Abstract
Purpose of Review
Mild traumatic brain injury (mTBI)/concussion is a significant health concern for military service members and veterans; however, these are distinct populations that warrant certain considerations related to clinical care and rehabilitation. This review elucidates these key aspects of military mTBI that differ from civilians.
Recent Findings
Several contextual variables pertaining to military culture, mechanism and frequency of mTBI in military settings, symptom attribution and over-reporting, potential secondary gain, and elevated mental health comorbidities, including posttraumatic stress disorder (PTSD), sleep disturbance, and chronic pain, are key moderating factors that often influence symptom presentation.
Summary
Characteristics of military mTBI differentially affect chronic post-concussive symptom reporting and recovery and are essential to understand to provide effective clinical management with this population. Evidence-based treatments (i.e., psychoeducation, cognitive rehabilitation, cognitive-behavioral psychotherapy) have been developed, though maximally effective mTBI diagnosis/evaluation, clinical management, recovery, and research are best facilitated by interdisciplinary collaboration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mild traumatic brain injury (mTBI), also known as concussion, is a significant health concern for civilian, active duty military, and veteran populations. The Defense and Veterans Brain Injury Center (DVBIC) estimates that annually, over 1.7 million people in the USA sustain a TBI, approximately 84% of which are mild in severity [1]. Military service members (SMs) are at greater risk for mTBI than civilians, due in part to the demographics of the US military. Most SMs are young, healthy males, representing a high risk group for TBI [1]. Additionally, several contextual aspects of military mTBI, including military culture, injury characteristics, symptom (mis)attribution, and co-occurring psychiatric disorders, frequently influence symptom reporting, clinical management, and evidence-based treatment of chronic post-concussive symptoms with this population.
Impact of Military Context
The circumstances and context of mTBI among SMs are dissimilar in several ways to those sustained by civilians [2•]. The most obvious differences are observed in deployment-related injuries involving potentially austere conditions, disruptions of sleep and dietary schedules, and threats to health from disease and environmental pollutants. Deployments to combat theaters of operation put SMs at risk for concussive blast exposures from improvised explosive devices (IEDs), suicide bombers, land mines, mortar rounds, and rocket-propelled grenades (RPGs). For those who sustain combat-related injuries, threat to life and exposure to psychological trauma represent significant contextual factors.
Although deployment/combat mTBI are notable, most recorded TBIs among SMs occur in non-deployed environments [1]. Military-specific activities such as participation in boxing and mandatory combative training put SMs at risk for concussion and repeated sub-concussive blows. Similar to civilians, SMs also sustain mTBI while participating in sports, driving motor vehicles, and in falls. Many SMs with a history of mTBI who transition out of the military receive subsequent healthcare in the Veterans Health Administration (VHA). As veterans age, the risk for TBI again increases at age 70+, primarily from falls [1].
Due to the lack of an objective biomarker or test confirming mTBI, diagnosis is necessarily based on patient report. Department of Defense (DoD) diagnostic criteria for mTBI require normal structural brain imaging, loss of consciousness less than 30 min, alteration of consciousness less than 24 h, posttraumatic amnesia (PTA) less than 24 h, and highest Glasgow Coma Scale (GCS) score within 24 h of injury of 13–15. According to DoD convention, the terms mTBI and concussion are diagnostically equivalent. It is difficult to verify mTBI among cases in which there is not a documented loss or notable alteration of consciousness from witness or acute medical records. This was frequently the case with mTBI among SMs injured during Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) prior the establishment of DoD policy and algorithms for concussion management in deployed settings [3, 4].
Symptoms following mTBI can be classified broadly into three categories: physical, emotional, and cognitive. Physical symptoms include headaches, sleep disturbance, dizziness/balance problems, nausea, fatigue, vision changes/light sensitivity, and tinnitus. Emotional changes involve irritability, anxiety, depression, and mood swings. Cognitive symptoms include trouble concentrating, attention problems, poor memory, slowed thinking, and word finding difficulty when speaking. The normal recovery trajectory for a single mTBI is back to full function within days to weeks, although contextual factors can lead to longer recovery time. A persistent constellation of symptoms following mTBI, known as post-concussion syndrome (PCS), may arise from the neural injury and become increasingly influenced by other ongoing psychological, social, and environmental factors as time goes on. Current VA/DoD Clinical Practice Guidelines for mTBI [5•] emphasize early identification and repeated symptom assessment in the primary care setting. Psychoeducation and gradual return to activity are key concepts in treatment.
Unique Aspects of TBI in the Military
While commonalities exist between civilian and military TBI, several distinct aspects within the military context are noteworthy as they influence TBI symptom reporting, recovery, and clinical care/rehabilitation with this population.
Mechanism of Injury
Historically, TBIs accounted for approximately 20% of combat-related injuries [6]. Whereas twentieth century wars saw more penetrating TBIs, advances in helmet technology contributed to a shift toward closed head injuries in the recent OEF/OIF wars, particularly blast-related injuries. Estimates of blast-related TBI during deployment range from 14 to 60% [6, 7•]. Primary blast trauma to the brain results when mechanical, thermal, and electromagnetic energy emanating from the explosion is transferred into compressed pressure waves that can pass through tissues within the cranium at rapid speed. The wave induces particle motion through tissues it passes through. Tissues with varying density (e.g., air-fluid or fluid-solid interfaces such as those in the ear region) are particularly vulnerable to blast injury [8]. Blast waves can also reflect off objects (e.g., walls in enclosed spaces) to produce complex wave fields. It is unknown exactly how rapid pressure gradients injure brain tissue, but blast within the context of combat also may be accompanied by secondary, tertiary, and quaternary effects. Secondary injury refers to objects and debris thrown by the explosion hitting the head and causing penetrating or blunt trauma. Energy given off by the blast can also propel SMs into hard surfaces (tertiary injury). Quaternary injuries include other blast effects such as burns or toxic fumes that can cause injury. Because mechanism of injury in primary blast trauma is different from blunt trauma, there have been efforts to examine whether blast-related TBI has different sequelae that require a different pathway of care. A systematic review showed that there is no dramatic difference due to injury mechanism in terms of vision loss, vestibular dysfunction, functional status, depression, sleep disorder, and alcohol misuse, but there are mixed findings with respect to headaches, neurocognitive outcomes, hearing loss, and presence of posttraumatic stress disorder (PTSD) symptoms [9•, 10,11,12,13,14,15]. There is mixed evidence of subtle white matter changes following blast using diffusion tensor imaging [16•, 17,18,19,20]. Since primary blast injury within the context of combat is almost always accompanied by psychological and/or blunt trauma, injury characteristics (e.g., distance from blast) are often based on self-report that may have questionable veracity because of the intense psychological stress during the time of the injury. Thus, it is difficult to control for injury and psychological variables that likely moderate outcome. Studies of blast exposure unaccompanied by psychological and blunt trauma, such as those experienced during blast-intensive weapons training, may elucidate if blast indeed conveys a different course of outcome compared to blunt mTBI.
Frequency of Injury (Single vs. Multiple)
Effects of repetitive mTBI are not well understood in the military. While many studies among SMs or veterans index deployment or combat related mTBIs, training for combat can also increase risk for mTBI. Military values of self-sacrifice and “warrior ethos” can lead to SMs not reporting or underreporting potential events, especially before the 2007 DoD mandatory concussion screening [21•]. Most of what is known about cumulative effects of TBI comes from civilian athletes. With respect to cognitive functioning, meta-analysis found that multiple mTBIs were associated with poorer performance on executive function and delayed memory, though the overall effect of multiple TBIs was minimal [22]. Miller and colleagues [23] evaluated symptom endorsement in soldiers during peacetime, before OEF/OIF/OND conflicts, and found increased symptom reporting among those with a recent mTBI (within 3 months) who have had a previous history of TBI compared to those with no prior TBI. This latter group did not differ from no-TBI controls in the number of reported symptoms. In contrast, previous TBI history did not affect symptom reporting when the index TBI occurred greater than 3 months prior. This pattern is consistent with a study that showed slower recovery among college football players with history of multiple concussions relative to a single concussion [24]. In contrast, several other studies did not find adverse cognitive performance or slowed recovery in those with multiple TBIs [25,26,27]. Mixed findings are likely influenced by important moderating variables such as time since injury, time between mTBIs, and injury characteristics such as whether blast exposure was in enclosed space. The current military guideline for acute treatment of recurrent TBI within a 12-month period is seven consecutive days of symptom resolution while on stages 1 (rest) and 2 (light routine activity) before completing the remainder of the progressive return to duty stages to minimize potential cumulative effects of multiple mTBIs [28].
Sensory and Vestibular Symptoms
In military/veteran populations, commonly reported symptoms after mTBI include sensory and vestibular symptoms, such as headaches, dizziness, balance difficulties, and noise sensitivity [29]. The current treatment paradigms for the medical management of persistent PCS symptoms are similar for both civilian and military populations [30, 31] and follow a symptom-based treatment approach. For example, management for persistent vestibular dysfunction (balance/dizziness) should begin with a comprehensive history and neurological examination with emphasis on hearing, balance, coordination, and vision. Once the etiology of the vestibular dysfunction is confirmed, then the treatment plan should ensue. For instance, the most common cause of post-traumatic peripheral vestibular dysfunction is benign paroxysmal positional vertigo, which should be diagnosed using the Dix-Hallpike maneuver, and if positive, treated with canalith repositioning therapy or a trial of vestibular rehabilitation [32]. It is important to remember that the mainstay of treatment of mTBI is education and reassurance of expected recovery trajectories [33].
Symptom Attribution, Over-Reporting, and Disability Status
Since historical mTBI diagnosis is frequently dependent on self-report, the potential for misrepresentation and misattribution of symptoms and problems exist. There often is no medical documentation at the time of the injury because of a lack of medical resources, SM’s prioritization of mission over self-care, or an ingrained military ethos of mission forwardness and self-sacrifice. One study examining the consistency of reporting mTBI in theater and post-deployment reported that 86% of soldiers were consistent in their reports of exposure to mTBI [34]. However, of those who were inconsistent, the vast majority (i.e., 90%) denied TBI in theater and affirmed TBI 1 year later. While SMs and veterans may underreport symptoms in order to return to full duty, to project an impression of strength, or to avoid stigma, this section will focus on over-reporting of symptoms/problems.
An important context is disability evaluation via the Integrated Disability Evaluation System, a multistep process that includes a Medical Evaluation Board (MEB) that involves clinical providers and a Physical Evaluation Board (PEB) that is an administrative review (https://health.mil/Military-Health-Topics/Conditions-and-Treatments/Physical-Disability/Disability-Evaluation/Medical-Evaluation). The commanding officer or treating physician requests the MEB; the SM does not self-refer, though the SM can influence treating clinician’s decision via their complaints and response to treatment. PEB review can result in return to duty, separation from the military with severance pay, temporary disability retirement, or permanent disability retirement. The amount of severance or retirement pay depends on the percentage of disability, and this determination carries into the Veterans Affairs (VA) benefits system. Veterans who make a claim for service-connected disability after separation from the military go through the VA’s Compensation & Pension Exam (https://www.benefits.va.gov/COMPENSATION/index.asp). Since clinical evaluation results can influence monetary benefits, the potential for secondary gain exists. Another context is decreased physical and psychological health post-deployment [34], which combined with media coverage of chronic traumatic encephalopathy, may contribute to a damaged sense of self that the SM attributes to TBI. In these instances, SMs may report symptoms or problems perceived to be related to mTBI without misrepresenting their true belief.
The clinical challenge is separating misrepresentations associated with secondary gain from misattributions of problem sources while maintaining an open mind that there may be biological consequences of mTBI that remain unknown. Efforts to evaluate symptom validity have led to development of screening scales such as the Mild Brain Injury Atypical Symptoms Scale (mBIAS) [35] and the Validity-10 scale of the Neurobehavioral Symptom Inventory (NSI) [36•], which is a DoD/VA core TBI outcome measure. The Validity-10 is composed of 10 symptoms that are infrequently seen in mTBI and reflect negative impression management, as validated against objective personality inventories (i.e., Personality Assessment Inventory [37, 38]; Minnesota Multiphasic Personality Inventory-2-Restructured Form [39, 40]). Cutoffs for symptom exaggeration vary across studies, but there is a general consensus that a higher cutoff is needed for screening for over-reporting in military/veteran populations [37, 38, 40, 41] compared to civilians [42, 43], and a higher cutoff is needed for screening those who have deployed versus those who have not as deployment history is associated with higher NSI scores irrespective of TBI history [44•]. Further, NSI scores are higher in clinical settings compared to research settings [45]. It is also critical to clarify that symptom validity tests (SVTs) on self-report measures, which assess for over- and underreporting, are different from and only partially overlap with performance validity tests (PVTs), which assess the credibility of one’s performance on objective tests of cognitive functioning [46, 47]. Invalid symptom over-reporting may not necessarily result in invalid performance on cognitive measures or vice versa; thus, both symptom and performance validity should be separately evaluated. In addition to symptom over-reporting, disability evaluations are also associated with diminished performance validity on objective PVTs [46, 48], which can limit a clinician’s ability to identify whether low cognitive test scores are due to actual neurocognitive impairment or are reflective of reduced task engagement/validity. Performance validity remains an important consideration even outside the context of disability given that 11–35% of active duty/veterans with mTBI who were not involved in disability evaluations fail at least one PVT [46, 47]. One study found abnormal metabolites in the hippocampus of veterans with blast exposure using an experimental 7 T magnet [49], while another found increased white matter burden among veterans with mTBI who failed at least one PVT [50•]. It is unknown whether psychological variables contributed to these findings, or whether blast mTBI may be associated with subtle biological changes that are not yet measurable using current neuropsychological and clinical imaging technology. In the face of these unknowns, each patient should be considered on a case-by-case basis while taking into account the degree to which his/her military experience and ingrained ethos may influence their clinical presentation.
Mental Health Comorbidities
The high comorbidity of mental health conditions among SMs/veterans relative to civilians is another important consideration. Notably, upwards of 89% veterans with TBI history receiving VA services were also diagnosed with a comorbid mental health condition [51]. Regarding specific conditions, PTSD is frequently present with overall prevalence of 23% and rates as high as 44–54% among those with mTBI history [51, 52•, 53]. Other relevant rates include 12–21% for depression [54, 55], 12% for generalized anxiety in isolation and 40% among those with PTSD [56], and 38% for comorbid insomnia and obstructive sleep apnea [57]. Moreover, among those with a psychiatric diagnosis, 24% also had concurrent substance abuse [58]. Finally, pain diagnoses are highly comorbid with approximately half of veterans with TBI being diagnosed with both PTSD and pain. This triad of persisting PCS symptoms, PTSD, and chronic pain is a commonly observed clinical phenomenon and is associated with both higher healthcare expenditure as well as specific clinical practice recommendations, such as providing education to patients/family and providers (e.g., clarifying difference between a history of concussion and current PCS endorsement) and developing interdisciplinary treatment plans that integrate input from all specialty providers to promote more collaborative care [51, 59, 60, 61•].
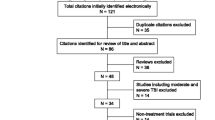
Mental health comorbidities further complicate TBI clinical care and recovery insomuch as PCS symptoms are nonspecific and mirror symptoms of many major psychiatric conditions. For example, concentration difficulties, sleep disturbance, fatigue, and irritability appear in the diagnostic criteria for PCS [62] as well as for PTSD and Depression [63]. Further, veterans with psychiatric conditions, notably PTSD, depression, generalized anxiety, and somatization disorders, all met diagnostic criteria for PCS at higher rates than those with actual mTBI history [64]. Similarly, per Fig. 1 below, military personnel with PTSD, but no mTBI history, endorsed significantly higher PCS symptoms relative to those with a history of mTBI, but no psychiatric comorbidity as well as non-deployed and deployed controls [44•]. Yet, despite elevated symptom reporting/cognitive complaints, a recent longitudinal study found veterans with mTBI generally performed within normal limits on objective neuropsychological tests, again highlighting that subjective cognitive complaints do not necessarily indicate objective deficits [65]. Nonetheless, symptom over-reporting is an important consideration as it can adversely affect the validity of clinical evaluation and should be assessed via objective measures of response bias [66•].
Graph shows mean scores on the four Neurobehavioral Symptom Inventory (NSI)-20 subscales, V = vestibular; S = somatic; C = cognitive; A = affective, for non-deployed-nonclinical (n = 1453), deployed-nonclinical (n = 1064), deployed-mTBI (n = 108), and deployed-PTSD (n = 52) subgroups. Subscale averages are displayed because of differences in number of items on each subscale. Higher scores indicate greater postconcussion symptom endorsement 44. Reprinted with permission from Taylor & Francis Ltd., www.tandfonline.com
Meta-analytic studies have consistently demonstrated that while acute mTBI sequelae may be present, symptoms quickly resolve over the ensuing days to weeks with nonsignificant objective cognitive effects generally found after 1–3 months, suggesting that ongoing symptom endorsement is unrelated to the mTBI itself [67,68,69]. Rather, litigation/compensation seeking status and psychiatric comorbidities, notably PTSD, can be predictive of chronic PCS symptom endorsement above demographics, time since injury, or TBI mechanism [70,71,72,73]. From a treatment perspective, this is promising given efficacious, evidence-based treatments for PTSD and other mental health conditions have been developed (see below). Unfortunately, misconceptions about mTBI recovery among both military personnel and behavioral health providers, as well as stigma associated with mental illness, often result in symptom misattribution and underutilization of appropriate mental health services in the military [74, 75, 76•].
Evidence-Based Treatments for MTBI
Several treatment approaches have been examined for PCS symptoms following mTBI including psychoeducation, cognitive rehabilitation (CR), and psychotherapeutic approaches. Several recent reviews have summarized the evidence in support of such interventions in both civilian [77,78,79] and military/veteran [80•] populations. These systematic reviews have concluded that brief psychoeducational interventions are supported in the acute phase of recovery. Further, these reviews have found limited evidence in support of CR and psychotherapeutic approaches among individuals with chronic symptoms, particularly in military and veteran populations. The empirical evidence underlying their conclusions is described in this section.
Psychoeducational Interventions for PCS
A brief psychoeducational intervention in the acute post-injury period can reduce both the severity and duration of PCS symptoms [78, 81]. Mittenberg et al. [81] demonstrated that providing educational information and meeting with a healthcare provider for 1 h prior to discharge from an emergency room after sustaining a concussion resulted in fewer symptoms and shorter symptom duration at 6-month follow-up compared to a matched control group who received standard care. This brief psychoeducational approach has been replicated in several additional RCTs, including studies with modifications to the delivery of psychoeducational information to include group sessions and handouts [79, 82, 83]. However, an expanded intervention did not demonstrate additional benefit [84, 85]. While using psychoeducational interventions in the acute phase of recovery is considered a standard of care [5•], it has not been shown to be effective among individuals with chronic PCS symptoms. A pilot study of a computer-based psychoeducational intervention specifically adapted for veterans with chronic PCS showed potential [86], although a subsequent randomized replication/extension trial failed to demonstrate effectiveness [87]. In summary, there is empirical support in the early/acute phase of recovery for providing patients with positive expectations of recovery, an explanation of common symptoms after mTBI, and basic strategies for managing symptoms, but research has not shown this intervention to be effective in reducing symptom reporting beyond the acute phase of recovery.
Cognitive Rehabilitation
Cognitive symptoms are frequently reported in chronic PCS, particularly in military/veteran populations [88]. CR interventions have considerable support in the acute and sub-acute phase of recovery from severe TBI [89,90,91], and several recent studies have examined the efficacy of CR in those with chronic PCS. It is important to note that there are several significant differences between CR interventions among individuals with mTBI and individuals with moderate-severe TBI. Most importantly, since meta-analytic studies have shown little evidence of impairment on neuropsychological measures beyond the acute phase in mTBI [67, 68, 92], CR interventions for PCS typically focus on compensating for subjective, functional cognitive complaints [93, 94], rather than restorative techniques targeting objective cognitive impairments. While a few small studies have demonstrated that the restorative techniques may improve neuropsychological abilities among individuals after mTBI, such studies were limited by small sample sizes [95] and/or potential sampling biases, including performance validity concerns in the subjects described in the treatment sample [96], thereby limiting the strength of the conclusions that can be drawn about the effectiveness of restorative techniques in this population.
Several recent studies have examined compensatory CR approaches in SMs/veterans [97, 98, 99•]. Compensatory techniques involve teaching individuals to cope with cognitive difficulties through training on adaptive functional skills or training in the use of external aids such as smart phone applications and other cognitive mnemonics. CogSMART [98], one of the most widely implemented CR interventions, includes both didactics and compensatory strategy training, organized in cognitive modules, that have been adapted for both individual and group interventions. In their initial RCT, reductions in PCS and improved prospective memory were demonstrated [98], with continued reduction in PCS at 1-year follow-up [100]. Adaptations of the CogSmart CR intervention has been replicated in two additional independent samples [97, 99•] and utilized in combined approaches using both CR and psychotherapy [101,102,103].
The most recent and largest CR trial to date, the SCORE clinical trial [104•], compared four, 6-week treatment arms: (1) psychoeducation, (2) independent self-administered computer-based CR, (3) therapist-directed manualized CR, and (4) therapist-directed CR integrated with cognitive behavioral therapy (CBT) psychotherapy. Treatment arms that included therapist-directed CR had superior outcomes compared to treatment arms without therapist-directed rehabilitation—on a self-report measure of day-to-day cognitive functioning. The addition of CBT to CR was associated with improved psychological outcomes compared to a treatment arm that only received psychoeducational intervention and medical treatment, but was not significantly better than the therapist-directed CR without CBT. No treatment gains were found on an objective neuropsychological measure of working memory and sustained attention. A detailed guide to CR interventions for chronic PCS in military SMs/veterans is available [105]: http://www.asha.org/uploadedFiles/ASHA/Practice_Portal/Clinical_Topics/Traumatic_Brain_Injury_in_Adults/Clinicians-Guide-to-Cognitive-Rehabilitation-in-Mild-Traumatic-Brain-Injury.pdf.
Psychotherapeutic Approaches
`Given the high comorbidity of psychological conditions (e.g., PTSD; depression) after mTBI, especially in military SMs/veterans [44•], psychotherapeutic approaches have also been examined. In a recent civilian RCT, Potter et al. [106•] used CBT to treat chronic PCS. CBT was focused on individually identified target problems, not any specific underlying psychological condition or problem. They found improvement on a quality of life measure, but not on PCS, global psychosocial functioning, anxiety, or depression. In part due to the potential interactive effect between PTSD and PCS symptom reporting [107], several studies have focused on providing evidence-based PTSD treatment among individuals with both mTBI and PTSD, including both prolonged exposure (PE) and cognitive processing therapy (CPT) [108]. In several independent studies [109,110,111, 112•], PE is effective not only in reducing PTSD symptoms, but has a generalized effect in reducing PCS and enhancing outcomes for individuals with chronic PCS [113].
Finally, a series of related studies examined treatment outcomes for veterans who were dually diagnosed with mTBI and PTSD using a combined approach of compensatory CR interventions and CPT [101,102,103], provided during the course of a 7-week intensive residential treatment program. In addition to reduced PTSD symptoms [101], treatment completers showed statistically significant reductions in PCS symptoms [103] with combined treatment, even in those subjects with comorbid depression [102]. Although limited by a pre-post design, these studies are consistent with findings in the combined treatment arm of the SCORE clinical trial104 and a prior RCT in a civilian sample [114], indicating support for the use of combined CR and psychotherapeutic approaches in military SMs/veterans with chronic PCS.
Conclusion
Mild TBI/concussion symptom reporting and recovery trajectories among military SMs/veterans are unique and warrant certain considerations when providing TBI clinical care to these populations. While several moderating factors initially believed to heavily influence mTBI outcomes (e.g., mechanism of injury; single vs. multiple concussions) generally known to exert smaller effects in subsequent research, other discrete contextual aspects (military culture, symptom misattribution, mental health comorbidities, disability status) significantly influence symptom reporting and outcomes. Further, given this heterogeneous population and multifactorial presentation of persistent PCS symptoms, it is important to have well-trained interdisciplinary team to provide the full spectrum of treatment options for optimal management. Currently, there are no urine, serum, blood, or cerebrospinal fluid, or neuroimaging biomarkers that can accurately detect concussion or the extent of damage after mTBI [115•]. Future research should focus on translational research, advanced neuroimaging, genetic studies, and neuroprosthetics (e.g., repetitive transmagnetic stimulation [rTMS]; transcranial direct current stimulation [tDCS]) to gain a better understanding of diagnosis, evaluation, recovery, and treatment after mTBI [116].
References
Paper of Particular Interest, Published Recently, Have Been Highlighted as: • of Importance
Defense and Veterans Brain Injury Center. DoD Worldwide Numbers for TBI. Available at: http://dvbic.dcoe.mil/dod-worldwide-numbers-tbi. Accessed 6 Oct 2017.
• Armistead-Jehle P, Soble JR, Cooper DB, Belanger HG. Unique aspects of traumatic brain injury in military and veteran populations. Phys Med Rehabil Clin N Am. 2017;28(2):323–37. This paper describes factors unique to military and Veteran populations with traumatic brain injury, including the epidemiology of TBI in the military/Veteran population, the influence of military culture on this condition, and identification and treatment of mTBI in the war zone.
Department of Defense Memorandum 09-033. 2010. Available at http://www.esd.whs.mil/Portals/54/Documents/FOID/Reading%20Room/Other/11-F-0369_DTM_09-033_Policy_Guidance_for_Management_of_Concussion_Mild_Traumatic_Brain_Injury_In_The_Deployed_Setting.pdf. Accessed 9 Oct 2017.
Department of Defense Instruction 6490.11. 2012. Available at: http://www.usaisr. amedd.army.mil/cpgs/DODI_6490.11_Policy_Guidance_for_Mgmt_of_Mild_Traumatic_Brain_Injury_or_Concussion_in_the_Deployed_Setting.pdf. Accessed 9 Oct 2017.
• VA/DoD Clinical Practice Guideline for the Management of Concussion-mild Traumatic Brain Injury. Version 2.0, 2016. These practice guidelines were developed jointly by the VA and DoD for clinicians who treat patients with mild TBI/concussion in military and Veteran settings. Available at: https://www.healthquality.va.gov/guidelines/Rehab/mtbi/mTBICPGFullCPG50821816.pdf. Accessed 24 Oct 2017.
Ling G, Bandak F, Armonda R, Grant G, Ecklund J. Explosive blast neurotrauma. J Neurotrauma. 2009;26(6):815–25.
• Swanson TM, Isaacson BM, Cyborski CM, French LM, Tsao JW, Pasquina PF. Traumatic brain injury incidence, clinical overview, and policies in the US military health system since 2000. Public Health Rep. 2017;132(2):251–9. This report summarizes statistics on the incidence and recent policy on TBI in the US military health system.
Depalma RG, Burris DG, Champion HR, Hodgson MJ. Blast injuries. N Engl J Med. 2005;352(13):1335–42.
• Greer N, Sayer N, Koeller E, Velasquez T, Wilt TJ. Outcomes associated with blast versus nonblast-related traumatic brain injury in us military service members and veterans: a systematic review. J Head Trauma Rehabil. 2017. The authors report results of a systematic review of 31 studies on comparative clinical and functional outcomes following blast-related versus nonblast-related traumatic brain injury (TBI) among US service members and Veterans. Most clinical and functional outcomes appeared comparable regardless of blast exposure. However, inconsistent findings and limited outcomes reporting indicate that more research is needed. https://doi.org/10.1097/HTR.0000000000000304
Belanger HG, Proctor-weber Z, Kretzmer T, Kim M, French LM, Vanderploeg RD. Symptom complaints following reports of blast versus non-blast mild TBI: does mechanism of injury matter? Clin Neuropsychol. 2011;25(5):702–15.
Pogoda TK, Hendricks AM, Iverson KM, Stolzmann KL, Krengel MH, Baker E, et al. Multisensory impairment reported by veterans with and without mild traumatic brain injury history. J Rehabil Res Dev. 2012;49(7):971–84.
Mac Donald CL, Johnson AM, Wierzechowski L, Kassner E, Stewart T, Nelson EC, et al. Prospectively assessed clinical outcomes in concussive blast vs nonblast traumatic brain injury among evacuated US military personnel. JAMA Neurol. 2014;71(8):994–1002.
Kennedy JE, Leal FO, Lewis JD, Cullen MA, Amador RR. Posttraumatic stress symptoms in OIF/OEF service members with blast-related and non-blast-related mild TBI. Neuro Rehabilitation. 2010;26(3):223–31.
Cooper DB, Chau PM, Armistead-Jehle P, Vanderploeg RD, Bowles AO. Relationship between mechanism of injury and neurocognitive functioning in OEF/OIF service members with mild traumatic brain injuries. Mil Med. 2012;177(10):1157–60.
Reid MW, Miller KJ, Lange RT, Cooper DB, Tate DF, Bailie J, et al. A multisite study of the relationships between blast exposures and symptom reporting in a post-deployment active duty military population with mild traumatic brain injury. J Neurotrauma. 2014;31(23):1899–906.
• Mac Donald CL, Barber J, Andre J, Evans N, Panks C, Sun S, et al. 5-year imaging sequelae of concussive blast injury and relation to early clinical outcome. Neuroimage Clin. 2017;14:371–8. Using an approach flexible to the heterogeneity of brain injury at the single-subject level, 74% of a concussive blast TBI cohort (n=50) had reductions in fractional anisotropy indicative of chronic brain injury at 5 year follow-up. Brain injury diagnosis, older age, verbal memory and verbal fluency best predicted the presence of DTI abnormalities 5 years post injury with an AUC of 0.78 indicating good prediction strength.
Levin HS, Wilde E, Troyanskaya M, Petersen NJ, Scheibel R, Newsome M, et al. Diffusion tensor imaging of mild to moderate blast-related traumatic brain injury and its sequelae. J Neurotrauma. 2010;27(4):683–94.
Mac Donald CL, Johnson AM, Cooper D, Nelson EC, Werner NJ, Shimony JS, et al. Detection of blast-related traumatic brain injury in U.S. military personnel. N Engl J Med. 2011;364(22):2091–100.
Davenport ND, Lim KO, Armstrong MT, Sponheim SR. Diffuse and spatially variable white matter disruptions are associated with blast-related mild traumatic brain injury. NeuroImage. 2012;59(3):2017–24.
Taber KH, Hurley RA, Haswell CC, Rowland JA, Hurt SD, Lamar CD, et al. White matter compromise in veterans exposed to primary blast forces. J Head Trauma Rehabil. 2015;30(1):E15–25.
• Helmick KM, Spells CA, Malik SZ, Davies CA, Marion DW, Hinds SR. Traumatic brain injury in the US military: epidemiology and key clinical and research programs. Brain Imaging Behav. 2015;9(3):358–66.This review summarizes current epidemiologic data for TBI in the Military, and describes contemporary Military procedures and strategies for TBI prevention, identification, evaluation, and acute and chronic care. Key TBI clinical research priorities and programs are described, and innovative organizational plans to address future TBI needs are summarized.
Belanger HG, Spiegel E, Vanderploeg RD. Neuropsychological performance following a history of multiple self-reported concussions: a meta-analysis. J Int Neuropsychol Soc. 2010;16(2):262–7.
Miller KJ, Ivins BJ, Schwab KA. Self-reported mild TBI and postconcussive symptoms in a peacetime active duty military population: effect of multiple TBI history versus single mild TBI. J Head Trauma Rehabil. 2013;28(1):31–8.
Guskiewicz KM, Mccrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA concussion study. JAMA. 2003;290(19):2549–55.
Iverson G. Predicting slow recovery from sport-related concussion: the new simple-complex distinction. Clin J Sport Med. 2007;17(1):31–7.
Iverson GL, Brooks BL, Lovell MR, Collins MW. No cumulative effects for one or two previous concussions. Br J Sports Med. 2006;40(1):72–5.
Macciocchi SN, Barth JT, Littlefield L, Cantu RC. Multiple concussions and neuropsychological functioning in collegiate football players. J Athl Train. 2001;36(3):303–6.
Defense and Veterans Brain Injury Center. Progressive return to activity following acute concussion/mild traumatic brain injury: Guidance for the primary care manager in deployed and non-deployed settings. Availabe at: https://dvbic.dcoe.mil/material/progressive-return-activity-following-acute-concussionmild-tbi-guidance-primary-care. Accessed 24 Oct 2017.
Ryan LM, Warden DL. Post concussion syndrome. Int Rev Psychiatry. 2003;15(4):310–6.
Nash WP, Watson PJ. Review of VA/DOD clinical practice guideline on management of acute stress and interventions to prevent posttraumatic stress disorder. J Rehabil Res Dev. 2012;49(5):637–48.
Marshall S, Bayley M, Mccullagh S, et al. Updated clinical practice guidelines for concussion/mild traumatic brain injury and persistent symptoms. Brain Inj. 2015;29(6):688–700.
Akin FW, Murnane OD, Hall CD, Riska KM. Vestibular consequences of mild traumatic brain injury and blast exposure: a review. Brain Inj. 2017;31(9):1188–94.
Tapia RN, Eapen BC. Rehabilitation of persistent symptoms after concussion. Phys Med Rehabil Clin N Am. 2017;28(2):287–99.
Nelson NW, Anderson CR, Thuras P, Kehle-Forbes SM, Arbisi PA, Erbes CR, et al. Factors associated with inconsistency in self-reported mild traumatic brain injury over time among military personnel in Iraq. Br J Psychiatry. 2015;206(3):237–44.
Cooper DB, Nelson L, Armistead-jehle P, Bowles AO. Utility of the mild brain injury atypical symptoms scale as a screening measure for symptom over-reporting in operation enduring freedom/operation iraqi freedom service members with post-concussive complaints. Arch Clin Neuropsychol. 2011;26(8):718–27.
• Vanderploeg RD, Cooper DB, Belanger HG, Donnell AJ, Kennedy JE, Hopewell CA, et al. Screening for postdeployment conditions: development and cross-validation of an embedded validity scale in the neurobehavioral symptom inventory. J Head Trauma Rehabil. 2014;29(1):1–10. This study developed embedded NSI validity scales to facilitate the detection of invalid response styles. The NSI Validity-10 scale appears to hold considerable promise for validity assessment when the NSI is used as a population-screening tool.
Dretsch MN, Williams K, Staver T, Grammer G, Bleiberg J, DeGraba T, et al. Evaluating the clinical utility of the Validity-10 for detecting amplified symptom reporting for patients with mild traumatic brain injury and comorbid psychological health conditions. Appl Neuropsychol Adult. 2017;24(4):376–80.
Lange RT, Brickell TA, Lippa SM, French LM. Clinical utility of the neurobehavioral symptom inventory validity scales to screen for symptom exaggeration following traumatic brain injury. J Clin Exp Neuropsychol. 2015;37(8):853–62.
Armistead-Jehle P, Cooper DB, Grills CE, et al. Clinical utility of the mBIAS and NSI validity-10 to detect symptom over-reporting following mild TBI: A multicenter investigation with military service members. J Clin Exp Neuropsychol. 2017;1–11.
Lange RT, Brickell TA, French LM. Examination of the mild brain injury atypical symptom scale and the Validity-10 scale to detect symptom exaggeration in US military service members. J Clin Exp Neuropsychol. 2015;37(3):325–37.
Lippa SM, Axelrod BN, Lange RT. The mild brain injury atypical symptoms (mBIAS) scale in a mixed clinical sample. J Clin Exp Neuropsychol. 2016;38(7):721–9.
Lange RT, Edmed SL, Sullivan KA, French LM, Cooper DB. Utility of the mild brain injury atypical symptoms scale to detect symptom exaggeration: an analogue simulation study. J Clin Exp Neuropsychol. 2013;35(2):192–209.
Sullivan KA, Lange RT, Edmed SL. Utility of the neurobehavioral symptom inventory Validity-10 index to detect symptom exaggeration: an analogue simulation study. Appl Neuropsychol Adult. 2016;23(5):353–62.
• Soble JR, Silva MA, Vanderploeg RD, Curtiss G, Belanger HG, Donnell AJ, et al. Normative data for the neurobehavioral symptom inventory (NSI) and post-concussion symptom profiles among TBI, PTSD, and nonclinical samples. Clin Neuropsychol. 2014;28(4):614–32. This study established NSI normative data using the four NSI factors (i.e., vestibular, somatic, cognitive, and affective) identified by Vanderploeg, Silva, et al. (2014). A deployed-nonclinical group endorsed greater PCS symptom severity than a non-deployed group, and the mTBI group endorsed more symptoms than both nonclinical groups. However, a PTSD group endorsed higher symptom severity than the other three groups.
Jackson CE, Nordstrom L, Fonda JR, Fortier CB, Milberg WP, Mcglinchey RE. Reporting of symptoms associated with concussion by OEF/OIF/OND veterans: comparison between research and clinical contexts. Brain Inj. 2017;31(4):485–92.
Armistead-Jehle P, Buican B. Evaluation context and symptom validity test performances in a U.S. military sample. Arch Clin Neuropsychol. 2012;27(8):828–39. https://doi.org/10.1093/arclin/acs086.
Lange RT, Pancholi S, Bhagwat A, Anderson-barnes V, French LM. Influence of poor effort on neuropsychological test performance in U.S. military personnel following mild traumatic brain injury. J Clin Exp Neuropsychol. 2012;34(5):453–66.
Nelson NW, Hoelzle JB, McGuire KA, Ferrier-Auerbach AG, Charlesworth MJ, Sponheim SR. Evaluation context impacts neuropsychological performance of OEF/OIF veterans with reported combat-related concussion. Arch Clin Neuropsychol. 2010;25(8):713–23. https://doi.org/10.1093/arclin/acq075.
Hetherington HP, Hamid H, Kulas J, Ling G, Bandak F, de Lanerolle NC, et al. MRSI of the medial temporal lobe at 7 T in explosive blast mild traumatic brain injury. Magn Reson Med. 2014;71(4):1358–67.
• Clark AL, Sorg SF, Schiehser DM, Bigler ED, Bondi MW, Jacobson MW, et al. White matter associations with performance validity testing in veterans with mild traumatic brain injury: the utility of biomarkers in complicated assessment. J Head Trauma Rehabil. 2016;31(5):346–59. White matter (WM) integrity and cognition were evaluated in Veterans with history of mTBI who passed PVTs (n = 43), history of mTBI who failed at least 1 PVT (n = 13), and military controls (n = 23) with no history of TBI. The TBI-failed group demonstrated significantly lower cognitive scores and more overall WM abnormalities than the other groups. More abnormalities were found in the anterior internal capsule and cingulum of both TBI subgroups relative to MCs. The TBI-failed group demonstrated significantly decreased WM integrity in the corpus callosum compared to the TBI-passed group.
Taylor BC, Hagel EM, Carlson KF, Cifu DX, Cutting A, Bidelspach DE, et al. Prevalence and costs of co-occurring traumatic brain injury with and without psychiatric disturbance and pain among Afghanistan and Iraq war veteran V.A. Users. Med Care. 2012;50(4):342–6.
• Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, et al. The prevalence of posttraumatic stress disorder in operation enduring freedom/operation Iraqi freedom (OEF/OIF) veterans: a meta-analysis. J Anxiety Disord. 2015;31:98–107. This meta-analysis examined 33 studies published between 2007 and 2013 involving 4,945,897 OEF/OIF veterans. PTSD prevalence was estimated at 23%. Publication year and percentage of Caucasian participants and formerly active duty participants explained significant variability in prevalence across studies. Most studies estimate prevalence among OEF/OIF veterans using VA medical chart review. Additional research is needed with randomly selected, representative samples administered diagnostic interviews.
Hoge CW, Mcgurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med. 2008;358(5):453–63.
Gadermann AM, Engel CC, Naifeh JA, Nock MK, Petukhova M, Santiago PN, et al. Prevalence of DSM-IV major depression among U.S. military personnel: meta-analysis and simulation. Mil Med. 2012;177(8 Suppl):47–59.
Vaughan CA, Schell TL, Tanielian T, Jaycox LH, Marshall GN. Prevalence of mental health problems among Iraq and Afghanistan veterans who have and have not received VA services. Psychiatr Serv. 2014;65(6):833–5.
Milanak ME, Gros DF, Magruder KM, Brawman-mintzer O, Frueh BC. Prevalence and features of generalized anxiety disorder in Department of Veteran Affairs primary care settings. Psychiatry Res. 2013;209(2):173–9.
Mysliwiec V, Gill J, Lee H, Baxter T, Pierce R, Barr TL, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549–57.
Pugh MJ, Finley EP, Copeland LA, et al. Complex comorbidity clusters in OEF/OIF veterans: the polytrauma clinical triad and beyond. Med Care. 2014;52(2):172–81.
Cifu DX, Taylor BC, Carne WF, Bidelspach D, Sayer NA, Scholten J, et al. Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND veterans. J Rehabil Res Dev. 2013;50(9):1169–76.
Lew HL, Otis JD, Tun C, Kerns RD, Clark ME, Cifu DX. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: polytrauma clinical triad. J Rehabil Res Dev. 2009;46(6):697–702.
• National Center for PTSD. Report of (VA) consensus conference: practice recommendations for treatment of veterans with comorbid TBI, pain, and PTSD. This report provides results of a consensus panel convened in Washington, D.C. on June 1 and 2, 2009 to make specific practice recommendations to improve the VA health care services, educational, and systems coordination for Veterans with posttraumatic stress disorder (PTSD), pain and a history of mild traumatic brain injury (mTBI). Three key questions were addressed: what are the best approaches to assessment, what are challenges to treatment planning and what are the most effective treatment strategies, according to the practice guidelines. Available at: https://www.ptsd.va.gov/professional/pages/handouts-pdf/TBI_PTSD_Pain_Practice_Recommend.pdf. Accessed 1 Oct 2017.
Word Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders, Clinical Descriptions and Diagnostic Guidelines. 1992. http://www.who.int/classifications/icd/en/bluebook.pdf. Accessed 3 Oct 2017.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). 2013. Washington, D.C.
Donnell AJ, Kim MS, Silva MA, Vanderploeg RD. Incidence of postconcussion symptoms in psychiatric diagnostic groups, mild traumatic brain injury, and comorbid conditions. Clin Neuropsychol. 2012;26(7):1092–101.
Donnelly K, Donnelly JP, Warner GC, Kittleson CJ, King PR. Longitudinal study of objective and subjective cognitive performance and psychological distress in OEF/OIF Veterans with and without traumatic brain injury. Clin Neuropsychol. 2017;1–20. https://doi.org/10.1080/13854046.2017.1390163
• Soble JR, Critchfield EA, O'rourke JJ. Neuropsychological evaluation in traumatic brain injury. Phys Med Rehabil Clin N Am. 2017;28(2):339–50. This article defines and reports on the clinical utility of neuropsychological evaluation after traumatic brain injury (TBI). The evaluation elucidates cognitive, behavioral, and emotional sequelae and can contribute to TBI patient care by aiding with prognostic assessment, measuring interval change/recovery over time (eg, resolution of posttraumatic amnesia), informing and implementing rehabilitation strategies, and evaluating the effectiveness of interventions.
Schretlen DJ, Shapiro AM. A quantitative review of the effects of traumatic brain injury on cognitive functioning. Int Rev Psychiatry. 2003;15(4):341–9.
Belanger HG, Vanderploeg RD. The neuropsychological impact of sports-related concussion: a meta-analysis. J Int Neuropsychol Soc. 2005;11(4):345–57.
Rohling ML, Binder LM, Demakis GJ, Larrabee GJ, Ploetz DM, Langhinrichsen-rohling J. A meta-analysis of neuropsychological outcome after mild traumatic brain injury: re-analyses and reconsiderations of binder et al. (1997), Frencham et al. (2005), and Pertab et al. (2009). Clin Neuropsychol. 2011;25(4):608–23.
Lippa SM, Pastorek NJ, Benge JF, Thornton GM. Postconcussive symptoms after blast and nonblast-related mild traumatic brain injuries in Afghanistan and Iraq war veterans. J Int Neuropsychol Soc. 2010;16(5):856–66.
Meares S, Shores EA, Taylor AJ, Batchelor J, Bryant RA, Baguley IJ, et al. The prospective course of postconcussion syndrome: the role of mild traumatic brain injury. Neuropsychology. 2011;25(4):454–65.
Belanger HG, Kretzmer T, Vanderploeg RD, French LM. Symptom complaints following combat-related traumatic brain injury: relationship to traumatic brain injury severity and posttraumatic stress disorder. J Int Neuropsychol Soc. 2010;16(1):194–9.
Carroll LJ, Cassidy JD, Peloso PM, et al. Prognosis for mild traumatic brain injury: results of the WHO collaborating Centre task force on mild traumatic brain injury. J Rehabil Med 2004;(43 Suppl):84–105.
Bradford LS. Misconceptions about traumatic brain injury among U.S. Army behavioral health professionals. Rehabil Psychol. 2015;60(4):344–52.
Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatr Serv. 2009;60(8):1118–22.
• Hoge CW, Grossman SH, Auchterlonie JL, Riviere LA, Milliken CS, Wilk JE. PTSD treatment for soldiers after combat deployment: low utilization of mental health care and reasons for dropout. Psychiatr Serv. 2014;65(8):997–1004. This study assessed the percentage of soldiers in need of PTSD treatment, the percentage receiving minimally adequate care, and reasons for dropping out of care. Results indicated that treatment reach for PTSD after deployment was low to moderate, with a high percentage of soldiers not accessing care or not receiving adequate treatment.
Al sayegh A, Sandford D, Carson AJ. Psychological approaches to treatment of postconcussion syndrome: a systematic review. J Neurol Neurosurg Psychiatry. 2010;81(10):1128–34.
Comper P, Bisschop SM, Carnide N, Tricco A. A systematic review of treatments for mild traumatic brain injury. Brain Inj. 2005;19:863–80.
Snell DL, Surgenor LJ, Hay-Smith EJ, Siegert RJ. A systematic review of psychological treatments for mild traumatic brain injury: an update on the evidence. J Clin Exp Neuropsychol. 2009;31:20–38.
• Cooper DB, Bunner AE, Kennedy JE, Balldin V, Tate DF, Eapen BC, et al. Treatment of persistent post-concussive symptoms after mild traumatic brain injury: a systematic review of cognitive rehabilitation and behavioral health interventions in military SMs and veterans. Brain Imaging Behav. 2015;9:403–20. This systematic review examined non-pharmacologic behavioral health interventions and cognitive rehabilitation interventions for PCS in military service members and veterans with a history of mild TBI (mTBI). 19 articles met criteria for inclusion. Studies were categorized into four subtypes: psychoeducational interventions, cognitive rehabilitation, psychotherapeutic approaches, and integrated behavioral health interventions for PCS and PTSD. The review provides an update of the empirical evidence for these four types of interventions for PCS in active duty service members and veterans and recommendations for future research are discussed.
Mittenberg W, Tremont G, Zielinski RE, Fichera S, Rayls KR. Cognitive-behavioral prevention of postconcussion syndrome. Arch Clin Neuropsychol. 1996;11:139–45.
Ponsford J, Willmott C, Rothwell A, Cameron P, Kelly AM, Nelms R, et al. Impact of early intervention on outcome following mild head injury in adults. J Neurol Neurosurg Psychiatry. 2002;73:330–2.
Wade DT, King NS, Wenden FJ, Crawford S, Caldwell FE. Routine follow up after head injury: a second randomized controlled trial. J Neurol Neurosurg Psychiatry. 1998;65:177–83.
Paniak C, Toller-Lobe G, Durand A, Nagy J. A randomized trial of two treatments for mild traumatic brain injury. Brain Inj. 1998;12:1011–23.
Paniak C, Toller-Lobe G, Reynolds S, Melnyk A, Nagy J. A randomized trial of two treatments for mild traumatic brain injury: 1 year follow-up. Brain Inj. 2000;14:219–26.
King EG, Kretzmer TS, Vanderploeg RD, Asmussen SB, Clement VL, Belanger HG. Pilot of a novel intervention for postconcussive symptoms in active duty, veterans, and civilians. Rehabil Psychol. 2013;58:272–9.
Belanger HG, Barwick F, Silva MA, Kretzmer T, Kip KE. Vanderploeg RD web-based psychoeducational intervention for postconcussion symptoms: a randomized trial. Mil Med. 2015;180:192–200. https://doi.org/10.7205/MILMED-D-14-00388.
Helmick K, Members of Consensus, C. Cognitive rehabilitation for military personnel with mild traumatic brain injury and chronic post-concussional disorder: results of April 2009 consensus conference. NeuroRehabilitation. 2010;26(3):239–55. https://doi.org/10.3233/NRE-2010-0560.
Cicerone KD, Dahlberg C, Kalmar K, Langenbahn DM, Malec JF, Bergquist TF, et al. Evidence-based cognitive rehabilitation: recommendations for clinical practice. Arch Phys Med Rehabil. 2000;81:1596–615.
Cicerone KD, Dahlberg C, Malec JF, Langenbahn DM, Felicetti T, Kneipp S, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 1998 through 2002. Arch Phys Med Rehabil. 2005;86:1681–92.
Cicerone KD, Langenbahn DM, Braden C, Malec JF, Kalmar K, Fraas M, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Arch Phys Med Rehabil. 2011;92:519–30. https://doi.org/10.1016/j.apmr.2010.11.015.
Belanger HG, Curtiss G, Demery JA, Lebowitz BK, Vanderploeg RD. Factors moderating neuropsychological outcomes following mild traumatic brain injury: a meta-analysis. J Int Neuropsychol Soc. 2005;11:215–27.
Drag LL, Spencer RJ, Walker SJ, Pangilinan PH, Bieliauskas LA. The contributions of self-reported injury characteristics and psychiatric symptoms to cognitive functioning in OEF/OIF veterans with mild traumatic brain injury. J Int Neuropsychol Soc. 2012;18(3):576–84.
Spencer RJ, Drag LL, Walker SJ, Bieliauskas LA. Self-reported cognitive symptoms following mild traumatic brain injury are poorly associated with neuropsychological performance in OIF/OEF veterans. J Rehabil Res Dev. 2010;47(6):521–30.
Chen AJ, Novakovic-agopian T, Nycum TJ, et al. Training of goal-directed attention regulation enhances control over neural processing for individuals with brain injury. Brain. 2011;134(Pt 5):1541–54.
Nelson LA, MacDonald M, Stall C, Pazdan R. Effects of interactive metronome therapy on cognitive functioning after blast-related brain injury: a randomized controlled pilot trial. Neuropsychology. 2013;27:666–79.
Huckans M, Pavawalla S, Demadura T, Kolessar M, Seelye A, Roost N, et al. A pilot study examining effects of group-based cognitive strategy training treatment on self-reported cognitive problems, psychiatric symptoms, functioning, and compensatory strategy use in OIF/OEF combat veterans with persistent mild cognitive disorder and history of traumatic brain injury. J Rehabil Res Dev. 2010;47:43–60.
Twamley EW, Jak AJ, Delis DC, Bondi MW, Lohr JB. Cognitive symptom management and rehabilitation therapy (CogSMART) for veterans with traumatic brain injury: pilot randomized controlled trial. J Rehabil Res Dev. 2014;51:59–70.
• Storzbach D, Twamley EW, Roost MS, Golshan S, Williams RM, OʼNeil M, et al. Compensatory cognitive training for operation enduring freedom/operation iraqi freedom/operation new dawn veterans with mild traumatic brain injury. J Head Trauma Rehabil. 2017;32:16–24. 50 Veterans were randomized to a Compensatory Cognitive Therapy (CCT) group, while 69 Veterans were randomized to a usual care control group. The CCT group participated in 10 weeks of CCT. Veterans who participated in CCT reported significantly fewer cognitive and memory difficulties and greater use of cognitive strategies. They also demonstrated significant improvements on neurocognitive tests of attention, learning, and executive functioning, which were 3 of the cognitive domains targeted in CCT.
Twamley EW, Thomas KR, Gregory AM, Jak AJ, Bondi MW, Delis DC, et al. CogSMART compensatory cognitive training for traumatic brain injury: effects over 1 year. J Head Trauma Rehabil. 2015;30:391–401.
Chard KM, Schumm JA, McIlvain SM, Bailey GW, Parkinson RB. Exploring the efficacy of a residential treatment program incorporating cognitive processing therapy-cognitive for veterans with PTSD and traumatic brain injury. J Trauma Stress. 2011;24:347–51. https://doi.org/10.1002/jts.20644.
Walter KH, Barnes SM, Chard KM. The influence of comorbid MDD on outcome after residential treatment for veterans with PTSD and a history of TBI. J Trauma Stress. 2012;25(4):426–32.
Walter KH, Kiefer SL, Chard KM. Relationship between posttraumatic stress disorder and postconcussive symptom improvement after completion of a posttraumatic stress disorder/traumatic brain injury residential treatment program. Rehabil Psychol. 2012;57(1):13–7.
• Cooper DB, Bowles AO, Kennedy JE, Curtiss G, French LM, Tate DF, et al. Cognitive rehabilitation for military service members with mild traumatic brain injury: a randomized clinical trial. J Head Trauma Rehabil. 2017;32(3):E1–E15. This randomized clinical trial included 126 service members with reported ongoing cognitive difficulties who were enrolled 3-24 month after mTBI and randomly assigned to one of four 6-week treatment arms: (1) psychoeducation, (2) computer-based CR, (3) therapist-directed manualized CR, and (4) integrated therapist-directed CR combined with cognitive-behavioral psychotherapy (CBT). All 4 treatment groups showed a significant improvement over time on 3 primary outcome measures. Both therapist-directed CR and integrated CR with CBT reduced functional cognitive symptoms in service members after mTBI beyond psychoeducation and medical management alone.
Cooper DB, Cornis-Pop M, Goo-Yoshino S., Hammond CS, Kennedy MT, MacLennan D, et al. Clinician’s guide to cognitive rehabilitation for mild traumatic brain injury: application for military SMs and veterans. http://www.asha.org/uploadedFiles/ASHA/Practice_Portal/Clinical_Topics/Traumatic_Brain_Injury_in_Adults/Clinicians-Guide-to-Cognitive-Rehabilitation-in-Mild-Traumatic-Brain-Injury.pdf. Accessed 20 Oct 2017.
• Potter SD, Brown RG, Fleminger S. Randomised, waiting list controlled trial of cognitive–behavioural therapy for persistent postconcussional symptoms after predominantly mild–moderate traumatic brain injury. J Neurol Neurosurg Psychiatry. 2016;87:1075–83. Two-center randomized trial with 46 adults with persistent PCS after predominantly mild-to-moderate TBI. Cognitive-behavioral therapy (12 sessions) was compared to waiting list control condition. Improvements associated with CBT were found on the primary outcome measures relating to quality of life (using the Quality of Life Assessment Schedule and the Brain Injury Community Rehabilitation Outcome Scale).
Cooper DB, Kennedy JE, Cullen MA, Critchfield E, Amador RR, Bowles AO. Association between combat stress and post-concussive symptom reporting in OEF/OIF service members with mild traumatic brain injuries. Brain Inj. 2011;25(1):1–7.
Davis JJ, Walter KH, Chard KM, Parkinson RB, Houston WS. Treatment adherence in cognitive processing therapy for combat-related PTSD with history of mild TBI. Rehabil Psychol. 2013;58:36–42.
Sripada RK, Rauch SA, Tuerk PW, Smith E, Defever AM, Mayer RA, et al. Mild traumatic brain injury and treatment response in prolonged exposure for PTSD. J Trauma Stress. 2013;26:369–75.
Gros DF, Lancaster CL, Horner MD, Szafranski DD, Back SE. The influence of traumatic brain injury on treatment outcomes of concurrent treatment for PTSD and substance use disorders using prolonged exposure (COPE) in veterans. Compr Psychiatry. 2017;78:48–53.
Wolf GK, Strom TQ, Kehle SM, Eftekhari A. A preliminary examination of prolonged exposure therapy with Iraq and Afghanistan veterans with a diagnosis of posttraumatic stress disorder and mild to moderate traumatic brain injury. J Head Trauma Rehabil. 2012;27:26–32.
• Wolf GK, Kretzmer T, Crawford E, Thors C, Wagner HR, Strom TQ, et al. Prolonged exposure therapy with veterans and active duty personnel diagnosed with PTSD and traumatic brain injury. J Trauma Stress. 2015;28:339–47. Prolonged exposure therapy was evaluated in 69 OIF/OEF/OND Veterans with TBI and PTSD via archival clinical data review. Treatment was associated with significant decreases in PTSD and depressive symptoms. Participants with moderate to severe injuries reported more rapid gains than those with a history of mild TBI.
Wolf GK, Mauntel GJ, Kretzmer T, et al. Comorbid posttraumatic stress disorder and traumatic brain injury: generalization of prolonged exposure PTSD treatment outcomes to postconcussive symptoms, cognition, and self-efficacy in veterans and active duty SMs. J Head Trauma Rehabil 2018. https://doi.org/10.1097/HTR.0000000000000344
Tiersky LA, Anselmi V, Johnston MV, Kurtyka J, Roosen E, Schwartz T, et al. A trial of neuropsychologic rehabilitation in mild-spectrum traumatic brain injury. Arch Phys Med Rehabil. 2005;86:1565–74.
• Gardner AJ, Shih SL, Adamov EV, Zafonte RD. Research Frontiers in traumatic brain injury: defining the injury. Phys Med Rehabil Clin N Am. 2017;28(2):413–31. This article summarizes the latest advances in TBI research, focusing on studies using sophisticated neuroimaging, serum and blood biomarkers, genetic markers and physiological parameters.
Eapen BC, Murphy DP, Cifu DX. Neuroprosthetics in amputee and brain injury rehabilitation. Exp Neurol. 2017;287(Pt 4):479–85.
Acknowledgements
The authors have no conflicts of interest to report, and none have any financial interest with the subject matter discussed in the manuscript. The views expressed herein are those of the authors and do not necessarily reflect the views or the official policy of the Department of Defense, Department of Veterans Affairs, or US Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the South Texas Veterans Healthcare System, the Army Office of the Surgeon General, the Department of the Army, the Department of Defense, the Department of Veterans Affairs or the U.S. Government.
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Brain Injury Medicine and Rehabilitation
Rights and permissions
About this article
Cite this article
Soble, J.R., Cooper, D.B., Lu, L.H. et al. Symptom Reporting and Management of Chronic Post-Concussive Symptoms in Military Service Members and Veterans. Curr Phys Med Rehabil Rep 6, 62–73 (2018). https://doi.org/10.1007/s40141-018-0173-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-018-0173-1