Abstract
Purpose
Lifestyle changes in diabetes mellitus leads to metabolic syndrome, thus resulting in a hike in micro and macrovascular complications in diabetes mellitus patients. The main objective of the study was to identify the occurrence of metabolic syndrome and to evaluate the gender-associated difference in each component of metabolic syndrome by using International Diabetic Federation (IDF) and National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III)criteria.
Methods
This is a cross-sectional study conducted in 350 type II diabetes mellitus patients. All the study participants within 30–80 years were enrolled. Subjects with type I DM and pregnant women were excluded from the study.
Results
The occurrence of metabolic syndrome among the diabetic population was found to be 42.28% and 28.85% using the IDF and the NCEP ATP III criteria respectively. It was observed that the prevalence was found to be higher in females than males as per IDF and NCEP ATP III criteria and was found to be statistically significant (p < 0.001). Central obesity elevated blood pressure, and reduced high-density lipoprotein was significantly higher in female patients. The most frequently occurring risk factor in this study population was central obesity followed by hypertension. A comparative analysis of IDF and NCEP ATP III criteria implies that when compared to diabetes patients without metabolic syndrome, all the metabolic risk elements were significantly higher in diabetes patients with metabolic syndrome.
Conclusions
This study concluded that the occurrence of metabolic syndrome was dreadfully high among the diabetic population, especially among female subjects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes Mellitus (DM) is a metabolic disease defined by hyperglycemia due to defects in insulin secretion, insulin action, or both. The predominance of diabetes has increased worldwide in both genders equally [1]. There is a dramatic increase in the ubiquity of diabetes owing to modernization and urbanization that has brought about a substantial burden on health care services [1, 2]. Metabolic syndrome (Met S) is defined as a cluster of cardiovascular risk factors which include raised fasting plasma glucose, central obesity, hypertension, raised triglycerides, and reduced High-Density Lipoprotein (HDL) cholesterol. Met S is known to be caused by insulin resistance or insulin resistance-linked obesity also known as syndrome X or insulin resistance syndrome; it has been recognized since the 1980s [3]. The guidelines for the diagnosis of metabolic syndrome have been given by different organizations such as World Health Organization (WHO), International Diabetic Federation (IDF), and National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) imparted a new working definition of the metabolic syndrome and thus, it is easily applicable and provides strong clinical evidence [3, 4]. DM is associated with a three to fivefold increased risk for the development of Metabolic Syndrome (Met S) which has now reached high proportions in many countries. The worldwide prevalence of Met S is between 7.9–43% in males and 7–56% in females. The Met S is influenced by several factors, some of which can accelerate the disease progression to various complications that aggravate the morbidity [5]. Studies on the prevalence of Met S among type II DM patients are still lacking in India especially in south India. There is a high need for identifying the risk factors and preventing the Met S in diabetic patients. Hence, identification of Met S and its factors helps to show maximum compliance to therapeutic regimen and healthy lifestyle. Moreover, the increase in public awareness and health education programs help in preventing the onset of more comorbidity that compromises the health and improvement of the quality of life of the population. [6]. The main aim of the study was to identify the occurrence of Met S and to evaluate the gender-associated difference in each component of Met S by using IDF and NCEP ATP III criteria.
Methods
A cross-sectional study was conducted in the department of general medicine K.S Hegde Charitable Hospital (a 1200 bed private tertiary care teaching hospital) located in Dakshina Kannada, Mangalore. Ethical approval was obtained from the Institutional Ethics Committee (Ref no. NGSMIPS/IEC/05/2019-20) and registered in the Clinical Trial Registry (CTRI REF/2019/08/027830) government of India before enrolling the patients. The study was conducted in accordance with the Helsinki declaration. The aim of the study was explained to all the participants and was assure about the confidentiality and freedom to participate in the study. The subjects giving consent after explaining the study were taken. The patient who met the inclusion criteria were enrolled in the study by random sampling method. Male and female patients diagnosed with type II Diabetes Mellitus. Patients age between 30 and 80 years and should be on diabetic treatment were included in the study. Type I Diabetes Mellitus patients, seriously ill patients, who were under ventilation support and in altered mental status, patients not giving consent and pregnant women were excluded from the study. Patient demographics, socioeconomic and lifestyle details, routine biochemical investigations, and comorbidities were collected from patient medical records and direct interview method. Metabolic Syndrome was assessed by IDF and NCEP ATP III guidelines.
Estimation of sample size
The sample size calculation was estimated by using the formula.
-
n = Sample Size.
-
Z1-α = Confidence Interval.
-
E = Absolute error.
-
P = Anticipated Proportion.
-
Q = Proportion of a target population with certain characteristics.
The minimum sample required for conducting this study was found to be 350.
Assessment of Metabolic Syndrome (Met S) using IDF Criteria
The subjects who meet the conditions defined by the International Diabetic Federation (IDF) to be considered as having metabolic syndrome (Met S). The condition is as follows: [7]
-
1)
Central obesity (defined as waist circumference with ethnicity-specific.
For South Asians:
-
Male ≥ 90 cm.
-
Female ≥ 80 cm).
PLUS any two of the following four factors.
2. | Raised Triglycerides | ≥ 150 mg/dL (1.7 mmol/L) Or specific treatment for this lipid abnormality |
3. | Reduced High Density Lipoproteins | < 40 mg/dL (1.03 mmol/L) in males < 50 mg/dL (1.29 mmol/L) in females Or specific treatment for this lipid abnormality |
4. | Raised Blood Pressure | Systolic BP ≥ 130 or Diastolic BP ≥ 85 mm Hg Or the treatment of previously diagnosed hypertension |
5. | Raised Fasting plasma glucose | (FPG) ≥ 100 mg/dL (5.6 mmol/L) Or previously diagnosed type II diabetes. |
Assessment of Metabolic Syndrome (Met S) using NCEP ATP III Criteria
The subjects who meet the conditions defined by NCEP ATP III Criteria to be considered as having metabolic syndrome (Met S) when three or more of the following criteria were satisfied. The condition is as follows:
1. | Raised Triglycerides | ≥ 150 mg/dL (1.7 mmol/L) Or specific treatment for this lipid abnormality |
2. | Reduced High Density Lipoproteins | HDL cholesterol < 40 mg/dL (1.0 mmol/l) in men, < 50 mg/dl (1.3 mmol/l) in women |
3. | Raised Blood Pressure | Systolic BP ≥ 130 or Diastolic BP ≥ 85 mm Hg Or known treatment for hypertension |
4. | Raised Fasting plasma glucose | fasting plasma glucose ≥ 150 mg/dL (5.6 mmol/l) |
5 | Central obesity | waist circumference > 88 cm (35 inches) women, 102 (40 inches) cm in men |
Statistical analysis
The data were tabulated and calculated using the Statistical Program for Social Science (SPSS V-21) for windows software. Continuous variables were expressed as mean ± SD. Categorical data were being expressed as a percentage and corresponding frequency. The χ2 – test helps to determine the association between categorical variables. For normally distributed variables difference between the groups were determined by an independent sample t-test. The Mann- Whitney U test can be used for nonparametric data.
Results
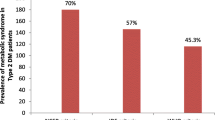
In this study, 450 patients were screened based on inclusion and exclusion criteria. A total of 350 patients (male:216, female:134) were enrolled in this study. Table 1 shows the general characteristics of study population. The mean age (± SD) of the study population was 57.76 (± 11.15) years. The mean age of the males were 57.59 (± 11.30) and females were 58.03 (± 10.930) with no significant difference. Of all type II DM patients, the 61.71% were males and 38.28% were females. The maximum numbers of patients were in the age group between 51 and 60 followed by 61–70. A total of 350 patients were analyzed for Met S 42.28% and 28.85% DM patients were found to have metabolic syndrome according to IDF and NCEP ATP III criteria respectively. A higher prevalence rate was observed with IDF criteria. Females were more affected according to two criteria. The overall prevalence of metabolic syndrome was found to be increased with age, peaking at 51–60 years of age followed by 61–70 years. The prevalence of metabolic syndrome was found to be significantly associated with age. Age-wise Prevalence of metabolic syndrome among type II DM patients is shown in Fig. 1. In this study, it was found that a higher number of patients were having DM for 1–5 years. The incidences rate of Met S more common in patients who have duration of diagnosis 1–5 years. It was found to be statistically significant (p < 0.01). Patients with metabolic syndrome had a significantly higher body weight and Body Mass Index as compared to the group without metabolic syndrome. A higher proportion of patients with Met S had increased waist circumference as compared to DM patients without Met S. It was not found to be statistically significant (83.46 ± 5.75 vs. 92.24 ± 7.35, p = 0.148)
.
In this study, we have used the IDF and NCEP ATP III guidelines for identifying Met S. Since this study population was diabetic, a higher fasting blood sugar level became an unchangeable criterion in our study cohort. Raised plasma glucose level was found in 92.85% of the study population. The most frequent metabolic components of the study subjects were higher BP (68.28%) and waist circumference (48.57%). Hypertension was present in more than half of the study subjects. The next most frequent component was lower HDL (34.85%). The least frequently occurring risk factors were found to be elevated TG levels (25.14%). Among various components of Met S were analyzed higher fasting blood sugar and waist circumference were most frequent risk factors found in DM patients with Met S. The least frequently occurring risk factors in DM patients with Met S was found to be elevated TG levels (43.91%). The Prevalence of each component of metabolic syndrome in patients with and without metabolic syndrome is shown in Table 2. The overall mean BMI value of females (25.1 ± 3.1) was found to be higher than that of males (24.94 ± 2.84). Associations of individual components of metabolic syndrome were significantly noted for female DM patients with hypertension (p < 0.001), low high-density lipoprotein (p = 0.013) and waist circumference (p = 0.006). Whereas triglyceride levels (p = 0.128) and fasting blood sugar level (p = 0.670) did not show any significant difference with gender. Association of components of metabolic syndrome with gender is shown in Fig. 2
.
Discussion
People with metabolic syndrome are at increased risk of developing macro and microvascular complications of diabetes mellitus and cardiovascular disease with an unclear mechanism. To our knowledge, this is the first study from this region to identify the prevalence of metabolic syndrome and its association with components of metabolic syndrome among type II DM patients. Risk factors that were analyzed for the significance of the relationship with Met S include age, gender, Blood pressure, WC, serum HDL, TG level blood glucose and BMI.
A higher prevalence of metabolic syndrome was observed in this population according to IDF (42.28%) and NCEP ATP III (28.85%) criteria. The highest prevalence of metabolic syndrome was observed with IDF criteria. The reason for IDF criteria is being more susceptible than NCEP ATP III for metabolic syndrome might be due to our patients were having higher body mass index and central obesity and the requirement of any two metabolic risk factors in addition to central obesity [8]. An important finding of this study according to IDF and ATP III criteria was the higher prevalence of metabolic syndrome among females (61.94% and 47.01%) compared with males (36.09% and 17.59%). The Prevalence of Met S in females was found to be twice as common as males. This result was found to be similar to the results obtained from other studies [1,2,3, 6,7,8,9,10,11,12,13]. A higher prevalence in women might be related to their higher rates of obesity and body mass index. In this study, it was found that upper body adiposity and abdominal obesity especially deposition of fats in the buttock, hip and limb areas are more common in females than males. We also found that a significant number of females with metabolic syndrome were at their post-menopausal age. These specific characteristics and lifestyle factors might be the reasons for the occurrence of metabolic syndrome in female patients [14]. The frequency of Met S more common in patients who have a duration of diagnosis 1–5 years. This might lead to more macro and microvascular complications.
The occurrence rate of Mets S was increased with age and number of comorbidities associated with DM. This study observed a significantly higher prevalence of metabolic syndrome in older people. Similar results were obtained from the study done by Xiao J et al. [15]. In this study, it was identified that a higher prevalence rate of Met S was seen in the fifth decade followed by the sixth decade. In a study done by Bhat RA et al. in Kasmir, similar results were found. In this study, it was observed that nearly 95% of patients with Met S were greater than 41 years old [16]. Yadav et al. also reported the same prevalence in Gwalior, India [17]. About three fourth of the subjects who participated in the study were overweight/obese (BMI ≥ 23 kg/m2), which is a prime determinant of Met S occurrence. Studies conducted by Sawant et al. also reported the high association between obesity and metabolic syndrome [18]. Studies have been identified that Asian Indians tend to develop central obesity rather than generalized obesity. This might be one of the main reasons for the higher occurrence of Met S among DM patients according to IDF criteria. Increased levels of triglyceride, raised BP, increased waist circumference and fasting blood glucose levels and reduction in HDL cholesterol were found to be strongly associated with Met S in diabetic patients of both genders. Higher BP and waist circumference were the strongest metabolic risk factors of Met S in this study. Similar results were found in a study done by Zafar U et al. Peterson PN et al. conducted a study reported that adverse cardiac outcomes are more common in diabetic women as compared to diabetic men [19, 20]. Our study shows that type II DM patients with Met S have been associated with higher rate of cardiometabolic risk factor especially abdominal obesity, high BMI, and hypertension. This result is consistent with a previously published report on the Indian population by Sharma KK et al. [21].
In this study, it was found that, Low HDL level more frequently seen in females than males. Studies conducted by Supriya et al., Linu Mohan et al. shared similar observations [10, 22]. This might be due to their menopausal age. Studies have been reported that lack of estrogens at menopausal age can lead to a decrease in HDL levels. In this study, it was observed that subjects with metabolic syndrome were physically inactive and were having a high body mass index. A possible explanation of effective physical activity on metabolic syndrome could be due to the reduction of systemic oxidative stress. Nitric oxides play an important role in the reduction of cardiometabolic risk factors through the dilation of blood vessels [12]. The positive effect of exercise against obesity, heart disease and metabolic syndrome has been already proven.
This study did not show a significant relationship between smoking and alcoholism with metabolic syndrome. Studies have been reported the effect of alcohol and nicotine on the incidence of metabolic syndrome. The higher incidence rate of metabolic syndrome among smokers could be due to an increase in the risk of abdominal obesity and insulin resistance [23]. The results in our study should be considered with some limitations. The sample size in our study was small. In addition, this study was a single centre hospital based study hence the result cannot be generalized. Large multicentre studies are required to confirm the results. Despite of these limitations, this study provides an important data regarding the relation between different components of metabolic syndrome in type II DM patients.
Conclusions
This study concluded that; the prevalence of Met S is higher in type II DM patients. Older age, female gender, high BMI/obesity, higher blood pressure, low HDL level, and waist circumference significantly contributed to an increased risk of metabolic syndrome among the diabetic population. Routine screening for metabolic components may be benefit for appropriate interventions and help in preventing premature morbidity and mortality. Many factors associated with metabolic syndrome are modifiable so, early intervention, particularly with a lifestyle change, would delay the onset of advanced forms of Met S and a high-risk status. Regular physical activity, lifetime abstinence of tobacco, avoidance in the consumption of trans fats (fried food), and reduced intake of saturated fats together with an increased intake of fruits and vegetables form the foundation of lifestyle changes. Adopting a healthy lifestyle beginning in childhood can reduce the incidence of complications associated with metabolic syndrome among patients with Diabetic Mellitus.
References
Khanal P, Mandar BK, Patil BM, Hullatti KK. In silico Antidiabetic Screening of Borapetoside C, Cordifolioside A and Magnoflorine. Indian J Pharm Sci. 2019; 81: 550 – 55.
Khanal P, Patil BM, Mandar BK, et al. Network pharmacology-based assessment to elucidate the molecular mechanism of anti-diabetic action of Tinospora cordifolia. Clin Phytosci. 2019;5:35.
James M, Varghese TP, Vijayan A, Anagha PP, Muhas C, Hyder M. Link between Metabolic Syndrome and Diabetes Mellitus: A Pathophysiological Implication. Int J Sci Technol Res. 2019;11:1935–40.
Rezaianzadeh A, Namayandeh SM, Sadr SM. National Cholesterol Education Program Adult Treatment Panel III Versus International Diabetic Federation Definition of Metabolic Syndrome, Which One is Associated with Diabetes Mellitus and Coronary Artery Disease? Int J Prev Med. 2012;3:552–58.
Faizal R, George L, Lakshmanan P, Varghese TP. Assesment of diabetes related quality of life and the impact of pharmaceutical care in its improvement. J Coastal Life Med. 2016: 4; 649 – 51.
Nsiah K, Shang O, Boateng KA, Mensah FO. Prevalence of metabolic syndrome in type 2 diabetes mellitus patients. Int J Appl Basic Med Res. 2015;5:133–38.
Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:3569.
Huang P. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2:231–37.
Felix Val K, Titty WK, Owiredu WK, Agyei Frimpong MT. Prevalence of metabolic syndrome and its components among diabetes patients in Ghana. J Biol Sci. 2008;8:105761.
Linu Mohan P, Jishnu NA, Remya PJ. Prevalence of metabolic syndrome in psychiatric OP patients in tertiary care hospital, Kerala. Indian J Pharm Pract. 2012;5:58–61.
Mawlieh BS, Shastry CS, Chand S. Evaluation of anti-diabetic activity of two marketed herbal formulations. Research J Pharm Tech. 2020;13:664 – 68.
Mayer-Davis EJ, et al. Intensity and amount of physicial activity in relation to insulin sensitivity: the insulin resistance atherosclerosis study. J Am Med Assoc. 1998;279:669–74.
Nsiah K, Shang VO, Boateng KA, Mensah FO. Prevalence of metabolic syndrome in type 2 diabetes mellitus patients. Int J Appl Basic Med Res. 2015;5:133–38.
White UA, Tchoukalova YD. Sex dimorphism and depot differences in adipose tissue function. Biochim Biophys Acta. 2014 Mar;1842:377–92.
Xiao J, Li Wu C, Gao YX, Wang SL, Wang L, Yun Lu Q, Wang XJ, et al. Prevalence of metabolic syndrome and its risk factors among rural adults in Nantong, China. Sci Rep. 2016;6:38089.
Bhat RA, Laway BA, Zargar AH. Prevalence of metabolic syndrome in Kashmir valley of Indian subcontinent. Indian J Med Sci. 2010;64:259–64.
Yadav D, Mahajan S, Subramanian SK, Bisen PS, Chung CH, Prasad GB. Prevalence of metabolic syndrome in type 2 diabetes mellitus using NCEP-ATPIII, IDF and WHO definition and its agreement in Gwalior Chambal region of Central India. Glob J Health Sci. 2013;17:5:142–55.
Sawant A, Mankeshwar R, Shah S, Raghavan R, Dhongde G, Raje H, et al. Prevalence of metabolic syndrome in urban India. Cholesterol. 2011;2011:920983.
Peterson PN, Spertus JA, Magid DJ, Masoudi FA, Reid K, Hamman RF, et al. The impact of diabetes on one year health status outcomes following acute coronary syndrome. BMC Cardiovasc Disord. 2006;6;41.
Zafar U, Khaliq S, Ahmad HU, Manzoor S, Lone KP. Metabolic syndrome: an update on diagnostic criteria, pathogenesis, and genetic links. Hormones (Athens). 2018;17:299–13.
Sharma KK, Mathur Mukul, Lodha S, Sharma SK, Sharma N, Gupta R. Study of differences in presentation, risk factors and management in diabetic and nondiabetic patients with acute coronary syndrome. Indian J Endocrinol Metab. 2016;20:354–58.
Supriya Simon A, Dinesh Roy D, Jayapal V, Vijayakumar T. Biochemical and genetic studies on cardiometabolic syndrome. Indian J Clin Biochem. 2010;25:164–68.
Chiolero A, Faeh D, Paccaud F, Cornuz J. Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am J Clin Nutr. 2008;87:801–09.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
James, M., Varghese, T.P., Sharma, R. et al. Association Between Metabolic Syndrome and Diabetes Mellitus According to International Diabetic Federation and National Cholesterol Education Program Adult Treatment Panel III Criteria: a Cross-sectional Study. J Diabetes Metab Disord 19, 437–443 (2020). https://doi.org/10.1007/s40200-020-00523-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-020-00523-2