Abstract
Purpose of Review
This narrative review explores the technical principles and evidence supporting the use of advanced respiratory monitoring tools in the perioperative setting to enhance patient care. We aim to identify which patients benefit most from these technologies during major surgeries.
Recent Findings
Advanced monitoring techniques, such as electrical impedance tomography (EIT), esophageal pressure (Pes) monitoring, and lung ultrasound (LUS), provide detailed insights into lung mechanics and function. Recent studies indicate these tools can optimize ventilation strategies by individualizing the lung protective ventilation, particularly in high-risk patients.
Summary
While these tools can help to improve intraoperative respiratory mechanics and oxygenation, further randomized clinical trials are needed to confirm their impact on patient-centered outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
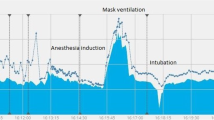
Postoperative pulmonary complications (PPCs) after major surgery and general anaesthesia are an important cause of morbidity and mortality in the perioperative setting [1]. To minimize such adverse events, it is crucial to identify predisposing conditions [2] and assess the underlying pathophysiology to provide a lung protective ventilation strategy [3, 4]. Ventilatory monitoring in the operating room is routinely based on the analysis of pressure, volume, and flow data provided by the ventilator [3, 5,6,7,8].
However, perioperative medicine has advanced, allowing for a broader array of surgeries on patients with serious health issues, such as extreme obesity or critical injuries. These include complex procedures like extended robotic surgeries in extreme positions or prolonged one-lung ventilation. Additionally, technological advancements provide new tools to monitor patients' physiological responses in real-time.
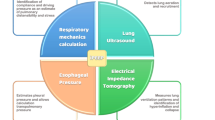
Currently, we can perioperatively employ devices such as electrical impedance tomography (EIT) that analyses lung regional ventilation [9], oesophageal pressure (Pes) monitoring which reflects approximately the pleural pressure, allowing transpulmonary pressure (Ptp) estimation [10], and lung and diaphragmatic ultrasound (US) that enable us to assess the echogenicity of the different lung fields to quantify aeration [11] or to assess diaphragmatic functionality [12]. This raises the question of whether and when these advanced respiratory monitoring tools should be used to prevent PPCs.
This review aims to summarize the technical underlying principles and explore the existing evidence on the usefulness of such advanced respiratory monitoring in the perioperative setting, specifically to ascertain which patients might benefit from it. We carried out a search in the Pubmed and Embase databases with the following criteria: (“respiratory monitoring" OR "ventilator monitoring" OR "lung function monitoring”) AND (intraoperative OR perioperative OR anesthesia OR surgery)”. We searched papers from 2009 to 2024 in the English language.
Monitoring of Ventilatory Mechanics Through Common Ventilatory Parameters Analysis
Conventional data such as pressure and flow curves or capnography can be leveraged to gain further insight into respiratory mechanics [13], helping us to assess the recruitment capacity and adequacy of patient ventilation [13, 14]. For instance, lung hysteresis, a physiological feature resulting from the visco-elastic properties of lung parenchyma, causes the pressure–volume relationship to differ between inflation and deflation [15, 16]. It can be quantified by the area enclosed within the quasi-static Pressure–Volume (PV) loops generated during mechanical ventilation [13]. These PV loops reveal a critical point where a sharp increase in ventilator pressure corresponds with a slower rise in lung volume, signaling the end of lung recruitment which could include some overdistension, whereas a pressure drop paired with a slower volume decrease indicates the onset of alveolar collapse [13, 15, 16]. Understanding these patterns helps to assess lung recruitability, and identify risks linked to mechanical ventilation [13].
The dynamic pressure–time curve can also be used to assess respiratory mechanics. For instance, the stress index (SI) [17], that assesses the dynamic pressure–time curve during constant inspiratory flow to detect intratidal recruitment or hyperinflation. A threshold SI value of greater than 1.05 has shown a sensitivity of 0.88 and a specificity of 0.50 to indicate injurious ventilation, which was contrasted with aeration indices based on computed tomography in ARDS patients. The SI obtained from the ventilator indicates the SI of the respiratory system and correlates with the lung SI with reasonable accuracy [18, 19].
Furthermore, volumetric capnography (VCap) performs a continuous assessment of the respiratory dead space [20] using the modified Bohr equation, which includes the tidal volume (VT), the partial pressure of CO2 at the end of alveolar respiration and the partial pressure of CO2 at the end of expiration (EtCO2) [21]. VCap divides the capnogram into three phases: Phase I, representing the CO2-free exhaled gas from the airways; Phase II, where a mix of airway and alveolar gases is present; and Phase III, which represents the alveolar plateau where gas exchange occurs. By separating the volume of gas in the airways from that within the alveolar compartment, it allows for precise calculations of dead space on a breath-by-breath basis. The slope of Phase III (SIII) is particularly informative as it reflects the ventilation-perfusion distribution in the alveoli. An increased slope indicates heterogeneity in alveolar ventilation. VCap is a current tool for clinical research works, proving to be an adequate guide in the assessment of end-expiratory lung volume (EELV) changes induced by surgical procedures and has proven to be useful in individualizing the level of PEEP during laparoscopic surgery [21, 22].
Nitrogen and helium techniques, particularly the washin/washout method, are commonly used to measure (EELV) [23]. This method calculates EELV based on the baseline nitrogen content in the lungs, which inversely correlates with alveolar oxygen levels [23, 24]. This approach has been extensively applied in studies on intraoperative mechanical ventilation and lung strain, revealing a high prevalence of expiratory flow limitation and airway closure in obese patients during laparoscopic surgery [25, 26].
Additional ventilatory parameters are used to evaluate lung characteristics non-invasively. For instance, the PEEP test identifies expiratory flow limitation and the air-test and the recruitment-to-inflation ratio assess alveolar recruitability. The PEEP-test consists in abruptly dropping from 3 cmH2O to 0 cmH2O and observing if there is outflow of gases, if not, there is expiratory flow limitation [27, 28]. The air test in healthy lungs checks if gas exchange at an FiO2 of 21–25% maintains a SatO2 above 96%; failure to do so suggests significant atelectasis with a shunt exceeding 10% [29]. The recruitment-to-inflation ratio involves a single breath test where PEEP is abruptly reduced from 15 to 5 cmH2O to measure expired volume and compare it against predicted compliance at low PEEP. This comparison estimates the volume of alveoli recruited by the PEEP, from which the compliance of the recruited lung is calculated. This ratio mathematically reflects the proportion of volume distributed into the recruited lung relative to the already aerated 'baby lung'. A higher R/I ratio indicates a greater potential for lung recruitment. Conversely, values below 0.5 suggest a lower probability of recruitment, which may warrant a lower PEEP setting [30].
Finally, some hemodynamic management strategies, such as the PEEP-test and tidal volume challenge (TVC), have been developed by manipulating ventilatory parameters. These tests assess fluid responsiveness by increasing intrathoracic pressure through enhanced PEEP or VT, utilizing heart–lung interactions to gauge hemodynamic effects [31, 32].
Advanced Respiratory Monitoring Tools Pros and Cons
Electrical Impedance Tomography
EIT is a non-invasive technique for monitoring lung ventilation as well as ventilation-perfusion mismatches. Electrodes are placed on the chest and record the surface voltage after repeated application of a small amount of electrical current. It provides images based on the chest tissues’ electrical conductivity [33]. The changes in electrical impedance are displayed as colour-coded images, providing a pixelated mapping of regional lung ventilation, thus adding information about the homogeneity of lung ventilation on a breath by breath [34]. EIT assesses hypoventilation, overdistension and areas of heterogeneous ventilation, allowing the clinician to estimate lung recruitability [35]. This technique has been used intraoperatively to individualize ventilator settings such as PEEP and VT [36,37,38,39], and in the postoperatively to assess the distribution of ventilation and to identify atelectatic regions [40, 41]. A recent meta-analysis of randomized-controlled trials (RCTs) [42] compared the effect of using EIT or Pes to guide individualized PEEP compared to standard monitoring, so it showed an improvement in intraoperative oxygenation. However, EIT is mostly used for research purposes and there are certain limitations to its routine roll both perioperatively and in critically ill patients [9, 37, 43]. For instance, its resolution is lower than that of other imaging techniques, such as computed tomography [37]. Moreover, incorrect placement of the electrodes can modify the image, affecting its intrapatient reproducibility [44]. Also, it should not be used in patients with pacemakers or automatic defibrillators due to possible interference with such devices [37].
Oesophageal Manometry
During mechanical ventilation, the peak pressure (Ppeak) is the force applied to overcome the airways resistance and inflate the lungs [45]. By setting a brief pause during inspiration, ventilators measure the plateau pressure (Pplat), which helps differentiate the lung’s elasticity from the airway resistance. Thus, Pplat indicates the elasticity of the lung, and the difference with Ppeak is due to airway resistance. The driving pressure (ΔP) that pushes each breath’s VT is the difference between Pplat and the set positive end-expiratory pressure (PEEP) or the intrinsic PEEP if it does exist [45]. The ratio of VT to ΔP indicates the lung’s compliance (C), or its ability to expand, which is the opposite of elastance [45]. Furthermore, lung strain is defined as the lung tissue stretch during each breath and is calculated by comparing the VT per ideal body weight to the end-expiratory lung volume (EELV), largely determined by PEEP [46].
The respiratory system consists of two main parts: the lung component, where elastic fibers help in breathing out, and the chest wall component, which expands during inhalation due to muscular action, creating a negative pressure during spontaneous breathing that stretches the lungs [47]. In anaesthetized patients, the chest wall does not expand, leading to a generally positive pleural pressure (Ppl), and an increased chest wall elastance (Ecw) [48, 49]. Ppl is the external force on the lungs that can cause them to collapse, and by measuring it, we can differentiate between the lung and chest wall components of the respiratory system [47, 48, 50, 51]. This distinction allows us to calculate the Ptp, the real pressure that distends the alveoli [50, 52,53,54]. Changes in Ptp on each ventilation generate lung stress [46, 55]. Negative end-expiratory Ptp can lead to lung collapse [56], while excessively high end-inspiratory Ptp increases the risk of ventilator-induced lung injury (VILI) [53]. It is usually recommended to keep Ptp below 15 cmH2O in healthy lungs and up to 12 cmH2O in pathological lungs [10].
Measurement of end-expiratory Pes as a surrogate for end-expiratory Ppl is useful in determining the level of PEEP required to achieve positive end-expiratory Ptp. When Ptp falls below atmospheric pressure at the end of expiration, the lung units may collapse [10, 46]. End-inspiratory Ptp measurement can discern whether an apparently high Pplat is safe [46].
Pes monitoring faces specific challenges that limit its routine implementation in clinical practice [57]. The primary challenge is that it requires a significant amount of technical skill and knowledge for accurate interpretation [43, 53]. Furthermore, it does not provide information on regional stress or strain but global stress and does not allow for an adequate source of data in heterogeneous lungs [58]. The oesophageal balloon is positioned at a specific point in the mid-lower third of the intrathoracic esophagus, and measurements taken may not correspond to the real Ppl at distant points in both dependent and non-dependent lung regions [59]. The relevance of using a calibrated oesophageal balloon method has recently been published [60], thus Pes gets a more accurate estimation of absolute values and respiratory changes in Ppl. Indeed, the traditional uncalibrated approach can be unreliable in this setting, since artifacts related to the oesophageal wall or the balloon can misguide mechanical ventilation [60]. Pes monitoring may be also misinterpreted and misguide a ventilatory strategy if spontaneous inspiratory stimulus is present [43].
In conclusion, Pes measurement can be useful in conditions characterized by an increase in chest wall elastance that compromise ventilatory mechanics [43] such as obesity or elevated intraabdominal pressure (IAP), including scenarios like pneumoperitoneum with the Trendelemburg position.
Lung Ultrasound
Lung ultrasound (LUS) is a non-invasive, radiation-free method used to evaluate lung mechanics that enables bedside assessment of pulmonary recruitment [61, 62]. It is based on the varying balances of gas and fluid within the lung parenchyma. Accordingly, three patterns are identified: Pattern A indicates predominant aeration, Pattern B suggests the presence of fluid, and Pattern C occurs when the lung parenchyma is dense, indicating consolidation or collapse [62, 63]. In healthy lungs subjected to mechanical ventilation, this technique aims to differentiate between the amount of aeration and alveolar collapse after analysing all the lung fields, thus assessing recruitability [64] and guiding pulmonary recruitment [61]. LUS not only analyses the lung parenchyma but also assesses with high diagnostic accuracy the presence of other pleural contents, i.e., pleural effusion, or the absence of inter-pleural motion, i.e., pneumothorax, apnoea, selective intubation [63, 65]. The practice of LUS for the diagnosis of pneumothorax has become the method of choice among physicians who can perform bedside LUS [66].
LUS can help to identify lung atelectasis [11] whereas predicting lung overdistension is currently the focus of research [61, 67]. Several recent studies in intraoperative and critical care settings use LUS to guide mechanical ventilation, identifying the best PEEP level, showing better oxygenation, ventilatory mechanics, and less PPCs [68,69,70,71,72]. LUS main drawback is its operator dependency [73].
Enhanced vigilance and tailored care are imperative for patients transferred from the emergency department to the operating room. The use of US in this context is quite widespread, even for the detection of a full stomach [74, 75]. In the initial management of a polytrauma patient, US assessment protocols are successful identifying major alterations, not only respiratory but also abdominal effusion or cardiac disorders [65, 76]. However, some of these alterations may go unnoticed in the initial assessment, or may be minimal at that time. It should be noted that in the event of a major change in the ventilatory mechanics of a trauma patient, US can detect pneumothoraxes that have been exacerbated by prolonged mechanical ventilation and surgeries. In addition, they can also detect pleural effusions, haemothoraces and consolidations [63].
Diaphragm Ultrasound
Ultrasound evaluation of the diaphragm is a non-invasive tool that allows us to assess the functionality of this muscle at the bedside [77, 78]. Within the perioperative setting of major surgeries a decreased inspiratory diaphragmatic dome excursion has been validated as an index of diaphragmatic dysfunction, as it is related to increased PPCs. In critically ill patients, diaphragmatic ultrasound (DUS) plays an established role in the assessment of diaphragmatic function and movement in weaning from mechanical ventilation and to guide rehabilitation in critically ill patients.
Within locoregional anaesthesia, brachial and cervical plexus blocks are standard procedures and the phrenic nerve may be blocked during these techniques. The clinical impact of blocking this nerve depends significantly on patient-specific, for example, existing phrenic nerve paralysis on the opposite side or obesity [79, 80]. During the procedure ipsilateral phrenic nerve palsy may go unnoticed. However, either in the hospital [81] or at home due to early discharge, these patients may develop severe PPCs due to unilateral diaphragmatic paralysis. DUS can help us for an early detection of the absence of diaphragmatic contraction [82]. DUS has been used to classify hemidiaphragmatic paresis into 3 grades (none, partial and complete) following cervical plexus blocks [83]. Thickness index of the diaphragm muscle (inspiratory thickness/expiratory thickness) obtained by US can be used in clinical practice to assess diaphragmatic paresis. This index has a 90% correlation with a reduction in FVC or FEV1 equal to or greater than 20% in spirometry [84].
Table 1 shows recent clinical studies that have used advanced respiratory monitoring in the perioperative setting.
Clinical Settings
Laparoscopic and Robotic Surgery
Laparoscopic and robotic approaches are now standard procedures in hospitals for many surgical interventions [85, 86]. During laparoscopy carbon dioxide (CO2) insufflation creates an artificial space known as a pneumoperitoneum [87,88,89]. This procedure increases IAP, which in turn raises Ppl and can cause lung collapse [90, 91]. This reduces the respiratory system compliance (CRS), hampering positive pressure ventilation. Alveolar overdistension, atelectrauma and atelectasis can coexist in laparoscopic surgeries generating heterogeneity in regional ventilation distribution (Fig. 1) [90,91,92]. Moreover, steep Trendelenburg i.e. head-down, and anti-Trendelenburg, i.e., head-up, positions, are commonly used in laparoscopic and robotic surgeries to enhance surgeon visibility and access to the abdominal or pelvic areas [93, 94]. While the anti-Trendelenburg position aids in shifting the diaphragm downward to improve breathing mechanics, the Trendelenburg position compounds on respiratory challenge posed by the pneumoperitoenum, particularly in patients with pre-existing conditions like obesity or chest wall stiffness [93]. Several studies have demonstrated the detrimental effect of the combination of Trendelemburg and pneumoperitoneum on ventilatory mechanics [95, 96].
This figure presents a schematic diagram of cross-sectional views of lung fields from the same patient, illustrating the heterogeneity in regional ventilation distribution that can occur during laparoscopic surgeries. This heterogeneity is exacerbated under Trendelenburg positioning or obesity. The color coding represents alveolar ventilation, with lighter shades indicating less ventilation and darker shades indicating more ventilation. A: Cross-section of basal segments, where the alveoli are collapsed during both inspiration and expiration, indicating atelectasis. B: Cross-section of mid-lung segments. In addition to atelectasis, this section also shows, as highlighted in the enlargement, overdistended alveoli during inspiration and airway collapse during expiration, which prevents proper emptying. This condition can be explained by expiratory flow limitation mechanism. C: Cross-section of apical segments. The enlargement illustrates a phenomenon where alveoli are ventilated during inspiration but collapse during expiration. This is known as tidal recruitment
A multicentre observational study analysed the incidence of PPCs after abdominal robotic surgery, finding an overall incidence of 19%. They used the Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT) score and found that patients at high risk according to this score had 22.4% of PPCs compared to 12.7% of patients with a low score [97]. Indeed, when IAP is high or accompanied by additional factors such as comorbidities, positioning, or surgical manipulation, the incidence of PPCs increases [98, 99]. For the same positive inspiratory pressure, as Ppl increases, Ptp decreases and becomes negative, so mechanically caused atelectasis becomes more abundant [99,100,101]. We are unable to accurately estimate Ptp in these patients using ventilator data and airway pressure measurements alone [56, 102]. Therefore, individualization of the protective lung ventilation strategy is one of the most studied areas in this field, and advanced respiratory monitoring is common in these research studies [66,67,68, 78, 103].
Pes monitoring is a key tool for measuring Ppl and Ptp, which is crucial for tailoring lung protective ventilation strategies during laparoscopic or robotic surgeries [56, 102]. Its utility arises because the increased intra-abdominal pressures from pneumoperitoneum do not uniformly affect Ppl [104, 105]. This monitoring allows for continuous customization of alveolar distension pressures and PEEP, helping prevent atelectasis and shunt phenomena [102, 106, 107]. While Pes monitoring has been effectively used in various clinical studies to determine the optimal PEEP for preventing alveolar collapse, evidence showing improvements in patient-centered outcomes like postoperative pulmonary complications (PPCs) is still lacking. Nevertheless, several studies have documented benefits such as better intraoperative oxygenation [108] and improved ventilatory mechanics with reduced transpulmonary driving pressures [102, 109,110,111].
EIT can theoretically avoid two frequent issues during mechanical ventilation in the presence of pneumoperitoneum: atelectrauma and regional overdistension [90, 91, 112]. It has mainly been used to calculate the best PEEP. A recent RCT has shown that EIT-guided PEEP in laparoscopic surgery improves PPCs, ventilatory mechanics, and intraoperative oxygenation compared to standard PEEP [103]. However, in 2016 another RCT had non-statistically significant results in terms of intraoperative oxygenation and reduction of CPP. In the latter case, they compared EIT-guided PEEP with ideal compliance-guided PEEP [113]. Several articles have demonstrated the value of EIT in improving ventilatory mechanics and intraoperative oxygenation during robotic [114, 115] and laparoscopic procedures [103]. Both EIT and Pes have been shown to be superior to non-advanced monitoring in oxygenation measured by PaO2/FiO2 in the intraoperative setting [42].
Given the high incidence of alveolar collapse in these patients and the widespread availability of LUS, there is a growing focus on using this tool to customize intraoperative ventilation during laparoscopic procedures [68, 69]. The randomised clinical trials performed so far demonstrate improved PPCs and clinical outcomes with the use of LUS to guide mechanical ventilation and PEEP compared to conventional management in the laparoscopic approach [68,69,70, 116]. Only one randomized clinical trial showed improvement in ventilatory mechanics and oxygenation without a reduction in PPCs [117]. A recent systematic review with meta-analysis on the use of LUS to guide intraoperative mechanical ventilation in non-cardiac surgery [71] found beneficial effects on intra- and postoperative atelectasis when using LUS versus conventional management. They selected a total of 9 randomised clinical trials including paediatric and adult patients, in open and laparoscopic surgery.
To date, the main focus of research using these advanced monitoring tools in laparoscopy has been on atelectasis, regional ventilation, recruitment and PEEP. There are no clinical studies, to our knowledge, using these tools to assess other challenges of mechanical ventilation in laparoscopy such as its relevance on expiratory flow limitation or mechanical power (MP). The mechanical power concept emerges from the analysis of the modifiable variables of positive pressure ventilation to estimate how much energy the ventilator delivers to the respiratory system per minute [118]. Then, MP analyses the elastic-static forces, i.e. PEEP, the elastic-dynamic forces, i.e. ΔP and VT, and the resistive forces, i.e. the airway flow and resistance or RR [119]. MP acts on lung parenchyma, deforming the epithelial and endothelial cells anchored to it [120]. High MP is associated with a higher rate of PPCs [121, 122]. MP has been shown to be higher in one-lung ventilation (OLV) during thoracic surgery [123], during pneumoperitoneum, in the trendelemburg position and in obese patients [109]. To the best of our knowledge, only one study has been published in a perioperative setting analysing the impact on mechanical power of a ventilatory strategy based on advanced respiratory monitoring [124]. In this study, Crs-guided PEEP achieved lower values of MP than transpulmonary ΔP-guided PEEP. In critically ill patients, it has been studied whether EIT-guided mechanical ventilation can reduce MP [125]. More research is needed on this very recent outcome related to PPCs.
Thoracic Surgery
The key challenge during thoracic surgery reside in oxygenating and ventilating the dependent lung without causing harm [7]. By a double-lumen endotracheal tube (DLT) or Bronchial Blockers (BB) we isolate and collapse the operated lung. By ventilating the dependent lung with a DLT or BB through a relatively thin and long lumen, we can generate autoPEEP, which may be harmful [126]. Furthermore, setting VT and PEEP OLV is complex. High VT increases VILI risk, whereas low VT promote the development of atelectasis. Additionally, while increasing PEEP can help prevent collapse, it may also cause regional overdistension and increase alveolar dead space [127]. Current evidence suggests that protective ventilation strategy combining low VT and increased PEEP, i.e., 10 cmH2O or individualized PEEP, improves ventilatory mechanics and PaO2 without impairing neither ventilation/perfusion ratio nor hemodynamics [39, 128]. EIT has proven to be useful in several tasks in these procedures. Essentially, EIT has allowed titration of VT during one lung ventilation (OLV), based on ventilation distribution and oxygenation [38], and it has also been used to individualize PEEP to achieve better ventilatory mechanics and intraoperative oxygenation [38, 129]. Indeed it is also useful in detecting correct OLV for double-lumen tube by detecting pulmonary regional ventilation [130].
Furthermore, a matter of concern in thoracic surgery, as well as in any surgical procedure that might impact the phrenic nerve, is maintaining proper diaphragmatic function. DUS has been shown to be useful in assessing hemidiaphragmatic paralysis after thoracic surgery, which is associated with PPCs [12].
Obese Patients
This is a common comorbidity that hinders mechanical ventilation [131]. In particular, one of the challenges is to find out what is the real pressure generated by excess weight on Ppl in our patients [132]. It can be challenging to maintain lung protection parameters without accurately estimating the Ptp we are generating. In obesity, as in other restrictive pathologies such as scoliosis, chest wall compliance is lower than lung compliance, which means that airway pressures are easily transferred to other intrathoracic structures (e.g. large vessels and pericardium) [133,134,135]. Of course, these patients need positive pressure values capable of counteracting this increase in pleural pressure, and the sum of all these factors makes the proper management of these patients so complex [136, 137].
Pes monitoring, which allows the partitioning of the respiratory mechanics, is the unique way to assess the real alveolar distension pressures of these patients with reduced chest compliance [138]. Only then the clinician will be able to manage adequate transpulmonary pressures (as in laparoscopy) and to individualize the lung protection values [110]. Pes has been used in several clinical studies in obese patients on mechanical ventilation. By establishing a Pes-guided ventilatory strategy in obese patients, improvements in ventilatory mechanics (partitioning of ventilatory mechanics by observing improvements in lung strain and lung elastance) [107] and oxygenation [139] have been demonstrated.
EIT has a role to play both intra-operatively [140] and in the postoperative context as a non-invasive tool [41]. Intraoperatively, EIT-guided mechanical ventilation with MRI and individualized PEEP has been shown to improve ventilatory mechanics and oxygenation parameters, but has not been shown to maintain these improvements postoperatively [140]. EIT allows breath-by-breath monitoring after extubation to monitor the dyshomeogenisation of spontaneous lung ventilation, thus allowing early detection of patients who are candidates for ventilatory support and indicating the response to the applied therapy [141].
The only advanced monitoring technique that does achieve evidence support for PPCs reduction in these patients is LUS. A randomized clinical trial has used it intraoperatively in bariatric surgery to guide individualized PEEP, achieving a reduction in PPCs as well as improved clinical outcomes compared to standard PEEP strategy [69].
Obese patients are potentially one of the groups that can benefit the most from advanced monitoring, but more clinical studies are required to really prove whether the intraoperative use of these techniques has advantages for them in patient-centred outcomes [142].
Conclusions and Future Directions
Advanced respiratory monitoring tools offer both advantages and limitations: EIT effectively individualizes PEEP titration and assesses regional ventilation, although its lower resolution and dependency on correct electrode placement limit its routine clinical use. Pes helps tailor lung protective ventilation by measuring transpulmonary pressure (Ptp), which is crucial in conditions with increased chest wall elastance, despite its technical complexity and limitations in regional stress assessment. LUS aids in identifying lung atelectasis and guiding mechanical ventilation adjustments, although operator dependency remains a drawback. DUS is useful for assessing diaphragmatic function and detecting diaphragmatic paralysis, which is associated with PPCs.
Despite the theoretical benefits of advanced respiratory monitoring technologies, there is currently a lack of clinical studies that demonstrate a clear improvement in patient-centered outcomes with these methods. To address this gap, there is a pressing need for randomized clinical trials. Such studies would help determine whether patients at higher risk, particularly those undergoing procedures involving pneumoperitoneum and those who are obese, would benefit from the use of advanced respiratory monitoring technologies. Focusing research on these groups could provide valuable insights into optimizing ventilation strategies to enhance patient safety and outcomes.
Key References
-
Esposito T, Fregonese M, Morettini G, Carboni P, Tardioli C, Messina A, et al. Intraoperative individualization of positive-end-expiratory pressure through electrical impedance tomography or esophageal pressure assessment: a systematic review and meta-analysis of randomized controlled trials. J Clin Monit Comput. 2024 Feb;38(1):89–100.
-
This systematic review and meta-analysis of RCTs compared the effects of PEEP individualized by EIT or esophageal pressure vs. non-individualized PEEP on intraoperative PaO2/FiO2 ratios in abdominal or pelvic surgeries. Six RCTs (240 patients) showed better intraoperative oxygenation in the intervention group, with reduced heterogeneity after adjusting for BMI.
-
-
Tharp WG, Neilson MR, Breidenstein MW, Harned RG, Chatfield SE, Friend AF, et al. Effects of obesity, pneumoperitoneum, and body position on mechanical power of intraoperative ventilation: an observational study. J Appl Physiol Bethesda Md 1985. 2023 Jun 1;134(6):1390–402.
-
This study investigated the impact of obesity, pneumoperitoneum, and body position on mechanical power during robotic-assisted laparoscopic surgery. Using esophageal manometry, the study found that obesity and specific surgical positions significantly altered ventilation bioenergetics.
-
Data Availability
No datasets were generated or analysed during the current study.
References
Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017;118(3):317–34.
Smetana GW, Lawrence VA, Cornell JE, American College of Physicians. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006;144(8):581–95.
Güldner A, Kiss T, Serpa Neto A, Hemmes SNT, Canet J, Spieth PM, et al. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015;123(3):692–713.
Deng QW, Tan WC, Zhao BC, Wen SH, Shen JT, Xu M. Intraoperative ventilation strategies to prevent postoperative pulmonary complications: a network meta-analysis of randomised controlled trials. Br J Anaesth. 2020;124(3):324–35.
Neto AS, Hemmes SNT, Barbas CSV, Beiderlinden M, Fernandez-Bustamante A, Futier E, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med. 2016;4(4):272–80.
Park SJ, Kim BG, Oh AH, Han SH, Han HS, Ryu JH. Effects of intraoperative protective lung ventilation on postoperative pulmonary complications in patients with laparoscopic surgery: prospective, randomized and controlled trial. Surg Endosc. 2016;30(10):4598–606.
Park M, Ahn HJ, Kim JA, Yang M, Heo BY, Choi JW, et al. Driving pressure during thoracic surgery: a randomized clinical trial. Anesthesiology. 2019;130(3):385–93.
Writing Committee for the PROBESE Collaborative Group of the PROtective VEntilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology, Bluth T, Serpa Neto A, Schultz MJ, Pelosi P, Gama de Abreu M, et al. Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low PEEP on postoperative pulmonary complications in obese patients: a randomized clinical trial. JAMA. 2019;321(23):2292–305.
Walsh BK, Smallwood CD. Electrical impedance tomography during mechanical ventilation. Respir Care. 2016;61(10):1417–24.
Mauri T, Yoshida T, Bellani G, Goligher EC, Carteaux G, Rittayamai N, et al. Esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med. 2016;42(9):1360–73.
Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9–15.
Spadaro S, Grasso S, Dres M, Fogagnolo A, Dalla Corte F, Tamburini N, et al. Point of care ultrasound to identify diaphragmatic dysfunction after thoracic surgery. Anesthesiology. 2019;131(2):266–78.
Mojoli F, Pozzi M, Arisi E. Setting positive end-expiratory pressure: using the pressure-volume curve. Curr Opin Crit Care. 2024;30(1):35–42.
Hess DR. Respiratory mechanics in mechanically ventilated patients. Respir Care. 2014;59(11):1773–94.
Mojoli F, Pozzi M, Arisi E, Mongodi S, Orlando A, Maggio G, et al. Tidal lung hysteresis to interpret PEEP-induced changes in compliance in ARDS patients. Crit Care. 2023;27(1):233.
Chiumello D, Arnal JM, Umbrello M, Cammaroto A, Formenti P, Mistraletti G, et al. Hysteresis and lung recruitment in acute respiratory distress syndrome patients: a CT scan study. Crit Care Med. 2020;48(10):1494–502.
Grasso S, Terragni P, Mascia L, Fanelli V, Quintel M, Herrmann P, et al. Airway pressure-time curve profile (stress index) detects tidal recruitment/hyperinflation in experimental acute lung injury. Crit Care Med. 2004;32(4):1018–27.
Terragni PP, Filippini C, Slutsky AS, Birocco A, Tenaglia T, Grasso S, et al. Accuracy of plateau pressure and stress index to identify injurious ventilation in patients with acute respiratory distress syndrome. Anesthesiology. 2013;119(4):880–9.
Terragni P, Bussone G, Mascia L. Dynamic airway pressure-time curve profile (Stress Index): a systematic review. Minerva Anestesiol. 2016;82(1):58–68.
Tusman G, Groisman I, Fiolo FE, Scandurra A, Arca JM, Krumrick G, et al. Noninvasive monitoring of lung recruitment maneuvers in morbidly obese patients: the role of pulse oximetry and volumetric capnography. Anesth Analg. 2014;118(1):137–44.
Ferluga M, Lucangelo U, Blanch L. Dead space in acute respiratory distress syndrome. Ann Transl Med. 2018;6(19):388.
Tusman G, Wallin M, Acosta C, Santanera B, Portela F, Viotti F, et al. Positive end-expiratory pressure individualization guided by continuous end-expiratory lung volume monitoring during laparoscopic surgery. J Clin Monit Comput. 2022;36(5):1557–67.
Chiumello D, Cressoni M, Chierichetti M, Tallarini F, Botticelli M, Berto V, et al. Nitrogen washout/washin, helium dilution and computed tomography in the assessment of end expiratory lung volume. Crit Care Lond Engl. 2008;12(6):R150.
Olegård C, Söndergaard S, Houltz E, Lundin S, Stenqvist O. Estimation of functional residual capacity at the bedside using standard monitoring equipment: a modified nitrogen washout/washin technique requiring a small change of the inspired oxygen fraction. Anesth Analg. 2005;101(1):206–12 table of contents.
Grieco DL, Anzellotti GM, Russo A, Bongiovanni F, Costantini B, D’Indinosante M, et al. Airway closure during surgical pneumoperitoneum in obese patients. Anesthesiology. 2019;131(1):58–73.
Grieco DL, Russo A, Romanò B, Anzellotti GM, Ciocchetti P, Torrini F, et al. Lung volumes, respiratory mechanics and dynamic strain during general anaesthesia. Br J Anaesth. 2018;121(5):1156–65.
Spadaro S, Caramori G, Rizzuto C, Mojoli F, Zani G, Ragazzi R, et al. Expiratory flow limitation as a risk factor for pulmonary complications after major abdominal surgery. Anesth Analg. 2017;124(2):524–30.
Fogagnolo A, Spadaro S, Karbing DS, Scaramuzzo G, Mari M, Guirrini S, et al. Effect of expiratory flow limitation on ventilation/perfusion mismatch and perioperative lung function during pneumoperitoneum and Trendelenburg position. Minerva Anestesiol. 2023;89(9):733–43.
Ferrando C, Suárez-Sipmann F, Librero J, Pozo N, Soro M, Unzueta C, et al. A noninvasive postoperative clinical score to identify patients at risk for postoperative pulmonary complications: the Air-Test Score. Minerva Anestesiol. 2020;86(4):404–15. https://doi.org/10.23736/S0375-9393.19.13932-6.
Chen L, Del Sorbo L, Grieco DL, Junhasavasdikul D, Rittayamai N, Soliman I, et al. Potential for lung recruitment estimated by the recruitment-to-inflation ratio in acute respiratory distress syndrome. A clinical trial. Am J Respir Crit Care Med. 2020;201(2):178–87.
Myatra SN, Prabu NR, Divatia JV, Monnet X, Kulkarni AP, Teboul JL. The changes in pulse pressure variation or stroke volume variation after a “tidal volume challenge” reliably predict fluid responsiveness during low tidal volume ventilation*. Crit Care Med. 2017;45(3):415–21.
Lai C, Shi R, Beurton A, Moretto F, Ayed S, Fage N, et al. The increase in cardiac output induced by a decrease in positive end-expiratory pressure reliably detects volume responsiveness: the PEEP-test study. Crit Care. 2023;27(1):136.
Frerichs I, Hinz J, Herrmann P, Weisser G, Hahn G, Dudykevych T, et al. Detection of local lung air content by electrical impedance tomography compared with electron beam CT. J Appl Physiol Bethesda Md 1985. 2002;93(2):660–6.
Bodenstein M, David M, Markstaller K. Principles of electrical impedance tomography and its clinical application. Crit Care Med. 2009;37(2):713–24.
Spadaro S, Mauri T, Böhm SH, Scaramuzzo G, Turrini C, Waldmann AD, et al. Variation of poorly ventilated lung units (silent spaces) measured by electrical impedance tomography to dynamically assess recruitment. Crit Care. 2018;22(1):26.
Ukere A, März A, Wodack KH, Trepte CJ, Haese A, Waldmann AD, et al. Perioperative assessment of regional ventilation during changing body positions and ventilation conditions by electrical impedance tomography. Br J Anaesth. 2016;117(2):228–35.
Spinelli E, Mauri T, Fogagnolo A, Scaramuzzo G, Rundo A, Grieco DL, et al. Electrical impedance tomography in perioperative medicine: careful respiratory monitoring for tailored interventions. BMC Anesthesiol. 2019;19(1):140.
Zhao Z, Wang W, Zhang Z, Xu M, Frerichs I, Wu J, et al. Influence of tidal volume and positive end-expiratory pressure on ventilation distribution and oxygenation during one-lung ventilation. Physiol Meas. 2018;39(3):034003.
Spadaro S, Grasso S, Karbing DS, Fogagnolo A, Contoli M, Bollini G, et al. Physiologic evaluation of ventilation perfusion mismatch and respiratory mechanics at different positive end-expiratory pressure in patients undergoing protective one-lung ventilation. Anesthesiology. 2018;128(3):531–8.
Rauseo M, Spinelli E, Sella N, Slobod D, Spadaro S, Longhini F, et al. Expert opinion document: ‘Electrical impedance tomography: applications from the intensive care unit and beyond.’ J Anesth Analg Crit Care. 2022;2(1):28.
Schaefer MS, Wania V, Bastin B, Schmalz U, Kienbaum P, Beiderlinden M, et al. Electrical impedance tomography during major open upper abdominal surgery: a pilot-study. BMC Anesthesiol. 2014;14:51.
Esposito T, Fregonese M, Morettini G, Carboni P, Tardioli C, Messina A, et al. Intraoperative individualization of positive-end-expiratory pressure through electrical impedance tomography or esophageal pressure assessment: a systematic review and meta-analysis of randomized controlled trials. J Clin Monit Comput. 2024;38(1):89–100.
Cammarota G, Simonte R, Longhini F, Spadaro S, Vetrugno L, De Robertis E. Advanced point-of-care bedside monitoring for acute respiratory failure. Anesthesiology. 2023;138(3):317–34.
Zhang F, Li C, Zhang Jn, Guo Hp, Wu Dw. Comparison of quantitative computed tomography analysis and single-indicator thermodilution to measure pulmonary edema in patients with acute respiratory distress syndrome. Biomed Eng Online. 2014;13:30.
Walter JM, Corbridge TC, Singer BD. Invasive mechanical ventilation. South Med J. 2018;111(12):746–53.
Chiumello D, Carlesso E, Cadringher P, Caironi P, Valenza F, Polli F, et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med. 2008;178(4):346–55.
Baydur A, Sassoon CS, Stiles CM. Partitioning of respiratory mechanics in young adults. Effects of duration of anesthesia. Am Rev Respir Dis. 1987;135(1):165–72.
Agostoni E. Mechanics of the pleural space. Physiol Rev. 1972;52(1):57–128.
Behazin N, Jones SB, Cohen RI, Loring SH. Respiratory restriction and elevated pleural and esophageal pressures in morbid obesity. J Appl Physiol. 2010;108(1):212–8.
Jonkman AH, Telias I, Spinelli E, Akoumianaki E, Piquilloud L. The oesophageal balloon for respiratory monitoring in ventilated patients: updated clinical review and practical aspects. Eur Respir Rev Off J Eur Respir Soc. 2023;32(168):220186.
Zin WA, Pengelly LD, Milic-Emili J. Partitioning of respiratory mechanics in anesthetized cats. J Appl Physiol. 1983;54(3):708–13.
Talmor D, Sarge T, O’Donnell CR, Ritz R, Malhotra A, Lisbon A, et al. Esophageal and transpulmonary pressures in acute respiratory failure. Crit Care Med. 2006;34(5):1389–94.
Gattinoni L, Giosa L, Bonifazi M, Pasticci I, Busana M, Macri M, et al. Targeting transpulmonary pressure to prevent ventilator-induced lung injury. Expert Rev Respir Med. 2019;13(8):737–46.
Williams EC, Motta-Ribeiro GC, Vidal Melo MF. Driving pressure and transpulmonary pressure: how do we guide safe mechanical ventilation? Anesthesiology. 2019;131(1):155–63.
Protti A, Andreis DT, Monti M, Santini A, Sparacino CC, Langer T, et al. Lung stress and strain during mechanical ventilation: any difference between statics and dynamics? Crit Care Med. 2013;41(4):1046–55.
Cinnella G, Grasso S, Spadaro S, Rauseo M, Mirabella L, Salatto P, et al. Effects of recruitment maneuver and positive end-expiratory pressure on respiratory mechanics and transpulmonary pressure during laparoscopic surgery. Anesthesiology. 2013;118(1):114–22.
Placenti A, Fratebianchi F. Interpretation and use of intraoperative protective ventilation parameters: a scoping review. Anaesthesiol Intensive Ther. 2022;54(4):320–33.
Goligher EC, Jonkman AH, Dianti J, Vaporidi K, Beitler JR, Patel BK, et al. Clinical strategies for implementing lung and diaphragm-protective ventilation: avoiding insufficient and excessive effort. Intensive Care Med. 2020;46(12):2314–26.
Mongodi S, De Luca D, Colombo A, Stella A, Santangelo E, Corradi F, et al. Quantitative lung ultrasound: technical aspects and clinical applications. Anesthesiology. 2021;134(6):949–65.
Cammarota G, Lauro G, Santangelo E, Sguazzotti I, Perucca R, Verdina F, et al. Mechanical ventilation guided by uncalibrated esophageal pressure may be potentially harmful. Anesthesiology. 2020;133(1):145–53.
Tang KQ, Yang SL, Zhang B, Liu HX, Ye DY, Zhang HZ, et al. Ultrasonic monitoring in the assessment of pulmonary recruitment and the best positive end-expiratory pressure. Medicine (Baltimore). 2017;96(39):e8168.
Mojoli F, Bouhemad B, Mongodi S, Lichtenstein D. Lung ultrasound for critically ill patients. Am J Respir Crit Care Med. 2019;199(6):701–14.
Mayo PH, Copetti R, Feller-Kopman D, Mathis G, Maury E, Mongodi S, et al. Thoracic ultrasonography: a narrative review. Intensive Care Med. 2019;45(9):1200–11.
Gattinoni L, Collino F, Camporota L. Assessing lung recruitability: does it help with PEEP settings? Intensive Care Med. 2024;50(5):749–51. https://doi.org/10.1007/s00134-024-07351-5.
Lichtenstein DA. BLUE-protocol and FALLS-protocol. Chest. 2015;147(6):1659–70.
Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest. 2011;140(4):859–66.
Tonelotto B, Pereira SM, Tucci MR, Vaz DF, Vieira JE, Malbouisson LM, et al. Intraoperative pulmonary hyperdistention estimated by transthoracic lung ultrasound: A pilot study. Anaesth Crit Care Pain Med. 2020;39(6):825–31.
Wu Xz, Xia Hm, Zhang P, Li L, Hu Qh, Guo Sp, et al. Effects of ultrasound-guided alveolar recruitment manoeuvres compared with sustained inflation or no recruitment manoeuvres on atelectasis in laparoscopic gynaecological surgery as assessed by ultrasonography: a randomized clinical trial. BMC Anesthesiol. 2022;22(1):261.
Elshazly M, Khair T, Bassem M, Mansour M. The use of intraoperative bedside lung ultrasound in optimizing positive end expiratory pressure in obese patients undergoing laparoscopic bariatric surgeries. Surg Obes Relat Dis. 2021;17(2):372–8.
Liu Y, Wang J, Geng Y, Zhang Y, Su H, Yang Y. The effect of ultrasound-guided lung recruitment maneuvers on atelectasis in lung-healthy patients undergoing laparoscopic gynecologic surgery: a randomized controlled trial. BMC Anesthesiol. 2022;22(1):200.
Liao B, Liao W, Yin S, Liu S, Wu X. Effect of ultrasound-guided lung recruitment to reduce pulmonary atelectasis after non-cardiac surgery under general anesthesia: a systematic review and meta-analysis of randomized controlled trials. Perioper Med. 2024;13(1):23.
Mousa A, Klompmaker P, Tuinman PR. Setting positive end-expiratory pressure: lung and diaphragm ultrasound. Curr Opin Crit Care. 2024;30(1):53–60.
Díaz-Gómez JL, Renew JR, Ratzlaff RA, Ramakrishna H, Via G, Torp K. Can lung ultrasound be the first-line tool for evaluation of intraoperative hypoxemia? Anesth Analg. 2018;126(5):1769–73.
Van de Putte P, Perlas A. Ultrasound assessment of gastric content and volume. Br J Anaesth. 2014;113(1):12–22.
Schwarz SKW, Prabhakar C. What to do when perioperative point-of-care ultrasound shows evidence of a full stomach despite fasting? Can J Anaesth J Can Anesth. 2020;67(7):798–805.
Whitson MR, Mayo PH. Ultrasonography in the emergency department. Crit Care Lond Engl. 2016;20(1):227.
Kim WY, Suh HJ, Hong SB, Koh Y, Lim CM. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med. 2011;39(12):2627–30.
Zambon M, Greco M, Bocchino S, Cabrini L, Beccaria PF, Zangrillo A. Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review. Intensive Care Med. 2017;43(1):29–38.
Kim DH, Lin Y, Beathe JC, Liu J, Oxendine JA, Haskins SC, et al. Superior trunk block: a phrenic-sparing alternative to the interscalene block: a randomized controlled trial. Anesthesiology. 2019;131(3):521–33.
Bao X, Huang J, Feng H, Qian Y, Wang Y, Zhang Q, et al. Effect of local anesthetic volume (20 mL vs 30 mL ropivacaine) on electromyography of the diaphragm and pulmonary function after ultrasound-guided supraclavicular brachial plexus block: a randomized controlled trial. Reg Anesth Pain Med. 2019;44(1):69–75.
Berg AA, Flaherty JM, Habeck JM, Harrison AK, Braman JP, Kaizer AM, et al. Evaluation of diaphragmatic function after interscalene block with liposomal bupivacaine: a randomized controlled trial. Anesthesiology. 2022;136(4):531–41.
Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg. 1991;72(4):498–503.
Kim HY, Soh EY, Lee J, Kwon SH, Hur M, Min SK, et al. Incidence of hemi-diaphragmatic paresis after ultrasound-guided intermediate cervical plexus block: a prospective observational study. J Anesth. 2020;34(4):483–90.
López Escárraga VM, Dubos España K, Castillo Bustos RH, Peidró L, Sastre S, Sala-Blanch X. Diaphragmatic thickness ratio (inspiratory/expiratory) as a diagnostic method of diaphragmatic palsy associated with interescalene block. Rev Esp Anestesiol Reanim. 2018;65(2):81–9.
Mazzinari G, Albers-Warlé KI, Rovira L, Warlé MC, Diaz Cambronero O, Navarro MPA. The why and how of the minimally invasive pneumoperitoneum in present-day laparoscopic surgery. Am J Surg. 2024;S0002–9610(24):00022–9.
Mazzinari G, Rovira L, Albers-Warlé KI, Warlé MC, Argente-Navarro P, Flor B, et al. Underneath images and robots, looking deeper into the pneumoperitoneum: a narrative review. J Clin Med. 2024;13(4):1080.
Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW, et al. Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg. 2018;267(2):199.
Veldkamp R, Kuhry E, Hop WCJ, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6(7):477–84.
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Meta-analysis of laparoscopic vs open cholecystectomy in elderly patients. World J Gastroenterol. 2014;20(46):17626–34.
Andersson LE, Bååth M, Thörne A, Aspelin P, Odeberg-Wernerman S. Effect of carbon dioxide pneumoperitoneum on development of atelectasis during anesthesia, examined by spiral computed tomography. Anesthesiology. 2005;102(2):293–9.
Valenza F, Chevallard G, Fossali T, Salice V, Pizzocri M, Gattinoni L. Management of mechanical ventilation during laparoscopic surgery. Best Pract Res Clin Anaesthesiol. 2010;24(2):227–41.
Hirvonen EA, Nuutinen LS, Kauko M. Ventilatory effects, blood gas changes, and oxygen consumption during laparoscopic hysterectomy. Anesth Analg. 1995;80(5):961–6.
Buonanno P, Marra A, Iacovazzo C, Merola R, De Siena AU, Servillo G, et al. Electric impedance tomography and protective mechanical ventilation in elective robotic-assisted laparoscopy surgery with steep Trendelenburg position: a randomized controlled study. Sci Rep. 2023;13(1):2753.
Shono A, Katayama N, Fujihara T, Böhm SH, Waldmann AD, Ugata K, et al. Positive end-expiratory pressure and distribution of ventilation in pneumoperitoneum combined with steep trendelenburg position. Anesthesiology. 2020;132(3):476–90.
Rubini A, Monte DD, Catena V. Effects of the pneumoperitoneum and Trendelenburg position on respiratory mechanics in the rats by the end-inflation occlusion method. Ann Thorac Med. 2012;7(4):205–9.
Sprung J, Whalley DG, Falcone T, Warner DO, Hubmayr RD, Hammel J. The impact of morbid obesity, pneumoperitoneum, and posture on respiratory system mechanics and oxygenation during laparoscopy. Anesth Analg. 2002;94(5):1345–50.
Queiroz VNF, Da Costa LGV, Takaoka F, Pelosi P, De Abreu MG, Schultz MJ, et al. Ventilation and outcomes following robotic-assisted abdominal surgery: an international, multicentre observational study. Br J Anaesth. 2021;126(2):533–43.
Lagier D, Zeng C, Fernandez-Bustamante A, Vidal Melo MF. Perioperative Pulmonary Atelectasis: Part II. Clinical Implications. Anesthesiology. 2022;136(1):206–36.
Futier E, Constantin JM, Pelosi P, Chanques G, Kwiatkoskwi F, Jaber S, et al. Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology. 2010;113(6):1310–9.
Strang CM, Hachenberg T, Fredén F, Hedenstierna G. Development of atelectasis and arterial to end-tidal Pco2-difference in a porcine model of pneumoperitoneum. Br J Anaesth. 2009;103(2):298–303.
Hedenstierna G, Tokics L, Scaramuzzo G, Rothen HU, Edmark L, Öhrvik J. Oxygenation impairment during anesthesia. Anesthesiology. 2019;131(1):46–57.
Mazzinari G, Diaz-Cambronero O, Alonso-Iñigo JM, Garcia-Gregorio N, Ayas-Montero B, Ibañez JL, et al. Intraabdominal pressure targeted positive end-expiratory pressure during laparoscopic surgery. Anesthesiology. 2020;132(4):667–77.
Ma X, Fu Y, Piao X, De Santis Santiago RR, Ma L, Guo Y, et al. Individualised positive end-expiratory pressure titrated intra-operatively by electrical impedance tomography optimises pulmonary mechanics and reduces postoperative atelectasis: A randomised controlled trial. Eur J Anaesthesiol. 2023;40(11):805–16.
Sindi A, Piraino T, Alhazzani W, Tunks M, Faden M, Ma J, et al. The correlation between esophageal and abdominal pressures in mechanically ventilated patients undergoing laparoscopic surgery. Respir Care. 2014;59(4):491–6.
Mazzinari G, Diaz-Cambronero O, Serpa Neto A, Martínez AC, Rovira L, Argente Navarro MP, et al. Modeling intra-abdominal volume and respiratory driving pressure during pneumoperitoneum insufflation-a patient-level data meta-analysis. J Appl Physiol Bethesda Md 1985. 2021;130(3):721–8.
Spadaro S, Karbing DS, Mauri T, Marangoni E, Mojoli F, Valpiani G, et al. Effect of positive end-expiratory pressure on pulmonary shunt and dynamic compliance during abdominal surgery. Br J Anaesth. 2016;116(6):855–61.
Tusman G, Acosta CM, Ochoa M, Böhm SH, Gogniat E, Martinez Arca J, et al. Multimodal non-invasive monitoring to apply an open lung approach strategy in morbidly obese patients during bariatric surgery. J Clin Monit Comput. 2020;34(5):1015–24.
Cammarota G, Lauro G, Sguazzotti I, Mariano I, Perucca R, Messina A, et al. Esophageal pressure versus gas exchange to set PEEP during intraoperative ventilation. Respir Care. 2020;65(5):625–35.
Tharp WG, Neilson MR, Breidenstein MW, Harned RG, Chatfield SE, Friend AF, et al. Effects of obesity, pneumoperitoneum, and body position on mechanical power of intraoperative ventilation: an observational study. J Appl Physiol Bethesda Md 1985. 2023;134(6):1390–402.
Eichler L, Truskowska K, Dupree A, Busch P, Goetz AE, Zöllner C. Intraoperative ventilation of morbidly obese patients guided by transpulmonary pressure. Obes Surg. 2018;28(1):122–9.
Piriyapatsom A, Phetkampang S. Effects of intra-operative positive end-expiratory pressure setting guided by oesophageal pressure measurement on oxygenation and respiratory mechanics during laparoscopic gynaecological surgery: A randomised controlled trial. Eur J Anaesthesiol. 2020;37(11):1032–9.
Pereira SM, Tucci MR, Morais CCA, Simões CM, Tonelotto BFF, Pompeo MS, et al. Individual positive end-expiratory pressure settings optimize intraoperative mechanical ventilation and reduce postoperative atelectasis. Anesthesiology. 2018;129(6):1070–81.
He X, Jiang J, Liu Y, Xu H, Zhou S, Yang S, et al. Electrical impedance tomography-guided PEEP titration in patients undergoing laparoscopic abdominal surgery. Medicine (Baltimore). 2016;95(14):e3306.
Girrbach F, Petroff D, Schulz S, Hempel G, Lange M, Klotz C, et al. Individualised positive end-expiratory pressure guided by electrical impedance tomography for robot-assisted laparoscopic radical prostatectomy: a prospective, randomised controlled clinical trial. Br J Anaesth. 2020;125(3):373–82.
Chun EH, Baik HJ, Moon HS, Jeong K. Comparison of low and high positive end-expiratory pressure during low tidal volume ventilation in robotic gynaecological surgical patients using electrical impedance tomography: A randomised controlled trial. Eur J Anaesthesiol. 2019;36(9):641–8.
Park SK, Yang H, Yoo S, Kim WH, Lim YJ, Bahk JH, et al. Ultrasound-guided versus conventional lung recruitment manoeuvres in laparoscopic gynaecological surgery: A randomised controlled trial. Eur J Anaesthesiol. 2021;38(3):275–84.
Yang Y, Geng Y, Zhang D, Wan Y, Wang R. Effect of lung recruitment maneuvers on reduction of atelectasis determined by lung ultrasound in patients more than 60 years old undergoing laparoscopic surgery for colorectal carcinoma: a prospective study at a single center. Med Sci Monit Int Med J Exp Clin Res. 2021;18(27):e926748.
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567–75.
Costa ELV, Slutsky AS, Brochard LJ, Brower R, Serpa-Neto A, Cavalcanti AB, et al. Ventilatory variables and mechanical power in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2021;204(3):303–11.
Gattinoni L, Carlesso E, Cadringher P, Valenza F, Vagginelli F, Chiumello D. Physical and biological triggers of ventilator-induced lung injury and its prevention. Eur Respir J Suppl. 2003;47:15s–25s.
Schuijt MTU, Hol L, Nijbroek SG, Ahuja S, van Meenen D, Mazzinari G, et al. Associations of dynamic driving pressure and mechanical power with postoperative pulmonary complications-posthoc analysis of two randomised clinical trials in open abdominal surgery. EClinicalMedicine. 2022;47:101397.
Karalapillai D, Weinberg L, Neto AS, Peyton P, Ellard L, Hu R, et al. Intra-operative ventilator mechanical power as a predictor of postoperative pulmonary complications in surgical patients: A secondary analysis of a randomised clinical trial. Eur J Anaesthesiol. 2022;39(1):67–74.
Chiumello D, Formenti P, Bolgiaghi L, Mistraletti G, Gotti M, Vetrone F, et al. Body position alters mechanical power and respiratory mechanics during thoracic surgery. Anesth Analg. 2020;130(2):391–401.
Boesing C, Schaefer L, Hammel M, Otto M, Blank S, Pelosi P, et al. Individualized positive end-expiratory pressure titration strategies in superobese patients undergoing laparoscopic surgery: prospective and nonrandomized crossover study. Anesthesiology. 2023;139(3):249–61.
Jimenez JV, Munroe E, Weirauch AJ, Fiorino K, Culter CA, Nelson K, et al. Electric impedance tomography-guided PEEP titration reduces mechanical power in ARDS: a randomized crossover pilot trial. Crit Care Lond Engl. 2023;27(1):21.
Spaeth J, Ott M, Karzai W, Grimm A, Wirth S, Schumann S, et al. Double-lumen tubes and auto-PEEP during one-lung ventilation. Br J Anaesth. 2016;116(1):122–30.
Lohser J, Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg. 2015;121(2):302–18.
Rauseo M, Mirabella L, Grasso S, Cotoia A, Spadaro S, D’Antini D, et al. Peep titration based on the open lung approach during one lung ventilation in thoracic surgery: a physiological study. BMC Anesthesiol. 2018;18(1):156.
Liu K, Huang C, Xu M, Wu J, Frerichs I, Moeller K, et al. PEEP guided by electrical impedance tomography during one-lung ventilation in elderly patients undergoing thoracoscopic surgery. Ann Transl Med. 2019;7(23):757.
Steinmann D, Stahl CA, Minner J, Schumann S, Loop T, Kirschbaum A, et al. Electrical impedance tomography to confirm correct placement of double-lumen tube: a feasibility study. Br J Anaesth. 2008;101(3):411–8.
Schetz M, De Jong A, Deane AM, Druml W, Hemelaar P, Pelosi P, et al. Obesity in the critically ill: a narrative review. Intensive Care Med. 2019;45(6):757–69.
Pépin JL, Timsit JF, Tamisier R, Borel JC, Lévy P, Jaber S. Prevention and care of respiratory failure in obese patients. Lancet Respir Med. 2016;4(5):407–18.
O’Quin RJ, Marini JJ, Culver BH, Butler J. Transmission of airway pressure to pleural space during lung edema and chest wall restriction. J Appl Physiol Bethesda Md 1985. 1985;59(4):1171–7.
Venus B, Cohen LE, Smith RA. Hemodynamics and intrathoracic pressure transmission during controlled mechanical ventilation and positive end-expiratory pressure in normal and low compliant lungs. Crit Care Med. 1988;16(7):686–90.
Jardin F, Genevray B, Brun-Ney D, Bourdarias JP. Influence of lung and chest wall compliances on transmission of airway pressure to the pleural space in critically ill patients. Chest. 1985;88(5):653–8.
Bazurro S, Ball L, Pelosi P. Perioperative management of obese patient. Curr Opin Crit Care. 2018;24(6):560–7.
Ball L, Pelosi P. How I ventilate an obese patient. Crit Care Lond Engl. 2019;23(1):176.
Stahl DL, North CM, Lewis A, Kimberly WT, Hess DR. Case scenario: power of positive end-expiratory pressure: use of esophageal manometry to illustrate pulmonary physiology in an obese patient. Anesthesiology. 2014;121(6):1320–6.
Rowley DD, Arrington SR, Enfield KB, Lamb KD, Kadl A, Davis JP, et al. Transpulmonary pressure-guided lung-protective ventilation improves pulmonary mechanics and oxygenation among obese subjects on mechanical ventilation. Respir Care. 2021;66(7):1049–58.
Nestler C, Simon P, Petroff D, Hammermüller S, Kamrath D, Wolf S, et al. Individualized positive end-expiratory pressure in obese patients during general anaesthesia: a randomized controlled clinical trial using electrical impedance tomography. Br J Anaesth. 2017;119(6):1194–205.
Reychler G, Uribe Rodriguez V, Hickmann CE, Tombal B, Laterre PF, Feyaerts A, et al. Incentive spirometry and positive expiratory pressure improve ventilation and recruitment in postoperative recovery: A randomized crossover study. Physiother Theory Pract. 2019;35(3):199–205.
Simonte R, Cammarota G, De Robertis E. Intraoperative lung protection: strategies and their impact on outcomes. Curr Opin Anaesthesiol. 2024;37(2):184–91.
Pan LL, Gao LL, Yang L, Pan CX, Yin YH, Zhu Y, et al. Effect of EIT-guided individualized PEEP setting on the incidence of hypoxemia in elderly patients undergoing robot-assisted radical prostatectomy. Zhonghua Yi Xue Za Zhi. 2022;102(47):3727–33.
Wang Z, Ye S, Fan Y, Shi C, Wu H, Miao C, et al. Individualized positive end-expiratory pressure with and without recruitment maneuvers in obese patients during bariatric surgery. Kaohsiung J Med Sci. 2022;38(9):858–68.
Boesing C, Schaefer L, Schoettler JJ, Quentin A, Beck G, Thiel M, et al. Effects of individualised positive end-expiratory pressure titration on respiratory and haemodynamic parameters during the Trendelenburg position with pneumoperitoneum: A randomised crossover physiologic trial. Eur J Anaesthesiol. 2023;40(11):817–25.
Cylwik J, Buda N. The impact of ultrasound-guided recruitment maneuvers on the risk of postoperative pulmonary complications in patients undergoing general anesthesia. J Ultrason. 2022;22(88):e6-11.
Lerolle N, Guérot E, Dimassi S, Zegdi R, Faisy C, Fagon JY, et al. Ultrasonographic diagnostic criterion for severe diaphragmatic dysfunction after cardiac surgery. Chest. 2009;135(2):401–7.
Cavayas YA, Eljaiek R, Rodrigue É, Lamarche Y, Girard M, Wang HT, et al. Preoperative diaphragm function is associated with postoperative pulmonary complications after cardiac surgery. Crit Care Med. 2019;47(12):e966–74.
Kim SH, Na S, Choi JS, Na SH, Shin S, Koh SO. An evaluation of diaphragmatic movement by M-mode sonography as a predictor of pulmonary dysfunction after upper abdominal surgery. Anesth Analg. 2010;110(5):1349–54.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
J.J., G.M and S.S. wrote the main manuscript text. M.P.A.N. prepared the figure and the table. S.S. alsosupervised and optimized the text. All authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Human and Animal Rights
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jimenez-Santana, J.D., Spadaro, S., Argente Navarro, M.P. et al. Advanced Respiratory Monitoring in the Perioperative Setting. Curr Anesthesiol Rep (2024). https://doi.org/10.1007/s40140-024-00646-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s40140-024-00646-9