Abstract
Objective
The aim of this study was to assess the type and frequency of adverse events (AEs) in children with attention-deficit/hyperactivity disorder (ADHD) treated with methylphenidate or atomoxetine over a 5-year period in a large naturalistic study.
Methods
We draw on data from the Italian ADHD Registry, a national database for postmarketing phase IV pharmacovigilance of ADHD medications across 90 centers. AEs were defined as severe or mild as per the classification of the Italian Medicines Agency. AE frequency in the two treatment groups was compared using incidence rates per 100 person-years (IR100PY) and incidence rate ratios (IRRs). Mantel–Haenszel adjusted IRRs were calculated to control for psychiatric comorbidity.
Results
A total of 1350 and 753 participants (aged 6–18 years, mean age 10.7 ± 2.8) were treated with methylphenidate and atomoxetine, respectively, from 2007 to 2012. Ninety participants (7 %) were switched from methylphenidate to atomoxetine, and 138 (18 %) from atomoxetine to methylphenidate. Thirty-seven children treated with atomoxetine and 12 with methylphenidate had their medication withdrawn. Overall, 645 patients (26.8 %) experienced at least one mild AE (including decreased appetite and irritability, for both drugs) and 95 patients (3.9 %) experienced at least one severe AE (including severe gastrointestinal events). IR100PY were significantly higher in the atomoxetine-treated group compared with the methylphenidate-treated group for a number of mild and severe AEs and for any severe or mild AEs. After controlling for comorbidities, IRR was still significantly higher in the atomoxetine group compared with the methylphenidate group for a number of mild (decreased appetite, weight loss, abdominal pain, dyspepsia, stomach ache, irritability, mood disorder and dizziness) and severe (gastrointestinal, neuropsychiatric, and cardiovascular) AEs.
Conclusions
In this naturalistic study, methylphenidate had a better safety profile than atomoxetine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In this naturalistic study, atomoxetine was less well tolerated than methylphenidate for a number of mild and severe adverse events. |
This finding remained significant even after controlling for psychiatric comorbidities in the methylphenidate and atomoxetine groups. |
1 Introduction
Attention-deficit/hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder [1], with a worldwide prevalence estimated at approximately 5 % in school-aged children [2] and persistence of impairing symptoms in adulthood in up to 65 % of cases [3]. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [4], ADHD is characterized by an age-inappropriate, persistent and impairing pattern of inattention and/or hyperactivity/impulsivity. ADHD is often comorbid with other psychiatric conditions, such as oppositional defiant disorder (ODD)/conduct disorder (CD), specific learning disorders, mood and anxiety disorders [5], sleep disturbances [6] and, in adulthood, personality disorders [7].
Available treatments for ADHD include pharmacological and nonpharmacological strategies. The former are recommended as the first-choice option in several guidelines/practice parameters (e.g. Pliszka [8]), at least for severe cases [9, 10], or as a treatment strategy for patients who did not respond to nonpharmacological interventions [9, 10]. Medications for ADHD include psychostimulant (i.e. methylphenidate and amphetamine derivatives) and nonpsychostimulant drugs (e.g. atomoxetine, clonidine, guanfacine). Psychostimulant medications are indicated as first-line treatment in some guidelines/recommendations (e.g. the UK National Institute for Health and Care Excellence [NICE] guidelines [9]).
As with all medications, and some nonpharmacological interventions, adverse events (AEs) can and do occur during treatment with ADHD drugs [11]. Although the majority of such AEs are clinically manageable [12], the tolerability and safety of medications for ADHD is of concern to regulatory bodies, clinicians, patients and their families. This may result in patients with ADHD being exposed to harm if AEs are overlooked, or not benefitting from effective medications if the potential AEs are overestimated [12]. Therefore, understanding the nature of AEs associated with ADHD medications is paramount. Additionally, tolerability and safety profile is an important element in the choice of the specific class of medication. Evidence of the types of AEs and comparative tolerability/safety of different ADHD medications, particularly methylphenidate versus atomoxetine, is available from a large body of randomized controlled trials (RCTs). Two meta-analyses of such RCTs [13, 14] concluded that methylphenidate and atomoxetine have similar profiles in terms of all-cause discontinuation and incidence of AEs. However, some individual studies reported significantly greater incidence of decreased appetite and insomnia [15], weight loss and heart rate increase [16] with methylphenidate, and significantly higher rates of anorexia, nausea, somnolence, dizziness and vomiting with atomoxetine [17].
Whilst the rigorous design of conventional RCTs allows for a reduction of many confounding factors, such studies may be hampered by selection bias [18] since they often include a selected subpopulation of subjects, which only, in part, reflects the type of patients commonly seen in day-to-day clinical practice. In addition, such trials are usually limited to a few weeks/months, therefore they do not allow for the detection of potential longer-term AEs. In this respect, longer-term naturalistic studies provide additional valuable information.
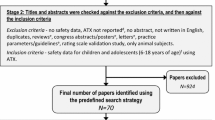
To address these issues, we draw on data from the Italian National ADHD Registry [19], set up to perform intensive postmarketing phase IV pharmacovigilance of ADHD medications across 90 Italian ADHD centers. We aimed to: (i) assess the type of AEs; and (ii) compare their frequency in children treated with methylphenidate or atomoxetine over a 5-year period. We focused on methylphenidate and atomoxetine, the only two classes of ADHD drugs licensed in Italy at the time of the study. Given the exploratory nature of this study, no a priori hypotheses were formulated.
2 Methods
2.1 Study Population
Participants were children/adolescents (aged 6–18 years) included in the Italian National ADHD Registry from June 2007 to December 2012. This time frame was established by the Italian Medicines Agency as an appropriate period for pharmacovigilance. The diagnosis of ADHD was based on the DSM, Fourth Edition-text revision (DSM-IV-TR) [20] criteria (the classification system used at the time of the study). Given the naturalistic design, no a priori exclusion criteria were applied. Comorbid disorders were not an exclusionary criterion since the presence of comorbid psychiatric disorders is the rule rather than the exception in ADHD.
2.2 Study Drugs
ADHD was treated with either of the following.
-
(i)
Methylphenidate chlorhydrate immediate release, 10 mg. Administration was orally at a dosage of 0.3–0.6 mg/kg/dose/day. First, as recommended by the official protocol of the Italian ADHD centers, methylphenidate was administered at a test dose of 0.3 mg/kg. The dosage could then be increased up to 0.6 mg/kg/dose based on clinical response and tolerability. The total dose was administered in two or three doses/day. Methylphenidate immediate-release was the only available formulation of methylphenidate in Italy at the time of the study;
-
(ii)
Atomoxetine chlorhydrate 5, 10, 18, 25, 40 or 60 mg. Administration was orally, starting with 0.5 mg/kg once a day, for at least 7 days, then increasing the dose up to 1.2 mg/kg/day, based on clinical response and tolerability.
Since atomoxetine was the only ADHD medication available in Italy until methylphenidate was reintroduced on the market in 2007 in our country, it was and still is customary for some Italian clinicians to use atomoxetine as a first-line treatment. Therefore, four types of participants could be identified based on their ADHD pharmacological treatment history: (i) those treated only with methylphenidate; (ii) those treated only with atomoxetine; (iii) those initially started on methylphenidate, and then switched to atomoxetine; and (iv) those who initially took atomoxetine and were then switched to methylphenidate.
2.3 Data Collection
The prescription of ADHD medications in Italy undergoes systematic monitoring, carried out by means of a national register, with compulsory compilation by local reference centers [21, 22]. An active pharmacovigilance system is performed via notification by clinical centers to the Italian Medicines Agency. Data regarding AEs are collected via a structured form, located in a restricted area of the website of the Italian ADHD registry (available upon request), which allows standardization of the procedure across centers. Information about the following AEs is collected via the aforementioned structured form.
-
(i)
Cardiovascular risk, complemented by data obtained via electrocardiogram (ECG), systematically performed for each participant before starting drug therapy and after 6 months. According to the procedure recommended by the Italian Medicines Agency, cardiovascular risk includes any clinically relevant ECG abnormalities (such as bundle branch block), change in heart rate, changes in at least one standard deviation (SD) of systolic or diastolic blood pressure, and lengthening of the QT interval, defined as any prolongation, in absolute value, in relation to the value detected at the screening before the first administration of the drug.
-
(ii)
Hepatic toxicity, complemented by a specific assessment of liver enzymes, bilirubin, ammonia and, if deemed clinically necessary, ultrasound imaging.
-
(iii)
Any neurological disorder, complemented, if needed, by information obtained via electroencephalogram (EEG) and magnetic resonance imaging (MRI).
-
(iv)
Any psychiatric symptomatology, such as change in mood (depression or elation), hallucinations, suicidal ideation, or psychosis
-
(v)
Acute diseases of the skin, such as rash, eczema, itching, or vasculitis.
-
(vi)
Any clinically relevant gastrointestinal events, including vomiting, nausea, diarrhea, constipation, and abdominal pain.
In the present study, AEs were classified as severe if their occurrence was followed by active notification by clinical centers to the Italian Medicines Agency; otherwise, they were labelled as mild. The Italian Medicines Agency requires active notification when an AE results in death, is life-threatening, requires hospitalisation or prolongation of existing inpatients’ hospitalisation, results in persistent or significant disability or incapacity, or leads to a congenital anomaly or birth defect [23].
2.4 Statistical Analysis
Categorical descriptive data (such as prevalence of psychiatric comorbidities) were presented as absolute and percentage frequencies, and were analyzed using the Fisher’s exact probability test to assess differences between methylphenidate- and atomoxetine-treated participants. Continuous descriptive data (such as age) were presented as means and SDs, and analyzed using the Mann–Whitney U test. Incidence rates per 100 person-years (IR100PY) were computed for any type of AE in methylphenidate- and atomoxetine-treated participants, in all children and separately for children with and without psychiatric comorbidities (one or more of ODD, CD, depression, anxiety, learning disorder). Incidence rates were calculated considering days of exposure to methylphenidate or atomoxetine. Data from any participant first exposed to methylphenidate and then switched to atomoxetine (or vice versa) contributed to the calculation of AE incidence rates for both methylphenidate and atomoxetine, in different time periods. Incidence rate ratios (IRRs) were computed as the ratio between the incidence rate in the atomoxetine group and the corresponding incidence rate in the methylphenidate group, separately for children with and without psychiatric comorbidities. Confidence intervals (CIs) were computed at the 95 % confidence level. Here, CIs for which the lower limit is higher than 1 indicate that atomoxetine significantly increased the risk of AEs with respect to methylphenidate; CIs for which the upper limit is lower than 1 indicate that atomoxetine significantly decreased the risk of AEs with respect to methylphenidate. When there were no events in the reference group of methylphenidate-treated children (with and/or without comorbidities), the corresponding IRRs could not be computed, therefore only the lower level of the 95 % CI was estimated and reported.
Despite the difference between the subjects initially receiving methylphenidate and those treated with atomoxetine in terms of rates of comorbidities (64 vs. 76 %), a much lower difference was observed between subjects actually receiving methylphenidate or atomoxetine with respect to the percentage of exposure time (methylphenidate: 736.1/1026.0 = 72 %; atomoxetine: 528.3/689.8 = 77 %). However, to take into account this difference, even if quite low, incidence rates were computed separately in subjects treated with methylphenidate, with comorbidities (total exposure = 736.1 person years), treated with methylphenidate, without comorbidities (total exposure = 289.9 person years), treated with atomoxetine, with comorbidities (total exposure = 528.3 person years), and treated with atomoxetine treatment, without comorbidities (total exposure = 161.5 person years). In order to control for the possible confounding effect of psychiatric comorbidities, heterogeneity between crude IRRs in children with and without comorbidities was assessed by means of the Chi-square test. The presence/absence of comorbidities was considered a stratifying factor, and the Mantel–Haenszel IRR with the corresponding 95 % CI was computed to estimate the overall adjusted IRR, for all AEs for which heterogeneity Chi-square test was not significant. STATA 8.1 was used for all statistical analyses (StataCorp LP, College Station, TX, USA). Statistical significance was defined as p < 0.05 (two-tailed). As discussed in Rothman [24], no correction for multiple comparison was needed.
3 Results
3.1 Description of the Sample
During the planned study period (June 2007–December 2012 [62 months]), a total of 2411 children enrolled in the national registry were pharmacologically treated for ADHD. The mean age of the study population was 10.68 years (SD 2.79) (Table 1). The sample included 2125 males (88.1 %) and 286 females (11.9 %). The majority of children (2041, 84.7 %) received a diagnosis of ADHD combined subtype, 283 (11.7 %) were diagnosed with ADHD inattentive subtype, and 87 (3.6 %) presented with ADHD hyperactive–impulsive subtype.
At enrolment, 1426 (59.1 %) children and adolescents received methylphenidate and 985 (40.9 %) were treated with atomoxetine. The average dose was 18.3 mg/day for methylphenidate and 38.5 mg/day for atomoxetine. The demographic and clinical characteristics of the methylphenidate- and atomoxetine-assigned groups at enrolment are reported in Table 1. Of note, the atomoxetine-assigned group presented with significantly higher rates of psychiatric comorbid disorders (any, ODD, CD, depressive disorders, anxiety disorders, and specific learning disorders) than the methylphenidate-assigned group.
3.2 Adverse Events
Data on AEs after the first dose of treatment were available for a total of 2331 participants (96.7 % of the subjects initially assigned to either methylphenidate or atomoxetine at enrolment). Of these, 1350 and 753 were treated with methylphenidate and atomoxetine, respectively, throughout the entire study period. Ninety participants (7 %) were switched from methylphenidate to atomoxetine, and 138 (18 %) were switched from atomoxetine to methylphenidate.
Overall, 645 patients (26.8 %) experienced at least one mild AE, including 276 (28.0 %) children treated with atomoxetine, and 369 (25.9 %) children treated with methylphenidate. Ninety-five patients (3.9 %) experienced at least one severe AE, including 31 (3.1 %) children treated with atomoxetine, and 64 (4.5 %) children treated with methylphenidate; 49 (51.6 %) of these children (37 in the atomoxetine group and 12 in the methylphenidate group) had medication withdrawn.
Table 2 reports the absolute number and IR100PY of mild AEs in subjects treated with methylphenidate or atomoxetine, stratified by the presence/absence of psychiatric comorbidities. It also reports significant differences in IR100PY between participants treated with methylphenidate and atomoxetine, with and without comorbidities. Considering children without comorbidities, a significantly higher IR100PY in the atomoxetine- versus methylphenidate-treated group was observed for the following mild AEs: weight loss, dyspepsia, and stomach ache. In children with comorbidities, a significantly higher IR100PY in the atomoxetine- versus methylphenidate-treated group was observed for the following mild AEs: decreased appetite, weight loss, abdominal pain, dyspepsia, stomach ache, irritability, mood disorder, and obsessive behaviour.
Crude and Mantel–Haenszel adjusted IRR of mild AEs in methylphenidate- and atomoxetine-treated children, with and without comorbidities, are reported in Table 3. After adjusting for comorbidities, compared with the methylphenidate-treated group, IRRs were significantly higher in the atomoxetine-treated group for the following mild AEs: decreased appetite, weight loss, abdominal pain, dyspepsia, stomach ache, irritability, mood disorder, and dizziness. Overall, the incidence rate ratio of any kind of AEs was significantly higher in the atomoxetine-treated group than in the methylphenidate-treated group.
Table 4 reports details about severe AEs, grouped by system/type. These included five cases of suicidal ideation (only in the atomoxetine group, including one participant with a history of depressive disorder), four cases of hyperbilirubinemia as proxy of hepatic toxicity (three in the atomoxetine group and one in the methylphenidate group), and one case of prolonged QTc in the atomoxetine group. The mean time to onset (SD) of severe AEs was 4.6 (4.4) months in the atomoxetine group and 6.2 (11.5) months in the methylphenidate group (p = 0.06); 26.2 % of severe AEs in the atomoxetine group and 52.8 % of those in the methylphenidate group occurred within 1 month of starting treatment. The mean age at onset (SD) of severe AEs was 10.2 (2.9) years for participants in the atomoxetine group and 10.7 (2.9) years for those in the methylphenidate group (p = 0.41).
As reported in Table 5, when considering participants without comorbidities, IR100PY was significantly higher in the atomoxetine-treated group versus the methylphenidate-treated group for severe AEs classified in the gastrointestinal system (atomoxetine 5.6; methylphenidate 0.0). In participants with comorbidities, IR100PY was significantly higher in the atomoxetine-treated group versus the methylphenidate group for severe neuropsychiatric AEs (atomoxetine 4.0; methylphenidate 1.4). Overall, the IRR of any kind of severe AE was significantly higher in atomoxetine recipients than methylphenidate recipients (IR100PY: atomoxetine 12.18, methylphenidate 3.51; IRR 3.47, 95 % CI 2.35–5.13).
Crude and Mantel–Haenszel adjusted IRR of severe AEs in methylphenidate- and atomoxetine-treated children, with and without comorbidities, are reported in Table 6. After controlling for the effect of psychiatric comorbidities, compared with the methylphenidate-treated group, IRRs were significantly higher in the atomoxetine-treated group for severe AEs classified as ‘gastrointestinal’, ‘neuropsychiatric’, and ‘cardiovascular’.
4 Discussion
We assessed the type of AEs, both mild and severe, and compared their prevalence in children with ADHD treated with methylphenidate or atomoxetine, drawing on data from a national registry for phase IV pharmacovigilance. To our knowledge, this is one of the largest available databases to evaluate the safety of medications for ADHD, involving approximately 90 ADHD centres.
The type of AEs that we observed in our study is in line with what has been reported in the previous literature [12]. Rather than discussing each individual AE, for ease of presentation we discuss the main AEs, grouping them by category/system.
With regard to cardiovascular events, we found ten cases (nine mild and one severe) of prolonged QTc (four with atomoxetine and six methylphenidate). However, importantly, all observed prolonged QTc intervals were not clinically significant since the prolongations of QTc interval were less than 450 ms, which represents the pathologic cutoff point. In addition, among the severe AEs, we observed other ECG abnormalities, including six cases of tachycardia (four with atomoxetine and two with methylphenidate) and one case of right bundle branch block in a methylphenidate-treated subject, but none of these were clinically significant. We also observed three cases of serious hypertension (one in the atomoxetine-treated participants and two in the methylphenidate-treated participants) and one case (treated with atomoxetine) of relevant hypotension that required drug withdrawal. A number of cases of hypertension (two with atomoxetine and nine with methylphenidate) and hypotension (nine with atomoxetine and three with methylphenidate) were reported as mild AEs and, rather than drug suspension, required only a dosage adjustment. Our findings are in line with the results of a systematic review of the European ADHD Guidelines Group (EAGG) [12], which concluded that there is no evidence supporting that ADHD drugs are associated with significant changes in electrocardiographic values, including QT interval. The EAGG review also concluded that psychostimulant medications and atomoxetine may slightly increase blood pressure (average increase systolic 1–4 mmHg; diastolic 1–2 mmHg) and heart rate (average increase 1–2 beats per min), but in a minority of individuals (5–15 %) this increase may be above the 95th percentile. Importantly, data from the Multimodal Treatment of ADHD (MTA) study at 12-year follow-up showed no systematic significant increase of blood pressure with psychostimulant treatment throughout the study period, although psychostimulants did have a persistent adrenergic effect increasing heart rate [25].
Regarding neuropsychiatric AEs, the most serious was suicidal ideation, which was, however, rare (frequency: 0.51 % of cases, 5/985). No complete suicides were observed. Importantly, the definition of ‘suicidal ideation’ was standardized across centers, which limited the likelihood of bias and heterogeneity in reporting ‘suicidal ideation’. Of note, all cases occurred during treatment with atomoxetine. Although the observed frequency of suicidal ideation was more frequent than expected on the basis of FDA warning [26], overall our findings are once again consistent with the EAGG systemic review, according to which suicide-related events rarely occur with ADHD drug treatment. Importantly, the EAGG pointed out that there is little compelling evidence to suggest that the rate of suicide-related events in children treated with ADHD drugs is greater than the expected rate in the general population.
Among hepatic AEs, hyperbilirubinemia occurred almost exclusively with atomoxetine (three cases vs. one with methylphenidate). This is an AE that has been noted in previous pharmacovigilance reports of atomoxetine tolerability and safety [27]. Although hyperbilirubinemia was reported in a relatively small number of participants, it is a potentially very severe AE, which may lead to liver failure resulting in death or the need for a liver transplant.
Seizures occurred in a limited number of patients (three in the methylphenidate group and two in the atomoxetine group). In four cases they were generalized, and in one case (treated with atomoxetine) they were focal/partial. They all resolved with drug discontinuation, except for one case who presented with previous absence seizures and who was successfully treated with valproate. With regard to seizures, the EAGG [12] concluded that, in patients with well-controlled epilepsy, methylphenidate is associated with a low risk for seizure, whilst it deemed that evidence for atomoxetine is still too limited to draw firm conclusions.
Whilst AEs (mild or severe) were observed both in methylphenidate- and atomoxetine-treated participants, an important finding of our study is that they were significantly more frequent in the latter. Importantly, after controlling for comorbid psychiatric disorders, this difference did remain significant for decreased appetite, weight loss, abdominal pain, dyspepsia, stomach ache, irritability, mood disorder and dizziness (mild AEs), as well as for severe gastrointestinal, neuropsychiatric, and cardiovascular events (severe AEs).
We also observed that mild AEs usually occurred after a shorter time of exposure to atomoxetine than methylphenidate. On the basis of the pharmacokinetics, it is not clear why the AEs occurred in patients treated with atomoxetine after a shorter exposure to the drug compared with patients with methylphenidate.
The atomoxetine non-comorbid group displayed low rates of insomnia, suggesting a potential benefit of atomoxetine for insomnia, as pointed out by the EAGG [12].
We note that our study also explored growth delay, defined as (i) height less than or equal to −3 SD, or less than or equal to −2 SD plus height velocity/year less than −1.0 SD for age and gender at 6 months or 0.5 after 2 years; (ii) height less than or equal to −1.5 SD plus height velocity/year less than −1.0 SD for age and gender at 6 months or 0.5 after 2 years; or (iii) height velocity/year <2 SD or −1.5 after 2 years [28]. Indeed, 16 cases of mild growth delay were notified (12 patients treated with methylphenidate and 4 with atomoxetine). In none of these cases was the growth delay more than 2 SD (data available upon request). However, these results should be considered with caution; a longer follow-up period might reveal more reliable data on growth. The EAGG concluded that there is evidence of significant psychostimulant-associated height and weight deficits (length of treatment 0.5–3.5 years). The deficit in height tends to increase with time, but the rate of deficit tends to decrease over time for height and weight, suggesting a tendency for the deficit to attenuate with time. As for atomoxetine, a meta-analysis [29] found that the mean actual weight and height at 24 months were 2.5 kg and 2.7 cm lower than the expected values, respectively, based on baseline weight and height percentile. The difference mostly occurred during the first 18 months of treatment.
Taken together, our results are at odds with two meta-analyses of RCTs [13, 14] that, as reported above, showed that methylphenidate and atomoxetine have similar profiles in terms of all-cause discontinuation and incidence of AEs, as well as with individual studies reporting a significantly greater incidence of decreased appetite and insomnia [15], weight loss and heart rate increase [16] with methylphenidate. We hypothesize that the differences between our results and the conclusions of these studies are accounted for by the different design (naturalistic in our study vs. RCTs in the meta-analyses and previous individual studies), as well as by the longer duration of our study compared with standard available RCTs.
Our results should be considered in light of the study limitations. First, this was not a randomized study, therefore differences between participants treated with methylphenidate and those who took atomoxetine may have accounted for the findings. However, it is worthy to note that significant differences in terms of prevalence of mild and severe AEs did stand, even after controlling for the effect of psychiatric comorbidities. Whilst the lack of randomization could be considered as a limitation, the naturalistic design of our study is, at the same time, its strength, allowing for an understanding of the differences in prevalence of AEs in a ‘real-world’ clinical context. Second, data on AEs were not available for all participants at follow-up visits following the baseline assessment and treatment assignment. However, this only occurred for 3.3 % of participants, therefore it is unlikely that our results were not representative of the entire sample. Third, our study could not be informative with regard to AEs occurring with extended-release formulations of methylphenidate as well as with other class of ADHD drugs since these were not available in Italy during the study period. Fourth, the average doses of methylphenidate and atomoxetine were rather low for usual standards of treatment, reflecting the caution to use ADHD drugs in Italy. However, we do not consider this a confounding factor since the average dose was low for both medications. Fifth, the naturalistic design did not allow to assess if children were adequately titrated, for both medications. Sixth, data on validity and reliability of measures across centres are not available. Finally, the study did not include a control group of healthy participants. However, our study focus was on the comparison of the prevalence of AEs between methylphenidate- and atomoxetine-treated participants rather than on the prevalence of AEs in children treated with ADHD and healthy controls.
As well as the naturalistic design with no exclusion criteria, study strengths were the sample size and the structured and standardized way of AE coding and data collection.
5 Conclusions
Our naturalistic postmarketing phase IV pharmacovigilance observational study showed that while mild and severe AEs were observed in children treated with methylphenidate and in those treated with atomoxetine, those who received atomoxetine were significantly more likely to experience AEs.
References
Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol. 2014;43(2):434–42.
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–8.
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159–65.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Biederman J, Faraone SV. Attention-deficit hyperactivity disorder. Lancet. 2005;366(9481):237–48.
Cortese S, Lecendreux M, Mouren MC, Konofal E. ADHD and insomnia. J Am Acad Child Adolesc Psychiatry. 2006;45(4):384–5.
Speranza M, Revah-Levy A, Cortese S, Falissard B, Pham-Scottez A, Corcos M. ADHD in adolescents with borderline personality disorder. BMC Psychiatry. 2011;11:158.
Pliszka S. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894–921.
NICE. National Institute for Health and Care Excellence. Attention deficit hyperactivity disorder: diagnosis and management of ADHD in children, young people and adults. Clinical Guidance 72 (CG72). 2008. Available at: http://www.nice.org.uk/CG72. Accessed 10 July 2015.
Taylor E, Dopfner M, Sergeant J, et al. European clinical guidelines for hyperkinetic disorder: first upgrade. Eur Child Adolesc Psychiatry. 2004;13(Suppl 1):17–30.
Schneider BN, Enenbach M. Managing the risks of ADHD treatments. Curr Psychiatry Rep. 2014;16(10):479.
Cortese S, Holtmann M, Banaschewski T, et al. Practitioner review: current best practice in the management of adverse events during treatment with ADHD medications in children and adolescents. J Child Psychol Psychiatry. 2013;54(3):227–46.
Hanwella R, Senanayake M, de Silva V. Comparative efficacy and acceptability of methylphenidate and atomoxetine in treatment of attention deficit hyperactivity disorder in children and adolescents: a meta-analysis. BMC Psychiatry. 2011;11:176.
Bushe CJ, Savill NC. Suicide related events and attention deficit hyperactivity disorder treatments in children and adolescents: a meta-analysis of atomoxetine and methylphenidate comparator clinical trials. Child Adolesc Psychiatry Ment Health. 2013;7:19.
Sangal RB, Owens J, Allen AJ, Sutton V, Schuh K, Kelsey D. Effects of atomoxetine and methylphenidate on sleep in children with ADHD. Sleep. 2006;29(12):1573–85.
Garg J, Arun P, Chavan BS. Comparative short term efficacy and tolerability of methylphenidate and atomoxetine in attention deficit hyperactivity disorder. Indian Pediatr. 2014;51(7):550–4.
Wang Y, Zheng Y, Du Y, et al. Atomoxetine versus methylphenidate in paediatric outpatients with attention deficit hyperactivity disorder: a randomized, double-blind comparison trial. Aust N Z J Psychiatry. 2007;41(3):222–30.
Purgato M, Barbui C, Stroup S, Adams C. Pragmatic design in randomized controlled trials. Psychol Med. 2014;2:1–6.
Panei P, Arcieri R, Vella S, Bonati M, Martini N, Zuddas A. Italian attention-deficit/hyperactivity disorder registry. Pediatrics. 2004;114(2):514.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
Panei P, Arcieri R, et al. Italian Register of ADHD (attention deficit hyperactivity disorder): first year report (2007–2008) [in Italian]. 2008. Rapporti ISTISAN 08/35: p. 31.
Ruggiero S, Rafaniello C, Bravaccio C, et al. Safety of attention-deficit/hyperactivity disorder medications in children: an intensive pharmacosurveillance monitoring study. J Child Adolesc Psychopharmacology. 2012;22(6):415–22.
Italian Medicines Agency. Available at: http://www.agenziafarmaco.gov.it/wscs_render_attachment_by_id/111.18359.11338317741280417.pdf?id=111.18364.1133831774289. Accessed 10 July 2015.
Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–6.
Vitiello B, Elliott GR, Swanson JM, et al. Blood pressure and heart rate over 10 years in the multimodal treatment study of children with ADHD. Am J Psychiatry. 2012;169:167–77.
US FDA. Drug safety warning. Available at: http://www.fda.gov/Drugs/DrugSafety/DrugSafetyNewsletter/ucm110235.htm#AtomoxetineMarketedasStrattera:SeriousLiverInjury. Accessed 10 July 2015.
US FDA. Drug safety warning. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/PublicHealthAdvisories/ucm051733.htm. Accessed 10 July 2015.
Italian Medicines Agency. Available at: http://www.agenziafarmaco.gov.it/it/content/nota-39. Accessed 10 July 2015.
Kratochvil CJ, Wilens TE, Greenhill LL, et al. Effects of long-term atomoxetine treatment for young children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2006;45:919–27.
Acknowledgments
The authors would like to thank Profs. Rossi and Pascotto and Dr. Bravaccio for their contribution to a previous version of this manuscript, as well as all participating Regional Reference Centres: Region Liguria (Dr. Edvige Veneselli, Dr. Maria Josè Baldizzone, Dr. Gianni De Nobili); region Lazio (Dr. Marco Marcelli, Prof. Maria Giulia Torrioli, Dr. Stefano Vicari, Dr. Sandro Bartolomeo, Prof. Paolo Curatolo, Prof. Roberta Penge, Prof. Antonio Persico, Dr. Maria Grazia Melegari, Dr. Renato Donfrancesco); region Emilia-Romagna (Dr. Stefano Palazzi, Dr. Antonella Squarcia, Dr. Stefano Trebbi, Dr Roberto Parisi, Dr. Nicoletta Modena, Dr. Flaviana Murru, Dr. Andrea Tullini, Dr. Simona Chiodo); region Veneto (Dr. Ettore Morbin, Prof. Bernardo Dalla Bernardina, Dr. Dino Maschietto, Dr.ssa Cristina Mambelli, Prof. Antonio Condini, Dr. Maurizio Brighenti, Dr. Piergiorgio Miottello, Dr. Roberto Tombolato, Dr Lenio Rizzo, Dr. Maria Rondinone, Dr. Alberto Angarano); region Sicilia (Dr. Sebastiano Musumeci, Dr. Giancarlo Costanza, Dr. Donatella Ragusa, Dr. Giuseppe Santangelo, Gaetano Tortorella, Dr. Renata Rizzo); region Friuli Venezia Giulia (Dr. Antonella Merlo, Dr. Marco Carrozzi, Dr. Giuseppe Zappulla); region Lombardia (Dr. Alberto Ottolini, Dr. Daniele Arisi, Prof. Alessandra Tiberti, Dr. Maria L. Terragni, Dr. Paola Morosini, Dr. Corrado Meraviglia, Prof. Carlo Lenti, Dr. Marco Pezzani, Prof. Umberto Balottin, Prof. Paolo Piccinelli, Dr. Simonetta Oriani, Dr. Emilio Brunati, Dr. Massimo Molteni, Dr. Francesco Rinaldi, Dr. Giorgio Rossi, Dr. Roberto Segala, Dr. Ottaviano Martinelli, Dr. Antonella Costantino, Dr. Francesco Bossi); region Piemonte (Dr. Flavio Guccione, Dr. Paolo Bailo, Dr. Bianca Bassi, Dr. Marco Rolando, Dr. Francesca Ragazzo, Prof. Orazio Pirro, Dr. Giovanni Galloni, Dr. Ilaria Maraucci); region Sardegna (Prof. Alessandro Zuddas, Prof. Massimo Tondi); province Bolzano (Prof. Andreas Conca, Dr. Gianni de Polo, Dr. Donatella Arcangeli, Dr. Ingo Stermann); province Trento (Dr. Costanza Giannelli); region Val D’Aosta (Dr. Giovanni Voltolin); region Abruzzo (Dr. Maria Pia Legge, Prof. Enzo Sechi, Dr. Elena Gennaro); region Calabria (Dr. Antonio La Vitola, Dr. Antonia Zavettieri, Dr. Daniela Mallamaci); region Puglia (Dr. Angelo Spina, Prof. Lucia Margari, Dr. Angelo Massagli); region Campania (Prof. Antonio Pascotto, Dr.ssa Carmela Bravaccio, Prof. Francesco Rossi, Dr.ssa Annalisa Capuano, Dr. Rosario Granato, Dott.ssa Giampina Grimaldi); region Umbria (Prof. Giovanni Mazzotta); region Toscana (Dr. Gabriele Masi, Prof. Giovanni Cioni); region Marche (Dr. Maurizio Pincherle, Dr. Vera Stoppioni, Dr. Rosolino Tasca, Dr. Maria Antonietta Tavoni).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures of potential conflict of interest
Prof. Curatolo has received honoraria from Shire for participation in Advisory Board Meetings. Drs. Cortese, Panei, Arcieri, Germinaro, Capuano, Margari, and Chiarotti declare no competing interests.
Research involving human participants
The study was approved by the Ethic Committee of the Italian National Institute of Health in 2005. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
No funding was used to assist with the conduct of the study or the preparation of this manuscript.
Informed consent
Informed consent was obtained from all individual patients whose data was extracted from the Italian ADHD Registry and used in the analysis presented in this manuscript.
Rights and permissions
About this article
Cite this article
Cortese, S., Panei, P., Arcieri, R. et al. Safety of Methylphenidate and Atomoxetine in Children with Attention-Deficit/Hyperactivity Disorder (ADHD): Data from the Italian National ADHD Registry. CNS Drugs 29, 865–877 (2015). https://doi.org/10.1007/s40263-015-0266-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-015-0266-7