Abstract
Introduction
In Germany, an extended-release (ER) combination of the high-potency opioid (HPO) oxycodone and the antagonist naloxone was approved in 2006. In recent years, the cardio- and cerebrovascular safety of opioid antagonists and of opioids themselves has been discussed.
Objectives
The objective of this study was to estimate the risk of major ischemic cardio- and cerebrovascular events in patients receiving ER oxycodone–naloxone compared with those receiving other ER HPOs.
Methods
We used the German Pharmacoepidemiological Research Database (GePaRD) to conduct a nested case–control study (2006–2011) within a cohort of ER HPO users. Cases were defined as patients hospitalized for acute myocardial infarction (MI) or ischemic stroke (IS). For each case, up to ten controls were selected by risk-set sampling. Using conditional logistic regression, confounder-adjusted odds ratios (aORs) and 95% confidence intervals (CIs) were obtained for the risk of MI/IS associated with (1) current HPO treatment, (2) recent discontinuation, or (3) recent switch of HPO therapy compared with past treatment.
Results
In 309,936 ER HPO users, 12,384 MI/IS events were detected, resulting in a crude incidence rate of 19.48 (95% CI 19.14–19.82) per 1000 person years. A small but significantly elevated aOR was found for morphine (1.12; 95% CI 1.04–1.22) but not for oxycodone–naloxone. Recent discontinuation and recent switch of any ER HPO also had a significant impact on the outcome (aOR 1.12; 95% CI 1.04–1.21 and 1.25; 95% CI 1.03–1.52, respectively).
Conclusions
Our study does not indicate an association between oxycodone–naloxone and ischemic cardio- or cerebrovascular events. However, our findings do suggest that every change in ER HPO therapy should be conducted with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Older age, female sex, and a diagnosis of cancer predicted initiating treatment with extended-release (ER) oxycodone–naloxone instead of ER oxycodone alone. |
Adjusted for relevant cardio- and cerebrovascular risk factors and co-medication, this study did not detect an increased risk for acute myocardial infarction or ischemic stroke for ER oxycodone–naloxone compared with other ER high-potency opioids. |
1 Introduction
The number of opioid prescriptions has risen substantially in recent decades [1–4]. A common and bothersome adverse effect associated with this type of pain therapy is opioid-induced constipation (OIC), which affects about 40% of patients with chronic non-malignant pain and 70–95% of those treated for cancer pain [5]. In contrast to other side effects, OIC is often observed throughout the whole treatment period.
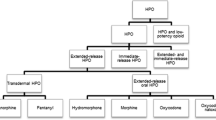
One way to reverse OIC is to combine the opioid agent with an opioid receptor antagonist that will not compromise pain reduction [6]. An example of this approach is the oral extended-release (ER) fixed combination of the high-potency opioid (HPO) oxycodone with naloxone as opioid antagonist. ER oxycodone–naloxone was first launched in Germany in 2006, then in other European countries, and is indicated for the treatment of severe pain that can be adequately managed only with opioids, providing analgesic efficacy comparable to that of oxycodone while counteracting OIC by blocking opioid receptors in the gut [7, 8].
In contrast, ER oxycodone–naloxone was approved by the US FDA in 2014 as an abuse-deterrent agent to treat pain severe enough to require daily, around-the-clock, long-term opioid treatment for which alternative treatment options are inadequate [6, 9, 10].
In recent years, the cardiovascular safety of opioid antagonists intended for use in OIC has been discussed [11]. For example, the FDA restricted use of the peripherally acting opioid receptor antagonist alvimopan to short-term in-hospital treatment because of the potential risk of myocardial infarction (MI) associated with long-term use [12]. The most commonly proposed mechanism for an association between ischemic cardiovascular events and opioid antagonists is physiologic stress induced by withdrawal, leading to increased myocardial work [11]. Though data linking opioid withdrawal resulting from abrupt discontinuation to adverse cardiovascular complications are limited [13], and other opioid antagonists for use in OIC have been recently approved in the USA [6] and in Europe [14, 15], this potential risk might also affect the fixed-dose ER combination of oxycodone and naloxone since symptoms of opioid withdrawal may occur in these patients given the opioid antagonistic properties of naloxone [10]. Furthermore, some studies have indicated a potential relationship between opioids themselves and cardio- and cerebrovascular outcomes [16–18]. A recent investigation found that prescription of long-acting and ER opioids for chronic non-cancer pain, compared with anticonvulsants or cyclic antidepressants, was associated with a significantly increased risk of all-cause mortality, including cardiovascular deaths [19].
Despite these safety concerns, the use of ER oxycodone–naloxone has increased considerably in Germany in recent years, accounting for more than 40% of all dispensed defined daily doses of oxycodone in 2014 [20].
Therefore, the objective of this study was to quantify the risk of major ischemic cardio- and cerebrovascular events in patients using ER oxycodone–naloxone compared with those using ER oxycodone or other ER HPOs.
To assess potential channeling of patients with cardiovascular and cerebrovascular risk factors to either ER oxycodone–naloxone or ER HPOs without naloxone, we also explored predictive factors for the choice of ER HPO.
2 Methods
2.1 Data Source and Study Design
Data for this analysis were obtained from the German Pharmacoepidemiological Research Database (GePaRD) established by the Leibniz Institute for Prevention Research and Epidemiology—BIPS. GePaRD is based on data from four statutory health insurance (SHI) providers covering over 20 million people from all regions of Germany. For each insurance member, GePaRD contains demographic characteristics, information on hospitalizations and outpatient physician visits, and outpatient dispensation data.
We conducted a retrospective study based on the years 2006–2011 in a cohort of subjects receiving ER oxycodone–naloxone and other ER HPOs included in the German Narcotic Drugs Act (electronic supplementary material [ESM] 1). Patients were enrolled in the study cohort if they had filled at least one outpatient prescription of an ER HPO approved for pain after a continuous insurance time of at least 12 months (baseline period). Patients receiving only immediate-release HPOs were not eligible to be included in the cohort. The date of the first ER HPO dispensation after the baseline period was defined as cohort entry. Cohort exit was set as the first of the following dates: (1) end of study, (2) death from any cause, (3) hospitalization for MI or ischemic stroke (IS), or (4) interruption of insurance status for more than 3 days or deregistration from the insurance provider.
We also conducted a nested case–control study matching up to ten controls to each hospitalized MI/IS case with respect to sex, year of birth, and SHI provider using risk-set sampling. An index day was assigned to each control resulting in the same length of follow-up as for the corresponding case. Cohort members who were hospitalized at the index day of the case were excluded from the set of potential controls because they were not at risk of hospitalization due to MI/IS. Patients might have served as controls for more than one case and were eligible to be selected as controls until they became a case [21].
In Germany, the use of health insurance data for scientific research is regulated by the Code of Social Law. All involved SHI providers and federal and regional authorities approved the use of the data for this study. Patient informed consent was not required by law because the study was based on pseudonymous data.
2.2 Extended-Release High-Potency Opioid Exposure
The duration of exposure for each ER HPO during the study period was estimated using the number of entities dispensed and according to the dosage scheme provided by the respective Summary of Product Characteristics analogously to a prior GePaRD-based study examining ER HPOs (ESM 1) [22]. The potency and strength of each dispensation were assessed using conversion factors based on morphine equivalents. Daily ER HPO doses ≥90 mg morphine equivalents were considered high [16, 23]. A grace period, defined as 20% of the supply of the previous dispensation, was allowed between subsequent dispensations to account for variable opioid dosing patterns.
In the case–control analysis, current ER HPO use was defined as exposure overlapping the index day. Patients were considered recent users if they had discontinued ER HPO treatment up to 30 days before the index day (recent discontinuation). All patients not classified as current or recent users were categorized as past users. Furthermore, a switch was considered recent if treatment had changed from one ER HPO substance to another in the 30 days before the index day. Concurrent use of different ER HPO substances or the addition of one ER HPO to continuous treatment with another ER HPO was not considered a switch.
2.3 Outcome
The outcome was defined as hospitalization for acute MI or IS identified by the main discharge diagnoses reflecting the reason for the hospitalization (ESM 2). The time of the event was defined as the hospital admission date.
2.4 Covariates
Baseline covariates were assessed in the 12 months preceding cohort entry. Comorbidity including cardio- and cerebrovascular risk factors was obtained from inpatient and outpatient diagnoses (ESM 2), and a history of cardiovascular medication was retrieved from outpatient dispensations (ESM 3). Patients diagnosed with mental and behavioral disorders due to opioid use and/or receiving opioid-replacement therapy were considered to be abusing or dependent on opioids. Addictive habits such as mental and behavioral disorders due to the use of alcohol or cannabinoids were classified as other substance use disorders.
Potential indications for ER HPO use were examined during the 6 months preceding cohort entry and at cohort entry. Patients were assumed to have received HPOs for cancer pain if they had at least one diagnosis of cancer. Further indications such as arthrosis or intervertebral disc conditions were classified according to a recent analysis of German claims data (ESM 2) [24]. For the case–control study, concomitantly used drugs were also assessed from outpatient dispensations during the 90 days before the index day. They encompassed immediate-release HPOs, low-potency opioids (LPOs) approved for pain therapy, and adjuvant analgesics. Drugs associated with increased cardio- and cerebrovascular risk, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or antipsychotics were also assessed (ESM 3).
2.5 Statistical Analyses
Crude incidence rates (IRs), overall and stratified by sex and age group, were calculated per 1000 person-years (PYs). Corresponding 95% confidence intervals (CIs) were determined with the substitution method, assuming the number of events was Poisson distributed [25]. Furthermore, a logistic regression model was used to identify predictors for initiating treatment with ER oxycodone–naloxone or ER oxycodone, including baseline covariates, recent hospitalizations, and the specialty of the prescribing physician. Finally, we conducted a nested case–control analysis using conditional logistic regression to obtain confounder-adjusted odds ratios (aORs) with corresponding 95% CIs for the risk of MI or IS associated with (1) current HPO treatment, (2) recent discontinuation, or (3) recent switch of HPO therapy compared with past treatment. We calculated aORs using the SAS procedure PHREG with the BRESLOW option for the handling of ties and used a backward selection procedure including ER HPO treatment-related variables and known cardio- and cerebrovascular risk factors as fixed variables. Analyses were performed using SAS software (version 9.2; SAS Institute Inc., Cary, NC, USA).
2.6 Sensitivity and Subgroup Analyses
In a sensitivity analysis, no grace period was allowed between subsequent dispensations. Subgroup analyses were based on (1) patients with <90 mg morphine equivalents on the index date and (2) those without prior MI/IS, respectively. Analyses were also stratified by outcome, sex, and age group. To examine whether a switch to ER oxycodone–naloxone was associated with an increased risk of MI/IS, a recent switch to ER oxycodone–naloxone was compared with no switch in current ER oxycodone–naloxone users in a further subgroup analysis.
3 Results
During the study period, 309,936 patients received at least one ER HPO. Median age at cohort entry was 70 years, and approximately two-thirds of patients were female (Table 1). The most common ER HPO leading to cohort entry was fentanyl (38.4%), followed by oxycodone (16.3%) and morphine (13.2%). Overall, 83.8% of patients had not received any HPO in the 6 months preceding cohort entry, nearly three-quarters of patients were treated with only one substance during the study period (ESM 4), and 80% of patients received only ER HPOs during the study period. Patients receiving fentanyl were oldest (median age 76 years), followed by those treated with buprenorphine (73 years). A history of ischemic heart disease, congestive heart failure, diabetes mellitus, or cerebrovascular diseases was most common among patients receiving fentanyl or buprenorphine.
Older age and female sex increased the probability of treatment with oxycodone–naloxone instead of oxycodone alone in patients new to ER HPO (Fig. 1). Patients receiving their first prescription from a specialist or having a diagnosis of cancer were also more likely to initiate treatment with the combination product (aOR 1.38; 95% CI 1.32–1.44 and 1.11; 95% CI 1.07–1.15, respectively). Among cardio- and cerebrovascular risk factors, only atherosclerosis/peripheral vascular disease increased the likelihood of ER oxycodone therapy. Patients who started ER HPO therapy later in the study period had a higher probability of receiving the combination product (by the factor 6–15). Opioid abuse/dependence had no significant impact, but other substance use disorders increased the probability of receiving oxycodone alone (aOR 0.87; 95% CI 0.81–0.94).
Predictors of treatment with oxycodone–naloxone vs. oxycodone in incident users of oxycodone–naloxone or oxycodone, where ‘incident’ means that no high-potency opioids were dispensed in the 6 months preceding cohort entry. See the electronic supplementary material 5 for the characteristics of incident users of oxycodone–naloxone or oxycodone. ‘Recent hospitalization’ refers to the 7 days preceding cohort entry, ‘physicians’ specialty’ refers to the physician issuing the index extended-release high-potency opioid prescription, and ‘other CV medication’ includes antihypertensive drugs, diuretics, beta-blocking agents, calcium antagonists, angiotensin-converting enzyme inhibitors, and angiotensin-2 antagonists. CI confidence interval, COX-2 cyclooxygenase 2, CV cardiovascular, GP general practitioner, NSAIDs nonsteroidal anti-inflammatory drugs, OR odds ratio
During the study period, 5585 MI and 6799 IS events occurred, resulting in a crude IR of 19.48 (95% CI 19.14–19.82) per 1000 PYs (ESM 6). Among individual ER HPOs, the highest crude IRs were observed for fentanyl and buprenorphine. Crude IRs were lower for MI (8.78; 95% CI 8.56–9.02) than for IS (10.69; 95% CI 10.44–10.95).
Current use of any ER HPO compared with past use yielded an aOR for MI/IS of 1.01 (95% CI 0.96–1.06; Table 2). Among specific ER HPOs, a small but significantly elevated aOR was observed only for morphine (1.12; 95% CI 1.04–1.22). Recent discontinuation and recent switch of any ER HPO had a significant impact on the outcome (aOR 1.12; 95% CI 1.04–1.21 and 1.25; 95% CI 1.03–1.52, respectively). Furthermore, morphine equivalents ≥90 mg on the index day yielded an aOR of 1.10 (95% CI 1.03–1.17).
With respect to the outcome, current use of any ER HPO compared with past use yielded an aOR for MI of 1.17 (95% CI 1.09–1.26). Among specific ER HPOs, significantly elevated aORs were observed for morphine (1.30; 95% CI 1.14–1.47), oxycodone (1.18; 95% CI 1.04–1.34), and fentanyl (1.17; 95% CI 1.06–1.30). Recent switch of any ER HPO also had a significant impact on the outcome (aOR 1.38; 95% CI 1.02–1.86). For IS, current use of any ER HPO compared with past use yielded an aOR of 0.95 (95% CI 0.88–1.02). For this outcome, only recent discontinuation revealed a small but significantly elevated aOR (1.14; 95% CI 1.02–1.27).
Allowing no grace period between subsequent dispensations, basing the analysis only on patients with <90 mg morphine equivalents on the index day, or excluding those with prior MI/IS events yielded results comparable to those from the main analysis (Table 3). A recent switch of substance among patients currently receiving oxycodone–naloxone revealed an aOR of 0.91 (95% CI 0.23–3.67) compared with no switch (ESM 8).
4 Discussion
We examined the risk of ischemic cardiovascular and cerebrovascular events in a large cohort of patients receiving ER HPO. Adjusted for relevant risk factors and co-medication, this study did not observe an increased risk of MI/IS with ER oxycodone–naloxone compared with other ER HPOs. This result is supported by a recent study assessing disproportionate reporting of adverse cardiac events associated with naloxone across large international pharmacovigilance systems [13]. The authors of that study found no increase in the relative reporting of cardiovascular disorders associated with naloxone monotherapy or in fixed-dose combinations with opioids.
We examined treatment predictors and found that older age, female sex, and a diagnosis of cancer were significant predictors of initiating use of the combination product instead of oxycodone alone. In contrast, comorbidity had no significant influence on treatment choice, indicating that channeling based on cardio- and cerebrovascular risk factors was of minor importance. This is plausible, as the discussion on oxycodone–naloxone in Germany focused on costs and effectiveness rather than safety [26, 27]. Calendar year as the strongest predictor for oxycodone–naloxone reflected the large uptake seen in the overall German prescription statistics [20]. In our study, neither opioid abuse/dependence nor substance use disorders predicted treatment with ER oxycodone–naloxone, which is supported by the fact that, in Germany, the antagonist is not intended to deter abuse but to prevent OIC [7, 28].
By stratifying the outcome, we found that any ER HPO use, as well as current treatment with morphine, oxycodone, or fentanyl or a recent switch of ER HPO treatment, significantly increased the risk of MI, whereas only recent discontinuation of ER HPO was associated with an increased risk of IS. Again, no significantly increased risk was observed for either outcome with the oxycodone–naloxone combination. These findings corroborate the increased risk of MI reported by previous studies [16, 18] and indicate that opioid treatment is not associated with ischemic cerebrovascular outcomes.
The aORs we observed for any ER HPO use and for morphine for the composite outcome as well as for MI only were lower than those reported by a recent nested case–control study based on 1.7 million non-cancer patients with no major risk factors for MI and a record of at least one opioid prescription from the Clinical Practice Research Datalink (CPRD) [18]. Based on about 12,000 incident MI cases and compared with non-use, the study showed an aOR of 1.28 (95% CI 1.19–1.37) for current use of any opioid and a 1.71-fold (95% CI 1.09–2.68) increased risk for morphine use. However, comparison with this and other studies is hampered by differences in the definition of the reference group and characteristics of users because the availability or use of opioids varies across countries.
Our findings regarding a recent discontinuation of ER HPO treatment support the assumption that ischemic cardio- and cerebrovascular events may be triggered by opioid withdrawal, particularly upon abrupt cessation of long-term opioid treatment [29]. Our study also suggests that a switch of ER HPO treatment might increase cardio- and cerebrovascular risk, but there is no indication that converting therapy to ER oxycodone–naloxone is associated with an increased risk of MI/IS.
Overall, the IRs we found per 1000 PY were 8.78 for MI and 10.69 for IS, which are higher than observed in other recent studies. For example, a US claims-based cohort analysis found an IR of 6.04 (95% CI 5.68–6.41) for MI [16], and a study using IMS® Disease Analyzer data reported even lower IRs per 1000 PY for MI (2.7; 95% CI 1.9–3.7) and stroke (5.3; 95% CI 4.1–6.2) for Germany [30]. However, these studies excluded patients with a baseline history of cancer, did not restrict opioid use to HPOs, and did not examine events during the first 6 months of treatment. In contrast, a US study examining IRs for safety events among propensity score-matched older adults with arthritis initiating opioid treatment reported substantially higher rates of 29 (95% CI 21–38) per 1000 PY for MI and 18 (95% CI 13–26) for stroke, but this was based on a broader outcome definition [17]. Furthermore, the study population was considerably older (mean age 80 years) than in our analysis.
With respect to individual ER HPOs, crude IRs for MI/IS were found to be highest for fentanyl and buprenorphine, mirroring the substantial differences with respect to age and comorbidity in patients receiving these ER HPOs compared with the other agents. However, these effects were not apparent in the case–control analysis after matching by age, sex, and SHI provider and adjusting for relevant risk factors and co-medication, including immediate-release HPOs.
The strengths of this study are its size and the representativeness of the data, which provided complete coverage of all age groups, and the lack of non-response because of the administrative nature of the data [31]. By determining exposure based on pharmacy dispensing data, recall bias can be ruled out, and information on dispensation date and product is precise [32]. Opioid prescriptions in GePaRD have been shown to be representative for Germany [33] and, since all opioids approved for pain therapy are available by prescription only, ascertainment of HPO exposure is assumed to be complete. Furthermore, the high uptake of ER oxycodone–naloxone since approval [20], and the overall preference for ER HPOs in chronic pain conditions [34, 35], which has been reported in previous studies [4, 22], make German data well suited for comparing ER oxycodone–naloxone with other ER HPOs.
A limitation of the study is that GePaRD does not provide prescribed daily doses and intended or actual treatment durations. This study was based on ER HPO analgesics usually given on fixed-dosage schedules, so we used a previously implemented algorithm to determine treatment durations [22]. Allowing no grace periods between subsequent prescriptions and thus varying the assumed duration of treatment did not change our results. Therefore, misclassification of exposure time appears less important.
This study did not include a review of individual patient files which for data protection reasons is not feasible in Germany. However, several studies [36, 37] have reported good validity for MI and IS identified from claims data. In GePaRD, MI/IS as outcomes have been investigated extensively in collaborative studies including different European and US healthcare databases [38, 39], and the validity of our outcome definition based on hospital discharge diagnoses is assumed to be high.
A further limitation is that, in Germany, outpatient diagnoses are coded quarterly; therefore, events such as withdrawal symptoms not necessarily leading to hospitalization refer only to the quarter of a year rather than an exact date. As we were also unable to examine whether discontinuation was conducted by tapering the dose, e.g., by splitting tablets, we could not investigate the potential causal chain between opioid discontinuation without downward titration, withdrawal symptoms, and the occurrence of ischemic cardio- and cerebrovascular events.
Accordingly, it was not possible to assess whether switching was performed abruptly or by slowly decreasing one ER HPO while titrating the new substance to effect [40]. Furthermore, the clinical consequences of both discontinuation and switch of treatment might be associated with the overall duration of opioid treatment or other patient-related factors, such as pain status or adverse drug reactions, not included in this analysis.
Finally, as we used administrative data, we could not assess all potential confounders such as smoking, and drugs available over the counter, including laxatives and low-dose NSAIDs are not covered, which might lead to residual but probably non-differential confounding.
Overall, our findings were consistent and robust. In contrast with other studies, this study does not provide a comparison with the general population or with patients receiving other analgesics such as NSAIDs but instead provides insight into the risks of ischemic events during treatment with individual ER HPOs.
5 Conclusion
Based on nearly 310,000 ER HPO users, our study does not postulate an association between oxycodone–naloxone and ischemic cardio- and cerebrovascular events. However, our findings regarding discontinuation and switch do suggest that every change in therapy with ER HPOs should be conducted very cautiously.
References
Kenan K, Mack K, Paulozzi L. Trends in prescriptions for oxycodone and other commonly used opioids in the United States, 2000–2010. Open Med. 2012;6:e41–7.
Frenk SM, Porter KS, Paulozzi LJ. Prescription opioid analgesic use among adults: United States, 1999–2012. NCHS Data Brief no. 189. Hyattsville, MD: National Center for Health Statistics. 2015; 1–8. https://www.cdc.gov/nchs/data/databriefs/db189.pdf.
Fischer B, Jones W, Rehm J. Trends and changes in prescription opioid analgesic dispensing in Canada 2005–2012: an update with a focus on recent interventions. BMC Health Serv Res. 2014;14:90.
Schubert I, Ihle P, Sabatowski R. Increase in opiate prescription in Germany between 2000 and 2010: a study based on insurance data. Dtsch Arztebl Int. 2013;110:45–51.
DePriest AZ, Miller K. Oxycodone/Naloxone: role in chronic pain management, opioid-induced constipation, and abuse deterrence. Pain Ther. 2014;3:1–15.
Wald A. Constipation advances in diagnosis and treatment. JAMA. 2016;315:185–91.
Mundipharma. Summary of Products Characteristics Targin. 2016. http://www.mundipharma.de/downloadFile/fi-targinpdf-00000522.html?tx_extbasefal_pi1[action]=showDownloadInfo&cHash=c71d2ad24d70fc022c45a65938caaa72. Accessed 5 Feb 2017.
Burness CB, Keating GM. Oxycodone/naloxone prolonged-release: a review of its use in the management of chronic pain while counteracting opioid-induced constipation. Drugs. 2014;74(3):353–75.
US Food and Drug Administration. FDA approves new extended-release oxycodone with abuse-deterrent properties. 2014. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm406407.htm. Accessed 11 Jan 2016.
Purdue Pharma. TARGINIQ ER Prescribing Information. Stamford, CT: Purdue Pharma L.P.; 2014. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/205777lbl.pdf. Accessed 1 April 2016.
US Food and Drug Administration; Center for Drug Evaluation and Research. Briefing document. Anesthetic and Analgesic Drug Products Advisory Committee Meeting. June 11-12, 2014. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/AnestheticAndAnalgesicDrugProductsAdvisoryCommittee/UCM400205.pdf. Accessed 4 Nov 2015.
US Food and Drug Administration (FDA). Entereg (alvimopan) capsules. Silver Spring, MD: US DFA; 2013. http://www.fda.gov/Safety/MedWatch/SafetyInformation/ucm194328.htm. Accessed 31 Jan 2016.
Sandhu A, Kao D, Mehler PS, Haigney MCP, Krantz MJ. Cardiovascular disorders associated with naloxone monotherapy and in fixed-dose combination with opioids: data from international safety surveillance. Int J Cardiol. 2016;212:360–3.
AstraZeneca AB. Summary of Product Characteristics Moventig. Södertälje: AstraZeneca AB; 2014. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002810/WC500179075.pdf. Accessed 18 May 2016.
Wyeth Lederle. Summary of Product Characteristics Relistor. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000870/WC500050562.pdf. Accessed 18 May 2016.
Carman WJ, Su S, Cook SF, Wurzelmann JI, McAfee A. Coronary heart disease outcomes among chronic opioid and cyclooxygenase-2 users compared with a general population cohort. Pharmacoepidemiol Drug Saf. 2011;20:754–62.
Solomon DH, Rassen JA, Glynn RJ, Lee J, Levin R, Schneeweiss S. The comparative safety of analgesics in older adults with arthritis. Arch Intern Med. 2010;170:1968–76.
Li L, Setoguchi S, Cabral H, Jick S. Opioid use for noncancer pain and risk of myocardial infarction amongst adults. J Intern Med. 2013;273:511–26.
Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Prescription of Long-Acting Opioids and Mortality in Patients With Chronic Noncancer Pain. JAMA. 2016;315:2415.
Böger R, Schmidt G. Analgetika. In: Schwabe U, Paffrath D, editors. Arzneiverordnungs-Report 2015. Berlin: Springer; 2015. p. 311–30.
Wacholder S, Silverman DT, McLaughlin JK, Mandel JS. Selection of controls in case-control studies III. Design options. Am J Epidemiol. 1992;135:1042–50.
Jobski K, Kollhorst B, Schink T, Garbe E. The risk of opioid intoxications or related events and the effect of alcohol-related disorders: a retrospective cohort study in german patients treated with high-potency opioid analgesics. Drug Saf. 2015;38:811–22.
Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315:1624.
Freytag A, Schiffhorst G, Thoma R, Strick K, Gries C, Becker A, et al. Identification and grouping of pain patients according to claims data. Schmerz. 2010;24:12–22.
Daly LE. Confidence limits made easy: interval estimation using a substitution method. Am J Epidemiol. 1998;147:783–90.
Hoffmann F. Stark wirkende Opioide. In: Glaeske G, Schicktanz C, editors. BARMER GEK Arzneimittelreport 2012. 14th ed. Siegburg: Asgard Verlagsservice GmbH; 2012. p. 113–30.
Arzneitelegramm. Oxycodon plus Naloxon (Targin): Was gibt es neues? 2010. http://www.arznei-telegramm.de/html/2010_05/1005051_01.html. Accessed 13 Nov 2015.
Walter C, Knothe C, Lötsch J. Abuse-deterrent opioid formulations: pharmacokinetic and pharmacodynamic considerations. Clin Pharmacokinet. 2016;55:751–67.
Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10:113–30.
LoCasale R, Kern DM, Chevalier P, Zhou S, Chavoshi S, Sostek M. Description of cardiovascular event rates in patients initiating chronic opioid therapy for noncancer pain in observational cohort studies in the US, UK, and Germany. Adv Ther. 2014;31:708–23.
Pigeot I, Ahrens W. Establishment of a pharmacoepidemiological database in Germany: methodological potential, scientific value and practical limitations. Pharmacoepidemiol Drug Saf. 2008;17:215–23.
Schneeweiss S, Avorn J. A review of uses of health care utilization databases for epidemiologic research on therapeutics. J Clin Epidemiol. 2005;58:323–37.
Fassmer A, Schink T. Representativity of outpatient drug prescriptions in the German Pharmacoepidemiological Research Database (GePaRD) In: Annual Conference of the German Society for Epidemiology (DGEpi); 17–20 Sept 2014; Ulm, p. 208. http://dgepi.de/fileadmin/pdf/tagungen_workshops/Programmheft_DGEpi_2014.pdf.
Tumorschmerzen [Empfehlungen zur Therapie von Tumorschmerzen]. 3rd ed. Köln: Drug Commission of the German Medical Association; 2007.
The Association of the Scientific Medical Societies in Germany (AWMF). S3 guideline LONTS. Long-term administration of opioids for non-tumor pain (Update 01/2015). http://www.awmf.org/uploads/tx_szleitlinien/145-003l_S3_LONTS_2015-01.pdf. Accessed 15 Oct 2015.
McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of myocardial infarction diagnoses in administrative databases: a systematic review. PLoS One. 2014;9:e92286.
McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA. Validity of diagnostic codes for acute stroke in administrative databases: a systematic review. PLoS One. 2015;10:e0135834.
Masclee G, Sturkenboom M, Leal I, De Berardis G, Bezemer I, Gil M, et al. Harmonization of Acute Myocardial Infarction Identification from Different Databases in the SAFEGUARD Project. Abstracts of the 29th International Conference on Pharmacoepidemiology & Therapeutic Risk Management, 25–28 Aug 2013, Montréal, Canada. Pharmacoepidemiol Drug Saf. 2013;22, p. s1:276.
Schmedt N, Gil M, Martin E, Requena G, Bezemer I, De Berardis G, et al. Harmonization of Outcome Extraction for Ischemic and Hemorrhagic Stroke Across Data Sources in the SAFEGUARD Project. Abstracts of the 29th International Conference on Pharmacoepidemiology & Therapeutic Risk Management, 25–28 Aug 2013, Montréal, Canada. Pharmacoepidemiol Drug Saf. 2013;22, p. s1:307.
Webster LR. Eight principles for safer opioid prescribing. Pain Med. 2013;14:959–61.
Acknowledgements
The authors thank all SHI providers for providing data for this study (Techniker Krankenkasse [TK], AOK Bremen/Bremerhaven, DAK-Gesundheit, Handelskrankenkasse). We also thank Marieke Niemeyer, MSc, and Nils Fabian Gesing, Dipl-Math, for contributing to the statistical analyses and Heike Gerds, PhD, for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Purdue Pharma LP. The funders had no role in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; in the preparation, review, or approval of the manuscript; or in the decision to submit the manuscript for publication. However, they did receive the study protocol and the manuscript to provide comments according to section VIII.B.5 of the Guideline on Good Pharmacovigilance Practice (GVP)—Module VIII.
Conflicts of interest
Bianca Kollhorst and Tania Schink are employees and Kathrin Jobski and Edeltraut Garbe are former employees of the Leibniz Institute for Prevention Research and Epidemiology—BIPS. As such, they have performed research studies sponsored by pharmaceutical companies (Bayer-Schering, Celgene, GSK, Mundipharma, Novartis, Sanofi-Aventis, Sanofi-Pasteur MSD, Stada, and Takeda) unrelated to this study. Edeltraut Garbe has acted as a consultant to Bayer, Nycomed, Takeda, Astellas, Novartis, and GSK on work unrelated to the subject of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jobski, K., Kollhorst, B., Garbe, E. et al. The Risk of Ischemic Cardio- and Cerebrovascular Events Associated with Oxycodone–Naloxone and Other Extended-Release High-Potency Opioids: A Nested Case–Control Study. Drug Saf 40, 505–515 (2017). https://doi.org/10.1007/s40264-017-0511-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-017-0511-8