplementary Figs. 4a and b.
3.6 Additional Analyses
3.6.1 Severity of Liver Injury
Serious liver injury was defined as any of one of the following categories: ALT > 8 × ULN, ALT > 3 × ULN, and TBIL > 2 × ULN, or hospitalization for the liver injury, and death or liver transplant (Table 3). There were no deaths or liver transplants, and no difference was noted in hospitalizations for liver injury between the treatment groups.
3.6.2 Type/Pattern of Injury
Based on the R value, the primary pattern of liver injury was hepatocellular for fasiglifam and the active comparators (Table 4). The rate of hepatocellular injury was substantially higher with fasiglifam than in either the placebo or active comparator arms. For fasiglifam, the rate of hepatocellular injury was slightly higher in the 50 mg dose group (2.3%) compared with the 25 mg dose group (1.8%).
3.6.3 Liver Safety Evaluation Committee Adjudication
A summary of LSEC adjudication findings prior to unblinding the treatment assignments is presented in Table 5. The predefined criteria used by the LSEC to determine adjudication of any case is included in the Methods section. Most of the adjudicated cases were classified as possibly or probably related to study drug. The number of cases assessed as probably due to study drug, and the percentage of the total treated cohort they represented, was higher among the fasiglifam-treated subjects compared with the placebo or active comparator arms. One case (Case 1), was adjudicated as ‘highly likely’ and was deemed a clear Hy’s Law case. Two additional cases experienced qualifying serum ALT elevations, and the elevations in TBIL approached, but did not, exceed 2 × ULN; one was adjudicated as probably related to study drug and the other was adjudicated as possibly related to study drug (Cases 2 and 3; see Sect. 3.6.5). These two cases were classified by the LSEC as nearly qualifying for designation as Hy’s Law cases. Three additional cases met the criteria of ALT > 3 × ULN and TBIL > 2 × ULN, only by local laboratory data. Two of these cases were adjudicated as not related to study drug, and one case was adjudicated as unlikely to be related to study drug. In all three cases, there was evidence of symptomatic cholelithiasis and/or choledocholithiasis, and one of the patients also had an additional diagnosis of gallstone pancreatitis. These cases were therefore not considered to be Hy’s Law cases and were not presented further.
3.6.4 Subgroup Analyses and Liver Safety Predictors
The subgroup analyses did not reveal any differences in liver safety test elevations among various demographic and baseline characteristics. Additionally, none of the variables in the logistic regression analysis appeared to be significant in predicting ALT > 3 × ULN elevation other than treatment with fasiglifam. There were no demographic or baseline patient characteristics identified or concomitant medications (defined in the Sect. 2) to predict the risk of hepatic AEs in fasiglifam-treated patients (Fig. 4).
3.6.5 Cases Leading to Development Termination
Further information is now presented on the clear Hy’s Law case (Case 1), the ‘near’ Hy’s Law cases (Cases 2 and 3), and two cases with a long time to recovery of ALT (Cases 4 and 5). A summary of the important characteristics for each one of these subjects is presented below and with graphic depiction on the serial liver chemistries (Fig. 5a–e).
Time profiles of ALT, AST, ALP, TBIL, HbA1c, and adverse events, panel by patient cases, treatment end indicated by horizontal green line, start and end dates of adverse events indicated by horizontal gray line, liver test ULN indicated by left vertical axis, and HbA1c percentage indicated by right vertical axis, respectively. Color coding by liver test and HbA1c. ALT alanine aminotransferase, AST aspartate aminotransferase, ALP alkaline phosphatase, TBIL total bilirubin, ULN upper limit of normal, HbA1c glycosylated hemoglobin, SAE serious adverse event, GGT γ-glutamyltransferase
3.6.5.1 Case 1/307: Hy’s Law Case
This was a 42-year-old man with a relevant medical history of T2DM. The patient’s AST, TBIL, and ALP levels were within normal limits at both screening and baseline. His ALT was modestly elevated at both of these times (Fig. 5a). At study visit 8 (day 57), the patient experienced a marked elevation in serum ALT (> 30 × ULN), AST (> 15 × ULN), and a rise in TBIL (< 2 × ULN). An AE of ‘hepatitis acute’ with the symptom of dark urine was reported. The event was subsequently upgraded to an SAE. Study drug was interrupted on day 59 due to the event. On day 62, the patient’s ALT and AST levels had decreased slightly, but the TBIL level had increased to > 2 × ULN. The serum ALT, AST, and TBIL levels returned to within normal limits by day 120.
Tests for acute viral hepatitis (anti-hepatitis A virus [HAV] immunoglobulin [Ig] M, anti-hepatitis B core [HBc] IgM, hepatitis B surface antigen [HBsAg], hepatitis B e-antigen [HBeAg], anti-hepatitis C virus [HCV], cytomegalovirus [CMV] IgM, hepatitis E virus [HEV] IgM, and Epstein–Barr virus viral capsid antigen [EBV VCA] IgM) on day 99 were negative, as were the results of tests for autoimmune hepatitis (antinuclear antibody [ANA], anti-smooth muscle antibody [ASMA], and anti-liver/kidney microsome [anti-LKM]). Abdominal ultrasound examinations on days 101 and 122 revealed only fatty liver. No concomitant medication use was reported, including no use of herbal supplements. The consensus causality assessment by the LSEC was that a causal role for fasiglifam was highly likely (75–95% likelihood).
3.6.5.2 Case 2/304: ‘Near’ Hy’s Law Case
This was a 75-year-old man with a relevant medical history of essential hypertension, hypertensive cardiomyopathy, myocardial ischemia, dyslipidemia, osteoarthritis, obesity, and T2DM. The patient’s AST, ALT, ALP, and TBIL levels were within normal limits at both screening and baseline (Fig. 5b). On day 146, the serum ALT transiently rose to > 3 × ULN, and the TBIL and ALP levels remained within normal limits. On day 187, the ALT level had increased to > 15 × ULN and the TBIL had increased to 2.3 mg/dl (1.9 × ULN), which was the peak value obtained. The serum ALP (2.2 × ULN) and γ-glutamyltransferase (GGT; 401 U/L [> 8 × ULN]) were also elevated at this time. An AE of ‘hepatitis B’ was reported on day 187, and study drug was discontinued permanently on day 189. All liver enzyme levels returned to within normal limits on day 253, approximately 2 months after the peak ALT, AST, ALP, and GGT were observed.
The results of tests for acute viral hepatitis (anti-HAV IgM, anti-HBc IgM, HBsAg, anti-HCV, CMV IgM, HEV IgM, and EBV VCA IgM) on day 194 were negative, as were the results of tests for autoimmune hepatitis (ANA, ASMA, and anti-LKM). Additional tests for hepatitis B (anti-HBc total and anti-HBs) were positive, consistent with a resolved prior, but not acute, hepatitis B infection. An abdominal ultrasound performed on day 194 was reported as normal.
Concomitant medications at the time of the liver enzyme elevations were indapamide, nebivolol hydrochloride, perindopril, metformin, atorvastatin, fenofibrate, dutasteride, and tamsulosin. None of these medications were discontinued as a result of the liver test elevations. The consensus causality assessment by the LSEC was that a causal role for fasiglifam was probable (50–74% likelihood). Drug-induced liver injury was probable due to consistent latency, but the double peak is atypical. In view of the rise in serum ALP exceeding 2 × ULN, and the peak TBIL not exceeding 1.9 × ULN, this event was not considered a clear Hy’s Law case but a ‘near’ Hy’s Law case.
3.6.5.3 Case 3/306: ‘Near’ Hy’s Law Case
This was a 60-year-old man with a relevant medical history of arthropathy, carpal tunnel decompression, osteoarthritis, hypertension, diabetic neuropathy, intermittent claudication, and T2DM. The patient had no history of alcohol use. The patient’s AST, ALT, ALP, and TBIL levels were within normal limits at both screening and baseline (Fig. 5c). On day 29, the serum ALT rose to > 20 × ULN, which was reported as a non-serious AE of ‘transaminases increased’. ALP (278 U/L [1.9 × ULN]) and peak serum TBIL (1.9 mg/dl [1.6 × ULN]) levels were also recorded at this time. Study drug was discontinued permanently on day 32. AST and TBIL levels returned to within normal limits on day 34, and ALT and ALP levels returned to within normal limits on day 43.
Concomitant medications at the time of the liver enzyme elevations were diclofenac, glibenclamide, losartan, cilostazol, and metformin. None of these medications were discontinued as a result of the liver test elevations.
Viral hepatitis serology, autoimmune hepatitis serology, and abdominal ultrasound were not performed at the time of the peak liver test elevations. On day 64, tests for acute viral hepatitis (anti-HAV IgM, anti-HBc IgM, HBsAg, anti-HCV, CMV IgM, HEV IgM, and EBV VCA IgM) were negative, as were the results of tests for autoimmune hepatitis (ANA, ASMA, and anti-LKM). An abdominal ultrasound performed on day 34 revealed only liver steatosis. The consensus causality assessment by the LSEC was that a causal role for fasiglifam was possible (25–49% likelihood); however, at the time of blinded adjudication by the LSEC, the results of viral studies, autoimmune antibodies, and the ultrasound were not available and for this reason the case was not scored higher (probable). The case was considered a ‘near’ Hy’s Law case with a TBIL of 1.9 mg/dl.
3.6.5.4 Case 4/306: Prolonged Recovery from the Event
This was a 57-year-old woman with a relevant medical history of hyperlipidemia, hypertension, osteoarthritis, and T2DM. The patient’s ALT, AST, ALP, and TBIL levels were within normal limits at both screening and baseline (Fig. 5d). On day 91, the patient experienced a rise in serum ALT [> 3 × ULN), which was reported as a non-serious AE of ‘liver function test abnormal’; the ALP and TBIL levels remained within normal limits. The ALT level had further increased to 12 × ULN by day 111; the ALP (< 2 × ULN) and GGT (> 3 × ULN) levels were also elevated, but the TBIL level remained within normal limits. Study drug was discontinued permanently on day 113 due to these liver enzyme elevations. An associated AE of abdominal pain was reported on day 114. The event of ‘liver function abnormal’ ended on day 230 and the event was considered resolved. The results of tests for acute viral hepatitis (anti-HAV IgM, anti-HBc IgM, HBsAg, anti-HCV, CMV IgM, HEV IgM, and EBV VCA IgM) on day 124 were negative.
Concomitant medications at the time of the liver enzyme elevations were gabapentin, glimepiride, hydrochlorothiazide, lisinopril, metformin, pravastatin and meloxicam. All of these medications, except for lisinopril, were stopped on day 114 due to these AEs. The consensus causality assessment by the LSEC was that a causal role for fasiglifam was probable (50–74% likelihood).
3.6.5.5 Case 5/306: Prolonged Recovery from the Event
This was a 79-year-old woman with a relevant medical history of hypothyroidism, diabetic retinopathy, dyslipidemia, hypertension, osteoarthritis, chronic obstructive pulmonary disease, and T2DM. The patient’s ALT, AST and TBIL levels were within normal limits at both screening and baseline (Fig. 5e). On day 92, the serum was noted to be > 5 × ULN and was reported as a non-serious AE of ‘transaminases increased’. At this time, the ALP level was also elevated (< 2 × ULN), but the TBIL level remained within normal limits. Study drug was discontinued on day 94 due to the liver enzyme elevations. However, the serum ALT level had increased further to > 10 × ULN on day 115. The AE ended on day 188 and was considered resolved. The results of tests for acute viral hepatitis (anti-HAV IgM, anti-HBc IgM, HBsAg, anti-HCV, CMV IgM, HEV IgM, and EBV VCA IgM) on day 101 were negative, as were the results of tests for autoimmune hepatitis (ANA, ASMA, and anti-LKM). An abdominal ultrasound performed on day 111 was reported as normal.
Concomitant medications at the time of the liver enzyme elevations were metformin, metoprolol, levothyroxine, ramipril, and a combination product containing fluticasone/salmeterol (inhaled). None of these medications were discontinued as a result of the liver enzyme elevations. The consensus causality assessment by the LSEC was that a causal role for fasiglifam was probable (50–74% likelihood). Drug-induced liver injury was also probable due to compatible latency, positive dechallenge, and the absence of confounders.
4 Discussion
In this integrated pooled analysis, we investigated the liver safety of fasiglifam, focusing primarily on aggregate data obtained in the fasiglifam double-blind controlled clinical trials. Overall, no differences were noted in the demographics and the baseline characteristics between fasiglifam, placebo, and active comparators.
There were also no differences across the treatment groups in the incidence of liver-related AEs not directly related to elevations in serum liver enzymes, including no difference between treatment groups in liver-related hospitalizations. In addition, there were no liver-related deaths or liver transplants in any of the treatment groups; however, there was a higher proportion of subjects in the fasiglifam arm who experienced elevations in serum aminotransferases at various thresholds compared with the placebo or active comparator arms. The primary pattern of the liver enzyme abnormalities was hepatocellular, both in the fasiglifam-treated patients and the patients receiving comparator treatments.
On the eDISH plot, the imbalance in the incidence of serum ALT elevations > 3 × ULN between fasiglifam treatment and the comparators was evident (Temple’s Corollary quadrant). Moreover, a greater number of subjects treated with fasiglifam experienced elevations in serum ALT > 3 × ULN and TBIL > 2 × ULN relative to the other treatments (Hy’s Law quadrant); however, the percentage of fasiglifam-treated subjects in this quadrant was similar to that observed in the placebo- or comparator-treated cohorts. When the clinical and laboratory data from each of the subjects experiencing elevations in serum ALT > 3 × ULN and TBIL > 2 × ULN were adjudicated by the LSEC (blinded to treatment assignments), one subject was considered to be a clear Hy’s Law case and two additional subjects were considered as ‘near’ Hy’s Law cases. After unblinding the treatment assignments, all three cases were determined to have received fasiglifam and none had been randomized to a comparator arm. It should be noted that one of the ‘near’ Hy’s Law cases was not considered to be a clear case because the ALP rose to > 2 × ULN (suggesting a component of cholestasis), which is an exclusion criteria for a Hy’s Law case, as stated in the 2009 FDA draft guidance [14]. However, the liver injury in this patient was hepatocellular according to the R value and probably would be considered a true Hy’s Law case at the time of this writing. The other ‘near’ Hy’s Law case had lacked the viral and autoimmune serologies at the time of the blinded adjudication and this was the basis for assessment as possibly, not probably, related to study drug. In view of the subsequently received report that these studies were negative, it seems likely that this case would also be considered equivalent to a Hy’s Law case since the TBIL almost rose to 2 × ULN. It is important that no Hy’s Law cases or ‘near’ Hy’s Law cases were observed in the other treatment groups.
Additional selected liver events were adjudicated by the LSEC, who were blinded to treatment, with most of these cases being classified as possible or probable. After unblinding the treatment assignments, more cases were judged as probably or possibly related to study drug among the fasiglifam-treated subjects compared with the other treatment arms. Cases considered probably related to fasiglifam included two events where the serum bilirubin remained within normal limits but there was a prolonged recovery after discontinuing treatment (Cases 4 and 5) (Fig. 5a–e). After unblinding, both of these patients were found to have received fasiglifam treatment.
A graph of time-to-first-occurrence of elevations in serum ALT > 3 × ULN (Fig. 2) revealed a time-dependent increase in incidence in the fasiglifam-treated subjects compared with the placebo and active comparator arms. Most of these events occurred during the first 6 months of treatment with fasiglifam, at which point the incidence of first-time elevations of serum ALT appeared to level off and approximate the incidence observed in the comparators. Such a 6-month ‘window of susceptibility’ is observed with other drugs that cause potentially serious liver injury [19]. The slope of the Kaplan–Meier plot for fasiglifam is also steeper between 90 and 180 days than in the previous 90-day period, which suggests that the risk peaked in this time interval prior to falling off.
The data used in the pooled analysis included data from Japanese- and US-sponsored double-blind controlled studies only. Not included in our analysis were data from open-label studies from a separate development program conducted in Japan to support a Japanese submission.
In a phase III, placebo-controlled study of fasiglifam in Japanese patients with T2DM also included in the pooled analysis, in which 67, 63, and 62 patients were randomized to placebo, fasiglifam 25 mg, and fasiglifam 50 mg, respectively, the incidence of ALT ≥ 3 × ULN was higher in the fasiglifam 25 and 50 mg groups (4.8% and 6.5%, respectively) compared with placebo (1.5%), while the incidence of ALT ≥ 5 × ULN was reported to be similar among all treatment groups (1.6% in the fasiglifam 25 mg treatment group and 0% in the fasiglifam 50 mg treatment groups vs. 1.5% in the placebo group) [9]. In an additional, open-label, phase III study of fasiglifam 25 and 50 mg in Japanese patients with T2DM, the incidences of ALT > 3 × ULN and > 5 × ULN were higher in the fasiglifam 50 mg group (2.9 and 0.8%, respectively) than in the 25 mg group (1.6 and 0.2%, respectively) [10]. The incidence of serum ALT elevations > 3 × ULN in the Japanese open-label clinical trials was comparable with that observed in this pooled analysis of controlled phase II–III studies, although the incidence of ALT elevations ≥ 5 × ULN relative to placebo was lower in the Japanese open-label study. No Hy’s Law cases were reported in the Japanese studies [9, 10], but overall patient exposure in the combined fasiglifam 25 and 50 mg groups in our pooled analysis presented here was higher than in these Japanese studies.
5 Conclusions
Fasiglifam is the first GPR40 agonist to undergo extensive clinical development in patients with T2DM. More than 5000 patients were exposed to the drug in controlled clinical studies at the time development was terminated. A fasiglifam liver safety signal was identified, primarily based on the examination of laboratory data. The cumulative incidence of elevations in serum ALT > 3 × ULN increased over the first 6 months of fasiglifam treatment compared with placebo and active comparators, and the incidence rate did not clearly differ at the two daily doses administered. Although the elevations in serum ALT were generally asymptomatic and reversed promptly after discontinuing treatment, recovery in at least two patients who probably experienced liver injury due to fasiglifam was prolonged. In addition, one clear Hy’s Law case and two cases that nearly met the Hy’s Law case criteria were identified among the fasiglifam-treated subjects. The totality of these observations played a key role in the decision-making process regarding termination of the clinical development program for fasiglifam. Additional work is ongoing to identify the mechanism of fasiglifam-associated hepatotoxicity, for which the exact mechanism of action remains unknown, although potential causes have been postulated [11, 20]. We hope that publication of the results and the experience of this clinical trial development program may be of use to future researchers of G protein-coupled receptors, as well as contribute to a better understanding of drug-induced liver injury.
Change history
17 October 2018
In the original publication of the article, the ALT and AST values in Fig. 5a–e were capped at 10× ULN, which did not accurately reflect the narrative provided for each case. In this correction, the original Fig. 5a–e (Fig. 1a–e) and the correct Fig. 5a–5e (Fig. 2a–e) are published.
References
Itoh Y, Kawamata Y, Harada M, et al. Free fatty acids regulate insulin secretion from pancreatic beta cells through GPR40. Nature. 2003;422:173–6.
Edfalk S, Steneberg P, Edlund H. Gpr40 is expressed in enteroendocrine cells and mediates free fatty acid stimulation of incretin secretion. Diabetes. 2008;57:2280–7.
Briscoe CP, Tadayyon M, Andrews JL, et al. The orphan G protein-coupled receptor GPR40 is activated by medium and long chain fatty acids. J Biol Chem. 2003;278:11303–11.
Tsujihata Y, Ito R, Suzuki M, et al. TAK-875, an orally available G protein-coupled receptor 40/free fatty acid receptor 1 agonist, enhances glucose-dependent insulin secretion and improves both postprandial and fasting hyperglycemia in type 2 diabetic rats. J Pharmacol Exp Ther. 2011;339:228–37.
Yashiro H, Tsujihata Y, Takeuchi K, Hazama M, Johnson PR, Rorsman P. The effects of TAK-875, a selective G protein-coupled receptor 40/free fatty acid 1 agonist, on insulin and glucagon secretion in isolated rat and human islets. J Pharmacol Exp Ther. 2012;340:483–9.
Naik H, Vakilynejad M, Wu J, et al. Safety, tolerability, pharmacokinetics, and pharmacodynamic properties of the GPR40 agonist TAK-875: results from a double-blind, placebo-controlled single oral dose rising study in healthy volunteers. J Clin Pharmacol. 2012;52:1007–16.
Leifke E, Naik H, Wu J, et al. A multiple-ascending-dose study to evaluate safety, pharmacokinetics, and pharmacodynamics of a novel GPR40 agonist, TAK-875, in subjects with type 2 diabetes. Clin Pharm Ther. 2012;92:29–39.
Burant CF, Viswanathan P, Marcinak J, et al. TAK-875 versus placebo or glimepiride in type 2 diabetes mellitus: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2012;379:1403–11.
Kaku K, Enya K, Nakaya R, Ohira T, Matsuno R. Efficacy and safety of fasiglifam (TAK-875), a G protein-coupled receptor 40 agonist, in Japanese patients with type 2 diabetes inadequately controlled by diet and exercise: a randomized, double-blind, placebo-controlled, phase III trial. Diabetes Obes Metab. 2015;17:675–81.
Kaku K, Enya K, Nakaya R, Ohira T, Matsuno R. Long-term safety and efficacy of fasiglifam (TAK-875), a G-protein-coupled receptor 40 agonist, as monotherapy and combination therapy in Japanese patients with type 2 diabetes: a 52-week open-label phase III study. Diabetes Obes Metab. 2016;18:925–9.
Wolenski FS, Zhu AZX, Johnson M, et al. Fasiglifam (TAK-875) alters bile acid homeostasis in rats and dogs: a potential cause of drug induced liver injury. Toxicol Sci. 2017;157:50–61.
Araki T, Hirayama M, Hiroi S, Kaku K. GPR40-induced insulin secretion by the novel agonist TAK-875: first clinical findings in patients with type 2 diabetes. Diabetes Obes Metab. 2012;14:271–8.
Kaku K, Araki T, Yoshinaka R. Randomized, double-blind, dose-ranging study of TAK-875, a novel GPR40 agonist, in Japanese patients with inadequately controlled type 2 diabetes. Diabetes Care. 2013;36:245–50.
US Food and Drug Administration. Guidance for industry drug-induced liver injury: premarketing clinical evaluation. Drug Safety. 2009. https://www.fda.gov/downloads/Drugs/../guidances/UCM174090.pdf. Accessed 12 Apr 2017.
Rockey DC, Seeff LB, Rochon J, et al. Causality assessment in drug-induced liver injury using a structured expert opinion process: comparison to the Roussel–Uclaf causality assessment method. Hepatology. 2010;51:2117–26.
Aithal GP, Watkins PB, Andrade RJ, et al. Case definition and phenotype standardization in drug-induced liver injury. Clin Pharmacol Ther. 2011;89:806–15.
Merz M, Lee KR, Kullak-Ublick GA, Brueckner A, Watkins PB. Methodology to assess clinical liver safety data. Drug Saf. 2014;37(Suppl 1):S33–45.
Regev A. How to avoid being surprised by hepatotoxicity at the final stages of drug development and approval. Clin Liver Dis. 2013;17:749–67.
Mosedale M, Watkins PB. Drug-induced liver injury: advances in mechanistic understanding that will inform risk management. Clin Pharmacol Ther. 2017;101:469–80.
Otieno MA, Snoeys J, Lam W, et al. Fasiglifam (TAK 875): Mechanistic investigation and retrospective identification of hazards for drug induced liver injury. Toxicol Sci. 2017. https://doi.org/10.1093/toxsci/kfx040 (Epub 16 Feb 2017).
Funding
The studies included in the analyses were funded by Takeda Development Center Americas, Inc. and Takeda Pharmaceutical Company Limited.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
John F. Marcinak and Neila Smith are employed by Takeda Development Center Americas, Inc. (Deerfield, IL, USA). Melvin S. Munsaka is a former employee of Takeda Development Center Americas, Inc. Paul B. Watkins has served as a compensated consultant for Takeda regarding the liver safety of TAK-875 and other drugs. He received no compensation for the preparation of this article. Takashi Ohira is employed by Takeda Pharmaceutical Company Limited (Chuo-ku, Osaka, Japan).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Marcinak, J.F., Munsaka, M.S., Watkins, P.B. et al. Liver Safety of Fasiglifam (TAK-875) in Patients with Type 2 Diabetes: Review of the Global Clinical Trial Experience. Drug Saf 41, 625–640 (2018). https://doi.org/10.1007/s40264-018-0642-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-018-0642-6