Abstract
Purpose of Review
The purpose of this review is to explore the underlying physiology and clinical applications of apneic oxygenation, a technique first described in humans in the mid-20th century. Specifically, we aim to summarize its significance in critical care and anesthetic management.
Recent Findings
High-flow nasal oxygenation (HFNO) has emerged as an innovative apneic oxygenation system with widespread acceptance, leading to its rapid adoption. Recent literature underscores the diverse applications of HFNO in perioperative medicine and its associated benefits. In this section, we analyze the latest available data and delineate the potential role of HFNO based on the current state of knowledge.
Summary
HFNO represents a groundbreaking advancement in apneic oxygenation, enhancing its efficacy significantly. This technique is rapidly gaining popularity due to its simplicity in setup, patient tolerability, and its capacity to deliver a high fraction of inspired oxygen along with positive airway pressure. Its versatility extends across various clinical scenarios, including induction of anesthesia and tubeless upper airway surgery. Furthermore, its utility extends to critical care, obese, obstetric, and pediatric patient populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The delivery of oxygen to patients is a fundamental aspect of anesthetic practice, given that oxygen saturation (SpO2) falling below 70% may precipitate dysrhythmias, hypoxic brain injury and death [1]. This becomes particularly important in patients with a difficult airway, compromised respiratory reserve (such as the obese patient, pregnant women, infants, individuals with obstructive pulmonary disease, or pulmonary fibrosis) or increased oxygen consumption (e.g., obese patients, pregnant women, children, or those with sepsis), and during rapid sequence induction (RSI). In recent years, the concept of a difficult physiological airway has emerged, in reference to the physiological conditions of some patients that complicate airway management, with an increased incidence of desaturation, hemodynamic instability and even cardiocirculatory arrest. In all these circumstances it is vital to maximize oxygen delivery to increase the safe apnea time in subjects especially prone and vulnerable to hypoxemia. It is precisely in these situations where apneic oxygenation plays a fundamental role in increasing safety during the intubation process.
The initial step in ensuring airway safety is effective preoxygenation tailored to each patient, aiming to achieve an exhaled fraction of oxygen (EtO2) exceeding 90% before apnea onset. Following induction of general anesthesia, oxygenation is typically achieved through intermittent positive pressure ventilation via a facemask, which must be removed during tracheal intubation. Subsequently, maintaining oxygen supply to the lungs becomes feasible through apneic oxygenation techniques, initially described in humans by Comroe and Dripps in 1946 [2]. The efficacy of these techniques hinges on three key factors: the presence of a high concentration of oxygen in the lungs and dead space, a patent airway (by jaw thrust or laryngoscopy with elevation of the epiglottis from the posterior pharyngeal wall), and adequate blood circulation [3]. These techniques serve to extend safe apnea duration and offer additional time to explore and execute alternative airway management strategies when securing the airway proves challenging. In recent years, significant advancements in these techniques have been facilitated by Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) systems, which also enable preoxygenation. Apneic oxygenation techniques hold particular significance during laryngotracheal surgeries where maintaining an airway that is not obstructed by an endotracheal tube is preferred for the procedure’s execution.
Methods
We conducted a comprehensive literature search in PubMed to identify pertinent articles (updated as of February 15, 2024). The search strategy involved employing the following terms: “apneic oxygenation”, “THRIVE,” and “high-flow nasal oxygen”. Abstracts of the identified articles were scrutinized for relevance, and their references were screened to locate additional pertinent publications. Subsequently, a thorough review of the full text was performed for 233 articles, out of which 107 met the inclusion criteria for the final review.
Physiological Mechanism of Apneic Oxygenation
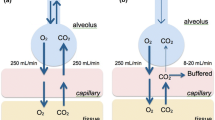
In adults, normal breathing entails approximately 250 mL/min of oxygen flowing from the alveoli into the bloodstream with a corresponding return of carbon dioxide (CO2) from the bloodstream to the alveoli. However, during apnea, while about 250 mL/min of oxygen continues to move from the alveoli into the bloodstream, only a fraction of blood CO2 is transported towards the alveoli (typically ranging from 8 to 20 mL/min), with the remainder buffered within the bloodstream and tissues. This disparity between the volume of oxygen exiting and CO2 entering the alveoli generates a negative pressure within the alveoli. This slightly subatmospheric pressure gradient facilitates gas diffusion from the pharynx to the alveoli, contingent upon the patency of the upper airway through techniques such as jaw thrust or suspension laryngoscopy [4, 5]. Consequently, alveoli continue to receive oxygen even in the absence of diaphragmatic movements or lung expansion. This phenomenon of mass movement of oxygen has been termed “aventilatory mass flow” [6], supplanting earlier terminologies such as “diffusion respiration” [7] and “apneic diffusion of oxygenation” [8], as gas transfer primarily occurs through mass flow rather than diffusion within the respiratory tree [9]. The onset of atelectasis under anesthesia induces ventilation–perfusion mismatch, progressively impeding the pulmonary circulation’s ability to extract insufflated oxygen, ultimately resulting in hypoxemia over a variable timeframe [10].
Apneic oxygenation is facilitated by the denitrogenation of the lungs during the preoxygenation phase preceding apnea. Denitrogenation elevates alveolar oxygen content and enhances the negative alveolar pressure generated upon oxygen transfer into the blood. Conversely, the presence of nitrogen (N2) and accumulated CO2 in the lungs diminishes the pressure gradient and oxygen transfer to the lungs, hastening the onset of hypoxemia [11]. Hence, apneic oxygenation lacks proven efficacy as a rescue technique in already desaturated patients [10].
Other mechanisms may also contribute to apneic oxygenation. Cardiogenic oscillations, which are airflow variations resulting from cardiac contractions, may aid in gas exchange during apnea [12]. Similarly, direct compression and expansion of the lung parenchyma adjacent to the heart, along with pulsatile flow in the pulmonary vasculature, might generate additional gas flow [13].
Moreover, the subatmospheric alveolar pressure facilitates CO2 transfer from the blood to the alveoli [10]. However, as alveolar CO2 accumulates over time, the pressure gradient for oxygen transfer diminishes, compounded by the adverse effects associated with profound hypercapnia, thus limiting the long-term utility of apneic oxygenation.
Apneic Oxygenation Techniques
Several techniques have been developed for apneic oxygenation, all aimed at delivering oxygen at high flow rates through various points in the airway [14]:
-
1.
Nasal techniques. Oxygen is administered directly into the nostrils through nasal prongs (Fig. 1A and B) or into the nasopharynx through a nasopharyngeal cannula (Fig. 1C).
Oxygen delivery techniques during apnea. Panel A: Nasal prongs placed in the nostrils. Panel B: High-flow nasal oxygen (HFNO) system delivering oxygen through the nostrils. Panel C: Nasal cannula delivering oxygen in the nasopharynx. Panel D: Oxygen administration through an endotracheal tube in the oropharynx during intubation
-
2.
Oral techniques. Oxygen is delivered via a endotracheal tube placed into the side of the mouth [15] or mounted in a videolaryngoscope (Fig. 1D).
-
3.
Other less commonly used techniques. Oxygen can be administered directly into the trachea through the lateral channel of a rigid bronchoscope during airway surgery (dilation of tracheal stenosis, resection of tracheal granulomas or tumors, etc.). Oxygen may also be administered into one of the main bronchi during one-lung ventilation via an endobronchial suction catheter positioned in the deflated lung or during the creation of bronchial anastomoses via a catheter inserted through the surgical field and positioned distal to the anastomosis. In this way, the possibility of hypoxemia can be reduced, but extreme precautions must be taken to avoid barotrauma, by using low oxygen flows and ensuring that there is no obstruction to the exit of the administered gases.
The term NODESAT (Nasal Oxygen During Efforts Securing A Tube) was introduced by Levitan to describe apneic oxygenation using unwarmed, dry oxygen via standard nasal cannula at 15 L/min [16]. This method is straightforward, as nasal prongs are readily accessible, require no prior preparation, and do not obstruct airway access during orotracheal intubation. Typically, patients are preoxygenated with a facemask concurrently with nasal oxygen, which is continued during intubation after removing the facemask. Initially, oxygen flow is set at around 5 L/min and then increased to as high as 15 L/min after induction to avoid drying the airway and discomfort for awake patients [17]. The utilization of nasal prongs during preoxygenation and bag-mask ventilation poses a potential challenge by compromising the integrity of the facemask seal. In order to mitigate this issue, a practical strategy involves temporarily resting the nasal prongs on the patient’s forehead during the preoxygenation and ventilation phases, followed by their placement nasally prior to laryngoscopy. This approach not only preserves the facemask seal but also diminishes the likelihood of barotrauma and gastric insufflation resulting from the simultaneous application of high-flow nasal oxygen and facemask oxygenation [10]. However, conventional oxygen therapy has limitations, including unpredictable and limited fractional inspired oxygen (FiO2) due to room air entrainment [18], as well as potential adverse effects such as impaired mucociliary function and bronchoconstriction due to cold and dry airflow [19].
Patel later introduced the term THRIVE (Transnasal Humidified Rapid-Insufflation Ventilatory Exchange) to describe apneic oxygenation via heated and humidified high-flow nasal cannula [18], also referred to as High-Flow Nasal Oxygenation (HFNO). THRIVE systems comprise a breathing circuit, an oxygen humidification system, contoured nasal prongs, and a head strap. Their physiological advantages include nasopharyngeal dead space washout, reduced work of breathing, alveolar recruitment, maintained mucociliary function and provision of apneic oxygenation [15]. The prescribed FiO2 (up to 1.0) can be delivered at various flow rates (0–70 L/min), resulting in proportional increases in mean airway pressure (continuous positive airway pressure between 2.7 and 7.4 cmH2O) [19, 20]. Oxygen is delivered at temperatures and humidity levels similar to those of healthy lungs, enhancing awake patient comfort and tolerance. These systems have been used for preoxygenation as well as other applications in the perioperative period (Table 1). However, THRIVE systems are contraindicated in cases of severe nasal obstruction, copious nasal bleeding, recent maxillofacial trauma or surgery, significantly elevated intracranial pressure, and skull base fractures [19, 21].
Uses of Apneic Oxygenation during Airway Management
During airway management and until definitive control is established through the placement of an extraglottic device, endotracheal intubation or front-of-neck access, continuous administration of oxygen during apnea has demonstrated several advantages. It enhances SpO2, reduces the incidence of hypoxemia, extends the safe apnea period, and increases the success rate of first-pass intubation [22]. Apneic oxygenation yields significant benefits by improving SpO2 and delaying desaturation in the majority of tracheal intubation cases, except in patients primarily suffering from respiratory failure [1, 23]. Hence, the integration of apneic oxygenation into intubation protocols is recommended, a notion supported by recent airway management guidelines [24,25,26,27,28]. However, compared to conventional oxygenation methods, HFNO does not seem to significantly decrease the occurrence of severe desaturation during the peri-intubation period [29].
Obesity
Obese patients exhibit a rapid desaturation once apnea ensues, attributed to their lower functional residual capacity and elevated oxygen consumption compared to non-obese individuals [30]. Consequently, difficulties encountered during facemask ventilation and tracheal intubation can escalate into critical scenarios within a short timeframe. Apneic oxygenation techniques have demonstrated significant efficacy in delaying desaturation before tracheal intubation in this population [15, 17, 32, 33]. Compared to conventional oxygen therapy, HFNO reduces the incidence of hypoxemia, increases the lowest SpO2, decreases the need for additional respiratory support, and shortens the hospital length of stay in obese patients during the perioperative period [34].
Obstetrics
Peri-intubation oxygen administration to pregnant women during the induction of general anesthesia is critical for preventing harm to both the mother and fetus. Pregnant women are particularly susceptible to hypoxemia during apnea due to decreased respiratory reserve, heightened metabolic demand, and increased challenges in intubation. Additionally, achieving successful intubation on the first attempt is imperative due to the elevated risk of aspiration resulting from anatomical and hormonal changes associated with pregnancy and the emergent nature of many surgical procedures.
While the evidence regarding the use of apneic oxygenation in pregnant women is not as extensive as in other populations, guidelines for managing difficult intubation in obstetric patients recommend employing these techniques [35, 36], drawing from existing evidence in non-obstetric settings. Some studies have indicated that combining preoxygenation with apneic oxygenation using HFNO is as effective as or even superior to preoxygenation with a facemask [37, 38]. Moreover, the “hands-free” nature of preoxygenation with HFNO allows anesthesia staff to attend to other tasks in time-critical situations, providing an added benefit [39].
Pediatrics
In children, the development of hypoxemia following the onset of apnea occurs more rapidly compared to adults. This is attributed to their smaller functional residual capacity, increased closing capacity, and heightened oxygen consumption [40]. These challenges are particularly pronounced in neonates, who may also present difficulties in tracheal intubation due to their anatomical characteristics [41]. Neonates exhibit a high incidence of severe desaturation (48%) and an overall first-attempt intubation success rate of 64% [42]. Consequently, tracheal intubation efforts may necessitate a stop–start approach to allow for intermittent bag-mask ventilation. Adverse events are directly correlated with the overall number of tracheal intubation attempts [43], hence the importance of first-attempt success in pediatric airway management.
There is a burgeoning body of evidence supporting the use of apneic oxygenation during pediatric intubation, because it has been associated with a reduced incidence of hypoxemia and improved first-pass intubation success rates [44, 45]. While data specific to neonates are limited, apneic oxygenation in this population appears to confer significant benefits [41]. Consequently, the latest guidelines for pediatric airway management strongly advocate for its utilization [46, 47]. However, the optimal technique for oxygen delivery during pediatric intubation, as well as the ideal oxygen flow rate and concentration, remain to be determined, necessitating further research [41, 44, 45]. High-flow oxygen delivery holds promise as an effective technique based on operating room data, although its superiority over low-flow oxygen has not been conclusively demonstrated [44]. Despite the potential complications of administering high concentrations of oxygen to premature babies and infants (oxidative stress-related conditions like bronchopulmonary dysplasia and retinopathy of prematurity), the potential risks associated with brief hyperoxia are lower than the risks derived from hypoxemia [45].
Role of Apneic Oxygenation in the Intensive Care Unit, the Emergency Department and Prehospital Medicine
Traditionally, the focus on difficult airway management has centered around identifying anatomic characteristics of patients that pose challenges in visualizing the glottic opening or successfully placing the endotracheal tube through the vocal cords [48]. However, in critically ill patients, there are physiological disturbances beyond mere inadequate airway protection or hypoxemia that contribute to what is termed the “physiologically difficult airway”. These disturbances are associated with complications such as cardiac arrest and death [49]. The physiologic risk is exacerbated when tracheal intubation requires more than one attempt [50, 51], with difficult tracheal intubation serving as an independent predictor of mortality [52]. Therefore, achieving first-pass success should be the goal.
There is robust evidence supporting the use of apneic oxygenation in reducing the incidence of hypoxemia and severe desaturation during emergency tracheal intubations in critically ill patients. Apneic oxygenation has been shown to significantly improve blood oxygenation levels and increase first-pass tracheal intubation success rates [54, 55]. Consequently, its utilization is recommended in guidelines for the management of tracheal intubation in critically ill adults [49, 56, 57].
Role of Apneic Oxygenation during Surgical Procedures Involving the Airway
The presence of an endotracheal tube can sometimes impede adequate access to the surgical field in airway procedures, necessitating brief periods of extubation and apnea to perform the surgical technique. Various methods have been employed to extend the period of safe apnea and mitigate these challenging conditions. These techniques include spontaneous ventilation, controlled mechanical ventilation via a small endotracheal tube, transglottic or subglottic jet ventilation, and apneic anesthesia with intermittent ventilation [58].
Although the initial description of a series of laryngeal surgeries performed using apneic oxygenation dates back to 1961 [59], it is only recently that the introduction of a novel apneic oxygenation technique using HFNO has facilitated anesthesia without tracheal intubation for extended periods beyond what is achievable with low-flow nasal or oral oxygen administration. This technique has been applied in various procedures, including microlaryngoscopy [60, 61], panendoscopy [62], vocal cord biopsy [62, 63], cordotomy [64], debulking or excision of laryngeal tumors [61, 64, 65], laser excision of pharyngeal-supraglottic stenosis secondary to cicatricial band scars [66], injection thyroplasty [61, 64], rigid bronchoscopy [64], and balloon dilation of stenosis [64, 65, 67] (Table 1).
Typically, patients are pre-oxygenated with HFNO at 30 L/min and FiO2 = 1.0. Immediately prior to anesthetic induction, the flow rate is increased to 50–70 L/min, followed by total intravenous anesthesia with the administration of propofol, remifentanil, and a neuromuscular blocking agent. Upper airway patency is maintained with a jaw thrust, after which a suspension laryngoscope is inserted, and surgery is performed under apneic conditions. When a laser is utilized, FiO2 is reduced to 0.3. This technique has also been employed to maintain oxygenation in patients undergoing emergent awake surgical tracheostomy for upper airway obstruction [68]. Booth el al. published a series of 26 patients in which sedation with propofol and remifentanil, along with HFNO in spontaneously ventilating patients, was utilized to maintain oxygenation and airway patency during the management of obstructed airways; only one patient required rescue tracheal intubation due to a remifentanil overdose [65].
Other Specific Applications of HFNO in the Perioperative Period
Preoxygenation
Compared to preoxygenation with a facemask, HFNO offers several advantages. Patients experience greater comfort and tolerance, and healthcare personnel can maintain hands-free operation during the procedure. Additionally, HFNO allows for apneic oxygenation after induction. However, during the preoxygenation phase, patients must keep their mouths closed to prevent the ingress of ambient air and the consequent reduction in FiO2. This requirement may pose limitations in patients with high metabolic demands or respiratory distress, as they often need to breathe with their mouths open [19]. Other limitations of HFNO include the need for specific equipment, assembly time (it is recommended to turn on the equipment approximately 5 min before use to ensure adequate humidification and heating), and the inability to continuously measure EtO2.
Studies investigating the effectiveness of HFNO for preoxygenation have yielded variable results. Several recent meta-analyses indicate that patients preoxygenated with HFNO exhibit higher arterial oxygen partial pressure (PaO2) and extended safe apnea time, with no significant differences in the incidence of desaturation, minimum SpO2 values, EtO2 levels, or expired fraction of carbon dioxide (EtCO2) [70, 71]. However, these studies exhibit high heterogeneity, attributed to variations in subject characteristics (healthy volunteers or patients), oxygenation protocols (oxygen flow rate, use of pressure support or positive end-expiratory pressure [PEEP], utilization of facemask ventilation during apnea, type of neuromuscular blocking agents used), and outcome definitions.
Rapid Sequence Induction (RSI)
During a standard RSI, positive pressure ventilation is withheld until intubation to minimize the risk of aspiration in cases of inadequate fasting, impaired gastric emptying, or gastroesophageal reflux. In this context, HFNO appears to be at least as effective and safe as conventional preoxygenation with a facemask across various scenarios [37, 38, 73, 74].
Awake Intubation
Awake intubation, utilizing either a flexible bronchoscope or videolaryngoscope, is the technique of choice in patients with a known or suspected difficult airway, particularly when challenges with facemask ventilation are anticipated. The systematic implementation of HFNO during awake tracheal intubation has been advocated for safer oxygen delivery and enhanced procedural quality, because it is associated with less desaturation and a lower rate of multiple attempts [75, 76].
Deep Sedation for Complex Procedures
HFNO has demonstrated effectiveness in reducing the occurrence of hypoxemic events and procedural interruptions during deep sedation in a range of procedures [77]. These include gastrointestinal endoscopies [80, 81], endoscopic retrograde cholangiography [82], bronchoscopies [83], and hysteroscopy for assisted reproduction [84]. Compared to a facemask, HFNO during endoscopic procedures provides good oxygenation without obstructing the mouth, facilitating scope placement. Additionally, HFNO has been proposed to mitigate lung atelectasis following prolonged deep sedation [85].
Extubation and Postoperative Respiratory Support
HFNO is linked to a notably lower rate of reintubation and reduced need for escalation of respiratory support when compared to conventional oxygen therapy in postextubation adult surgical patients. However, there appears to be no significant difference in the incidence of postoperative pulmonary complications or mortality [86]. HFNO has been suggested as a potential strategy to prevent respiratory failure in the immediate postoperative period, particularly among high-risk and/or obese patients undergoing cardiac or thoracic surgery [87, 88].
Complications
Apneic oxygenation techniques are generally considered safe and contribute to enhancing patient safety in airway management, particularly in individuals who are most susceptible and vulnerable to hypoxemia. Nevertheless, like any medical procedure, they are not without potential complications, which warrant careful consideration.
-
Hypercapnia and acidosis represent the most common complications associated with apneic oxygenation techniques, which consequently limit their utility to short periods of time. Hypercapnia induces respiratory acidosis, leading to an elevation in mean pulmonary arterial pressure and cardiac output through the stimulation of tachycardia and reduction in systemic vascular resistance. The likelihood of arrhythmias significantly rises with a pH < 7.0 and escalates exponentially with a pH < 6.8 [89]. The clearance of CO2 during HFNO may surpass that achieved with a low-flow oxygen delivery system [18]. Utilizing flow rates of up to 70 L/min may be necessary to attain maximal CO2 clearance [19]. However, it is crucial to note that HFNO may delay the early detection of CO2 elevation and airway obstruction compared to bag-mask ventilation. Therefore, employing transcutaneous monitoring of CO2 and oxygen reserve index sensors may aid in mitigating this risk [19].
-
Hypoxemia. In cases where preoxygenation before apnea has been inadequate or if airway patency cannot be effectively maintained, patients may experience more rapid desaturation than anticipated [10].
-
Barotrauma poses a risk when there is no clear route for gas egress during apneic oxygenation. Accumulation of gas within a space of finite capacity, such as the nostrils, thorax or stomach, can lead to harm [10, 90]. Reported cases include pneumocephalus [91, 92], pneumo-orbitus [92, 93], subcutaneous emphysema, pneumomediastinum and pneumothorax [94, 95], primarily observed in pediatric patients using nasal prongs. Administration of oxygen via a nasopharyngeal catheter has resulted in esophageal and gastric distension and perforation [96, 97]. Recent guidelines advise caution regarding simultaneous use of HFNO and facemask ventilation [56], as a tight facemask seal could prevent the escape of high-flow gases from the nose and mouth [90]. Special precautions are necessary in pediatric patients; to achieve a balance between safety and efficacy, it is recommended to use a nasal cannula size that is half the diameter of the nares [90].
-
Aspiration of gastric contents. There has been an ongoing debate regarding whether HFNO might elevate the risk of regurgitation of gastric contents by generating positive pressure, which theoretically could lead to gastric distension. However, studies utilizing ultrasonographic assessment of gastric volumes have not observed gastric insufflation [98, 99]. In fact, HFNO may even decrease the incidence of reflux and microaspiration during the induction of general anesthesia compared to facemask ventilation [100]. Nevertheless, it is important to note that in the presence of upper airway contamination from bleeding or regurgitation, high-flow oxygen insufflation can disperse pharyngeal contents [10]. Therefore, careful consideration should be given to the patient’s individual risk factors and clinical context when deciding on the appropriate oxygenation technique.
-
Epistaxis is a known but uncommon risk associated with HFNO [95, 101], and also with nasal airways and nasopharyngeal catheters. However, efficient humidification of gases in HFNO theoretically may reduce the likelihood of this complication. It is worth noting that the incidence of epistaxis may be more common in obstetric patients due to increased nasopharyngeal mucosal edema and vascularity [39]; hence, careful monitoring and consideration of risk factors are warranted, particularly in this patient population.
-
Airway fire is a well-known complication that can occur during certain head and neck surgeries. Ignition sources, such as laser or diathermy equipment, may inadvertently come into contact with flammable items (such as tracheal tubes or surgical drapes) in an oxygen-rich environment, resulting in a surgical fire. Therefore, during tubeless laryngeal surgery, delivering oxygen via an open system is not recommended when lasers or diathermy are in use [102]. Although there has been debate over whether airway tissues are less likely to combust than endotracheal tubes [103, 104], and the use of THRIVE has been described in case series without incidents [105], the risk remains nonzero [106, 107]. If the use of HFNO is deemed necessary, the FiO2 should be minimized, and clinicians must maintain constant vigilance throughout the entire procedure [64].
-
Accidental awareness. Apneic oxygenation does not deliver volatile agents to the lungs. Therefore, during airway management or tubeless anesthesia, total intravenous anesthesia is essential to prevent accidental awareness [10].
Conclusions
Apneic oxygenation stands as a valuable technique in airway management, significantly reducing the risk of desaturation and improving patient safety during various airway procedures. Its simplicity, accessibility, and effectiveness make it an indispensable tool in any clinical setting. Universal application of apneic oxygenation, particularly in populations vulnerable to hypoxemia such as obese individuals, pregnant women, children, critically ill patients, and during rapid sequence induction, is paramount until the airway is securely managed. The advent of THRIVE systems has revolutionized apneic oxygenation, extending its utility to preoxygenation and tubeless surgical procedures. These advancements further highlight the significance of apneic oxygenation in optimizing patient outcomes and underscore its role as a cornerstone in contemporary airway management practices.
Data Availability
No datasets were generated or analysed during the current study.
References
Gleason JM, Christian BR, Barton ED. Nasal cannula apneic oxygenation prevents desaturation during endotracheal intubation: an integrative literature review. West J Emerg Med. 2018;19:403–11. https://doi.org/10.5811/westjem.2017.12.34699.
Comroe JH Jr, Dripps RD, Artificial. respiration. 1946; 130: 381–3. J Am Med Assoc. 1946;130:381–383. https://doi.org/10.1001/jama.1946.02870070001001.
Enghoff H, Holmdahl MH, Risholm L. Diffusion respiration in man. Nature. 1951;168:830. https://doi.org/10.1038/168830a0.
Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59:165–e1751. https://doi.org/10.1016/j.annemergmed.2011.10.002.
Rudlof B, Hohenhorst W. Use of apneic oxygenation for the performance of pan-endoscopy. Otolaryngol Head Neck Surg. 2013;149:235–9. https://doi.org/10.1177/0194599813486248.
Bartlett RG, Brubach HF, Specht H. Demonstration of aventilatory mass flow during ventilation and apnea in man. J Appl Physiol. 1959;14:97–101. https://doi.org/10.1152/jappl.1959.14.1.97.
Draper WB, Whitehead RW. Diffusion respiration in the dog anesthetized by pentothal sodium. Anesthesiology. 1944;5:262–3.
Holmdahl MH. Pulmonary uptake of oxygen, acid-base metabolism, and circulation during prolonged apnoea. Acta Chir Scand Suppl. 1956;212:1–128.
Joels N, Samueloff M. Metabolic acidosis in diffusion respiration. J Physiol 1. 1956;133:347–59. https://doi.org/10.1113/jphysiol.1956.sp005591.
Lyons C, Callaghan M. Uses and mechanisms of apnoeic oxygenation: a narrative review. Anaesthesia. 2019;74:497–507. https://doi.org/10.1111/anae.14565.
Kolettas A, Grosomanidis V, Kolettas V, Zarogoulidis P, Tsakiridis K, Katsikogiannis N, et al. Influence of apnoeic oxygenation in respiratory and circulatory system under general anaesthesia. J Thorac Dis. 2014;6:S116–45. https://doi.org/10.3978/j.issn.2072-1439.2014.01.17.
West JB, Hugh-Jones P. Pulsatile gas flow in bronchi caused by the heart beat. J Appl Physiol. 1961;16:697–702. https://doi.org/10.1152/jappl.1961.16.4.697.
Tusman G, Suarez-Sipmann F, Peces-Barba G, Climente C, Areta M, Arenas PG, et al. Pulmonary blood flow generates cardiogenic oscillations. Respir Physiol Neurobiol. 2009;167:247–54. https://doi.org/10.1016/j.resp.2009.04.026.
Wong DT, Yee AJ, Leong SM, Chung F. The effectiveness of apneic oxygenation during tracheal intubation in various clinical settings: a narrative review. Can J Anesth. 2017;64:416–27. https://doi.org/10.1007/s12630-016-0802-z.
Heard A, Toner AJ, Evans JR, Aranda Palacios AM, Lauer S. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of buccal RAE tube oxygen administration. Anesth Analg. 2017;124:1162–7. https://doi.org/10.1213/ANE.0000000000001564.
Levitan RM. NO DESAT! Nasal oxygen during efforts securing a tube. Emerg Physicians Monthly 2010. https://www.epmonthly.com/article/no-desat/ (accessed 25/03/2024).
Moon TS, Tai K, Kim A, Gonzales MX, Lu R, Pak T, et al. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, double-blinded, controlled trial of nasal cannula oxygen administration. Obes Surg. 2019;29:3992–9. https://doi.org/10.1007/s11695-019-04077-y.
Patel A, Nouraei SAR. Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015;70:323–9. https://doi.org/10.1111/anae.12923.
Kim HJ, Asai T. High-flow nasal oxygenation for anesthetic management. Korean J Anesthesiol. 2019;72:527–47. https://doi.org/10.4097/kja.19174.
Ritchie JE, Williams AB, Gerard C, Hockey H. Evaluation of a humidified nasal high-flow oxygen system, using oxygraphy, capnography and measurement of upper airway pressures. Anaesth Intensive Care. 2011;39:1103–10. https://doi.org/10.1177/0310057x1103900620.
Kotwinski D, Paton L, Langford R. The role of high flow nasal oxygen therapy in anaesthesia. Br J Hosp Med. 2018;79:620–7. https://doi.org/10.12968/hmed.2018.79.11.620.
Silva LOJE, Cabrera L, Barrionuevo P, Johnson R, Erwin PJ, Murad MH, et al. Effectiveness of apneic oxygenation during intubation: a systematic review and meta-analysis. Ann Emerg Med. 2017;70:483–e49411. https://doi.org/10.1016/j.annemergmed.2017.05.00.
White LD, Melhuish TM, White LK, Wallace LA. Apnoeic oxygenation during intubation: a systematic review and meta-analysis. Anaesth Intensive Care. 2017;45:21–7. https://doi.org/10.1177/0310057x1704500104.
Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115:827–48. https://doi.org/10.1093/bja/aev371.
Myatra SN, Shah A, Kundra P, Patwa A, Ramkumar V, Divatia JV, et al. All India difficult airway association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian J Anaesth. 2016;60:885–98. https://doi.org/10.4103/0019-5049.195481.
Law JA, Duggan LV, Asselin M, Baker P, Crosby E, Downey A et al. Canadian Airway Focus Group updated consensus-based recommendations for management of the difficult airway: part 2. Planning and implementing safe management of the patient with an anticipated difficult airway. Can J Anaesth. 2021;68(9)1405–1436. https://doi.org/10.1007/s12630-021-02008-z. 2021.
Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiol. 2022;136(1):31–81. https://doi.org/10.1097/ALN.0000000000004002.
Gómez-Ríos MÁ, Sastre JA, Onrubia-Fuertes X, López T, Abad-Gurumeta A, Casans-Frances R et al. Spanish Society of Anesthesiology, Reanimation and Pain Therapy (SEDAR) Spanish Society of Emergency and Emergency Medicine (SEMES) and Spanish Society of Otolaryngology, Head and Neck Surgery (SEORL-CCC) Guideline for difficult airway management. Part I. Rev Esp Anestesiol Reanim. 2024;8:S2341-1929(24)00021 – 0. https://doi.org/10.1016/j.redare.2024. This guideline, a collaborative effort among prominent medical societies including SEDAR, SEMES and SEORL-CCC, consolidates current evidence-based recommendations for difficult airway management, including the crucial aspect of apneic oxygenation. It thereby provides healthcare professionals with a standarized approach to enhance patient safety and improve clinical outcomes in challenging airway situations.
Chaudhuri D, Granton D, Wang DX, Einav S, Helviz Y, Mauri T, et al. Moderate certainty evidence suggests the use of high-flow nasal cannula does not decrease hypoxia when compared with conventional oxygen therapy in the peri-intubation period: results of a systematic review and meta-analysis. Crit Care Med. 2020;48:571–8. https://doi.org/10.1097/CCM.0000000000004217.
Jense HG, Dubin SA, Silverstein PI, O’Leary-Escolas U. Effect of obesity on safe duration of apnea in anesthetized humans. Anesth Analg. 1991;72:89–93. https://doi.org/10.1213/00000539-199101000-00016.
Baraka AS, Taha SK, Siddik-Sayyid SM, Kanazi GE, El-Khatib MF, Dagher CM, et al. Supplementation of pre-oxygenation in morbidly obese patients using nasopharyngeal oxygen insufflation. Anaesthesia. 2007;62:769–73. https://doi.org/10.1111/j.1365-2044.2007.05104.x.
Ramachandran SK, Cosnowski A, Shanks A, Turner CR. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of nasal oxygen administration. J Clin Anesth. 2010;22:164–8. https://doi.org/10.1016/j.jclinane.2009.05.006.
Wong DT, Dallaire A, Singh KP, Madhusudan P, Jackson T, Singh M, et al. High-flow nasal oxygen improves safe apnea time in morbidly obese patients undergoing general anesthesia: a randomized controlled trial. Anesth Analg. 2019;129:1130–6. https://doi.org/10.1213/ANE.0000000000003966.
Zhou R, Wang HT, Gu W. Efficacy of high-flow nasal cannula versus conventional oxygen therapy in obese patients during the perioperative period: A systematic review and meta-analysis. Can Respir J. 2022;20;2022:415313. doi: 10.1155/2022/4415313. This meta-analysis investigates the efectiveness of high-flow nasal oxygenation in preventing peri- and post-procedural hypoxemia specifically in patients with obesity, shedding light on an important clinical consideration during anesthesia and procedural sedation.
Mushambi MC, Kinsella SM, Popat M, Swales H, Ramaswamy KK, Winton AL, et al. Obstetric Anaesthetists’ Association and Difficult Airway Society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anaesthesia. 2015;70:1286–306. https://doi.org/10.1111/anae.13260.
Ramkumar V, Dinesh E, Shetty SR, Shah A, Kundra P, Das S, et al. All India difficult airway association 2016 guidelines for the management of unanticipated difficult tracheal intubation in obstetrics. Indian J Anaesth. 2016;60:899–905. https://doi.org/10.4103/0019-5049.195482.
Zhou S, Zhou Y, Cao X, Ni X, Du W, Xu Z, et al. The efficacy of high flow nasal oxygenation for maintaining maternal oxygenation during rapid sequence induction in pregnancy: a prospective randomised clinical trial. Eur J Anaesthesiol. 2021;38:1052–8. https://doi.org/10.1097/EJA.0000000000001395.
Sjöblom A, Hedberg M, Johansson S, Henningsson R, Soumpasis I, Lafrenz H, et al. Pre-oxygenation using high-flow nasal oxygen in parturients undergoing caesarean section in general anaesthesia: a prospective, multi-centre, pilot study. Acta Anaesthesiol Scand. 2023;67:1028–36. https://doi.org/10.1111/aas.14264.
Tan PCF, Dennis AT. High flow humidified nasal oxygen in pregnant women. Anaesth Intensive Care. 2018;46:36–41. https://doi.org/10.1177/0310057X1804600106.
Trachsel D, Svendsen J, Erb TO, von Ungern-Sternberg BS. Effects of anaesthesia on paediatric lung function. Br J Anaesth. 2016;117:151–63. https://doi.org/10.1093/bja/aew173.
Baker EK, Davis PG, Hodgson KA. Apnoeic oxygenation during neonatal intubation. Semin Fetal Neonatal Med. 2023;28:101487. https://doi.org/10.1016/j.siny.2023.101487.
Foglia EE, Ades A, Sawyer T, Glass KM, Singh N, Jung P, et al. Neonatal intubation practice and outcomes: an international registry study. Pediatrics. 2019;143:1–10. https://doi.org/10.1542/peds.2018-0902.
Fiadjoe JE, Nishisaki A, Jagannathan N, Hunyady AI, Greenberg RS, Reynolds PI, et al. Airway management complications in children with difficult tracheal intubation from the Pediatric difficult intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med. 2016;4:37–48. https://doi.org/10.1016/S2213-2600(15)00508-1.
George S, Wilson M, Humphreys S, Gibbons K, Long E, Schibler A. Apnoeic oxygenation during paediatric intubation: a systematic review. Front Pediatr. 2022;10:1–11. https://doi.org/10.3389/fped.2022.918148.
Fuchs A, Huber M, Aebli J, Afshari A, Bonfiglio R, Greif R, et al. Apnoeic oxygenation during paediatric tracheal intubation: a systematic review and meta-analysis. Br J Anaesth. 2024;132:392–406. https://doi.org/10.1016/j.bja.2023.10.039.
Pawar DK, Rajan J, Raveendra US, Ramesh S, Shetty SR, Divatia JV, et al. All India difficult airway association 2016 guidelines for the management of unanticipated difficult tracheal intubation in paediatrics. Indian J Anaesth. 2016;60:906–14. https://doi.org/10.4103/0019-5049.195483.
Disma N, Asai T, Cools E, Cronin A, Engelhardt T, Fiadjoe J, et al. Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. Br J Anaesth. 2024;132:124–44. https://doi.org/10.1016/j.bja.2023.08.040.
Mosier JM, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles JC. The physiologically difficult airway. West J Emerg Med. 2015;16:1109–17. https://doi.org/10.5811/westjem.2015.8.27467.
Kornas RL, Owyang CG, Sakles JC, Foley LJ, Mosier JM, Terndrup T, et al. Evaluation and management of the physiologically difficult airway: Consensus recommendations from Society for Airway Management. Anesth Analg. 2021;132:395–405. https://doi.org/10.1213/ANE.0000000000005233.
Hasegawa K, Shigemitsu K, Hagiwara Y, Chiba T, Watase H, Brown CA, et al. Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Ann Emerg Med. 2012;60:749–e7542. https://doi.org/10.1016/j.annemergmed.2012.04.005.
Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. 2013;20:71–8. https://doi.org/10.1111/acem.12055.
Jabre P, Avenel A, Combes X, Kulstad E, Mazariegos I, Bertrand L, et al. Morbidity related to emergency endotracheal intubation - A substudy of the KETAmine SEDation trial. Resuscitation. 2011;82:517–22. https://doi.org/10.1016/j.resuscitation.2011.01.015.
Binks MJ, Holyoak RS, Melhuish TM, Vlok R, Bond E, White LD. Apneic oxygenation during intubation in the emergency department and during retrieval: a systematic review and meta-analysis. Am J Emerg Med. 2017;35:1542–6. https://doi.org/10.1016/j.ajem.2017.06.046.
Binks MJ, Holyoak RS, Melhuish TM, Vlok R, Hodge A, Ryan T, et al. Apnoeic oxygenation during intubation in the intensive care unit: a systematic review and meta-analysis. Hear Lung J Acute Crit Care. 2017;46:452–7. https://doi.org/10.1016/j.hrtlng.2017.08.001.
Pavlov I, Medrano S, Weingart S. Apneic oxygenation reduces the incidence of hypoxemia during emergency intubation: a systematic review and meta-analysis. Am J Emerg Med. 2017;35:1184–9. https://doi.org/10.1016/j.ajem.2017.06.029.
Higgs A, McGrath BA, Goddard C, Rangasami J, Suntharalingam G, Gale R, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120:323–52. https://doi.org/10.1016/j.bja.2017.10.021.
Myatra SN, Ahmed SM, Kundra P, Garg R, Ramkumar V, Patwa A, et al. The all India difficult airway association 2016 guidelines for tracheal intubation in the intensive care unit. Indian J Anaesth. 2016;60:922–30. https://doi.org/10.4103/0019-5049.195485.
Jaquet Y, Monnier P, Van Melle G, Ravussin P, Spahn DR, Chollet-Rivier M. Complications of different ventilation strategies in endoscopic laryngeal surgery: a 10-year review. Anesthesiology. 2006;104:52–9. https://doi.org/10.1097/00000542-200601000-00010.
Woodman D. Laryngoscopy under general anesthesia: apnoeic oxygenation technique. A report of over 100 cases. Ann Otol Rhinol Laryngol. 1961;70:1113–6. https://doi.org/10.1177/000348946107000415.
Gustafsson IM, Lodenius, Tunelli J, Ullman J, Jonsson Fagerlund M. Apnoeic oxygenation in adults under general anaesthesia using Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) - a physiological study. Br J Anaesth. 2017;118:610–7. https://doi.org/10.1093/bja/aex036.
Saad M, Albi-Feldzer A, Taouachi R, Wagner I, Fischler M, Squara P, et al. High-flow nasal oxygen for suspension laryngoscopy: a multicenter open-label study. J Int Med Res. 2022;50:3000605221140685. https://doi.org/10.1177/03000605221140685.
Lee S-J, Quek KH. Facilitating airway surgery in a morbidly obese patient using transnasal humidified Rapid Insufflation Ventilatory Exchange (THRIVE). Case Rep Anesthesiol. 2018;19:20185310342. https://doi.org/10.1155/2018/5310342.
Yang SH, Wu CY, Tseng WH, Cherng WY, Hsiao TY, Cheng YJ, et al. Nonintubated laryngomicrosurgery with Transnasal Humidified Rapid-Insufflation Ventilatory Exchange: a case series. J Formos Med Assoc. 2019;118:1138–43. https://doi.org/10.1016/j.jfma.2018.11.009.
Lyons C, Callaghan M. Apnoeic oxygenation with high-flow nasal oxygen for laryngeal surgery: a case series. Anaesthesia. 2017;72:1379–87. https://doi.org/10.1111/anae.14036.
Booth AWG, Vidhani K, Lee PK, Thomsett CM. SponTaneous respiration using IntraVEnous anaesthesia and Hi-flow nasal oxygen (STRIVE hi) maintains oxygenation and airway patency during management of the obstructed airway: an observational study. Br J Anaesth. 2017;118:444–51. https://doi.org/10.1093/bja/aew468.
Tam K, Jeffery C, Sung CK. Surgical management of supraglottic stenosis using intubationless Optiflow. Ann Otol Rhinol Laryngol. 2017;126:669–72. https://doi.org/10.1177/0003489417720220.
Riva T, Seiler S, Stucki F, Greif R, Theiler L. High-flow nasal cannula therapy and apnea time in laryngeal surgery. Paediatr Anaesth. 2016;26:1206–8. https://doi.org/10.1111/pan.12992.
Ffrench-O’carroll R, Fitzpatrick K, Jonker WR, Choo M, Tujjar O. Maintaining oxygenation with high-flow nasal cannula during emergent awake surgical tracheostomy. Br J Anaesth. 2017;118:954–5. https://doi.org/10.1093/bja/aex149.
Kuo HC, Liu WC, Li CC, Cherng YG, Chen JT, Wu HL, et al. A comparison of high-flow nasal cannula and standard facemask as pre-oxygenation technique for general anesthesia: a PRISMA-compliant systemic review and meta-analysis. Med (Baltim). 2022;101:E28903. https://doi.org/10.1097/MD.0000000000028903.
Li Y, Yang J. Comparison of Transnasal Humidified Rapid-Insufflation Ventilatory Exchange and facemasks in preoxygenation: a systematic review and meta-analysis. Biomed Res Int. 2022;13:20229858820. https://doi.org/10.1155/2022/9858820.
Song J-L, Sun Y, Shi Y-B, Liu X-Y, Su Z-B. Comparison of the effectiveness of high-flow nasal oxygen vs. standard facemask oxygenation for pre- and apneic oxygenation during anesthesia induction: a systematic review and meta-analysis. BMC Anesthesiol. 2022;22:1–12. https://doi.org/10.1186/s12871-022-01615-7.
Mir F, Patel A, Iqbal R, Cecconi M, Nouraei SAR. A randomised controlled trial comparing transnasal humidified rapid insufflation ventilatory exchange (THRIVE) pre-oxygenation with facemask pre-oxygenation in patients undergoing rapid sequence induction of anaesthesia. Anaesthesia. 2017;72:439–43. https://doi.org/10.1111/anae.13799.
Lodenius, Piehl J, Östlund A, Ullman J, Jonsson Fagerlund M. Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) vs. facemask breathing pre-oxygenation for rapid sequence induction in adults: a prospective randomised non-blinded clinical trial. Anaesthesia. 2018;73:564–71. https://doi.org/10.1111/anae.14215.
Sjöblom A, Hedberg M, Gille A, Guerra A, Aanesen V, Forsberg IM, et al. Pre-oxygenation using high-flow nasal oxygen versus tight facemask in trauma patients undergoing emergency anaesthesia. Acta Anaesthesiol Scand. 2024;68:447–56. https://doi.org/10.1111/aas.14368.
Badiger S, John M, Fearnley RA, Ahmad I, Asai T. Optimizing oxygenation and intubation conditions during awake fibre-optic intubation using a high-flow nasal oxygen-delivery system. Br J Anaesth. 2015;115:629–32. https://doi.org/10.1093/bja/aev262.
Kim HJ, Kim MS, Kim SY, Min IK, Park WK, Song SH, et al. A propensity score-adjusted analysis of efficacy of high-flow nasal oxygen during awake tracheal intubation. Sci Rep. 2022;12:11306. https://doi.org/10.1038/s41598-022-15608-6.
Liu H-Y, Tam K-W, Loh E-W, Liu W-C, Kuo H-C, Li C-C, et al. High-flow nasal oxygenation reduces the risk of desaturation in adults receiving procedural sedation: a meta-analysis of randomized controlled trials. Perioper Med Perioperative Med. 2021;10:41. https://doi.org/10.1186/s13741-021-00212-5.
Carron M, Tamburini E, Safaee Fakhr B, De Cassai A, Linassi F, Navalesi P. High-flow nasal oxygenation during gastrointestinal endoscopy. Systematic review and meta-analysis. BJA Open. 2022;18:100098. https://doi.org/10.1016/j.bjao.2022.100098.
Khanna P, Haritha D, Das A, Sarkar S, Roy A. Utility of high-flow nasal oxygen in comparison to conventional oxygen therapy during upper gastrointestinal endoscopic procedures under sedation: a systematic review and meta-analyses. Indian J Gastroenterol. 2023;42:53–63. https://doi.org/10.1007/s12664-022-01308-6.
Gu W-J, Wang H-T, Huang J, Pei J-P, Nishiyama K, Abe M, et al. High flow nasal oxygen versus conventional oxygen therapy in gastrointestinal endoscopy with conscious sedation: systematic review and meta-analysis with trial sequential analysis. Dig Endosc. 2022;34:1136–46. https://doi.org/10.1111/den.14315.
Hung K-C, Chang Y-J, Chen I-W, Soong T-C, Ho C-N, Hsing C-H, et al. Efficacy of high flow nasal oxygenation against hypoxemia in sedated patients receiving gastrointestinal endoscopic procedures: a systematic review and meta-analysis. J Clin Anesth. 2022;77:110651. https://doi.org/10.1016/j.jclinane.2022.110651. This systematic review and meta-analysis explore the efficay of high-flow nasal oxygenation in preventing hypoxemia during sedated gastrointestinal endoscopic procedures. The findings provide valuable insights into the use of high-flow nasal oxygenation in a specific clinical setting.
Cha B, Lee MJ, Park JS, Jeong S, Lee DH, Park TG. Clinical efficacy of high-flow nasal oxygen in patients undergoing ERCP under sedation. Sci Rep. 2021;11:350. https://doi.org/10.1038/s41598-020-79798-7.
Ben-Menachem E, McKenzie J, O’Sullivan C, Havryk A. 4 2. High-flow nasal oxygen versus standard oxygen during flexible bronchoscopy in lung transplant patients: a randomized controlled trial. J Bronchol Interv Pulmonol. 2020;27:259–65. https://doi.org/10.1097/LBR.0000000000000670.
Tang Y, Huang P, Chai D, Zhang X, Zhang X, Chen S, et al. High-flow nasal oxygen reduces the incidence of hypoxia in sedated hysteroscopy for assisted reproduction. Front Med. 2022;8:929096. https://doi.org/10.3389/fmed.2022.929096.
Shih C-C, Liang P-C, Chuang Y-H, Huang Y-J, Lin P-J, Wu C-Y. Effects of high-flow nasal oxygen during prolonged deep sedation on postprocedural atelectasis: a randomised controlled trial. Eur J Anaesthesiol. 2020;37:1025–31. https://doi.org/10.1097/EJA.0000000000001324.
Lu Z, Chang W, Meng SS, Zhang X, Xie J, Xu JY, et al. Effect of high-flow nasal cannula oxygen therapy compared with conventional oxygen therapy in postoperative patients: a systematic review and meta-analysis. BMJ Open. 2019;9:e027523. https://doi.org/10.1136/bmjopen-2018-027523.
Rochwerg B, Einav S, Chaudhuri D, Mancebo J, Mauri T, Helviz Y, et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med. 2020;46:2226–37. https://doi.org/10.1007/s00134-020-06312-y.
Chaudhuri D, Granton D, Wang D, Burns KEA, Helviz Y, Einav S, et al. High-flow nasal cannula in the immediate postoperative period: a systematic review and meta-analysis. Chest. 2020;158:1934–46. https://doi.org/10.1016/j.chest.2020.06.038.
Price HL. Effects of carbon dioxide on the cardiovascular system. Anesthesiology. 1960;21:652–63. https://doi.org/10.1097/00000542-196011000-00009.
Lyons C, Callaghan M. Apnoeic oxygenation in paediatric anaesthesia: a narrative review. Anaesthesia. 2021;76:118–27. https://doi.org/10.1111/anae.15107.
Iglesias-Deus A, Pérez-Munuzuri A, López-Suárez O, Crespo P, Couce ML. Tension pneumocephalus induced by high-flow nasal cannula ventilation in a neonate. Arch Dis Child Fetal Neonatal Ed. 2017;102:F173–5. https://doi.org/10.1136/archdischild-2015-309777.
O’Brien BJ, Rosenfeld JV, Elder JE. Tension pneumo-orbitus and pneumocephalus induced by a nasal oxygen cannula: report on two paediatric cases. J Paediatr Child Health. 2000;36:511–4. https://doi.org/10.1046/j.1440-1754.2000.00550.x.
Jasin LR, Kern S, Thompson S, Walter C, Rone JM, Yohannan MD. Subcutaneous scalp emphysema, pneumo-orbitis and pneumocephalus in a neonate on high humidity high flow nasal cannula. J Perinatol. 2008;28:779–81. https://doi.org/10.1038/jp.2008.99.
Hegde S, Prodhan P. Serious air leak syndrome complicating high-flow nasal cannula therapy: a report of 3 cases. Pediatrics. 2013;131:e939–944. https://doi.org/10.1542/peds.2011-3767.
Baudin F, Gagnon S, Crulli B, Proulx F, Jouvet P, Emeriaud G. Modalities and complications associated with the use of high-flow nasal cannula: experience in a pediatric ICU. Respir Care. 2016;61:1305–10. https://doi.org/10.4187/respcare.04452.
Alifano M, Veyrie N, Rabbat A. Pneumothorax, pneumomediastinum and hemorrhagic shock complicating oxygen administration through a nasopharyngeal catheter. Ann Thorac Surg. 2010;90:2061. https://doi.org/10.1016/j.athoracsur.2010.02.096.
Yao HHI, Tuck MV, McNally C, Smith M, Usatoff V. Gastric rupture following nasopharyngeal catheter oxygen delivery - a report of two cases. Anaesth Intensive Care. 2015;43:244–8. https://doi.org/10.1177/0310057x1504300216.
Chang MY, Kwak HJ, Kim JY, Park JY, Park HY, Yi IK. Effect of high-flow nasal oxygenation on gastric insufflation in patients undergoing laryngeal microsurgery under tubeless general anesthesia with neuromuscular blockade. J Clin Med. 2023;12:1800. https://doi.org/10.3390/jcm12051800.
Zhou X, Huang X, Zhou Z, Xu Q, Mei A, Mazomba LX, et al. Effect of Transnasal Humidified Rapid-Insufflation Ventilatory Exchange on gastric insufflation during anaesthesia induction: a randomised controlled trial and multivariate analysis. Eur J Anaesthesiol. 2023;40:521–8. https://doi.org/10.1097/EJA.0000000000001846.
Ding Y, Huang T, Ge Y, Gao J, Zhang Y. Effect of trans-nasal Humidified Rapid Insufflation Ventilatory Exchange on reflux and microaspiration in patients undergoing laparoscopic cholecystectomy during induction of general anesthesia: a randomized controlled trial. Front Med. 2023;10:1212646. https://doi.org/10.3389/fmed.2023.1212646.
Sotello D, Rivas M, Mulkey Z, Nugent K. High flow nasal cannula oxygen in adult patients: a narrative review. Am J Med Sci. 2015;349:179–85. https://doi.org/10.1097/MAJ.0000000000000345.
Apfelbaum JL, Caplan RA, Barker SJ, Connis RT, Cowles C, Ehrenwerth J, et al. Practice advisory for the prevention and management of operating room fires: an updated report by the American Society of Anesthesiologists Task Force on operating room fires. Anesthesiology. 2013;108:271–90. https://doi.org/10.1097/ALN.0b013e31827773d2.
Ward P. THRIVE and airway fires. Anaesthesia. 2017;72:1035. https://doi.org/10.1111/anae.13993.
Roy S, Smith LP. Surgical fires in laser laryngeal surgery: are we safe enough? Otolaryngol - Head Neck Surg. 2015;152:67–72. https://doi.org/10.1177/0194599814555853.
Khan NC, Vukkadala N, Saxena A, Damrose EJ, Nekhendzy V, Sung CK. Safety and utility of Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) for laser laryngeal surgery. Otolaryngol - Head Neck Surg. 2023;169:598–605. https://doi.org/10.1002/ohn.324.
Baudouin R, Rigal T, Circiu M, Lechien JR, Couineau F, Guen MLE, et al. Feasibility and safety of THRIVE in transoral laser microsurgery. Am J Otolaryngol. 2022;43:103605. https://doi.org/10.1016/j.amjoto.2022.103605.
Onwochei D, El-Boghdadly K, Oakley R, Ahmad I. Intra-oral ignition of monopolar diathermy during Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE). Anaesthesia. 2017;72:781–3. https://doi.org/10.1111/anae.13873.
Funding
Not aplicable.
Author information
Authors and Affiliations
Contributions
T.L. and A.S. wrote the main manuscript text and prepared figure. M.A.G.R. edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
No ethics approval was needed because this is a systematic review of published studies.
Human and Animal Rights
All images contained in this study have been made with the approval of the patients.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
López, T., Sastre, J.A. & Gómez-Ríos, M.Á. Apneic Oxygenation: A Narrative Review. Curr Anesthesiol Rep 14, 426–437 (2024). https://doi.org/10.1007/s40140-024-00640-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-024-00640-1