Abstract
Electroconvulsive therapy (ECT) is an effective treatment for severe psychiatric disorders. Patients referred to ECT are often taking multiple medications, many of which can potentially affect the safety and efficacy of their course of ECT. This review evaluates the impact of a variety of psychotropic medications often used in conjunction with ECT and examines strategies to optimize their management. The review encompasses mood stabilizers, antidepressants, benzodiazepines, antiepileptics, antipsychotics, and other commonly used psychotropics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Navigating electroconvulsive therapy (ECT) and concomitant psychotropic use in patients with severe psychiatric illnesses can be challenging. |
Certain psychotropic medications used during ECT can affect seizure thresholds, seizure propagation, and ECT safety and efficacy. |
The majority of psychotropic medications can be safely administered along with ECT; however, continued evaluation of risks versus benefits is indicated to optimize treatment. |
1 Introduction
Electroconvulsive therapy (ECT) is highly effective in the treatment of severe mood and psychotic disorders requiring rapid improvement or manifesting relative resistance to pharmacotherapy [1]. ECT is also effective in pharmacotherapy refractory medical conditions, including neuroleptic malignant syndrome, status epilepticus, and behavioral disturbances in dementia [2,3,4]. Patients who present to ECT are often taking multiple psychotropic medications after not responding to pharmacotherapy (for example, see Kellner et al. [5] and Beale and Kellner [6]). In fact, the recent US FDA guidelines for ECT call for ECT to be administered in treatment-resistant depression (TRD) [2].
Thirty years ago, ECT was primarily an inpatient procedure and the common practice was to discontinue psychotropic medications prior to beginning an ECT course. However, the lengths of psychiatric hospitalizations have decreased dramatically and ECT is increasingly shifting to an outpatient procedure [7,8,9]. Medication ‘washouts’ are more complicated and, in many cases, impractical due to the pressures to initiate treatment quickly and the difficulty of discontinuing medications abruptly in this patient population.
Many of the medications used during ECT increase the seizure threshold or impede seizure propagation (e.g. benzodiazepines and anticonvulsants), and other psychotropics may decrease the seizure threshold (e.g. antipsychotics and antidepressants). Using techniques such as stimulus titration to determine the seizure threshold for an individual patient may mitigate the impact of concomitant medication on maintaining an adequate stimulus dose. However, ECT practitioners also need to know if concomitant medications may cause other adverse effects or influence the efficacy of a course of ECT. The efficacy of ECT is clearly correlated with the quality of the ECT-induced seizure [10] and it would be reasonable to assume that an anticonvulsant medication could potentially influence the seizure threshold, quality, and duration. Medications that could decrease the seizure threshold may potentially cause longer seizures and associated adverse effects.
Understanding the impact of concomitant psychotropic medication on the efficacy and safety of ECT is the focus of this review. A PubMed query was completed reviewing current and past literature regarding psychotropic use during ECT. Search queries include names of different psychotropic medications and ECT. There were no date restrictions used in the query.
2 Anticonvulsant Medications
ECT efficacy is determined by the relationship of the ECT stimulus dose to the seizure threshold [11]. Several factors impact the seizure threshold, which is increased with bilateral versus unilateral ECT, older age, and male sex [12]. Anticonvulsant medications also affect seizure thresholds [13] and may therefore affect both the efficacy and safety of ECT. Anticonvulsant medication used during ECT could potentially affect the seizure quality and length, and lead to missed or inadequate seizures.
The efficacy of ECT is primarily correlated with the quality of the seizure (e.g. ictal activity and postictal suppression [14]) and not necessarily the length of the seizure [15]. However, missed or very short seizures (< 15 s) are also practical problems that need to be addressed. Clearly, to be effective, the ECT stimulus must elicit a seizure [16, 17] and, in the case of unilateral ECT, the stimulus must be significantly suprathreshold [11].
The primary anticonvulsant medications used in patients receiving ECT include the non-benzodiazepine antiepileptic drugs (AEDs) and benzodiazepines themselves. Abruptly stopping benzodiazepines in a severely depressed patient can be difficult, particularly in an outpatient setting. Patients with bipolar disorder and mood instability often present to ECT while taking anticonvulsant medications and/or benzodiazepines, which are used as mood stabilizers and to treat associated anxiety. AEDs are also used during a course of ECT to prevent a depressed bipolar patient from cycling into mania [18]. Older retrospective chart reviews demonstrated the potential for ECT treatments and antidepressants to increase mood switches to mania in bipolar patients [19]. Although there are data from more recent trials showing ECT rarely induces mania [20, 21], many patients are continued on AEDs and benzodiazepines during a course of ECT.
2.1 Antiepileptic Drugs
In a retrospective, single-site study of 550 patients, investigators examined the effect of benzodiazepines and AEDs on the initial titrated seizure length and threshold, and found that these medications were associated with no significant changes in seizure characteristics or ECT parameters [22]. A large retrospective study [13] and one prospective study [23] also found no relationship between AEDs and initial seizure threshold. However, as van Waarde et al. point out [23], in large studies that do not control the medications patients are taking, patients are often taking drugs that may both increase (e.g. antiepileptics and benzodiazepines) and decrease (e.g. tricyclic antidepressants and antipsychotics) the seizure threshold, cancelling out each other’s effects.
Virupaksha et al. [24] evaluated 201 consecutive admissions of patients with bipolar disorder (depressed, manic, or mixed states) treated with ECT and compared patients who were either taking AEDs or not taking concomitant AEDs. The patients taking AEDs had significantly higher seizure thresholds, shorter motor seizures and an increased number of missed seizures, higher maximum charge received during the ECT course, and required an increased number of treatments during the ECT course. Although both groups had similar clinical outcomes, the AED group had longer hospital stays. Other studies of specific AEDs are outlined below.
2.1.1 Sodium Valproate and Carbamazepine
Jahangard et al. compared the efficacy of ECT in bipolar disorder, manic phase, with and without concurrent use of sodium valproate [25]. Forty-two patients with mania were randomly assigned to either sodium valproate (minimum dose of 750 mg/day) or the control group (sodium valproate discontinuation). All patients underwent bifrontal ECT for a minimum of six sessions. Manic symptoms significantly improved over time regardless of group. Concomitant sodium valproate did not negatively impact or improve the efficacy of ECT.
Rakesh et al. [26] conducted a randomized control trial (RCT) to assess clinical improvement and adverse cognitive effects in bipolar patients receiving ECT alone versus ECT and AEDs, specifically carbamazepine and sodium valproate. Patients were randomized into three groups: full-dose AED (FD), half-dose AED (HD), or discontinue AED. Thirty-six patients with bipolar disorder, currently manic, were randomized and there were no differences across the three groups when assessing the primary outcomes, although patients in the FD group improved faster than patients in the HD group. There were no differences across the groups in the context of cognitive adverse effects. Additionally, seizure parameters did not vary across the groups.
2.1.2 Lamotrigine
Lamotrigine is FDA-approved as a maintenance medication for recurrent depression in patients with bipolar disorder. Patients with bipolar disorder may be receiving lamotrigine, or may be started on lamotrigine, as a maintenance medication during a course of ECT.
In a case series of nine patients with acute bipolar depression, lamotrigine was titrated to doses ranging from 25 to 225 mg/day (with a mean dose of 102.8 mg) during the acute and maintenance ECT course [27]. There was no significant change in mean seizure duration or time to reorientation in patients from the lowest to highest doses of lamotrigine, and lamotrigine was well tolerated with no serious adverse events.
In a retrospective study, Sienaert et al. [28] found that lamotrigine was not associated with a higher stimulus dose or a decreased seizure duration in 19 patients receiving ECT. In this study, eight patients were prescribed lamotrigine at doses > 200 mg/day. The study did however find that patients taking concomitant lamotrigine with ECT were more likely to have missed seizures. Additionally, in a retrospective review of 187 patients, Joo et al. found that benzodiazepine dose, lamotrigine use (range of 6.25–200 mg/day), and older age were associated with decreased motor seizure duration during ECT [29]. Lamotrigine may therefore be associated with a decrease in seizure length and more missed seizures.
2.1.3 Topiramate and Gabapentin
Topiramate and gabapentin are AEDs with no reports of their impact on safety or efficacy in the context of concomitant use during ECT.
Conclusion: There are no clear contraindications to continuing AEDs during a course of ECT. There may however be a risk for missed seizures and an increase in the number of seizures required to reach remission during a course of ECT with concomitant AEDs. The evidence is somewhat mixed as other studies have found that AEDs are associated with improved efficacy and no significant adverse events. Using the dose-titration method and holding the medication the night before and the morning of the ECT treatment can mitigate the effects on the seizure threshold. More prospective studies are needed to make more definitive guidelines on the use of AEDs in patients receiving acute and maintenance ECT.
3 Benzodiazepines
Patients who present for ECT are often taking benzodiazepines to control anxiety, mania, and/or catatonia. Benzodiazepines are associated with decreased ECT-associated seizure length, but are not associated with a significant decrease in seizure threshold in some studies [12, 13]. Another large study reported no effect of benzodiazepines on seizure length or threshold [22].
Although seizure duration is not associated with efficacy, decreases in seizure duration can result in missed or short seizures [12, 15, 30]. One strategy has been to limit benzodiazepines or block the benzodiazepine receptor with flumazenil prior to initiating the stimulus [31, 32]. The pharmacodynamics of flumazenil are such that a dose of 0.1–0.2 mg produces partial agonism of the benzodiazepine receptor, and a dose of 0.4–1.0 mg produces nearly complete blockade of the receptor (https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=436f5616-9626-4b6a-9deb-2986444179d0&type=display). Flumazenil is typically administered after the patient is sedated to minimize the potential for benzodiazepine withdrawal symptoms in an awake patient. However, the time between the anesthesiologist administering the sedating anesthetic medication (e.g. methohexital or propofol) and seizure initiation is only 2–3 min. Only 80% of the effect of flumazenil is apparent at 3 min and a peak effect occurs at 6–10 min (). Flumazenil therefore provides only a partial blockade of the receptor during the ECT stimulus.
In a retrospective study, concomitant benzodiazepines did not decrease the response to bitemporal ECT [33]. This study used the half-age method to dose ECT, therefore the investigators could not analyze the effect of benzodiazepines on the seizure threshold. Another retrospective study of patients receiving right unilateral ECT for major depression used an algorithm to determine stimulus dose [30]. In this study, there was a decrease in the number of responders in the group taking benzodiazepines, and a significant increase in the final depression scores in the patients taking benzodiazepines who were responders, indicating more residual symptoms in the benzodiazepine group. Interestingly, the non-responders in the benzodiazepine group who were switched to bilateral ECT had an 82% response rate (9/11) after an average of only five bilateral ECT treatments. Similarly, Jha and Stein found that concomitant benzodiazepines used during an ECT course decreased the response to right unilateral ECT and resulted in longer hospital stays, but did not affect the efficacy of bilateral ECT [34].
In a recent retrospective study of 70 patients (22 taking concomitant benzodiazepines) receiving bitemporal ECT using a dose-titration method, the benzodiazepine group had a significantly higher rate of response than the non-benzodiazepine group [35]. There were no differences in the two groups in terms of seizure thresholds or duration of the ECT-induced seizures.
Conclusion: These studies support the hypothesis that concomitant benzodiazepines may affect the response to unilateral and bilateral ECT differentially [36]. This dichotomy would at least argue for a course of bilateral ECT in patients taking benzodiazepines and not responding to a course of right unilateral ECT.
4 Antipsychotics, Antidepressants, Lithium, and Stimulants
The antidepressants, antipsychotics, lithium, and stimulants are associated with, to varying degrees, lowering the seizure threshold. The concern with these medications is their potential for producing prolonged seizures, leading to postictal confusion or increased cognitive problems. Continuing these medications during a course of ECT is common as ECT patients are often using these medications when they present for ECT and the medications may be important to keep them stable during ECT.
Initiating antidepressants during ECT, including lithium, may decrease the risk of early relapse, which is especially high in the first few weeks following a successful course of ECT [37]. In addition, many patients receiving maintenance ECT will be kept on adjunctive antidepressants and antipsychotics. Understanding the potential therapeutic effects of these medications and the risks associated with them during ECT is important.
4.1 Antipsychotics
ECT has been used as an augmentation strategy in patients with mood disorders and psychosis [38], and the combination of an antipsychotic with ECT has been shown to be effective in treatment-resistant schizophrenia [39,40,41,42,43,44,45,46,47]. A meta-analysis of RCTs in patients receiving ECT and taking concomitant antipsychotic medications (except clozapine) showed that the combination was effective in treatment-resistant schizophrenia, but was associated with more memory impairment and post-ECT headaches than ECT alone [48].
There are other concerns about the combination of ECT with antipsychotics, particularly phenothiazines and clozapine, given the potential impact on the seizure threshold and the risk for prolonged seizures. In a review of 208 patients (primarily diagnosed with schizophrenia and schizoaffective disorder) who received a combination of clozapine and ECT, Grover et al. [49] found the combination was generally well tolerated, with only five patients experiencing delirium and four patients with prolonged seizures. Other reports of clozapine prescribed during a course of ECT have also found it to be well tolerated and effective [50].
Petrides et al. conducted an 8-week, single-blind study of clozapine versus clozapine and ECT in patients diagnosed with schizophrenia who previously did not respond adequately to clozapine alone [42]. The ECT group received bilateral ECT three times per week for 4 weeks and then twice a week for 4 weeks. At the end of the trial, 50% of the ECT group met the response criteria but none of the patients in the clozapine-only group. Subjects who did not meet the response criteria could crossover to an 8-week trial of ECT; of the patients who crossed over, 47% met the response criteria. ECT was well tolerated and few adverse effects were reported.
Conclusion: The combination of antipsychotics and ECT appears to be generally well tolerated and effective in the treatment of schizophrenia that has been resistant to pharmacotherapy. Patients should be monitored closely for cognitive problems, including emergent delirium, and there is at least a potential for prolonged seizures. The data on the combined use of ECT and antipsychotics in mood disorders are less well researched.
4.2 Antidepressants
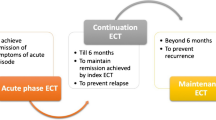
ECT is widely recognized as one of the most effective antidepressant treatments, even in patients with TRD [1]; however, relapse prevention after an acute course of ECT has remained a significant challenge. Relapse rates are generally reported in the range of 50% within the first 6 months after an acute course of ECT [37, 51, 52]. The need for carefully planned continuation therapy strategies is compelling and should be considered early in the acute ECT course. The use of antidepressant medications for the purpose of treatment augmentation and relapse prevention is discussed below, along with the potential adverse effects of using comorbid antidepressants during a course of ECT.
4.2.1 Tricyclic Antidepressants
Recent research combining ECT and antidepressant medications has focused on relapse rates and short-term antidepressant effects of ECT. Many of these studies, which included tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) and were conducted in the 1950s and 1960s, were inconclusive due to multiple methodological issues, including retrospective designs, small sample sizes, lack of controls, low medication doses, and flawed outcome assessments [53,54,55]. TCAs pose a potential risk of cardiovascular or anticholinergic toxicity, particularly at higher doses. TCAs have also been associated with a longer electroencephalogram (EEG) seizure duration [22]; however, TCAs have generally been found to be well tolerated when combined with ECT at therapeutic doses [56, 57].
A retrospective study conducted in 1989 of 84 patients with major depression found that patients who received a combination of ECT and nortriptyline treatment had better acute antidepressant outcomes than those receiving ECT alone [57]. The effect was graded as the study included a low-dose TCA group and A therapeutic-dose TCA group. Patients in the therapeutic-dose TCA group required significantly fewer ECT treatments than the group that received only ECT (8.1 vs. 9.8 treatments). There was no difference between the two groups in terms of adverse effects or safety. A study from 2009 found the concurrent use of nortriptyline, and, to a lesser extent, venlafaxine, increased acute ECT response rates. In addition, patients receiving concurrent nortriptyline (but not venlafaxine) had improved short-term cognitive outcomes following ECT [58].
Much of the focus of the research using concomitant antidepressants with ECT has been on improving the relapse rates following ECT. Prudic et al. found that starting nortriptyline or venlafaxine at the beginning of an ECT course did not improve depression relapse rates [52]. A separate RCT compared placebo, nortriptyline, and nortriptyline + lithium administered after a successful acute course of ECT and showed 6-month relapse rates of 84%, 60%, and 39%, respectively [56]. The study showed that without active continuation treatment, almost all patients relapsed within 6 months after an index ECT course.
In another RCT, when lithium was added to nortriptyline or venlafaxine following the index ECT course, both the nortriptyline + lithium and venlafaxine + lithium groups had a 6-month relapse rate of 50%, similar to the 39% relapse rates with nortriptyline + lithium found in the 2001 study by Sackeim et al. cited above [56], and comparable to the 6-month relapse rates reported with a continuation ECT (cECT) protocol [59]. A recent multisite study [60] prospectively assigned 120 elderly patients who remitted with ECT to receive continuation pharmacotherapy with venlafaxine + lithium alone or combined with an individualized cECT protocol. The combined pharmacotherapy and cECT group was 1.7-fold more likely to remain in remission after 6 months than the pharmacotherapy-alone group (13.1% vs. 20.3%).
4.2.2 Monoamine Oxidase Inhibitors
There has been an ongoing concern related to the use of MAOIs in the context of general anesthesia and ECT, with general guidelines recommending a 2-week washout period prior to starting ECT. This recommendation does not match the very limited available evidence.
Dolenc et al. published four case reports and found no evidence of adverse effects in patients taking MAOIs during a course of ECT [61]. All case reports in this publication included the use of tranylcypromine and found no major changes in seizure length or reports of autonomic instability. The largest case series evaluating concomitant MAOIs during a course of ECT included 100 patients randomized to phenelzine versus placebo. This study concluded that there was increased antidepressant response in the phenelzine group and reported no major complications [62].
4.2.3 Selective Serotonin Reuptake Inhibitors
There is evidence that selective serotonin reuptake inhibitors (SSRIs) may increase the seizure length; however, this increase does not appear to be clinically significant [63] and the SSRIs have been associated with increased postictal suppression [63], which has been correlated with clinical efficacy [64, 65].
A double-blind RCT in 1996 compared outcomes in depressed patients, with and without cardiac disease, receiving ECT, placebo, or concomitant pharmacotherapy [66]. Thirty patients with cardiac disease were assigned to ECT and placebo or 30 mg paroxetine, while 52 patients without cardiac disease were assigned to ECT and 30 mg paroxetine or 150 mg imipramine. There was no difference in short-term outcomes between the paroxetine and placebo groups in relation to the cardiac patients. However, in the group without cardiac disease, those treated with ECT and imipramine had better short-term outcomes than those receiving ECT and paroxetine, as demonstrated by lower depression scores. Moreover, in the continuation phase, patients receiving paroxetine had lower relapse rates than those receiving imipramine or placebo.
In a 2006 retrospective review of patients taking antidepressants during a course of ECT, Baghai et al. found that seizure duration was unaffected by most antidepressants, except for SSRIs, which increased the mean EEG seizure duration to a modest degree [63]. The postictal suppression index was lower on mirtazapine and higher (better) with SSRIs and serotonin norepinephrine reuptake inhibitors (SNRIs). Nonetheless, the response rate, as measured by the Clinical Global Improvement (CGI) scale, was significantly lower (improved mood) in patients receiving concomitant mirtazapine and SSRIs compared with those receiving no pharmacotherapy. Importantly, there were no serious adverse events.
4.2.4 Serotonin and Norepinephrine Inhibitors
Early reports found that the SNRI venlafaxine at high doses (300 mg or more) was associated with transient asystole when combined with propofol anesthesia [67]. Baghai et al. [63] also reported higher rates of transient cardiovascular adverse effects in patients receiving a mean dose of 225 mg of venlafaxine.
Concomitant venlafaxine during an acute course of ECT was also associated with increased cognitive adverse effects and a lower rate of improvement compared with nortriptyline [58], although the combination of venlafaxine and lithium was both well tolerated and effective as a maintenance medication in the elderly after a successful course of ECT [60].
4.2.5 Bupropion
Bupropion has the potential to lower the seizure threshold, therefore the combination of bupropion and ECT has raised concerns that the combination may cause prolonged seizures [68,69,70]. A retrospective chart review compared patients treated with ECT alone and those treated with ECT with concomitant bupropion [71]. Surprisingly, patients on ECT and bupropion had significantly shorter motor and EEG seizure durations and an equivalent number of treatments, with no increase in prolonged seizures. A second retrospective review found concomitant bupropion had no effect on the initial seizure threshold or duration [22], while another 2016 review highlighted the proconvulsant nature of bupropion and advised a dose-related seizure risk approach [72]. Additionally, extended-release formulations were advised to prevent variable peak serum concentrations. Therefore, from the limited data available, therapeutic doses of bupropion appear to be well tolerated when administered with ECT, although caution is appropriate and it is important to be mindful of the dose-dependent seizure risk with bupropion [73].
Conclusion: Antidepressants may provide significant benefit in preventing relapse after a course of ECT. The benefits of starting an antidepressant prior to the start of or during a course of ECT appear to outweigh the risks, although caution should be observed when the patient is receiving high doses of the antidepressant, particularly bupropion and venlafaxine. While there are no reports of adverse effects of patients taking MAOIs during a course of ECT, the studies are limited. MAOIs may also pose a risk of hypertensive crisis in patients who are administered, for example, medications to support their blood pressure in recovery from ECT. Patients receiving MAOIs during ECT should be identified clearly during their course of ECT.
4.3 Lithium
ECT is not associated with a significant change in lithium distribution or pharmacokinetics, or interactions with drugs used during ECT (e.g. barbiturate anesthetics) [74], although lithium may lower the initial seizure threshold [13]. Early reports of patients taking lithium during a course of ECT cited an increased risk of delirium [75,76,77], prolonged apnea [78,79,80], and spontaneous seizures [81]. By 1985, the consensus was that patients should be lithium-free prior to the initiation of ECT [82].
Stopping lithium abruptly prior to ECT may have significant clinical consequence. Lithium has been shown to be an effective maintenance medication after ECT [56, 60, 83,84,85,86] and can be used as a mood stabilizer for patients with bipolar disorder who are receiving ECT. A 2005 review by Dolenc and Rasmussen [87] showed the safe and effective use of lithium and ECT in 12 patients with lithium levels between 0.3 and 1.4 mEq/L. A recent literature review examining factors associated with delirium following ECT did not find a relationship with any medications, including lithium, in the eight studies that addressed concomitant medication [88]. Patient characteristics (e.g. dementia), bitemporal electrode placement, and higher stimulus intensity were more salient variables in determining treatment-emergent delirium.
A prospective comparison of 55 inpatients with diverse psychiatric diagnoses (schizophrenia, non-organic psychosis, mania, and depression) who received ECT, compared patients who were either taking (n = 27) or not taking (n = 28) lithium. Thirthalli et al. found no significant difference in the two groups in terms of seizure variables, apnea time, or recovery from anesthesia [89]. Cardiovascular measures, including average maximum heart rate, average maximum systolic blood pressure, and average maximum rate pressure product, were significantly lower in patients who had combined lithium and ECT. In lithium-treated patients, the average time to post-ECT recovery, which can be an early sign of ECT-associated delirium when prolonged, was positively correlated with serum lithium levels. The investigators concluded that if lithium is continued during ECT, then maintaining the lithium level in the low therapeutic range and in patients with relatively low-risk profiles for delirium (i.e. young patients without baseline cognitive complications) will increase the safety of lithium use during ECT administration.
Perugi et al. conducted a review of 522 consecutive patients diagnosed with bipolar disorder, including patients with depression, mania, mixed states, and catatonia [21]. In this naturalistic study, anticonvulsant medications, including sodium valproate or carbamazepine, were discontinued and antidepressant and antipsychotic treatments were kept stable for at least 1 week before and during the ECT course. Lithium was allowed and the dose was reduced to maintain a level of 0.3–0.4 mEq/L, and was not administered the night before ECT. Benzodiazepines were allowed to a dosage equivalent of up to 3 mg/day of lorazepam. They demonstrated a clinically significant response in approximately two-thirds of patients who were pharmacotherapy-resistant, and did not find evidence of mood destabilization or cycling into mania or severe adverse events.
In a recent sample of 64,728 adult US psychiatric inpatients, Patel et al. examined the odds of delirium and cognitive problems associated with ECT and lithium [90], and found a higher prevalence of delirium in the lithium and ECT group (5.7%) versus ECT alone (0.6%) and lithium alone (0%). Patients treated with ECT and lithium had 11.7 higher odds of delirium compared with the ECT-alone group. Further stratification by diagnosis found the prevalence of delirium was 7.8% in unipolar depression, 3.4% in bipolar depression, and 0.0% in bipolar mania. These results support caution when prescribing lithium in patients receiving ECT, but unfortunately do not provide guidance on the safety of low-dose versus high-dose lithium with concomitant ECT.
Conclusion: There is evidence that concomitant lithium with ECT may also be associated with potential adverse events, most notably postictal delirium. Other reports have associated lithium and ECT with prolonged seizures, toxic lithium levels, and neuromuscular blockade [91]. Careful consideration of the risks/benefits of continuing lithium during ECT should include evaluating the vulnerability of the particular patient to ECT-related cognitive problems (e.g. older age, baseline cognitive status) and monitoring patients carefully for early signs of emerging ECT-related cognitive problems (i.e. longer post-ECT recovery times). If lithium is continued during ECT, then decreasing the lithium level to the range that is most effective for antidepressant treatment (0.4–0.6 mEq/L) and holding the dose of lithium the night before and the morning of each ECT treatment may decrease the potential for adverse events.
4.4 Stimulants
The use of methylphenidate and dexamphetamine, as well as stimulant-like drugs such as modafinil and armodafinil, is becoming more widespread to address apathy and mood symptoms in late-life and TRD [92]. Stimulants such as methylphenidate have the potential to lower the seizure threshold and lead to prolonged seizures, although a systematic chart review did not show an effect of stimulants on the initial titrated seizure length or threshold [22]. An additional consideration is that stimulants may produce dysrhythmias and hypertension [93], although there are no RCTs of concomitant stimulant use in ECT.
Conclusion: Although not an absolute contraindication, holding stimulants until after the ECT course may limit any potential cardiac complications.
5 Other Psychotropic Medications
5.1 Acetylcholinesterase Inhibitors
Geriatric patients with pre-existing cognitive impairment may be referred for ECT while taking acetylcholinesterase inhibitors (AchEIs). AchEIs have been effective in decreasing the cognitive adverse effects of ECT [94]; however, there are also concerns that this class of drugs could potentially interact with succinylcholine, prolonging paralysis and leading to potential complications such as apnea and bradycardia associated with the increased cholinergic tone from ECT [95, 96].
In a 2017 review of the available literature, Henstra et al. found that the five available clinical trials showed significantly better cognitive performance in individuals treated with AchEIs during ECT [97]. There were no significant adverse events or effects on ECT seizure parameters. In a case report, donepezil was shown to decrease cognitive impairment in patients undergoing maintenance ECT, with no significant adverse effects [98]. An RCT comparing donepezil with placebo also found that post-ECT recovery time was also significantly improved in patients taking donepezil [99]. Two case reports found that post-ECT delirium was reduced or controlled with the addition of donepezil [100, 101].
Conclusion: Despite the potential for an interaction with succinylcholine, the limited database on AchEIs show they are well tolerated in ECT and may provide some cognitive benefits.
5.2 Ketamine
Ketamine is an N-methyl-d-aspartate receptor antagonist that when administered intranasally or intravenously at a subanesthetic dose has been demonstrated to produce a rapid and significant antidepressant response in major depression and suicidal ideation [102, 103]. When compared with other anesthetics used in ECT, ketamine may have less effect on the seizure threshold and overall seizure quality [104]. In fact, both ketamine and etomidate may have advantages as anesthetic agents as they are less anticonvulsant than methohexital, thiopental, and propofol, and may have a decreased effect on the seizure threshold, duration, and quality [105]. Additionally, in a retrospective analysis of patients receiving a total of 3239 ECT-induced seizures at one site in Germany, the investigators found that in ECT-induced seizures using ketamine and etomidate anesthesia, the EEGs had a higher seizure quality and longer motor activity compared with seizures using methohexital and propofol anesthesia [106]. However, concerns have been raised about the adverse effect profile of ketamine and whether it has clear advantages in relation to the other anesthetic medications. Ketamine has been associated with adverse effects post ECT, including nausea, dizziness, vomiting, vertigo, and psychotomimetic effects [107].
In a multicenter randomized trial, 79 patients were randomized to adjunctive ketamine (0.5 mg/kg intravenous bolus) or saline with their anesthetic during a course of ECT [108]. There were no advantages in the ketamine group in relation to neuropsychological or clinical outcomes. In an RCT in which 18 patients received either thiopental alone or with ketamine (0.5 mg/kg), or thiopental alone, there was no enhancement of the antidepressant effect in the ketamine group [109]. Finally, in an RCT comparing thiopental anesthesia and adjunctive ketamine or saline, Loo et al. found ketamine was well tolerated but did not differ from saline in terms of impact on neuropsychological measures following ECT [110]. The ketamine group did show a small but significant advantage in efficacy measures in the first week of the ECT course, but both groups eventually had the same antidepressant response.
While ketamine could potentially have positive effects on cognition and mood during a course of ECT compared with standard anesthetics such as methohexital, this was not demonstrated in an RCT comparing methohexital and ketamine as anesthetic agents [111]. In contrast, an RCT comparing 29 patients randomized to either thiopental or ketamine found the ketamine patients showed an earlier response in depressive symptoms (although both groups improved significantly) and was associated with a better cognitive performance [as measured by the Mini-Mental State Examination (MMSE)] and longer seizure duration [112]. Despite this positive study, two later meta-analyses of RCTs comparing ketamine as the sole anesthetic or added to other anesthetic agents during ECT did not find evidence of improved neurocognitive or antidepressant outcomes with ketamine compared with barbiturate or propofol anesthesia [113, 114]. While there is evidence to support an earlier response to ECT, the overall response rates showed no difference and ketamine was associated with cardiovascular changes (i.e. increased blood pressure), psychotomimetic experiences (e.g. dissociation), and vestibular adverse effects (e.g. vertigo) that may complicate compliance and patient management.
Conclusion: Ketamine is not recommended as a routine anesthetic in ECT but may have a role when it is difficult to elicit a seizure, as long as the patient is tolerating the procedure and is not psychotic or at risk of dissociative episodes in recovery.
6 Discussion
Management of concomitant psychotropic medications during a course of ECT requires balancing the risks of continuing medications that may have adverse effects or interactions, with the ECT procedure, versus stopping medications and destabilizing a patient’s psychiatric status and losing potential benefits in augmenting response or maintaining benefit after ECT. Stopping certain medications may also result in discontinuation adverse effects, delays in initiating ECT, or decreased compliance with treatment.
The effects of medications on seizure threshold may be overshadowed by intrinsic factors, which may account for as much as a 50-fold variation in seizure thresholds across patients. These include factors such as age, sex, medical illness, hydration status, weight and duration of mood disorder and history of ECT [12]. Using a stimulus dose-titration method allows the practitioner to individualize the stimulus dose and incorporates all these variables, including medication.
Anticonvulsant medications can lead to missed or inadequate seizures. Strategies to manage inadequate seizures include stimulating at a higher dose, holding anticonvulsant medication the night before and the morning of ECT, using adjunctive short-acting opiates (e.g. remifentanil and alfentanil) in order to lower the barbiturate dose, changing anesthetics to ketamine or etomidate, adding flumazenil for patients on high doses of benzodiazepines, and vigorous hyperventilation [1].
Proconvulsant medications can lead to prolonged seizures with associated complications, including postictal delirium. Again, the use of stimulus dose titration to determine the seizure threshold can personalize the treatment parameters and reduce the risk of excessive stimulus doses.
Limited data suggest that certain antidepressants, including TCAs, may augment the acute antidepressant response to ECT. These and other antidepressants appear to be generally well tolerated with ECT, and there is a theoretical rationale to start antidepressants for continuation treatment early in the ECT course. However, case report literature would advise caution with high doses of venlafaxine and, by inference, other SNRIs during ECT.
The extant data suggest that antipsychotics, including clozapine, can be used safely with ECT. In addition, ECT has been shown to augment antipsychotic response, even in patients diagnosed with schizophrenia who have not responded to clozapine. The data for patients with mood disorders taking antipsychotics during a course of ECT are less clear.
The management of lithium during a course of ECT involves the most subtleties when determining the risk/benefit ratio. Clearly there are reports of serious complications in patients taking lithium while receiving ECT. However, lithium is also a valuable medication to use in maintenance after ECT and an excellent mood stabilizer in patients with unipolar as well as bipolar disorder. Discontinuing lithium in all patients receiving ECT, and waiting five half-lives before starting ECT, could take 5 days or more depending on renal function. Practical considerations include holding the evening and morning doses in patients receiving ECT, maintaining lower blood levels (0.4–0.6 mEq/L) for depressed patients, and monitoring patients carefully for evidence of delirium (e.g. longer recovery times).
Determining which psychotropic medications should be started, continued, or stopped involves a careful and comprehensive evaluation of the entire clinical picture for each patient starting a course of ECT.
7 Conclusions
There are multiple reasons why psychotropic medications may be continued or added during a course of ECT—avoidance of discontinuation effects, management of intercurrent symptoms, as part of an augmentation or relapse prevention strategy, or at times for unrelated medical reasons (as in patients with seizure disorder). Prescribing psychotropic medications during ECT is challenging since certain medications may significantly impact the safety or efficacy profile of ECT. It is important to be mindful of individual risks versus benefits of each medication. Many psychotropic medications can be safely administered during ECT, including antiepileptics, antipsychotics, and AchEIs; however, it is advisable to limit the use of benzodiazepines and stimulants in order to optimize ECT. Lithium and certain antidepressants have been shown to be well tolerated and likely can help reduce relapse after a course of ECT, although it is prudent to keep lithium dose and levels as low as clinically feasible during the ECT course. Close monitoring is advised, especially with bupropion, venlafaxine, and MAOIs. Continued review of risks versus benefits, openness to change of treatment algorithms, and careful attention to a number of factors, including stimulus dosing, seizure characteristics, and treatment-related adverse effects, is essential to maximize the likelihood of favorable outcomes.
References
McDonald WM, Meeks TW, Carpenter LL, McCall WV, Zorumski CF. Electroconvulsive therapy and other neuromodulation therapies. In: Schatzberg AF, Nemeroff CB, editors. Textbook of psychopharmacology. 5th ed. Washington, DC: American Psychiatric Press; 2017. p. 861–899.
McDonald WM, Weiner RD, Fochtmann LJ, McCall WV. The FDA and ECT. J ECT. 2016;32(2):75–7. https://doi.org/10.1097/YCT.0000000000000326.
Hermida AP, Tang YL, Glass O, Janjua AU, McDonald WM. Efficacy and safety of ECT for behavioral and psychological symptoms of dementia (BPSD): a retrospective chart review. Am J Geriatr Psychiatry. 2020;28(2):157–63. https://doi.org/10.1016/j.jagp.2019.09.008.
The Practice of Electroconvulsive Therapy: Recommendations for treatment, training and privileging. Task Force Report of the American Psychiatric Association, 2nd ed. Washington, DC: American Psychiatric Association; 2001.
Kellner CH, Greenberg RM, Murrough JW, Bryson EO, Briggs MC, Pasculli RM. ECT in treatment-resistant depression. Am J Psychiatry. 2012;169(12):1238–44. https://doi.org/10.1176/appi.ajp.2012.12050648.
Beale MD, Kellner CH. ECT in treatment algorithms: no need to save the best for last. J ECT. 2000;16(1):1–2.
Canadian Agency for Drugs and Technologies in Health. Delivery of electroconvulsive therapy in non-hospital settings: a review of the safety and guidelines. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2014.
Sato M, Hirota K, Shirakami G, Kakuyama M, Tanabe H, Fukuda K. Safety in general anesthesia for ambulatory electroconvulsive therapy (in Japanese). Masui. 2013;62(1):52–9.
Reti IM, Walker M, Pulia K, Gallegos J, Jayaram G, Vaidya P. Safety considerations for outpatient electroconvulsive therapy. J Psychiatr Pract. 2012;18(2):130–6. https://doi.org/10.1097/01.pra.0000413280.95843.d3.
Sackeim HA, Decina P, Portnoy S, Neeley P, Malitz S. Studies of dosage, seizure threshold, and seizure duration in ECT. Biol Psychiatry. 1987;22(3):249–68.
Sackeim HA, Prudic J, Devanand DP, Nobler MS, Lisanby SH, Peyser S, et al. A prospective, randomized, double-blind comparison of bilateral and right unilateral electroconvulsive therapy at different stimulus intensities. Arch Gen Psychiatry. 2000;57(5):425–34.
Boylan LS, Haskett RF, Mulsant BH, Greenberg RM, Prudic J, Spicknall K, et al. Determinants of seizure threshold in ECT: benzodiazepine use, anesthetic dosage, and other factors. J ECT. 2000;16(1):3–18. https://doi.org/10.1097/00124509-200003000-00002.
Galvez V, Hadzi-Pavlovic D, Smith D, Loo CK. Predictors of seizure threshold in right unilateral ultrabrief electroconvulsive therapy: role of concomitant medications and anaesthesia used. Brain Stimul. 2015;8(3):486–92. https://doi.org/10.1016/j.brs.2014.12.012.
Sackeim HA, Luber B, Katzman GP, Moeller JR, Prudic J, Devanand DP, et al. The effects of electroconvulsive therapy on quantitative electroencephalograms. Relationship to clinical outcome. Arch Gen Psychiatry. 1996;53(9):814–24.
Sackeim HA, Devanand DP, Prudic J. Stimulus intensity, seizure threshold, and seizure duration: impact on the efficacy and safety of electroconvulsive therapy. Psychiatr Clin N Am. 1991;14(4):803–43.
Ottosson JO. Seizure characteristics and therapeutic efficency in electroconvusive therapy: an analysis of the antidepressant efficiency of grand mal and lidocaine-modified seizures. J Nerv Ment Dis. 1962;135:239–51.
Fink M. The seizure, not electricity, is essential in convulsive therapy: the flurothyl experience. J ECT. 2014;30(2):91–3. https://doi.org/10.1097/yct.0000000000000110.
Bost-Baxter E, Reti I, Payne J. ECT in bipolar disorder: incidence of switch from depression to hypomania or mania. J Depress Anxiety. 2012;1:1–4.
Angst J, Angst K, Baruffol I, Meinherz-Surbeck R. ECT-induced and drug-induced hypomania. Convuls Ther. 1992;8(3):179–85.
Medda P, Toni C, Perugi G. The mood-stabilizing effects of electroconvulsive therapy. J ECT. 2014;30(4):275–82. https://doi.org/10.1097/yct.0000000000000160.
Perugi G, Medda P, Toni C, Mariani MG, Socci C, Mauri M. The role of electroconvulsive therapy (ECT) in bipolar disorder: effectiveness in 522 patients with bipolar depression, mixed-state, mania and catatonic features. Curr Neuropharmacol. 2017;15(3):359–71. https://doi.org/10.2174/1570159x14666161017233642.
Chiao S, Isenberg K, North CS. Psychotropic medication effects on seizure threshold and seizure duration during electroconvulsive therapy stimulus titration. J ECT. 2019. https://doi.org/10.1097/yct.0000000000000621.
van Waarde JA, van Oudheusden LJ, Verwey B, Giltay EJ, van der Mast RC. Clinical predictors of seizure threshold in electroconvulsive therapy: a prospective study. Eur Arch Psychiatry Clin Neurosci. 2013;263(2):167–75. https://doi.org/10.1007/s00406-012-0342-7.
Virupaksha HS, Shashidhara B, Thirthalli J, Kumar CN, Gangadhar BN. Comparison of electroconvulsive therapy (ECT) with or without anti-epileptic drugs in bipolar disorder. J Affect Disord. 2010;127(1–3):66–70. https://doi.org/10.1016/j.jad.2010.05.008.
Jahangard L, Haghighi M, Bigdelou G, Bajoghli H, Brand S. Comparing efficacy of ECT with and without concurrent sodium valproate therapy in manic patients. J ECT. 2012;28(2):118–23. https://doi.org/10.1097/YCT.0b013e31824b64b5.
Rakesh G, Thirthalli J, Kumar CN, Muralidharan K, Phutane VH, Gangadhar BN. Concomitant anticonvulsants with bitemporal electroconvulsive therapy: a randomized controlled trial with clinical and neurobiological application. J ECT. 2017;33(1):16–211. https://doi.org/10.1097/yct.0000000000000357.
Penland HR, Ostroff RB. Combined use of lamotrigine and electroconvulsive therapy in bipolar depression: a case series. J ECT. 2006;22(2):142–7.
Sienaert P, Roelens Y, Demunter H, Vansteelandt K, Peuskens J, Van Heeringen C. Concurrent use of lamotrigine and electroconvulsive therapy. J ECT. 2011;27(2):148–52. https://doi.org/10.1097/YCT.0b013e3181e63318.
Joo SW, Joo YH, Kim CY, Lee JS. Effects of stimulus parameters on motor seizure duration in electroconvulsive therapy. Neuropsychiatr Dis Treat. 2017;13:1427–34. https://doi.org/10.2147/ndt.S134503.
Pettinati HM, Stephens SM, Willis KM, Robin SE. Evidence for less improvement in depression in patients taking benzodiazepines during unilateral ECT. Am J Psychiatry. 1990;147(8):1029–35. https://doi.org/10.1176/ajp.147.8.1029.
Bailine SH, Safferman A, Vital-Herne J, Bernstein S. Flumazenil reversal of benzodiazepine-induced sedation for a patient with severe pre-ECT anxiety. Convuls Ther. 1994;10(1):65–8.
Krystal AD, Watts BV, Weiner RD, Moore S, Steffens DC, Lindahl V. The use of flumazenil in the anxious and benzodiazepine-dependent ECT patient. J ECT. 1998;14(1):5–14.
Galvez V, Loo CK, Alonzo A, Cerrillo E, Menchon JM, Crespo JM, et al. Do benzodiazepines moderate the effectiveness of bitemporal electroconvulsive therapy in major depression? J Affect Disord. 2013;150(2):686–90. https://doi.org/10.1016/j.jad.2013.03.028.
Jha A, Stein G. Decreased efficacy of combined benzodiazepines and unilateral ECT in treatment of depression. Acta Psychiatr Scand. 1996;94(2):101–4. https://doi.org/10.1111/j.1600-0447.1996.tb09832.x.
Delamarre L, Galvao F, Gohier B, Poulet E, Brunelin J. How much do benzodiazepines matter for electroconvulsive therapy in patients with major depression? J ECT. 2019;35(3):184–8. https://doi.org/10.1097/yct.0000000000000574.
Greenberg RM, Pettinati HM. Benzodiazepines and electroconvulsive therapy. Convuls Ther. 1993;9(4):262–73.
Sackeim HA, Prudic J, Devanand DP, Decina P, Kerr B, Malitz S. The impact of medication resistance and continuation pharmacotherapy on relapse following response to electroconvulsive therapy in major depression. J Clin Psychopharmacol. 1990;10(2):96–104.
Petrides G, Fink M, Husain MM, Knapp RG, Rush AJ, Mueller M, et al. ECT remission rates in psychotic versus nonpsychotic depressed patients: a report from CORE. J ECT. 2001;17(4):244–53.
Chanpattana W, Sackeim HA. Electroconvulsive therapy in treatment-resistant schizophrenia: prediction of response and the nature of symptomatic improvement. J ECT. 2010;26(4):289–98. https://doi.org/10.1097/YCT.0b013e3181cb5e0f.
Zervas IM, Theleritis C, Soldatos CR. Using ECT in schizophrenia: a review from a clinical perspective. World J Biol Psychiatry. 2012;13(2):96–105. https://doi.org/10.3109/15622975.2011.564653.
Tang YL, Jiang W, Ren YP, Ma X, Cotes RO, McDonald WM. Electroconvulsive therapy in China: clinical practice and research on efficacy. J ECT. 2012;28(4):206–12. https://doi.org/10.1097/YCT.0b013e31825957b1.
Petrides G, Malur C, Braga RJ, Bailine SH, Schooler NR, Malhotra AK, et al. Electroconvulsive therapy augmentation in clozapine-resistant schizophrenia: a prospective, randomized study. Am J Psychiatry. 2015;172(1):52–8. https://doi.org/10.1176/appi.ajp.2014.13060787.
Tharyan P, Adams CE. Electroconvulsive therapy for schizophrenia. Cochrane Database Syst Rev. 2005;2:CD000076. https://doi.org/10.1002/14651858.CD000076.pub2.
Lin HT, Liu SK, Hsieh MH, Chien YL, Chen IM, Liao SC, et al. Impacts of electroconvulsive therapy on 1-year outcomes in patients with schizophrenia: a controlled, population-based mirror-image study. Schizophr Bull. 2018;44(4):798–806. https://doi.org/10.1093/schbul/sbx136.
Sinclair DJ, Zhao S, Qi F, Nyakyoma K, Kwong JS, Adams CE. Electroconvulsive therapy for treatment-resistant schizophrenia. Cochrane Database Syst Rev. 2019;3:CD011847. https://doi.org/10.1002/14651858.CD011847.pub2.
Ahmed S, Khan AM, Mekala HM, Venigalla H, Ahmed R, Etman A, et al. Combined use of electroconvulsive therapy and antipsychotics (both clozapine and non-clozapine) in treatment resistant schizophrenia: a comparative meta-analysis. Heliyon. 2017;3(11):e00429. https://doi.org/10.1016/j.heliyon.2017.e00429.
Pawelczyk T, Kolodziej-Kowalska E, Pawelczyk A, Rabe-Jablonska J. Augmentation of antipsychotics with electroconvulsive therapy in treatment-resistant schizophrenia patients with dominant negative symptoms: a pilot study of effectiveness. Neuropsychobiology. 2014;70(3):158–64. https://doi.org/10.1159/000366484.
Zheng W, Cao XL, Ungvari GS, Xiang YQ, Guo T, Liu ZR, et al. Electroconvulsive therapy added to non-clozapine antipsychotic medication for treatment resistant schizophrenia: meta-analysis of randomized controlled trials. PLoS ONE. 2016;11(6):e0156510. https://doi.org/10.1371/journal.pone.0156510.
Grover S, Hazari N, Kate N. Combined use of clozapine and ECT: a review. Acta Neuropsychiatr. 2015;27(3):131–42. https://doi.org/10.1017/neu.2015.8.
Kupchik M, Spivak B, Mester R, Reznik I, Gonen N, Weizman A, et al. Combined electroconvulsive-clozapine therapy. Clin Neuropharmacol. 2000;23(1):14–6.
Jelovac A, Kolshus E, McLoughlin DM. Relapse following successful electroconvulsive therapy for major depression: a meta-analysis. Neuropsychopharmacology. 2013;38(12):2467–74. https://doi.org/10.1038/npp.2013.149.
Prudic J, Haskett RF, McCall WV, Isenberg K, Cooper T, Rosenquist PB, et al. Pharmacological strategies in the prevention of relapse after electroconvulsive therapy. J ECT. 2013;29(1):3–12. https://doi.org/10.1097/YCT.0b013e31826ea8c4.
Seager CP, Bird RL. Imipramine with electrical treatment in depression: a controlled trial. J Ment Sci. 1962;108:704–7. https://doi.org/10.1192/bjp.108.456.704.
Monaco JT, Delaplaine P. Tranylcypromine with ECT. Am J Psychiatry. 1964;120:1003. https://doi.org/10.1176/ajp.120.10.1003.
Kay DW, Fahy T, Garside RF. A seven-month double-blind trial of amitriptyline and diazepam in ECT-treated depressed patients. Br J Psychiatry. 1970;117(541):667–71. https://doi.org/10.1192/bjp.117.541.667.
Sackeim HA, Haskett RF, Mulsant BH, Thase ME, Mann JJ, Pettinati HM, et al. Continuation pharmacotherapy in the prevention of relapse following electroconvulsive therapy: a randomized controlled trial. JAMA. 2001;285(10):1299–307.
Nelson JP, Benjamin L. Efficacy and safety of combined ECT and tricyclic antidepressant therapy in the treatment of depressed geriatric patients. Convuls Ther. 1989;5:321–9.
Sackeim HA, Dillingham EM, Prudic J, Cooper T, McCall WV, Rosenquist P, et al. Effect of concomitant pharmacotherapy on electroconvulsive therapy outcomes: short-term efficacy and adverse effects. Arch Gen Psychiatry. 2009;66(7):729–37. https://doi.org/10.1001/archgenpsychiatry.2009.75.
Kellner CH, Knapp RG, Petrides G, Rummans TA, Husain MM, Rasmussen K, et al. Continuation electroconvulsive therapy vs pharmacotherapy for relapse prevention in major depression: a multisite study from the Consortium for Research in Electroconvulsive Therapy (CORE). Arch Gen Psychiatry. 2006;63(12):1337–444. https://doi.org/10.1001/archpsyc.63.12.1337.
Kellner CH, Husain MM, Knapp RG, McCall WV, Petrides G, Rudorfer MV, et al. A novel strategy for continuation ECT in geriatric depression: phase 2 of the PRIDE study. Am J Psychiatry. 2016;173(11):1110–8. https://doi.org/10.1176/appi.ajp.2016.16010118.
Dolenc TJ, Habl SS, Barnes RD, Rasmussen KG. Electroconvulsive therapy in patients taking monoamine oxidase inhibitors. J ECT. 2004;20(4):258–61.
Muller D. 1. Nardil (phenelzine) as a potentiator of electroconvulsive therapy (E.C.T.) 2. A survey of outpatient E.C.T. J Ment Sci. 1961;107:994–6. https://doi.org/10.1192/bjp.107.451.994.
Baghai TC, Marcuse A, Brosch M, Schule C, Eser D, Nothdurfter C, et al. The influence of concomitant antidepressant medication on safety, tolerability and clinical effectiveness of electroconvulsive therapy. World J Biol Psychiatry. 2006;7(2):82–90. https://doi.org/10.1080/15622970500213871.
Krystal AD, Weiner RD. ECT seizure therapeutic adequacy. Convuls Ther. 1994;10(2):153–64.
Krystal AD, Weiner RD, Coffey CE. The ictal EEG as a marker of adequate stimulus intensity with unilateral ECT. J Neuropsychiatry Clin Neurosci. 1995;7(3):295–303.
Lauritzen L. Relapse prevention by means of paroxetine in ECT-treated patients with major depression: a comparison with imipramine and placebo in medium-term continuation therapy. Acta Psychiatr Scand. 1996;94(4):241–51.
Gonzalez-Pinto A, Gutierrez M, Gonzalez N, Elizagarate E, de Heredia PJL, Mico JA. Efficacy and safety of venlafaxine-ECT combination in treatment-resistant depression. J Neuropsychiatry Clin Neurosci. 2002;14(2):206–9.
Doellinger OV, Ribeiro JP, Ribeiro A, Freitas C, Ribeiro B, Silva JC. Spontaneous seizures after ECT in a patient medicated with bupropion, sertraline and risperidone. Trends Psychiatry Psychother. 2016;38(2):111–3. https://doi.org/10.1590/2237-6089-2015-0055.
Dersch R, Zwernemann S, Voderholzer U. Partial status epilepticus after electroconvulsive therapy and medical treatment with bupropion. Pharmacopsychiatry. 2011;44(7):344–6. https://doi.org/10.1055/s-0031-1284425.
Conway CR, Nelson LA. The combined use of bupropion, lithium, and venlafaxine during ECT: a case of prolonged seizure activity. J ECT. 2001;17(3):216–8.
Takala CR, Leung JG, Murphy LL, Geske JR, Palmer BA. Concurrent electroconvulsive therapy and bupropion treatment. J ECT. 2017;33(3):185–9. https://doi.org/10.1097/yct.0000000000000423.
Johannessen Landmark C, Henning O, Johannessen SI. Proconvulsant effects of antidepressants: what is the current evidence? Epilepsy Behav. 2016;61:287–91. https://doi.org/10.1016/j.yebeh.2016.01.029.
Rudorfer MV, Manji HK, Potter WZ. Bupropion, ECT, and dopaminergic overdrive. Am J Psychiatry. 1991;148(8):1101–2.
Rudorfer MV, Linnoila M, Potter WZ. Combined lithium and electroconvulsive therapy: pharmacokinetic and pharmacodynamic interactions. Convuls Ther. 1987;3(1):40–5.
Hoenig J, Chaulk R. Delirium associated with lithium therapy and electroconvulsive therapy. Can Med Assoc J. 1977;116(8):837–8.
DePaulo JR Jr, Folstein MF, Correa EI. The course of delirium due to lithium intoxication. J Clin Psychiatry. 1982;43(11):447–9.
Ahmed SK, Stein GS. Negative interaction between lithium and ECT. Br J Psychiatry. 1987;151:419–20. https://doi.org/10.1192/bjp.151.3.419.
Hill GE, Wong KC, Hodges MR. Potentiation of succinylcholine neuromuscular blockade by lithium carbonate. Anesthesiology. 1976;44(5):439–42. https://doi.org/10.1097/00000542-197605000-00019.
Jephcott GKR. Lithium: an anaesthetic risk. Br J Anaesth. 1974;46:389–90.
Borden H, Clarke MT, Katz H. The use of pancuronium bromide in patients receiving lithium carbonate. Can Anaesth Soc J. 1974;21(1):79–82. https://doi.org/10.1007/bf03004581.
Weiner RD, Whanger AD, Erwin CW, Wilson WP. Prolonged confusional state and EEG seizure activity following concurrent ECT and lithium use. Am J Psychiatry. 1980;137(11):1452–3. https://doi.org/10.1176/ajp.137.11.1452.
Peterson GN. Consensus on electroconvulsive therapy. JAMA. 1986;255(15):2023. https://doi.org/10.1001/jama.1986.03370150065014.
Coppen A, Abou-Saleh MT, Milln P, Bailey J, Metcalfe M, Burns BH, et al. Lithium continuation therapy following electroconvulsive therapy. Br J Psychiatry. 1981;139:284–7. https://doi.org/10.1192/bjp.139.4.284.
Perry P, Tsuang MT. Treatment of unipolar depression following electroconvulsive therapy. Relapse rate comparisons between lithium and tricyclics therapies following ECT. J Affect Disord. 1979;1(2):123–9. https://doi.org/10.1016/0165-0327(79)90031-4.
Atiku L, Gorst-Unsworth C, Khan BU, Huq F, Gordon J. Improving relapse prevention after successful electroconvulsive therapy for patients with severe depression: completed audit cycle involving 102 full electroconvulsive therapy courses in West Sussex, United Kingdom. J ECT. 2015;31(1):34–6. https://doi.org/10.1097/yct.0000000000000164.
Brus O, Cao Y, Hammar A, Landen M, Lundberg J, Nordanskog P, et al. Lithium for suicide and readmission prevention after electroconvulsive therapy for unipolar depression: population-based register study. BJPsych Open. 2019;5(3):e46. https://doi.org/10.1192/bjo.2019.37.
Dolenc TJ, Rasmussen KG. The safety of electroconvulsive therapy and lithium in combination: a case series and review of the literature. J ECT. 2005;21(3):165–70.
Tsujii T, Uchida T, Suzuki T, Mimura M, Hirano J, Uchida H. Factors associated with delirium following electroconvulsive therapy: a systematic review. J ECT. 2019;35(4):279–87. https://doi.org/10.1097/yct.0000000000000606.
Thirthalli J, Harish T, Gangadhar BN. A prospective comparative study of interaction between lithium and modified electroconvulsive therapy. World J Biol Psychiatry. 2011;12(2):149–55. https://doi.org/10.3109/15622975.2010.504860.
Patel RS, Bachu A, Youssef NA. Combination of lithium and electroconvulsive therapy (ECT) is associated with higher odds of delirium and cognitive problems in a large national sample across the United States. Brain Stimul. 2020;13(1):15–9. https://doi.org/10.1016/j.brs.2019.08.012.
Zolezzi M. Medication management during electroconvulsant therapy. Neuropsychiatr Dis Treat. 2016;12:931–9. https://doi.org/10.2147/ndt.S100908.
Malhi GS, Byrow Y, Bassett D, Boyce P, Hopwood M, Lyndon W, et al. Stimulants for depression: on the up and up? Aust N Z J Psychiatry. 2016;50(3):203–7. https://doi.org/10.1177/0004867416634208.
Naguib M, Koorn R. Interactions between psychotropics, anaesthetics and electroconvulsive therapy: implications for drug choice and patient management. CNS Drugs. 2002;16(4):229–47.
Pigot M, Andrade C, Loo C. Pharmacological attenuation of electroconvulsive therapy—induced cognitive deficits: theoretical background and clinical findings. J ECT. 2008;24(1):57–67. https://doi.org/10.1097/YCT.0b013e3181616c14.
Boman B. Concurrent use of ECT and cholinesterase inhibitor medications. Aust N Z J Psychiatry. 2002;36(6):816. https://doi.org/10.1046/j.1440-1614.2002.t01-5-01101a.x.
Bhat RS, Mayur P, Chakrabarti I. ECT-donepezil interaction: a single case report. Int J Geriatr Psychiatry. 2004;19(6):594–5. https://doi.org/10.1002/gps.1085.
Henstra MJ, Jansma EP, van der Velde N, Swart EL, Stek ML, Rhebergen D. Acetylcholinesterase inhibitors for electroconvulsive therapy-induced cognitive side effects: a systematic review. Int J Geriatr Psychiatry. 2017;32(5):522–31. https://doi.org/10.1002/gps.4702.
Rao NP, Palaniyappan P, Chandur J, Venkatasubramanian G, Gangadhar BN. Successful use of donepezil in treatment of cognitive impairment caused by maintenance electroconvulsive therapy: a case report. J ECT. 2009;25(3):216–8. https://doi.org/10.1097/YCT.0b013e3181926ada.
Prakash J, Kotwal A, Prabhu H. Therapeutic and prophylactic utility of the memory-enhancing drug donepezil hydrochloride on cognition of patients undergoing electroconvulsive therapy: a randomized controlled trial. J ECT. 2006;22(3):163–8. https://doi.org/10.1097/01.yct.0000230365.81368.2d.
Logan CJ, Stewart JT. Treatment of post-electroconvulsive therapy delirium and agitation with donepezil. J ECT. 2007;23(1):28–9. https://doi.org/10.1097/01.yct.0000263259.29291.c4.
Takamiya A, Sawada K, Hirano J, Mimura M, Kishimoto T. Prolonged post-electroconvulsive therapy delirium controlled with donepezil. J ECT. 2019;35(3):e29–e30. https://doi.org/10.1097/yct.0000000000000590.
Newport DJ, Carpenter LL, McDonald WM, Potash JB, Tohen M, Nemeroff CB. Ketamine and other NMDA antagonists: early clinical trials and possible mechanisms in depression. Am J Psychiatry. 2015;172(10):950–66. https://doi.org/10.1176/appi.ajp.2015.15040465.
Xu Y, Hackett M, Carter G, Loo C, Galvez V, Glozier N, et al. Effects of low-dose and very low-dose ketamine among patients with major depression: a systematic review and meta-analysis. Int J Neuropsychopharmacol. 2016;19(4):1. https://doi.org/10.1093/ijnp/pyv124.
Rudolph U, Antkowiak B. Molecular and neuronal substrates for general anaesthetics. Nat Rev Neurosci. 2004;5(9):709–20. https://doi.org/10.1038/nrn1496.
Modica PA, Tempelhoff R, White PF. Pro- and anticonvulsant effects of anesthetics (Part II). Anesth Analg. 1990;70(4):433–44. https://doi.org/10.1213/00000539-199004000-00016.
Hoyer C, Kranaster L, Janke C, Sartorius A. Impact of the anesthetic agents ketamine, etomidate, thiopental, and propofol on seizure parameters and seizure quality in electroconvulsive therapy: a retrospective study. Eur Arch Psychiatry Clin Neurosci. 2014;264(3):255–61. https://doi.org/10.1007/s00406-013-0420-5.
Rasmussen KG, Ritter MJ. Some considerations of the tolerability of ketamine for ECT anesthesia: a case series and review of the literature. J ECT. 2014;30(4):283–6. https://doi.org/10.1097/yct.0000000000000100.
Anderson IM, Blamire A, Branton T, Clark R, Downey D, Dunn G, et al. Ketamine augmentation of electroconvulsive therapy to improve neuropsychological and clinical outcomes in depression (Ketamine-ECT): a multicentre, double-blind, randomised, parallel-group, superiority trial. Lancet Psychiatry. 2017;4(5):365–77. https://doi.org/10.1016/s2215-0366(17)30077-9.
Abdallah CG, Fasula M, Kelmendi B, Sanacora G, Ostroff R. Rapid antidepressant effect of ketamine in the electroconvulsive therapy setting. J ECT. 2012;28(3):157–61. https://doi.org/10.1097/YCT.0b013e31824f8296.
Loo CK, Katalinic N, Garfield JB, Sainsbury K, Hadzi-Pavlovic D, Mac-Pherson R. Neuropsychological and mood effects of ketamine in electroconvulsive therapy: a randomised controlled trial. J Affect Disord. 2012;142(1–3):233–40. https://doi.org/10.1016/j.jad.2012.04.032.
Rasmussen KG, Kung S, Lapid MI, Oesterle TS, Geske JR, Nuttall GA, et al. A randomized comparison of ketamine versus methohexital anesthesia in electroconvulsive therapy. Psychiatry Res. 2014;215(2):362–5. https://doi.org/10.1016/j.psychres.2013.12.027.
Yoosefi A, Sepehri AS, Kargar M, Akhondzadeh S, Sadeghi M, Rafei A, et al. Comparing effects of ketamine and thiopental administration during electroconvulsive therapy in patients with major depressive disorder: a randomized, double-blind study. J ECT. 2014;30(1):15–211. https://doi.org/10.1097/YCT.0b013e3182a4b4c6.
Zheng W, Li XH, Zhu XM, Cai DB, Yang XH, Ungvari GS, et al. Adjunctive ketamine and electroconvulsive therapy for major depressive disorder: a meta-analysis of randomized controlled trials. J Affect Disord. 2019;250:123–31. https://doi.org/10.1016/j.jad.2019.02.044.
Galvez V, McGuirk L, Loo CK. The use of ketamine in ECT anaesthesia: a systematic review and critical commentary on efficacy, cognitive, safety and seizure outcomes. World J Biol Psychiatry. 2017;18(6):424–44. https://doi.org/10.1080/15622975.2016.1252464.
Acknowledgements
The work in this paper was supported by the J.B. Fuqua Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist with the preparation of this article.
Conflict of interest
William M. McDonald has research contracts from Stanley Foundation, Soterix, Neuronetics, NeoSync, and Cervel Neurotherapeutics. He is an ad hoc member of several National Institute of Mental Health (NIMH) and National Institute of Neurological Disorders and Stroke (NINDS) study sections; is a member of the American Psychiatric Association (APA) Council on Research and Quality representing ECT and Neuromodulation Therapies; receives royalties from Oxford University Press to co-edit a book titled ‘Clinical Guide to Transcranial Magnetic Stimulation in the Treatment of Depression’; is a paid consultant for Signant Health; and is an employee of Emory University School of Medicine. A. Umair Janjua, Amitha L. Dhingra, and Robert Greenberg declare they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Janjua, A.U., Dhingra, A.L., Greenberg, R. et al. The Efficacy and Safety of Concomitant Psychotropic Medication and Electroconvulsive Therapy (ECT). CNS Drugs 34, 509–520 (2020). https://doi.org/10.1007/s40263-020-00729-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-020-00729-1