Abstract
Greater trochanteric pain syndrome (GTPS) is a common cause of extra-articular lateral hip pain. The underlying etiology of GTPS ranges from gluteus medius and minimus tendinopathy or tears, to external coxa saltans or iliotibial band syndrome. Historically, this source of lateral hip pain was typically diagnosed as trochanteric bursitis as it was believed to be due to inflammation of the subgluteus maximus bursa. However, recent imaging and histopathological studies have shown that most cases are instead due to underlying gluteus medius or minimus tendon disorders. Identifying the specific pain generator in GTPS is important as the treatment differs depending on the cause. Strengthening should be prescribed in cases of gluteal tendinopathy; corticosteroid injections and NSAIDs may be helpful in cases of primary bursitis; and surgery may be indicated in functionally limiting gluteal tendon tears unresponsive to conservative treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Greater trochanteric pain syndrome (GTPS) describes a spectrum of lateral hip pain causes characterized by peritrochanteric pain and focal tenderness [1]. GTPS occurs in up to 10–25 % of the general population [2, 3]. In the primary care setting, the incidence is 1.8 patients per 1,000 per year [2].
The etiology of GTPS ranges from gluteus medius and minimus tendinopathy or tears to less commonly trochanteric bursitis, iliotibial band friction syndrome, or external coxa saltans. Previously, most cases were diagnosed as trochanteric bursitis, as the pain generator was believed to be bursal inflammation from gluteal tendon friction at the greater trochanteric attachment. As a result, standard treatments for this condition included non-steroidal anti-inflammatory medications and corticosteroid injections. However, treatments focused on relieving inflammation typically only provide short-term pain relief as bursitis is not the primary underlying pathology in most cases [4••, 5, 6].
Imaging and histopathological studies have not identified bursal inflammation as a consistent finding in GTPS [7–9]. In patients with trochanteric bursitis who had their bursae removed during total hip arthroplasty, histopathological analysis of the bursae demonstrated fibroadipose and fibroconnective tissue with no signs of acute or chronic inflammation or of increased fibrosis [9]. Bursal abnormalities such as increased fluid or thickening occur as reactive or secondary findings to underlying gluteal muscle tendon tear [10]. In an MRI study of 24 patients with GTPS, only 2 had trochanteric bursal distension, whereas 11 had a gluteus medius tear and 9 had gluteus medius tendinitis [7]. Trochanteric bursal distension was an uncommon finding and did not occur in the absence of gluteus medius pathology [7]. Recent studies suggest that the most common cause of GTPS is gluteus medius or minimus tendinopathy [7, 11].
Anatomy
An understanding of the anatomy of the greater trochanteric region helps elucidate the possible sites and mechanisms for pathology. The greater trochanteric muscle attachment configuration has been likened to that of a “rotator cuff of the hip” [12]. Pfirrman et al. described the greater trochanter as having four major facets which are identifiable landmarks on ultrasound and MRI imaging [13]. The gluteus medius and minimus originate from the external iliac fossa. The gluteus medius tendon has a broad insertion at the lateral and a narrow insertion at the superolateral facet. The gluteus minimus tendon inserts at the anterior facet [14]. The tensor fascia lata, with its insertion on the iliotibial band, overlies the gluteus medius and minimus muscles.
Trochanteric bursal anatomy varies as described in cadaveric and imaging studies [14–16]. Bursae are small fluid-filled sacs that act as gliding interfaces between bony surfaces and soft tissue. There are three main bursae. The subgluteus maximus bursa, the largest of the three, lies deep to the gluteus maximus muscle, covers the posterior facet, and overlies the attachment of the gluteus medius, minimus, and vastus lateralis muscles on the greater trochanter [15]. The subgluteus minimus bursa lies between the gluteus minimus tendon and the anterior facet. The subgluteus medius bursa lies beneath the insertion of the gluteus medius tendon on the lateral and superolateral facet [14]. Another cadaveric study identified as many as four bursae present beneath the gluteus maximus muscle and the tensor fascia lata. Usually two bursae, the anterior and posterior subgluteus medius bursae, lie beneath the gluteus medius tendon. In most cases, a single bursa is located deep to the gluteus minimus tendon [16]. The sensory innervation of the greater trochanter bursae and periosteum is supplied by branches of the femoral nerve [17].
Risk Factors and Associated Conditions
It is important to identify predisposing risk factors for GTPS through detailed history taking. Intrinsic risk factors include older age, female sex, and biomechanical factors [18•]. Extrinsic risk factors include recent changes in physical activity type, intensity, or duration.
The peak incidence of GTPS is between 40 and 60 years of age [2, 3]. This older age distribution is similar to that for other degenerative tendinopathies and tendon tears [19, 20]. Female sex is also commonly described as a risk factor as GTPS is diagnosed three to five times more frequently in women than in men. The greater incidence of GTPS in women has been postulated to relate to differences in pelvic biomechanics, hormonal effects, or activity between the populations [3, 21].
It is controversial in the literature whether obesity and leg length discrepancy are true risk factors for GTPS. In 1976, a case series including 4 patients with hip arthritis was documented to have leg length discrepancy associated with GTPS [22]. However, in a cross-sectional analysis of 277 patients with GTPS and 1159 without GTPS, leg length discrepancy was not associated with GTPS [23].
While elevated abdominal obesity and peripheral adiposity have been associated with tendinopathies in general [24–26], Segal et al. found that BMI alone was not related to GTPS [3]. In women, specifically, a gynoid pattern adiposity has been associated with GTPS [18•]. The wider pelvis in women has also been implicated as a risk factor because the gluteal tendons wrap over a greater proportion of the greater trochanter leading to increased compressive forces [27]. Fearon et al. elaborated on this further to describe that a lower femoral neck shaft angle or coxa vara is an independent risk factor for GTPS in women [18•].
The presence of other lower limb or spine injuries or disorders is important to identify. Prior or associated trauma, surgery, or injury to the spine, hip, or lower limb may contribute to altered forces at the greater trochanteric tendon attachments. The higher prevalence of GTPS in adults with iliotibial band pain and knee osteoarthritis suggests that lower limb biomechanics relates to GTPS [3]. In patients with back pain referred to a tertiary care orthopedic spine referral center, 20.2 % had GTPS [28].
Suspected cases of GTPS in patients with prior THA deserve special consideration as hip abductor tendon avulsions can occur following THA performed through the anterolateral, trans-gluteal approach [29]. The anterolateral THA approach is associated with potential complications including superior gluteal nerve injury or failure of the abductor muscle repair [30]. GTPS can present as an early or late finding. In a study of 543 patients post THA, lateral trochanteric pain was identified in 4.4 % of patients beginning at a mean of 19 months after surgery (range 6–43 months) [31]. GTPS was also significantly more common in patients who underwent lateral versus posterior approach THA (p < 0.01) [31]).
In athletes, running on an asymmetric surface, such as a crowned road, has been described as a risk factor [32]. Other factors to consider in athletes include asymmetric shoe wear, iliotibial band tightness, and training errors [11]. It is also important to evaluate for kinetic chain factors such as core stability or the presence of other sports injuries as abnormal motion and joint loading in one region of the kinetic chain can contribute to the development of GTPS.
Diagnosis and Physical Exam
GTPS is characterized by lateral hip pain and focal tenderness to palpation at the greater trochanter. Symptom onset may be acute or insidious. The pain may radiate as a pseudoradiculopathy down the lateral thigh to the knee [33]. Aggravating factors include weight-bearing activities such as prolonged standing, walking, stair climbing, or running. Pain may be provoked by crossing the legs or lying on the affected side, due to direct pressure, or unaffected side, due to the adducted position of the affected lower limb at night while sleeping [1].
One should consider both extra- and intra-articular causes in the differential diagnosis of lateral hip pain. Aside from GTPS, other extra-articular causes include iliotibial band syndrome and external snapping coxa saltans. Intra-articular hip pathology such as labral tears, femoroacetabular impingement, osteoarthritis, femoral neck stress fractures, or avascular necrosis of the femoral head can also cause lateral hip pain. If localized signs of inflammation—redness, heat, and swelling—are appreciated at the lateral hip, consider septic bursitis in the differential diagnosis as these clinical signs should not occur typically in GTPS. Septic trochanteric bursitis has been described due to infectious causes such as tuberculosis [34, 35]. Post-traumatic trochanteric bursitis can result from direct impact to the hip region from a fall or from contact sports and may be accompanied by contusions [36]. Crystal arthropathy such as gout or pseudogout can also cause trochanteric bursitis [33]. An L2 or L3 radiculitis or radiculopathy can refer pain to the lateral hip region. An L5 radiculopathy may also be associated with lateral hip and buttock pain as the gluteal muscles are innervated by the superior and inferior gluteal nerves, which receive innervation from this nerve root [37]. Radiculopathy should be ruled out in the history and neurologic examination, as the neurologic examination is normal in GTPS except for possible hip abductor weakness.
On physical examination in GTPS, local discomfort may be reproduced by palpating the greater trochanteric region. Physical exam maneuvers such as passive hip rotation and resisted hip abduction in a side lying position have low sensitivity and high specificity for gluteal tendinopathy [16, 38]. Pain may also be elicited with active hip internal or external rotation at 45 degrees of hip flexion [11].
The hip lag sign is helpful in predicting hip abductor injury [39]. The hip lag sign has a 90 % sensitivity and 97 % specificity for predicting MRI confirmed gluteus medius or minimus tear, atrophy, or tendinosis. This physical exam maneuver is performed by having the patient lie in a lateral position with the affected leg on top. The examiner passively extends the affected hip to 10°, abduct to 20° and rotate internally as far as possible, while the knee remains 45° flexed. The patient is asked to actively hold the leg in this position, and the hip lag sign is considered positive if the patient is not able to maintain the leg in the original position and the foot drops more than 10 cm [39].
The Trendelenburg sign can be seen in GTPS due to weakness or pain-related inhibition of the gluteus medius or minimus muscles [7]. The gluteus medius and minimus muscles play a primary role in hip abduction and pelvic stabilization in walking, running, and the single-legged activities [40]. In GTPS with weight bearing on the affected limb during the single-leg stance, the hip abductors are unable to stabilize the pelvis, resulting in contralateral pelvic drop [41]. The Trendelenburg sign has 73 % sensitivity and 77 % specificity for detecting gluteus medius tears [7]. A similar test is a 30-s single-leg stance test, in which pain is reproduced while standing on the affected limb for 30 s. This test has a 100 % sensitivity and 97.3 % specificity for gluteal tendinopathy in patients with GTPS [38].
Measuring true leg length can help identify patients with clinically significant leg length discrepancies who may benefit from a trial of corrective orthotic footwear. A positive Ober test may indicate IT band tightness which can contribute to GTPS.
Diagnostic Imaging
In the majority of cases, GTPS is a clinical diagnosis. Imaging studies are indicated when there is concern for other underlying pathology, and the diagnosis is unclear, or to evaluate cases unresponsive to appropriate trial of conservative management. Plain radiographs are helpful when the hip pain is suspected due to bony pathology such as femoroacetabular impingement, osteoarthritis, or femoral neck stress fracture. In GTPS, hip plain films may demonstrate calcifications localized to the bursae or in the gluteal tendon insertions due to calcific tendinosis. Radiographs are also helpful in identifying patients with a lower femoral neck shaft angle, coxa vara, as that has been described as a risk factor for GTPS [18•].
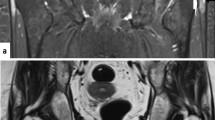
MRI can help identify gluteal tendinopathy, muscle tears, greater trochanteric cortical irregularity, bursal fluid or thickening, muscle atrophy, or fatty degeneration [8, 14, 42]. MRI is also indicated if underlying hip intra-articular pathology is suspected. Clinical correlation of imaging findings is important because peritrochanteric abnormalities can also be seen on MRIs in asymptomatic individuals [42]. Specifically, peritrochanteric edema T2 signal change on MRI is seen with increasing age even in the absence of clinical symptoms [43].
Ultrasound is helpful given the dynamic nature of the imaging modality; however, its diagnostic accuracy is operator dependent. Ultrasound can help visualize the gluteal muscle insertions on the greater trochanteric facets to localize pathology, and it has a high positive predictive value (PPV = 1.0) for identifying peritrochanteric abnormalities [10]). Gluteal tendinopathy is characterized by tendon heteroechogenicity, hypertrophy, neovascularization, or abnormal tendon architecture. Partial or full thickness gluteal tendon tears appear as focal hypoechoic or anechoic regions. Bursal effusions appear as anechoic fluid collections [11].
Rehabilitation
Conservative treatments are first line for GTPS and include icing, analgesic pain relief, relative rest, and activity modification. Advice on avoiding the activities and positions that exacerbate symptoms is helpful during the acute phase.
The rehabilitation plan should address any kinetic chain factors and gait abnormalities identified during the physical exam. Strengthening should incorporate the core and lumbopelvic stabilizers, hip abductors, extensors, and external rotators. Gluteal strengthening should progress from open chain kinetic muscle activation to functional, dynamic, and weight-bearing closed kinetic chain exercises while also advancing from concentric to eccentric loading. Rompe et al., in a trial comparing home exercises, low-energy extracorporeal shockwave therapy, and corticosteroid injections, described an exercise program incorporating piriformis stretch, iliotibial band stretching, straight leg raise, wall squats, and prone gluteal isometric contractions [6]. Commonly prescribed physical therapy exercises which activate a high maximal voluntary isometric contraction percentage of the gluteus medius muscle include the side plank with hip abduction, the single-limb squat, and clamshell [44, 45]. While no published study to date has evaluated the outcome of eccentric strengthening for gluteal tendinopathy, eccentric loading exercises have been effective in the rehabilitation of Achilles, patellar, and other common tendinopathies [46, 47].
If symptoms have been chronic, the patient may have developed dysfunctional neuromuscular control patterns in the hip and pelvis and have impaired activation of the gluteal muscles in isolation or during functional activities. Neuromuscular re-education to improve dynamic alignment and loading is helpful to address gluteal muscle activation and timing deficits. A running gait analysis is a potentially beneficial diagnostic tool in runners. If a tight IT band or IT band syndrome is identified, myofascial release or foam roller use for self soft tissue mobilization and stretching should be incorporated into the rehabilitation program. Low-energy extracorporeal shockwave therapy has also been described as an effective non-invasive treatment for GTPS [6, 48].
Medications and Injections
Symptomatic pain relief oral analgesics such as acetaminophen may be helpful. The role of nonsteroidal anti-inflammatory drugs (NSAIDs) is controversial in the treatment of tendinopathies. While NSAIDs may help in cases of primary bursitis or for analgesia in the acute period, long-term NSAIDs use is not advisable in chronic gluteal tendinopathy or tendon tears given the literature suggesting the potential adverse effects of NSAIDs on tendon healing [49–51].
In cases of isolated trochanteric bursitis, local anesthetic and corticosteroid trochanteric bursa injections correlated with a greater reduction in lateral hip symptoms following both in the immediate post-injection phase and in the long term [52]. However, given that the majority of cases of GTPS are due to gluteal tendon disorders and are non-inflammatory in nature, corticosteroid injections are not advisable as a first-line treatment. While some studies have found corticosteroid injections to be effective in the short term for improving pain and activity in GTPS, other studies report incomplete long-term relief and symptom recurrence [6, 53••, 54]. In a randomized controlled trial comparing exercise training, low-energy extracorporeal shockwave therapy, and corticosteroid injection, at 1-month follow-up, steroid injections provided the best pain relief. However, at 15-month follow-up, shock wave therapy and exercise training were superior to corticosteroid injection in terms of pain relief [6].
While regenerative biologic therapies such as platelet-rich protein and autologous conditioned plasma injections have been studied for the Achilles and patellar tendinopathy, lateral epicondylosis, and plantar fasciitis [19, 55–57], there are no published studies to date on the outcomes of these injections for GTPS.
Surgery
Surgery may be indicated in cases of full thickness or partial thickness gluteal tendon tears that are functionally limiting and not improving with conservative management. Procedures include open or arthroscopic gluteal tendon repair or reconstruction, bursectomy, or iliotibial band release or lengthening [58, 59]. Endoscopic repair of full and partial thickness gluteus medius tendon tears in patients who have failed conservative treatments has been found to provide good pain relief and return of hip abductor strength at one and 2 years follow-up [60•, 61]). While younger patients are reported to have better post-operative outcomes, McCormick et al. described in a case series of 11 patients with mean age 65.9 years (range 60–74 years) that elderly patients also have good to excellent functional outcomes and significantly improved hip abduction strength at a mean of 23 months follow-up [61].
The rehabilitation program following surgical repair of hip abductor tendon tears can vary depending on surgical technique and patient specific factors. Generally, patients are allowed to mobilize post-operatively with crutches and to fully weight bear as tolerated. Active and passive abduction of the post-operative hip is avoided for the initial 6 weeks. Subsequently, patients are allowed to perform passive hip abduction for activities of daily and progress to active hip abduction strengthening exercises under physical therapy instruction [30].
Conclusion
GTPS is a common cause of lateral hip pain that can impact an individual’s quality of life and activity participation [62]. The majority of cases are due to gluteus medius or minimus tendon disorders. Trochanteric bursitis, if present, exists most commonly as a secondary or associated finding. Appropriate identification of the underlying pain generator and predisposing risk factors is important for individualizing the treatment plan. Most cases of GTPS respond to appropriate conservative treatments including gluteal strengthening, neuromuscular re-education, and activity modification with surgery indicated in cases of functionally limiting gluteal tendon tears.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Karpinski MR, Piggott H. Greater trochanteric pain syndrome. A report of 15 cases. J Bone Joint Surg Br. 1985;67(5):762–3.
Lievense A, Bierma-Zeinstra S, Schouten B, Bohnen A, Verhaar J, Koes B. Prognosis of trochanteric pain in primary care. Br J Gen Pract. 2005;55:199–204.
Segal NA, Felson DT, Torner JC, Zhu Y, Curtis JR, Niu J, Nevitt MC. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehabil. 2007;88:988–92.
•• Del Buono A, Papalia R, Khanduja V, Denaro V, Maffulli N. Management of the greater trochanteric pain syndrome: a systematic review. Br Med Bull. 2012;102:115–31. This systematic review found that while published studies report significant pain relief and improved outcomes after conservative and surgical management of GTPS, the overall poor available data from small studies does not allow definitive conclusions to be drawn on what is the best treatment course for GTPS.
Labrosse JM, Cardinal E, Leduc BE, Duranceau J, Rémillard J, Bureau NJ, Belblidia A, Brassard P. Effectiveness of ultrasound-guided corticosteroid injection for the treatment of gluteus medius tendinopathy. AJR Am J Roentgenol. 2010;194(1):202–6.
Rompe JD, Segal NA, Cacchio A, Furia JP, Morral A, Maffulli N. Home training, local corticosteroid injection, or radial shock wave therapy for greater trochanter pain syndrome. Am J Sports Med. 2009;37:1981–90.
Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis Rheum. 2001;44(9):2138–45.
Kingzett-Taylor A, Tirman PF, Feller J, McGann W, Prieto V, Wischer T, Cameron JA, Cvitanic O, Genant HK. Tendinosis and tears of gluteus medius and minimus muscles as a cause of hip pain: MR imaging findings. AJR Am J Roentgenol. 1999;173(4):1123–6.
Silva F, Adams T, Feinstein J, Arroyo RA. Trochanteric bursitis: refuting the myth of inflammation. J Clin Rheumatol. 2008;14(2):82–6.
Fearon AM, Scarvell JM, Cook JL, Smith PN. Does ultrasound correlate with surgical or histologic findings in greater trochanteric pain syndrome? A pilot study. Clin Orthop Relat Res. 2010;468(7):1838–44.
Ho GW, Howard TM. Greater trochanteric pain syndrome: more than bursitis and iliotibial tract friction. Curr Sports Med Rep. 2012;11(5):232–8.
Bunker TD, Esler CN, Leach WJ. Rotator-cuff tear of the hip. J Bone Joint Surg Br. 1997;79(4):618–20.
Pfirrmann C, Chung C, Theurmann N, Trudell D, Resnick D. Greater trochanter of the hip: attachment of the abductor mechanism and a complex of three bursae-MR imaging and MR bursography in cadavers and MR imaging in asymptomatic volunteers. Radiology. 2001;221(3):469–77.
Kong A, Van der Vliet A, Zadow S. MRI and US of gluteal tendinopathy in greater trochanteric pain syndrome. Eur Radiol. 2007;17(7):1772–83.
Dunn T, Heller CA, McCarthy SW, Dos Remedios C. Anatomical study of the “trochanteric bursa”. Clin Anat. 2003;16(3):233–40.
Woodley SJ, Mercer SR, Nicholson HD. Morphology of the bursae associated with the greater trochanter of the femur. J Bone Joint Surg Am. 2008;90(2):284–94.
Genth B, Von Düring M, Von Engelhardt LV, Ludwig J, Teske W, Von Schulze-Pellengahr C. Analysis of the sensory innervations of the greater trochanter for improving the treatment of greater trochanteric pain syndrome. Clin Anat. 2012;25(8):1080–6.
• Fearon A, Stephens S, Cook J, Smith P, Neeman T, Cormick W, Scarvell J. The relationship of femoral neck shaft angle and adiposity to greater trochanteric pain syndrome in women. A case control morphology and anthropometric study. Br J Sports Med. 2012;46(12):888–92. This prospective case control study of four groups: those with GTPS, gluteal tendon reconstruction, or hip osteoarthritis, and of asymptomatic controls found that a lower femoral neck shaft angle is a risk factor for, and adiposity is associated with, GTPS in women.
de Jonge S, van den Berg C, de Vos RJ, van der Heide HJ, Weir A, Verhaar JA, Bierma-Zeinstra SM, Tol JL. Incidence of midportion Achilles tendinopathy in the general population. Br J Sports Med. 2011;45(13):1026–8.
Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604.
Blank E, Owens BD, Burks R, Belmont PJ Jr. Incidence of greater trochanteric pain syndrome in active duty US military servicemembers. Orthopedics. 2012;35(7):e1022–7.
Swezey RL. Pseudo-radiculopathy in subacute trochanteric bursitis of the subgluteus maximus bursa. Arch Phys Med Rehabil. 1976;57(8):387–90.
Segal NA, Harvey W, Felson DT, Yang M, Torner JC, Torner JC, Nevitt MC. Multicenter Osteoarthritis Study Group. Leg-length inequality is not associated with greater trochanteric pain syndrome. Arthritis Res Ther. 2008;10(3):R62.
Franceschi F, Papalia R, Paciotti M, Franceschetti E, Di Martino A, Maffulli N, Denaro V. Obesity as a risk factor for tendinopathy: a systematic review. Int J Endocrinol. 2014;2014:670262.
Gaida JE, Alfredson H, Kiss ZS, Bass SL, Cook JL. Asymptomatic Achilles tendon pathology is associated with a central fat distribution in men and a peripheral fat distribution in women: a cross sectional study of 298 individuals. BMC Musculoskelet Disord. 2010;2(11):41.
Rechardt M, Shiri R, Karppinen J, Jula A, Heliövaara M, Viikari-Juntura E. Lifestyle and metabolic factors in relation to shoulder pain and rotator cuff tendinitis: a population-based study. BMC Musculoskelet Disord. 2010;20(11):165.
Birnbaum K, Pandorf T. Finite element model of the proximal femur under consideration of the hip centralizing forces of the iliotibial tract. Clin Biomech (Bristol, Avon). 2011;26(1):58–64.
Tortolani PJ, Carbone JJ, Quartararo LG. Greater trochanteric pain syndrome in patients referred to orthopedic spine specialists. Spine J. 2002;2(4):251–4.
Lachiewicz PF. Abductor tendon tears of the hip: evaluation and management. J Am Acad Orthop Surg. 2011;19(7):385–91.
Rao BM, Kamal TT, Vafaye J, Taylor L. Surgical repair of hip abductors. A new technique using Graft Jacket allograft acellular human dermal matrix. Int Orthop. 2012;36(10):2049–53.
Iorio R, Healy WL, Warren PD, Appleby D. Lateral trochanteric pain following primary total hip arthroplasty. J Arthroplasty. 2006;21(2):233–6.
Sussman DH, Walker M, Tamburello M, et al. The effect of road camber on running kinematics. In: 19th International Symposium on Biomechanics in Sport. San Francisco. Blackwell J.R.; 2001. p. 109–212.
Gordon EJ. Trochanteric bursitis and tendinitis. Clin Orthop. 1961;20:193–202.
Jaovisidha S, Chen C, Ryu KN, Siriwongpairat P, Pekanan P, Sartoris DJ, Resnick D. Tuberculous tenosynovitis and bursitis: imaging findings in 21 cases. Radiology. 1996;201:507–13.
Yamamoto T, Iwasaki Y, Kurosaka M. Tuberculosis of the greater trochanteric bursa occurring 51 years after tuberculous nephritis. Clin Rheumatol. 2002;21:397–400.
Haller CC, Coleman PA, Estes NC, Grisolia A. Traumatic trochanteric bursitis. Kans Med. 1989;90(17–18):22.
Ellenberg M, Honet JC. Chapter 43: Lumbar Radiculopathy. In: Frontera WR, Silver JK, Rizzo TD, editors. Essentials of physical medicine & rehabilitation: musculoskeletal disorders, pain, and rehabilitation. 2nd ed. Philadelphia: Saunders; 2008.
Lequesne M, Mathieu P, Vuillemin-Bodaghi V, Bard H, Djian P. Gluteal tendinopathy in refractory greater trochanter pain syndrome: diagnostic value of two clinical tests. Arthritis Rheum. 2008;59(2):241–6.
Kaltenborn A, Bourg CM, Gutzeit A, Kalberer F. The Hip Lag Sign-prospective blinded trial of a new clinical sign to predict hip abductor damage. PLoS ONE. 2014;9(3):e91560.
Beck M, Sledge JB, Gautier E, Dora CF, Ganz R. The anatomy and function of the gluteus minimus muscle. J Bone Joint Surg Br. 2000;82-B(3):358–63.
Hardcastle P, Nade S. The significance of the Trendelenburg test. J Bone Joint Surg Br. 1985;67:741–6.
Blankenbaker DG, Ullrick SR, Davis KW, De Smet AA, Haaland B, Fine JP. Correlation of MRI findings with clinical findings of trochanteric pain syndrome. Skeletal Radiol. 2008;37(10):903–9.
Haliloglu N, Inceoglu D, Sahin G. Assessment of peritrochanteric high T2 signal depending on the age and gender of the patients. Eur J Radiol. 2010;75(1):64–6.
Boren K, Conrey C, Le Coguic J, Paprocki L, Voight M, Robinson TK. Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Int J Sports Phys Ther. 2011;6(3):206–23.
Distefano LJ, Blackburn JT, Marshall SW, Padua DA. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther. 2009;39(7):532–40.
Kingma JJ, de Knikker R, Wittink HM, Takken T. Eccentric overload training in patients with chronic Achilles tendinopathy: a systematic review. Br J Sports Med. 2007;41(6):e3.
Visnes H, Bahr R. The evolution of eccentric training as treatment for patellar tendinopathy (jumper’s knee): a critical review of exercise programmes. Br J Sports Med. 2007;41(4):217–23.
Furia JP, Rompe JD, Maffulli N. Low-energy extracorporeal shock wave therapy as a treatment for greater trochanteric pain syndrome. Am J Sports Med. 2009;37(9):1806–13.
Cohen DB, Kawamura S, Ehteshami JR, Rodeo SA. Indomethacin and celecoxib impair rotator cuff tendon-to-bone healing. Am J Sports Med. 2006;34(3):362–9.
Ferry ST, Dahners LE, Afshari HM, Weinhold PS. The effects of common anti-inflammatory drugs on the healing rat patellar tendon. Am J Sports Med. 2007;35(8):1326–33.
Su B, O’Connor JP. NSAID therapy effects on healing of bone, tendon, and the enthesis. J Appl Physiol. 1985. 2013;115(6):892–9.
Wilson SA, Shanahan EM, Smith MD. Greater trochanteric pain syndrome: does imaging-identified pathology influence the outcome of interventions? Int J Rheum Dis. 2013 Dec 6.
•• Brinks A, van Rijn RM, Willemsen SP, Bohnen AM, Verhaar JA, Koes BW, Bierma-Zeinstra SM. Corticosteroid injections for greater trochanteric pain syndrome: A randomized controlled trial in primary care. Ann Fam Med. 2011;9(3):226–34. This is the first randomized controlled trial assessing the effectiveness of corticosteroid injections versus usual care in GTPS. The study found that while injections had better reported outcomes at the 3-month follow-up visit, at the 12-month follow-up visit, the differences in outcome were no longer present.
Shbeeb MI, O’Duffy JD, Michet CJ Jr, O’Fallon WM, Matteson EL. Evaluation of glucocorticosteroid injection for the treatment of trochanteric bursitis. J Rheumatol. 1996;23:2104–6.
Chew KT, Leong D, Lin CY, Lim KK, Tan B. Comparison of autologous conditioned plasma injection, extracorporeal shockwave therapy, and conventional treatment for plantar fasciitis: a randomized trial. PM R. 2013;5(12):1035–43.
Dragoo JL, Wasterlain AS, Braun HJ, Nead KT. Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am J Sports Med. 2014;42(3):610–8.
Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34(11):1774–8.
Domb BG, Nasser RM, Botser IB. Partial-thickness tears of the gluteus medius: rationale and technique for trans-tendinous endoscopic repair. Arthroscopy. 2010;26(12):1697–705.
Fox JL. The role of arthroscopic bursectomy in the treatment of trochanteric bursitis. Arthroscopy. 2002;18:E34.
• Domb BG, Botser I, Giordano BD. Outcomes of endoscopic gluteus medius repair with minimum 2-year follow-up. Am J Sports Med. 2013;41(5):988–97. At two years follow up of cases of endoscopic repair of partial- and full-thickness gluteus medius tears, 14 of the 15 patients showed postoperative improvement in all 4 hip-specific outcome measures and reported satisfaction of good to excellent range with the surgery.
McCormick F, Alpaugh K, Nwachukwu BU, Yanke AB, Martin SD. Endoscopic repair of full-thickness abductor tendon tears: surgical technique and outcome at minimum of 1-year follow-up. Arthroscopy. 2013;29(12):1941–7.
Fearon AM, Cook JL, Scarvell JM, Neeman T, Cormick W, Smith PN. Greater trochanteric pain syndrome negatively affects work, physical activity and quality of life: a case control study. J Arthroplasty. 2014;29(2):383–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical collection on Musculoskeletal Rehabilitation.
Rights and permissions
About this article
Cite this article
Lin, C.Y., Fredericson, M. Greater Trochanteric Pain Syndrome: An Update on Diagnosis and Management. Curr Phys Med Rehabil Rep 3, 60–66 (2015). https://doi.org/10.1007/s40141-014-0071-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-014-0071-0