Abstract
The diagnosis of cutaneous lymphomas is challenging and requires skin tissue for histology and immunophenotyping using immunohistochemistry and molecular studies. In recent years, the role of non-invasive imaging techniques has been described as part of the clinical assessment of cutaneous lymphoma lesions. Imaging modalities such as dermoscopy, reflectance confocal microscopy (RCM), and high frequency ultrasound (HFUS) have been shown to be very valuable in raising the clinical suspicion for lymphomas of the skin, and in distinguishing cutaneous lymphomas from inflammatory dermatoses such as lupus, psoriasis, or eczema. These non-invasive methods can be used to direct the clinician to the optimal biopsy site to maximize the histopathological results and minimize false negatives. These methods also have a potential place in monitoring treatment response. In this review we present a concise summary of the dermoscopic imaging, RCM, and HFUS features seen in cutaneous T-cell lymphomas (CTCL) and B-cell lymphomas (CBCL).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Imaging modalities such as dermoscopy, reflectance confocal microscopy, and high frequency ultrasound are useful in the assessment of cutaneous lymphoma lesions. |
Non-invasive techniques have a promising role in raising suspicion of lymphomas of the skin and in distinguishing cutaneous lymphomas from inflammatory dermatoses such as lupus, psoriasis, or eczema. These non-invasive methods can be used to direct the clinician to the optimal biopsy site to maximize the histopathological results and minimize false negatives. |
1 Introduction
Cutaneous lymphomas are a heterogeneous group of distinct B-cell and T-cell neoplasms that originate in the skin. The diagnosis of cutaneous lymphomas can be difficult due to the clinical and histological overlap with other dermatologic disorders and between the different skin lymphoma subtypes. A histopathological correlation is of pivotal importance in the correct diagnosis of cutaneous lymphomas. It is not uncommon that multiple dermatologist consultations and skin biopsies may be required before a diagnosis of cutaneous lymphoma is made.
Non-invasive imaging techniques such as dermoscopy, reflectance confocal microscopy (RCM), and high frequency ultrasound (HFUS) have been proven to be useful in the assessment of cutaneous lymphoma lesions, offering a link between the clinical appearance and histopathology features. Although such skin imaging modalities cannot replace tissue biopsy for immunophenotyping, molecular and genetic analyses, which are mandatory for accurate skin lymphoma diagnosis, these non-invasive methods do have a role in raising suspicion of lymphoma of the skin, leading to a skin biopsy and directing the optimal lesion and the exact location for sampling.
2 Dermoscopy in Cutaneous Lymphomas
Dermoscopy is a widely used and inexpensive non-invasive technique to better characterize dermatological lesions. While many of the dermoscopic features of primary cutaneous lymphomas are non-specific, dermoscopic evaluation can be a helpful tool in increasing the index of suspicion for cutaneous lymphoma as a differential diagnosis [1]. Moreover, dermoscopy may be a useful diagnostic aid when differentiating primary cutaneous lymphoma from other inflammatory and tumorous conditions that may appear indistinguishable on clinical assessment alone [2].
Primary cutaneous lymphomas most commonly present on dermoscopy as organized lesions with orange/salmon-colored background and follicular plugs [3]. In a retrospective comparative study by Errichetti et al., structureless orange areas were the strongest predictor of primary cutaneous lymphoma when compared with tumorous lesions and non-infiltrative dermatoses such as discoid lupus erythematosus and granuloma faciale [2]. Out-of-focus short linear vessels with branches (Fig. 1) and focal white structureless areas have also been reported and are positively associated with primary cutaneous lymphomas when compared with infiltrative dermatoses in particular, including granulomatous dermatoses and histiocytoses [2].
2.1 Dermoscopy in Cutaneous T-Cell Lymphomas
The dermoscopic findings of classic mycosis fungoides (MF) have been better described than other subtypes of cutaneous T-cell lymphomas (CTCL). Patch stage MF shows a characteristic vasculature pattern consisting of fine short linear vessels and spermatozoa-like structures that are composed of a dotted vessel adjacent to a short curved vessel [4, 5]. White scales in the skin furrows can also be present [4]. Dotted vessels are similarly seen in plaque-stage MF, but tend to have a clustered arrangement with a non-specific distribution [4]. In tumor-stage MF, ulceration, peripheral linear vessels with branches, and red globules separated by white lines are common [4]. Orange structureless areas can be seen in all stages of classic MF. In patch and plaque stages, these regions correspond to dermal hemosiderin deposits on histopathology [4, 5]. In tumor-stage MF, the orange structureless areas reflect dense cellular infiltrate on histopathology [3, 4].
Dermoscopy of several MF variants have also been described in the literature, albeit to a lesser degree. Folliculotropic MF has a highly variable dermoscopic presentation, making clinical and histopathological correlation important for accurate diagnosis [6]. Loss of hairs, dilated follicles, perifollicular accentuation presenting as white halos, comedo openings, and follicular plugs have all been reported [4, 5]. The erythrodermic variant of MF has been characterized on dermoscopy by linear and dotted vessels, patchy white scales, and focal white-pinkish and orange structureless areas [4, 7]. Scalp examination using trichoscopy in patients with erythrodermic CTCL may be particularly useful, with one study of 16 patients with erythrodermic CTCL reporting pili torti, broken hairs, white thick interfollicular bands, and patchy background hyperpigmentation present in 81%, 75%, 56%, and 38% of patients, respectively [8]. Finally, few studies on the dermoscopy of poikilodermatous MF exist, although the cases that have been reported describe white and brown structureless areas, white patchy scales, and brown reticular lines as prominent features [4].
Several studies have investigated the dermoscopic differences between MF and other common inflammatory conditions. When compared with diseases like chronic dermatitis, psoriasis, lichen planus, pityriasis rosea, and nummular dermatitis, spermatozoa-like vessels and white scales are significantly more prominent in MF [9,10,11,12]. Such spermatozoa-like structures have been reported as 100% specific for early-stage MF but only 74.2% sensitive [10, 11]. Fine short linear vessels have a higher sensitivity of 93.7% for early-stage MF with a specificity of 97.1% [10, 11]. Finally, orange-yellowish patchy areas, another characteristic feature of CTCL, have had sensitivities and specificities of 90.6% and between 91.4% and 99.7% reported, respectively [10, 11].
Of the CD30-positive T-cell lymphoproliferative disorders, the dermoscopy of lymphomatoid papulosis (LyP) has been best described. Moura and colleagues characterized the dermoscopic findings at different stages of the disease in a cohort of eight patients with LyP. As an erythematous papule, LyP demonstrates tortuous, irregular vessels radiating from the lesion center with a surrounding white structureless area [13]. When the lesions become hyperkeratotic, they contain a similarly tortuous vessel pattern; however, unlike in the erythematous stage, these vessels spare the central region of the lesion [13]. White structureless areas are also seen in the hyperkeratotic papules [13]. In the necrotic papule stage, the characteristic tortuous vessel pattern can only be seen at the far periphery of the lesion, with the central area consisting of a brown-gray area corresponding to fibrinoid material [13]. Finally, in the cicatricial stage, no vessels can be identified and only a brown-gray structureless area remains representing postinflammatory pigmentation [13, 14]. The dermoscopic features of various CTCL subtypes are presented in Table 1.
2.2 Dermoscopy in Cutaneous B Cell Lymphomas
Although studies assessing dermoscopy of cutaneous B-cell lymphomas (CBCL) are limited, a characteristic dermoscopic pattern has been described. Early case series first reported features of white circles with salmon-colored areas, scales, and arborizing vessels in CBCL lesions [15, 16]. In 2018, Geller et al. performed a retrospective study evaluating the dermatoscopic findings of 58 primary CBCLs. The authors confirmed that nearly 80% of lesions demonstrated a salmon-colored background. Prominent blood vessels were seen in a majority of the lesions, two-thirds of which had a notable serpentine morphology [17]. Importantly, dermoscopic findings did not differ between CBCL subtypes, highlighting the diagnostic limitations of this tool [17].
While less common than the salmon-colored areas and serpentine vessels, crystalline structures and pseudopod-like vessels have also been reported as CBCL dermoscopic features [18] as have vessels with a fine, short, linear, and irregular pattern [5]. Additionally, in one case report, notable yellow plugs surrounded by well-defined white circles were evident on dermoscopy of a patient with CBCL [19]. The pronounced follicular plugging corresponded to an upward epidermal displacement caused by the underlying dermal lymphocytic infiltrate [19]. Table 2 summarizes the dermoscopic features found in CBCL.
3 Reflectance Confocal Microscopy in Cutaneous Lymphomas
RCM is an imaging technique with cellular resolution (lateral resolution 0.5–1 µm, 3.5–4 µm optical sectioning), which allows in vivo visualization of horizontal sections of skin. Due to its high resolution, it is possible to obtain near-histological greyscale images but limited to a depth of around 250 µm (papillary dermis) [20]. In addition, RCM visualizes better structures with high refractility such as melanin and keratin (seen as white), as opposed to structures with low refractility such as water present mostly in the nuclei of cells (seen as black) [21].
RCM has been used in the diagnosis and treatment monitoring of skin lymphomas, mostly CTCL since B-cell lymphomas are mostly dermal and cannot be easily evaluated with RCM. Therefore, the usefulness of RCM in cutaneous lymphomas is limited to the depth of penetration (RCM cannot clearly see the reticular dermis) and the limited refractility of atypical lymphocytes, which can make the diagnosis of cutaneous lymphomas challenging also under the lens of RCM. In addition, RCM does not allow performing immunohistochemical or molecular studies, which can be crucial not only from a diagnostic standpoint, but also from a therapeutic standpoint (i.e., the presence of CD30+ cells, which could be treated with brentuximab). Nevertheless, if available, RCM is a very valuable tool in distinguishing cutaneous lymphomas from other erythematosquamous conditions such as lupus, psoriasis, or eczema, helps selecting the best biopsy site in order to maximize the histopathological results and minimize false negatives [22,23,24,25], and enables treatment monitoring [26, 27].
3.1 Reflectance Confocal Microscopy in Cutaneous T-Cell Lymphomas
Several studies and case reports have described the RCM features in different CTCLs, mostly MF and to a lesser extent LyP. RCM allows the visualization of epidermal changes such as the presence of epidermal lymphocytes, as well as the presence of an inflammatory infiltrate in the dermal–epidermal junction (DEJ) and upper dermis. However, although RCM has cellular resolution, it is limited to the nuclear contour and does not allow the visualization of nuclear atypia, a key feature to diagnose CTCL [28]. Nevertheless, the presence of several RCM features may be suggestive of CTCL in the appropriate clinical context.
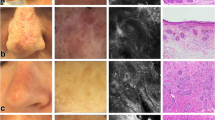
In 2007, Agero et al. first described the RCM features on a series of seven patients with MF [23]. They classified the features according to the clinical presentation: patch, plaque, and tumor stages. They identified the presence of single lymphocytes (epidermotropism/exocytosis) in the epidermis seen as weakly refractile round cells, mostly in patch and plaque stages (Fig. 1). They also identified aggregates of lymphocytes in the epidermis mostly in the plaque stage and less in patch stage, correlating histologically with Pautrier’s microabscesses (Fig. 2). Also, they identified the presence of disruption of the normal dermal papillae (non-edged papillae, seen as hyporefractile dermal papillae), thus revealing disruption the DEJ caused by atypical lymphocytes (Fig. 1). This was present mostly in the patch and plaque stage. In tumor stage, their findings were limited since they only included one case and the imaging depth was limited to the papillary dermis; however, they observed non-edged papillae (disruption of the DEJ) and to a lesser extent epidermal lymphocytes.
Mycosis fungoides, patch stage. Clinical and RCM images. a Hyperpigmented patch of mycosis fungoides located on the sole of a 55-year-old male patient. b RCM images showing parakeratosis (oval) in the stratum corneum surrounding eccrine gland opening; c spongiosis (circle) and exocitosis of inflamatory cells (arrows); d Pautrier's micro-abscesses in the epidermis (cirles); e inflammatory cells at the level of the DEJ with partial obscuration of the DP rimming (non-edge papillae); and f sclerosis of the superficial dermis. DEJ dermal-epidermal junction, DP dermal papillae, RCM reflectance confocal microscopy
Further studies confirmed these findings and described some additional ones such as the presence of epidermal disarray [25, 29, 30], blood vessel dilation [29], and dermal fibrosis [29], among others features, which were summarized in a systematic review [28] (Table 3). Regarding MF variants, folliculotropic MF also presents with fibrosis and lymphocyte infiltration surrounding the hair follicles [29, 31], and transformed MF presents with large hyperrefractile roundish pleomorphic cells in the epidermis [32], on top of the aforementioned RCM features in MF. In an attempt to distinguish MF from other erythematosquamous dermatoses such as psoriasis, eczema, or lupus, Koller et al. [33] showed that the classic RCM findings for MF (interface dermatitis, exocytosis, dermal lymphocytes) had a sensitivity and specificity of 63.33% and 92.89%, respectively. Regarding Sézary syndrome (SS) and erythrodermic MF [29], the presence of dilated blood vessels is the most prominent and distinctive RCM feature of this form of CTCL. Additionally, it is also possible to identify atypical cells in the epidermis, DEJ, and dermis.
LyP is the other CTCL where RCM has been shown to be of significant utility, especially to select the best lesion to biopsy. The first three LyP cases were described in 2012 by Lange-Asschenfeldt et al. [30] in a series of patients with CTCL, although the goal of that study was to assess the interobserver reproducibility of MF features. In 2013, Ardigò et al. described the RCM features and their histopathologic correlates [24]. They identified similar findings to MF such as atypical cells in the epidermis (either isolated or aggregated), as well as disruption in the DEJ (Fig. 3). Additionally, they also identified spongiosis, parakeratosis, dermal fibrosis, and dermal lymphocytes in a significant number of cases. Interestingly, they did not see epidermal disarray in any of their cases as opposed to the Lange-Asschenfeldt et al. series. A summary of the most relevant RCM features of LyP can be found in Table 4.
Lymphomatoid papulosis. Clinical and RCM images. a Partially necrotic papule of lymphomatoid papulosis on the left right arm of a 35-year-old female patient. b RCM image of the stratum corneum with focal parakeratosis (circle); c diffuse exocytosis of highly refractile inflammatory cells in the epidermis; d 1.5 mm × 1.5 mm block showing diffuse distribution of inflammatory cells in the epidermis (arrows); e non-edge papillae with obscuration of the DEJ by dense infiltrate of inflammatory cells (arrows); and f dermal sclerosis with inflammatory cells (arrows) in the upper dermis and dilated vessels (circle). DEJ dermal-epidermal junction, RCM reflectance confocal microscopy
3.2 Reflectance Confocal Microscopy in Cutaneous B-Cell Lymphomas
Since CBCLs are, by definition, dermal proliferations, the description of RCM features in these tumors is anecdotal due to its limited depth penetration. In fact, most of the scarce cases described come from ophthalmological journals in which RCM has been used to assess thin B-cell lymphomas of the conjunctiva. These cases correspond to mucosa-associated lymphoid tissue (MALT) lymphomas and under confocal microscopy showed hyperrefractile roundish cells in the stroma, together with a normal epithelium [34, 35]. Regarding skin CBCL, only one case has been reported by Laghi et al. [36] who described a secondary cutaneous follicular B-cell lymphoma on the scalp with dermoscopy, RCM, and histology. In RCM, they identified nucleated cellular infiltration and fibrosis in the papillary dermis surrounding the adnexa, which corresponded to atypical lymphocytes on histology.
4 High Frequency Ultrasound in Cutaneous Lymphomas
In recent years, HFUS has become an integral non-invasive clinical imaging tool in dermatology [37]. High frequency probes (≥ 15 MHz) produce high resolution images in vivo, which are ideal for examining the skin and its appendages [38, 39]. While some cutaneous neoplasms, such as basal cell carcinoma, have been well studied using dermatologic sonography [40], the study of sonographic features of primary cutaneous lymphomas are limited and scarce. Although HFUS has high sensitivity for diagnosis of primary cutaneous lymphomas, it has a low specificity and a histological assessment is required to confirm the diagnosis [41]. Furthermore, HFUS can underestimate the disease burden in patients with multifocal lesions [41]. This imaging modality, however, may be helpful in monitoring the therapeutic response to various treatments of cutaneous lymphomas, including brachytherapy, particularly in MF, and also topical medications [42].
In 1997, Giovangnorio et al. were the first to describe the sonographic characteristics of primary cutaneous lymphomas. Their study identified that CBCLs produce sharply delineated nodular patterns while CTCLs present sonographically with more diffuse dermal involvement [43]. It appears that the sonographic features of cutaneous lymphoma are mostly homogeneously hypoechoic (Fig. 4), except the panniculitis like T-cell lymphoma [44]. These homogeneous patterns correspond to the large and uniform clusters of the atypical lymphocytes seen in histology [45, 46]. Years later, a retrospective series by Mandava and colleagues disclosed four sonographic patterns of primary cutaneous lymphoma: nodular, pseudo-nodular, focal, and diffuse infiltrative [47]. In this study, 70% of CBCL had nodular or pseudonodular patterns, while only half of the infiltrative types were CTCL. All examined cases of skin lymphomas showed a thick dermis with no evidence of calcifications, posterior artifacts, or necrosis. Hypervascularity was more prominent in the nodular and pseudonodular types. In general, it seems that there is a positive correlation between the hypervascularity of the lesions as seen by HFUS and the severity of the cutaneous lymphoma [46].
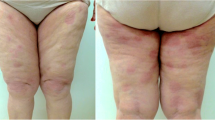
Mycosis fungoides, tumor stage. Clinical dermoscopy and high frequency ultrasound (HFUS) images. a Red tumor (arrow) and pink patches on the medial thigh of a 75-year-old female patient. b Dermoscopic imaging of the lesion showed dotted vessels, white scale, and bright white lines with orange structureless areas. c HFUS of the tumor shows thickened dermis and hypodermis with hypoechoic to unechoic dermis and hyperechoic hypdermis, with d significant vascularization of the tumor
4.1 High Frequency Ultrasound in Cutaneous T-Cell Lymphomas
The sonographic features of CTCL have been studied more than CBCL. HFUS may be particularly helpful in monitoring treatment response to brachytherapy in CTCL. A subepidermal low echogenic band (SLEB), thick dermis, and thick epidermis are the most common sonographic characteristics of CTCL, particularly in MF [48]. The SLEB is a well-recognized sonographic characteristic of inflammatory dermatosis including psoriasis and atopic dermatitis [49, 50]. In CTCL, the hypoechogenicity of this band is attributed to the loss of impedance second to the accumulation of lymphocytes in the upper dermis [9]. Polanska et al. demonstrated a significant positive correlation between the severity and activity of CTCL and the band’s thickness. The thickness of the SLEB was higher in plaque stage compared to the patch stage of MF. Moreover, in cases of clinical response to treatment, the SLEB disappeared or flattened [51,52,53]. Recently, Wang et al. described more detailed sonographic characteristics of the stages of MF, SS, and folliculotropic MF (Table 5) [52]. As the stages of MF are more advanced the epidermis becomes less even and the SLEB is wider with unclear boundaries [53]. In both folliculotropic MF and SS there is evidence of wide hypoechoic follicular opening, sometimes with hyperechoic spots within it [45]. Nonetheless, this research lacks data regarding of the vascularization of the lesions.
4.2 High Frequency Ultrasound in Cutaneous B-Cell Lymphomas
Only few publications discuss the sonographic features of CBCL [54,55,56]. Torres et al. published the sonographic evaluation of 12 patients divided to the major three subtypes of CBCL. The low grade CBCL have a predominant nodular or pseudonodular appearance, while the more aggressive form has a more heterogeneous presentation. Hypervascularization is notable in all types [54]. Of note, the presence of SLEB was not mentioned in any study of CBCL.
Cutaneous pseudolymphomas may sonographically resemble CBCL. Wortsman et al. described a case series of ten patients with lymphocytoma cutis using 18 MHz and 71 MHz transducers [57]. Two-thirds of lesions involved the dermis and hypodermis, while other cases involved only the dermis. The globule sign (hypoechoic nodular or pseudonodular areas within the lesions) and the teardrop sign (hypoechoic structure with a triangular shape within the lesions) were investigated. On color doppler, all cases presented with internal vascularity [57].
5 Conclusion
Dermoscopy, RCM, and HFUS are useful techniques for the non-invasive evaluation of cutaneous lymphomas. These tools, however, are limited and oftentimes non-specific, necessitating clinical and pathological correlation for definitive diagnosis. On dermoscopy, the presence of dotted vessels is more common in CTCL than CBCL, the latter of which shows a characteristic salmon-colored background and serpentine vasculature pattern. On RCM, CTCL presents with atypical cells in the epidermis and disruption of the DEJ. The shallow depth of RCM penetration limits the utility of this tool for CBCL lesions. The literature on HFUS for primary cutaneous lymphomas is scarce, with studies on CTCL and CBCL reporting the non-specific presence of SLEBs and hypervascularization, respectively. In conclusion, although further studies are needed, recognizing the prominent features of primary cutaneous lymphoma on non-invasive imaging modalities can guide clinicians in diagnosis and assist in treatment response monitoring and identification of recurrence.
References
Geller S, Navarrete-Dechent C, Myskowski PL. Dermoscopy in lymphoproliferative disorders-experience from a cutaneous lymphoma clinic in a tertiary cancer center. J Am Acad Dermatol. 2019;80(6):e171–2.
Errichetti E, Geller S, Zalaudek I, Longo C, Kyrgidis A, Akay BN, et al. Dermatoscopy of nodular/plaque-type primary cutaneous T- and B-cell lymphomas: a retrospective comparative study with pseudolymphomas and tumoral/inflammatory mimickers by the International Dermoscopy Society. J Am Acad Dermatol. 2022;86(4):774–81.
Navarrete-Dechent C, Del Puerto C, Abarzúa-Araya Á, Molgó M, Geller S, Andreani S, et al. Dermoscopy of primary cutaneous B- and T-cell lymphomas and pseudolymphomas presenting as solitary nodules and tumors: a case–control study with histopathologic correlation. Int J Dermatol. 2019;58(11):1270–6.
Errichetti E, Apalla Z, Geller S, Sławińska M, Kyrgidis A, Kaminska-Winciorek G, et al. Dermoscopic spectrum of mycosis fungoides: a retrospective observational study by the International Dermoscopy Society. J Eur Acad Dermatol Venereol. 2022;36(7):1045–53.
Sławińska M, Sokołowska-Wojdyło M, Olszewska B, Nowicki RJ, Sobjanek M, Zalaudek I. Dermoscopic and trichoscopic features of primary cutaneous lymphomas—systematic review. J Eur Acad Dermatol Venereol. 2021;35(7):1470–84.
Geller S, Rishpon A, Myskowski PL. Dermoscopy in folliculotropic mycosis fungoides—a possible mimicker of follicle-based inflammatory and infectious disorders. J Am Acad Dermatol. 2019;81(3):e75–6.
Sławińska M, Sokołowska-Wojdyło M, Sobjanek M, Golińska J, Nowicki RJ, Rudnicka L. The significance of dermoscopy and trichoscopy in differentiation of erythroderma due to various dermatological disorders. J Eur Acad Dermatol Venereol. 2021;35(1):230–40.
Rakowska A, Jasińska M, Sikora M, Czuwara J, Gajda-Mróz P, Warszawik-Hendzel O, et al. Cutaneous T-cell lymphoma in erythrodermic cases may be suspected on the basis of scalp examination with dermoscopy. Sci Rep. 2021;11(1):282.
Wohlmuth-Wieser I, Ramjist JM, Shear N, Alhusayen R. Morphologic features of cutaneous T-cell lymphomas using dermoscopy and high frequency ultrasound. J Clin Med. 2020;10(1):17.
Lallas A, Apalla Z, Lefaki I, Tzellos T, Karatolias A, Sotiriou E, et al. Dermoscopy of early stage mycosis fungoides. J Eur Acad Dermatol Venereol. 2013;27(5):617–21.
Xu C, Liu J, Wang T, Luo Y, Liu Y. Dermoscopic patterns of early-stage mycosis fungoides in a Chinese population. Clin Exp Dermatol. 2019;44(2):169–75.
Bilgic SA, Cicek D, Demir B. Dermoscopy in differential diagnosis of inflammatory dermatoses and mycosis fungoides. Int J Dermatol. 2020;59(7):843–50.
Moura FN, Thomas L, Balme B, Dalle S. Dermoscopy of lymphomatoid papulosis. Arch Dermatol. 2009;145(8):966–7. https://doi.org/10.1001/archdermatol.2009.167. (PubMed PMID: 19687447).
Caccavale S, Vitiello P, Mascolo M, Ciancia G, Argenziano G. Dermoscopy of different stages of lymphomatoid papulosis. J Eur Acad Dermatol Venereol. 2018;32(5):e198–200.
Mascolo M, Piccolo V, Argenziano G, Costa C, Lo Presti M, De Rosa G, et al. Dermoscopy pattern, histopathology and immunophenotype of primary cutaneous B-cell lymphoma presenting as a solitary skin nodule. Dermatology. 2016;232(2):203–7.
Piccolo V, Mascolo M, Russo T, Staibano S, Argenziano G. Dermoscopy of primary cutaneous B-cell lymphoma (PCBCL). J Am Acad Dermatol. 2016;75(4):e137–9.
Geller S, Marghoob AA, Scope A, Braun RP, Myskowski PL. Dermoscopy and the diagnosis of primary cutaneous B-cell lymphoma. J Eur Acad Dermatol Venereol. 2018;32(1):53–6.
Ghahramani GK, Goetz KE, Liu V. Dermoscopic characterization of cutaneous lymphomas: a pilot survey. Int J Dermatol. 2018;57(3):339–43.
Conforti C, Giuffrida R, Dri A, Zalaudek I, Di Meo N. Yellow plugs: an additional dermoscopic criterion in the diagnosis of primary cutaneous B-Cell lymphoma. Dermatol Pract Concept. 2022;12(1): e2022006.
Rajadhyaksha M, González S, Zavislan JM, Anderson RR, Webb RH. In vivo confocal scanning laser microscopy of human skin II: advances in instrumentation and comparison with histology. J Investig Dermatol. 1999;113(3):293–303.
Rajadhyaksha M, Grossman M, Esterowitz D, Webb RH, Anderson RR. In vivo confocal scanning laser microscopy of human skin: melanin provides strong contrast. J Investig Dermatol. 1995;104(6):946–52 (Epub 1995/06/01 PubMed PMID: 7769264).
González S. Reflectance confocal microscopy in dermatology: fundamentals and clinical applications. González S, editor. Madrid: Aula Médica; 2012.
Agero AL, Gill M, Ardigo M, Myskowski P, Halpern AC, González S. In vivo reflectance confocal microscopy of mycosis fungoides: a preliminary study. J Am Acad Dermatol. 2007;57(3):435–41.
Ardigò M, Donadio C, Vega H, Cota C, Moscarella E, Agozzino M. Concordance between in vivo reflectance confocal microscopy and optical histology of lymphomatoid papulosis. Skin Res Technol. 2013;19(3):308–13.
Li W, Dai H, Li Z, Xu AE. Reflectance confocal microscopy for the characterization of mycosis fungoides and correlation with histology: a pilot study. Skin Res Technol. 2013;19(3):352–5.
Ardigò M, El Shabrawi-Caelen L, Tosti A. In vivo reflectance confocal microscopy assessment of the therapeutic follow-up of cutaneous T-cell lymphomas causing scalp alopecia. Dermatol Ther. 2014;27(4):248–51.
Farabi B, Jamgochian M, Hussain A, Rao B. Reflectance confocal microscopy: a new emerging technique for diagnosing and predicting outcome of mycosis fungoides. Skin Res Technol. 2021;27(5):997–1001.
Melhoranse Gouveia B, Wells J, Kim J, Consuegra G, Longo C, Fernandez-Penas P. Systematic review and proposal of an in vivo reflectance confocal microscopy assessment tool for cutaneous lymphoma. J Cutan Pathol. 2020;47(3):295–304.
Mancebo SE, Cordova M, Myskowski PL, Flores ES, Busam K, Jawed SI, et al. Reflectance confocal microscopy features of mycosis fungoides and Sézary syndrome: correlation with histopathologic and T-cell receptor rearrangement studies. J Cutan Pathol. 2016;43(6):505–15.
Lange-Asschenfeldt S, Babilli J, Beyer M, Ríus-Diaz F, González S, Stockfleth E, et al. Consistency and distribution of reflectance confocal microscopy features for diagnosis of cutaneous T cell lymphoma. J Biomed Opt. 2012;17(1): 016001.
Fabbrocini G, Mazzella C, Cantelli M, Baldo A, Russo D, De Rosa G, et al. Reflectance confocal microscopy as new diagnostic tool in folliculotropic mycosis fungoides. Skin Appendage Disord. 2018;4(2):118–21.
Melhoranse Gouveia B, Wells J, Kim J, Ardigó M, Consuegra G, Suárez Magdalena O, et al. Reflectance confocal microscopy as a new diagnostic tool in transformed mycosis fungoides. Australas J Dermatol. 2020;61(3):e358–63.
Koller S, Gerger A, Ahlgrimm-Siess V, Weger W, Smolle J, Hofmann-Wellenhof R. In vivo reflectance confocal microscopy of erythematosquamous skin diseases. Exp Dermatol. 2009;18(6):536–40.
Pichierri P, Martone G, Loffredo A, Traversi C, Polito E. In vivo confocal microscopy in a patient with conjunctival lymphoma. Clin Exp Ophthalmol. 2008;36(1):67–9.
Cinotti E, Perrot JL, Labeille B, Campolmi N, Espinasse M, Grivet D, et al. Handheld reflectance confocal microscopy for the diagnosis of conjunctival tumors. Am J Ophthalmol. 2015;159(2):324-33.e1.
Laghi A, Lee C, Witkowski A, Hsu M, Pellacani G, Ludzik J. The role of dermatoscopy and reflectance confocal microscopy in the assessment of relapsing secondary cutaneous follicular B-cell lymphoma. JAAD Case Rep. 2022;24:91–3.
Wortsman X. Practical applications of ultrasound in dermatology. Clin Dermatol. 2021;39(4):605–23.
Jasaitiene D, Valiukeviciene S, Linkeviciute G, Raisutis R, Jasiuniene E, Kazys R. Principles of high-frequency ultrasonography for investigation of skin pathology. J Eur Acad Dermatol Venereol. 2011;25(4):375–82.
Wortsman X, Alfageme F, Roustan G, Arias-Santiago S, Martorell A, Catalano O, et al. Guidelines for performing dermatologic ultrasound examinations by the DERMUS group. J Ultrasound Med. 2016;35(3):577–80.
Catalano O, Roldán FA, Varelli C, Bard R, Corvino A, Wortsman X. Skin cancer: findings and role of high-resolution ultrasound. J Ultrasound. 2019;22(4):423–31.
Mandava A. Ultrasound of cutaneous lymphomas. In: Wortsman X, editor. Textbook of dermatologic ultrasound. Cham: Springer; 2022. p. 251–8.
Shukla G, Lockamy V, Keller J, Sahu J, Pro B, Alpdogan O, et al. High dose rate (HDR) brachytherapy for mycosis fungoides of the wrist. Int J Clin Med. 2015;6(3):154–7.
Giovagnorio F. Sonography of cutaneous non-Hodgkin’s lymphomas. Clin Radiol. 1997;52(4):301–3.
Jeong SI, Lim HS, Choi YR, Kim JW, Park MH, Cho JS, et al. Subcutaneous panniculitis-like T-cell lymphoma of the breast. Korean J Radiol. 2013;14(3):391–4.
Wortsman X. Dermatologic ultrasound with clinical and histologic correlations. New York: Springer; 2013.
Chiou HJ, Chou YH, Chiou SY, Chen WM, Chen W, Wang HK, et al. High-resolution ultrasonography of primary peripheral soft tissue lymphoma. J Ultrasound Med. 2005;24(1):77–86.
Mandava A, Koppula V, Wortsman X, Catalano O, Alfageme F. The clinical value of imaging in primary cutaneous lymphomas: role of high resolution ultrasound and PET-CT. Br J Radiol. 2019;92(1095):20180904.
Polańska A, Dańczak-Pazdrowska A, Jałowska M, Żaba R, Adamski Z. Current applications of high-frequency ultrasonography in dermatology. Postepy Dermatol Alergol. 2017;34(6):535–42.
Crișan M, Badea R, Crisan D, Bezugly A, Colosi H, Strilciuc S, Ciobanu A, Crivii CB. Ultrasonography as a new, non-invasive imagistic technique used for the diagnosis and monitoring of psoriasis. IntechOpen. 2017. https://doi.org/10.5772/67812.
Dańczak-Pazdrowska A, Polańska A, Silny W, Sadowska A, Osmola-Mańkowska A, Czarnecka-Operacz M, et al. Seemingly healthy skin in atopic dermatitis: observations with the use of high-frequency ultrasonography, preliminary study. Skin Res Technol. 2012;18(2):162–7.
Polańska A, Bowszyc-Dmochowska M, Olek-Hrab K, Adamski Z, Żaba R, Dańczak-Pazdrowska A. High-frequency ultrasonography a new quantitative method in evaluation of skin lymphomas—first comparative study in relation to histopathology. Skin Res Technol. 2019;25(5):720–4.
Wang Y, Niu Z, Liu J, Zhu Q, Liu Z, Liu Y, et al. Value of high-frequency ultrasound in accurate staging of mycosis fungoides/Sézary syndrome. J Ultrasound Med. 2020;39(10):1927–37.
Polańska A, Dańczak-Pazdrowska A, Olek-Hrab K, Osmola-Mańkowska A, Bowszyc-Dmochowska M, Żaba R, et al. High-frequency ultrasonography-New non-invasive method in assessment of skin lymphomas. Skin Res Technol. 2018;24(3):517–21.
Torre-Castro J, Moya-Martínez C, Mendoza-Cembranos MD, Macías-Del-Toro E, Díaz-Recuero JL, Machan S, et al. Sonographic appearance of primary cutaneous B-cell lymphomas. Int J Dermatol. 2021;60(9):1156–8.
Genovese G, Nazzaro G, Alberti Violetti S, Passoni E, Berti E. Rosacea-like cutaneous localization of small lymphocytic lymphoma unmasked by high-frequency-ultrasound. Skin Res Technol. 2018;24(4):701–3.
Rodríguez Bandera AI, Moreno Bonilla G, Feito Rodríguez M, Beato Merino MJ, de Lucas LR. Usefulness of high-frequency ultrasonography in the assessment of cutaneous lesions in children with hematologic malignancies. Pediatr Dermatol. 2018;35(5):e276–80.
Wortsman X, Ferreira-Wortsman C, Pizarro K, Morales C. Ultrasonography of cutaneous nodular pseudolymphoma at 18 and 71 MHz. Skin Res Technol. 2022;28(1):176–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the NIH/NCI Cancer Center (Support Grant P30 CA008748).
Conflict of interest
Author Taleb declares that they have no conflicts of interest that might be relevant to the contents of this manuscript. Author Yélamos has received consultancy honoraria from Almirall, Bioderma, Isispharma and Leo Pharma, and speakers’ honoraria from Almirall, BMS, Isdin, Isispharma, Jannsen-Cilag, La Roche Posay, Leo Pharma, MSD, Pierre Fabre, and Viatris. Author Ardigo has received consultancy honoraria from Recordati Rare Diseases, and Helsinn; speaker honoraria from Recordati rare diseases, Kyowa Kirin, and Mavig GmbH; and is a lecturer for Vivascope GmbH, Recordati Rare Diseases, Helsinn, kyowa Kirin, Takeda. Author Christensen declares that they have no conflicts of interest that might be relevant to the contents of this manuscript. Author Geller has received speakers’ honoraria from Rafa and Takeda.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Freely given, informed consent was obtained from all participants to have their data published in a journal article.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Code availability
Not applicable.
Authors’ contributions
Taleb: data curation (equal), formal analysis (equal), investigation (equal), writing original draft (equal), and writing review and editing. Yélamos: data curation (equal), formal analysis (equal), investigation (equal), methodology (equal), supervision, writing original draft (equal), and writing review and editing (equal). Ardigo: data curation (equal), formal analysis (equal), investigation (equal), and writing review and editing (equal). Christensen: data curation (equal), formal analysis (equal), investigation (equal), writing original draft (equal), and writing review and editing (equal). Geller: data curation (equal), formal analysis (equal), funding acquisition, investigation (equal), methodology (equal), project administration, resources, supervision, and writing review and editing (equal).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taleb, E., Yélamos, O., Ardigo, M. et al. Non-invasive Skin Imaging in Cutaneous Lymphomas. Am J Clin Dermatol 25, 79–89 (2024). https://doi.org/10.1007/s40257-023-00824-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-023-00824-1