Abstract
Background
Topiramate (TPM) is effective for treating epilepsy, but executive dysfunction is a common side effect that could significantly affect everyday life. Additionally, previous studies have suggested that patients might be unaware of these changes.
Objective
To evaluate a rapid TPM titration scheme for the early detection of adverse cognitive side effects.
Methods
In this retrospective study, we assessed changes in objective cognitive performance (EpiTrack®) after rapidly titrating TPM (50 mg per day during an inpatient stay) in 49 epilepsy patients and compared those results with an outpatient control group that underwent the recommended standard titration (n = 23 with 25–50 mg per week).
Results
Using Bayesian statistics, analyses revealed decisive evidence of a negative effect on cognitive performance when TPM was introduced (BF 31480000000) independent of the titration speed (BF 0.739). When using a fast titration rate, deficits in executive function increased from a baseline of 53.1 to 73.5% at follow-up, and 55.1% experienced a statistically significant intraindividual decline. When using the standard titration scheme, impairments increased from 52.2 to 65.2%, with an intraindividual deterioration found in 52.2% of the patients.
Conclusion
Physicians might be able to detect adverse cognitive side effects sooner in epilepsy patients if TPM is administered using a faster titration rate while applying repeated cognitive assessments within days. This approach might help prevent any unnoticed intolerance and eventual negative consequences for the patient. Therefore, we recommend monitoring early on for adverse changes instead of withholding a potentially effective treatment option because of anticipated side effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Topiramate (TPM) is a highly effective drug with a broad range of applications. However, commonly occurring adverse side effects that affect cognition and that may diminish the patient’s ability to notice these changes pose a challenge in clinical practice. |
Rapid titration of TPM along with early cognitive monitoring appears to be a pragmatic approach for safely testing whether TPM is a tolerable treatment option, and thereby avoiding unnoticed intolerance and helping prevent negative consequences for the patient. |
1 Introduction
Topiramate (TPM) is an effective medication for treating generalized tonic-clonic seizures, focal seizures with or without focal to bilateral tonic-clonic seizures, and seizures associated with the Lennox–Gastaut syndrome [1]. Furthermore, it is also administered as a migraine-prophylaxis [2] and is used in the treatment of obesity [3], neuropathic pain [4], and alcohol-dependence [5]. TPM is currently the seventh most commonly prescribed antiepileptic medication (ASM) in German neurological practices [6]. However, executive dysfunction is a common cognitive side effect of TPM [7,8,9,10]. Drug-induced impairments in divergent thinking, fluency of speech, and working memory can significantly affect how epilepsy patients function on a daily basis [11, 12]. The cognitive and behavioral side effects of an ASM belong to the least tolerated class of side effects [9] and may negatively affect long-term retention, adherence, and quality of life. Out of all the available ASMs, TPM has, by far, the highest rate of intolerable cognitive side effects [13].
Attempts at gradually titrating TPM [14] in order to reduce the occurrence and the extent of cognitive side effects have been, for the most part, unsuccessful [12, 15, 16]. A slower titration could even complicate matters, as patients may not be aware of adverse cognitive effects if these develop slowly [17, 18]. Since cognitive side effects have also been observed in patients with low doses of TPM [12, 19], it appears as though no safe dose range exists that would exclude the adverse effects on cognition. Therefore, one would tend to attribute the negative cognitive side effects of TPM to an idiosyncratic intolerance, rather than an intrinsic feature of the drug that would affect all patients depending on the dose or titration rate.
A potentially highly effective drug with a broad range of applications that, unfortunately, also has an adverse cognitive side-effect profile, is a clinical dilemma. Currently, no clinical predictors are available that identify those patients who are able to tolerate TPM. This leaves physicians with two options: (1) to deprive patients, per se, of a potentially effective treatment option, or (2) to carry out trial and error experimentation. We reject the former and recommend the latter but performed in a controlled setting [20]. In the present study, we utilized a pragmatic approach that included a faster titration rate with TPM during an inpatient hospital stay combined with early cognitive monitoring [21]. This approach could help prevent any unnecessary burden (i.e., the long-term, negative effects on the overall vocational, social, and physical outlook of the patient) to the patients and also prevent them from slowly developing unnoticed side effects after they have been discharged. In this retrospective study, we assessed the objective cognitive changes that occurred after TPM was administered using a rapid titration rate within an inpatient hospital setting. A group of outpatients served as controls and were administered TPM using the recommended standard titration rate. The objective of this study was to evaluate the feasibility of this approach and to ascertain whether faster titration leads to a higher incidence of cognitive side effects. Preliminary data presented as a scientific poster [22] revealed a 70% incidence of cognitive side effects in ten patients who were administered TPM with rapid titration, whereas the 15 patients with standard titration showed an incidence rate of 47%.
2 Methods
2.1 Study Design and Patients
In this retrospective controlled study conducted at the Department of Epileptology at the University Hospital Bonn (UKB), we analyzed the cognitive effects of a rapid titration scheme [50 mg TPM per day with a starting dose of 50 mg/day: day 1: 0 (morning)—0 (midday)—50 (evening); day 2: 50—0—50; day 3: 50—0—100, etc.] and provided early cognitive monitoring to inpatients who were scheduled to undergo their first dose of (generic) TPM. Patients were informed of the procedure and the modifications associated with a rapid titration rate (as compared to the standard titration scheme). Written informed consent was acquired. The control group was comprised of patients who were prescribed TPM and the recommended standard titration scheme (25–50 mg per week with starting doses of 25–50 mg/day) was carried out and a cognitive reassessment was conducted at the next outpatient follow-up visit (i.e., after the recommended dose had been achieved and maintained).
Inclusion criteria were: (1) age ≥ 16 years; (2) an epilepsy diagnosis; (3) a cognitive baseline without evidence of a floor effect (i.e., a performance that can no longer deteriorate according to reliable change indices).
The study was approved by the ethics committee of the medical faculty of the University of Bonn (180/15).
2.2 Cognitive Assessment
Executive functions were compared before and after rapid versus standard titration using the screening tool, EpiTrack®. EpiTrack® (third edition) is a screening tool devised for tracking the adverse cognitive effects of antiepileptic medication [23, 24]. The test is comprised of six subtests on response inhibition, visuo-motor speed, mental flexibility, visual motor planning, verbal fluency, and working memory. Based on the subtest results, an age-corrected total score was calculated. Application and evaluation of this test is simple, thereby enhancing objectivity. Age-corrected norms from 689 healthy subjects (age range 16–87 years) and reliable change indices (RCIs) for reassessments are provided. Patients can achieve a maximum score of 49 points. The interval for mild impairment is 29–31 points (i.e., > 1 standard deviation and ≤ 2 standard deviations below the mean of the normative sample), and the cutoff for significant impairment is ≤ 28 points (i.e., > 2 standard deviations below the mean of the normative sample). Practice-corrected RCIs indicated a significant intraindividual change with a gain of > 3 points, and a loss of > 2 points. Studies demonstrated the usefulness of EpiTrack® with regard to cognitive monitoring of pharmacological treatments [8, 25,26,27,28,29] and its sensitivity with regard to the overall drug load, i.e., the number of concurrent ASMs [30, 31].
The EpiTrack® was performed by trained staff of the neuropsychological unit in the morning (9–11 am) or afternoon (2–4 pm).
2.3 Statistical Analyses
The statistical analyses are based on Bayesian statistics. These differ from the typical frequentist (p value) statistics in that they do not refer to the likelihood of the data given the null hypothesis of no effect. Instead, the likelihoods of both the null and alternative hypotheses are calculated given the data. Etz et al. [32] provide a short overview about background and methodology.
Bayes factors (BFs) quantify the credibility of each hypothesis given the data and relate them to each other, such that a BF10 value of 10 means that the H1 is ten times as credible as the H0. BF10 = 1 would indicate that the data does not differentiate between H0 and H1. Importantly, this works in both directions, i.e., a BF10 < 1 can be interpreted as evidence against an effect. The positive confirmation of a non-effect is one of the biggest advantages of Bayesian statistics [32]. As established in the literature, we defined BF > 3 as weak evidence, BF > 10 as substantial evidence and BF > 100 as decisive evidence for an effect.
We used Bayesian contingency tables and Bayesian independent-samples t tests to compare characteristics of the two subgroups, and we conducted Bayesian repeated-measures analysis to analyze intraindividual change of EpiTrack® performance after introduction of TPM considering group (rapid vs. standard titration) as between-subject factor.
In addition to the group analysis, we also reported statistically significant cognitive changes on an individual level by means of RCIs.
JASP 0.9.2 was used to calculate all analyses.
3 Results
This study was comprised of 49 inpatients who were administered TPM using a rapid titration rate and a control group of 23 outpatients who were administered TPM using the recommended standard scheme. No statistically significant differences in demographics or clinical characteristics were found in either group (see Table 1).
All patients underwent a cognitive screening before TPM was administered. Cognitive reassessment was conducted after 5.8 ± 2.5 days (mean ± standard deviation) (during an inpatient stay lasting for 9.7 ± 2.9 days) for the rapid titration group and after 96.7 ± 41.7 days for the outpatients with standard titration. The end doses were comparable, with 204.6 ± 70.7 mg/day for the rapid titration group and 247.8 ± 136.1 mg/day for the standard titration group (BF 0.969).
At baseline, the number of ASMs (BF 0.756) and cumulative defined daily dose (DDD) (BF 0.303) were comparable between the two subgroups (Table 1). The age-corrected EpiTrack® score indicated mild and significant impairment in 26.5% and 26.5% of patients with subsequent rapid titration and 38.1% and 23.5% in those with scheduled standard titration, respectively (BF 0.191). The mean EpiTrack® score was comparable as well (BF 0.466).
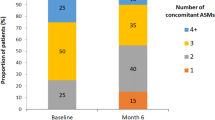
Bayesian repeated-measures analysis revealed decisive evidence of a negative effect on cognitive performance when TPM was introduced (BF 31 480 000 000) without any evidence of an interaction effect with the group (BF 0.739). Thus, we could discern that both groups displayed a similar negative effect of TPM on executive functions (Fig. 1).
With rapid titration, the objective deficits in executive function increased from 53.1% (26.5% mild and 26.5% significant impairment) at baseline to 73.5% (16.3% mild and 57.1% significant impairment) at follow-up, and 55.1% experienced a statistically significant intraindividual decline according to RCIs. With standard titration, the impairments increased from 52.2% (34.8% mild and 17.4% significant impairment) to 65.2% (30.4% mild and 34.8% significant impairment) with statistically significant intraindividual deteriorations in 52.2% of the patients.
TPM was withdrawn after the follow-up visit in 26.5% of the patients following rapid titration and in 34.8% of the controls following standard titration (BF 0.365). Reasons for a continuation of the treatment despite a statistically significant objective deterioration of executive functions included subjective cognitive tolerance, enhanced seizure control, the hope that the side effects after rapid titration were acute and could vanish with time, and the assumption that a dose reduction could improve the cognitive status.
4 Discussion
In this study, we addressed a clinical dilemma in the pharmacological treatment of epilepsy, namely in dealing with TPM, which is potentially highly effective for controlling seizures, but is often accompanied by adverse effects on cognition [20]. Instead of depriving epilepsy patients of a potentially effective treatment option, we evaluated the pragmatic approach of using a faster titration scheme with TPM combined with early cognitive monitoring.
With the rapid titration rate of 50 mg of TPM per day, 55.1% of the patients showed a statistically significant intraindividual decline in executive function, whereas the standard titration rate (25–50 mg of TPM per week) was associated with a statistically significant intraindividual cognitive deterioration in 52.2% of the patients. Apparently, the proportion of patients displaying cognitive side effects is comparable between the two titration schemes. Thus, patients do not appear to display an elevated risk due to the faster titration rate; this had been previously suggested in a preliminary data analysis [22] of just ten patients with rapid TPM titration versus 15 patients with standard titration. In the current sample, with a nearly fivefold increase in patients using a rapid titration rate, one in two patients is affected by TPM-induced cognitive side effects, regardless of the titration regimen. The major difference between these two groups is that the standard titration group had to tolerate weeks to months of cognitive side effects and the potential negative impact these side effects played on their daily functioning. In contrast, this unnecessary burden could be avoided with those patients who were administered TPM using a faster titration scheme and whose cognitive abilities were reassessed days later. We recently published a case report of a patient who had been suffering from the severe cognitive side effects of TPM for more than 16 years, with profound negative, partly irreversible, consequences for her daily functioning, career, and social life [11].
If the objective reassessment reveals adverse cognitive side effects, this does not automatically mean that TPM must be discontinued. The result of the cognitive test is rather the basis for the subsequent discussion between the patient and the treating physician in deciding how to proceed. Subjective tolerability, achieved seizure control, and potential non-cognitive side effects must be taken into consideration as well. Overall, an individual balancing of the degree of seizure control and ASM-related side effects is necessary when striving for a constellation that provides the highest possible quality of life [20].
Although our approach was performed in a controlled inpatient setting, an inpatient stay is not a prerequisite. Early cognitive reassessment can also be performed in outpatient settings, scheduling a control follow-up visit 1 week after the rapid titration of TPM.
Limitations of this study include its retrospective study design, the limited representativity of patients enrolled in a specialized epilepsy center, and the non-standardized follow-up intervals.
5 Conclusion
Rapid titration of TPM with early cognitive monitoring appears to be a pragmatic approach for safely testing whether TPM is a tolerable treatment option, thereby avoiding unnoticed intolerance and hopefully preventing negative consequences for the patient. Future studies would be appreciated that confirm these results and evaluate this approach with other ASMs that also have adverse cognitive side-effect profiles (e.g., zonisamide [8]) and that are suitable for rapid titration.
References
Lyseng-Williamson KA, Yang LPH. Topiramate: a review of its use in the treatment of epilepsy. Drugs. 2007;67:2231–56.
Silberstein S, Diener HC, Lipton R, Goadsby P, Dodick D, Bussone G, et al. Epidemiology, risk factors, and treatment of chronic migraine: a focus on topiramate. Headache. 2008;48:1087–95.
Astrup A, Toubro S. Topiramate: a new potential pharmacological treatment for obesity. Obes Res. 2004;12(Suppl):167S-S173.
Nazarbaghi S, Amiri-Nikpour MR, Eghbal AF, Valizadeh R. Comparison of the effect of topiramate versus gabapentin on neuropathic pain in patients with polyneuropathy: a randomized clinical trial. Electron physician. 2017;9:5617–22.
Guglielmo R, Martinotti G, Quatrale M, Ioime L, Kadilli I, Di Nicola M, et al. Topiramate in alcohol use disorders: review and update. CNS Drugs. 2015;29:383–95.
Scholten J, Hamer HM, Kostev K. Usage of antiepileptic drugs in different diseases in Germany—a retrospective study. Epilepsy Behav. 2020;111: 107210.
Kockelmann E, Elger CE, Helmstaedter C. Cognitive profile of topiramate as compared with lamotrigine in epilepsy patients on antiepileptic drug polytherapy: relationships to blood serum levels and comedication. Epilepsy Behav. 2004;5:716–21.
Meschede C, Witt JA, Brömling S, Moskau-Hartmann S, Rademacher M, Surges R, et al. Changes in cognition after introduction or withdrawal of zonisamide versus topiramate in epilepsy patients: a retrospective study using Bayes statistics. Epilepsia. 2020;61:1481–90.
Witt J-A, Elger CE, Helmstaedter C. Which drug-induced side effects would be tolerated in the prospect of seizure control? Epilepsy Behav. 2013;29:141–3.
Jansen JFA, Aldenkamp AP, Marian Majoie HJ, Reijs RP, de Krom MCTFM, Hofman PAM, et al. Functional MRI reveals declined prefrontal cortex activation in patients with epilepsy on topiramate therapy. Epilepsy Behav. 2006;9:181–5.
Witt JA, Rademacher M, von Wrede R, Surges R, Helmstaedter C. Cognitive reawakening and improved quality of life achieved after discontinuing 16 years of anti-seizure treatment with topiramate. Neurocase. 2022;28:102–6.
Huppertz HJ, Quiske A, Schulze-Bonhage A. Kognitive Beeinträchtigungen unter Add-on-Therapie mit Topiramat. Nervenarzt. 2001;72:275–80.
Javed A, Cohen B, Detyniecki K, Hirsch LJ, Legge A, Chen B, et al. Rates and predictors of patient-reported cognitive side effects of antiepileptic drugs: an extended follow-up. Seizure. 2015;29:34–40.
Aldenkamp AP, Baker G, Mulder OG, Chadwick D, Cooper P, Doelman J, et al. A multicenter, randomized clinical study to evaluate the effect on cognitive function of topiramate compared with valproate as add-on therapy to carbamazepine in patients with partial-onset seizures. Epilepsia. 2000;41:1167–78.
Gomer B, Wagner K, Frings L, Saar J, Carius A, Härle M, et al. The influence of antiepileptic drugs on cognition: a comparison of levetiracetam with topiramate. Epilepsy Behav. 2007;10:486–94.
Salinsky MC, Storzbach D, Spencer DC, Oken BS, Landry T, Dodrill CB. Effects of topiramate and gabapentin on cognitive abilities in healthy volunteers. Neurology. 2005;64:792–8.
Kockelmann E, Elger CE, Helmstaedter C. Significant improvement in frontal lobe associated neuropsychological functions after withdrawal of topiramate in epilepsy patients. Epilepsy Res. 2003;54:171–8.
Fritz N, Glogau S, Hoffmann J, Rademacher M, Elger CE, Helmstaedter C. Efficacy and cognitive side effects of tiagabine and topiramate in patients with epilepsy. Epilepsy Behav. 2005;6:373–81.
Romigi A, Cervellino A, Marciani MG, Izzi F, Massoud R, Corona M, et al. Cognitive and psychiatric effects of topiramate monotherapy in migraine treatment: an open study. Eur J Neurol. 2008;15:190–5.
Witt J-A, Helmstaedter C. How can we overcome neuropsychological adverse effects of antiepileptic drugs? Expert Opin Pharmacother. 2017;18:1–4.
Witt J-A, Helmstaedter C. Monitoring the cognitive effects of antiepileptic pharmacotherapy—approaching the individual patient. Epilepsy Behav. 2013;26:450–6.
Widman G, Witt J-A, Elger CE, Helmstaedter C. Does fast titration of topiramate reveal the early detection of patients who will experience negative cognitive side effects? [poster]. Eur J Neurol. 2015;22:338.
Lutz MT, Helmstaedter C. EpiTrack: tracking cognitive side effects of medication on attention and executive functions in patients with epilepsy. Epilepsy Behav. 2005;7:708–14.
Helmstaedter C. EpiTrack® – Veränderungssensitives kognitives Screening zur Beurteilung der Aufmerksamkeit und der Exekutivfunktionen für die Qualitäts- und Ergebniskontrolle der Behandlung von Patienten mit Epilepsie. 3. Auflage. 2019. https://www.eisai.de/fachkreise/neurologie/service/#EpiTrack. Accessed 12 Oct 2022.
Meschede C, Witt J, Rademacher M, Von WRD, Elger CE, Helmstaedter C. Evaluating the longer-term cognitive effects of adjunctive perampanel compared to lacosamide in a naturalistic outpatient setting. Seizure Eur J Epilepsy. 2018;58:141–6.
Helmstaedter C, Witt J-A. The longer-term cognitive effects of adjunctive antiepileptic treatment with lacosamide in comparison with lamotrigine and topiramate in a naturalistic outpatient setting. Epilepsy Behav. 2013;26:182–7.
Helmstaedter C, Witt J-A. Cognitive outcome of antiepileptic treatment with levetiracetam versus carbamazepine monotherapy: a non-interventional surveillance trial. Epilepsy Behav. 2010;18:74–80.
Helmstaedter C, Witt J-A. The effects of levetiracetam on cognition: a non-interventional surveillance study. Epilepsy Behav. 2008;13:642–9.
Witt J-A, Elger CE, Helmstaedter C. Short-term and longer-term effects of brivaracetam on cognition and behavior in a naturalistic clinical setting—preliminary data. Seizure. 2018;62:49–54.
Witt J-A, Elger CE, Helmstaedter C. Adverse cognitive effects of antiepileptic pharmacotherapy: Each additional drug matters. Eur Neuropsychopharmacol. 2015;25:1954–9.
Helmstaedter C, Elger CE, Witt JA. The effect of quantitative and qualitative antiepileptic drug changes on cognitive recovery after epilepsy surgery. Seizure. 2016;36:63–9.
Etz A, Gronau QF, Dablander F, Edelsbrunner PA, Baribault B. How to become a Bayesian in eight easy steps: an annotated reading list. Psychon Bull Rev. 2018;25:219–34.
Acknowledgements
Preliminary data of this project have been presented as scientific poster at the First Congress of the European Academy of Neurology [22]. We thank Karen Wörmann for proof-reading and language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the conduct or publication of this study. Open Access funding enabled and organized by Projekt DEAL.
Conflict of interest
RvW has received fees as speaker, consultant or travel support by Arvelle, Cerbomed, Desitin, GW Pharmaceuticals/JAZZ pharma, Eisai and UCB. CH reports honoria for speeches, webinars, counseling, etc. from UCB, Eisai, Angelini, GW, Precisis, Jazz Pharma, honoraria for expert testimonies, as well as license fees from UCB and Eisai. JAW, GW, NH, and CEE have no conflicts of interest to declare.
Ethics approval
The study has been approved by the ethics committee of the medical faculty of the University of Bonn (180/15).
Consent to participate
All participants provided written informed consent.
Consent for publication
Not applicable.
Availability of data and material
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
CH and GW conceptualized the study. GW, NH, RW, and CEE were involved in the acquisition of patients. JAW performed the data analysis and prepared the first draft of the manuscript. All authors revised the manuscript for intellectual content, approved the final version of the manuscript and are accountable for their work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Witt, JA., Widman, G., Hansen, N. et al. Evaluation of a Rapid Topiramate Titration Scheme for the Early Detection of Cognitive Side Effects. CNS Drugs 36, 1325–1330 (2022). https://doi.org/10.1007/s40263-022-00969-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-022-00969-3