Abstract
Purpose of Review
Over the past decade, the perception of prescription opioids changed dramatically. Once considered a savior from all types of pain, with few side effects and no celling dose, opioids are now restricted by many states, health insurance companies, and pharmacies. This narrative review aims to synthesize the latest evidence for managing oncology patients at risk for non-medical opioid use (NMOU).
Recent Findings
Opioids are effective medications for reducing severe cancer pain, despite their side effects. Screening tools identify high-risk patients, and a nomogram is available, using routine clinical data. Prescription monitoring plans have some evidence for improving selected outcomes; however, the role of UDT remains unclear. Harm reduction measures include de-prescribing of benzodiazepines, opioid rotation, and scheduled rather than PRN dosing.
Summary
About one in five cancer patients are at risk for NMOU. There are effective strategies for identifying high-risk patients, reducing harm, and providing interdisciplinary psychosocial support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prescriptions for medications such as oxycodone and hydrocodone increased by 244% and 732%, respectively, over a 10-year period. These trends coincided with increased prescription opioid abuse, increased mortality, and increased healthcare utilization [1]. Since the declaration of a national health crisis in 2017, broad efforts at both state and federal levels may be improving specific outcomes. In 2018, there were 67,367 drug overdose deaths in the USA, 4.1% fewer deaths than in 2017; however, drug overdose death rates increased for methamphetamine, cocaine, and synthetic opioids other than methadone such as fentanyl and tramadol [2].
Despite ample evidence regarding their addictive potential and the high risk of diversion, opioids are often indispensable for managing severe cancer-related pain. A Cochrane review found that 19 out of 20 people with moderate or severe pain able to tolerate opioids will have pain reduced to mild or no pain within 14 days [3••]. Up to 70% of oncology patients referred to a palliative care clinic experienced moderate to severe pain levels [4]. Opioids are also prescribed for acute pain, chronic non-malignant pain, and neuropathic pain. Patients with cancer may, therefore, present with a multifaceted combination of acute on chronic cancer-related pain, compounded by a prior history of chronic non-malignant pain and neuropathy because of chemotherapy or surgery. The shortcomings in pain management training and the complexity of pain syndromes that often encompass physical, psychological, social, and spiritual dimensions present clinicians with a daunting clinical challenge [5]. A survey of oncology healthcare providers [6] found that fewer than 25% reported adequate knowledge of opioid prescribing. In addition, the survey results illustrated the paradox facing many clinicians: although 69% felt that non-medical opioid use (NMOU) among patients is frequently under-detected, 63% reported that cancer pain is frequently undertreated. NMOU is defined as either the use of opioids in a non-prescribed manner for the experience or feeling they cause or the use of opioids without a prescription [7].
Education measures, prescription monitoring programs, and opioid management guidelines appear to be intuitive, common-sense measures targeting the crisis; however, a systematic review of interventions and programs for the appropriate prescribing of opioids concluded that literature evidence for their effectiveness is scarce [8••]. Based on the limited available evidence from cancer pain and non-malignant chronic pain studies, our approach to the clinical assessment and management of patients at risk is as follows.
Assessment
Effective pain management requires an assessment of patients’ pain syndrome. A study of inpatients with cancer pain found that those patients evaluated by assessment tools such as the Brief Pain Inventory (BPI) and Edmonton Symptom Assessment Scale (ESAS) experienced improved pain scores and significant increases in regular use of paracetamol, anti-neuropathic pain drugs, and opioids compared with a control group [9]. The initial evaluation should also include an opioid risk screening tool. Ideally, the tool should be validated, brief, and self-administered by patients. A systematic review found that the presence of opioid use disorder or other substance use disorder, certain mental health diagnoses (e.g., personality disorder), and concomitant prescription of certain psychiatric medications (e.g., atypical antipsychotics) identified patients at high risk of opioid use disorder [10•]. The authors noted that a few quality studies were available and that no symptoms, signs, or screening tools were particularly useful for identifying those at lower risk. Based on the assessment of over 700 consecutive patients referred to a supportive care clinic, male sex, prior history of alcoholism or illicit drug use, anxiety, and financial distress were predictive of aberrant opioid use [11].
For cancer-related pain, there is no single instrument identified as the benchmark for assessment of risk. An integrative review underscored the importance of screening, reporting about one in five patients with cancer are at risk of NMOU. Some studies demonstrated associations between high-risk patients and adverse outcomes, such as aberrant behavior, prolonged opioid use, higher morphine equivalent daily dose (MEDD), greater healthcare utilization, and symptom burden [12].
Questionnaires
The four-item CAGE score is a pragmatic choice for evaluating risk. There are over 13 studies in oncology patients, with several indicating that a score of ≥ 2 out of 4 is associated with adverse clinical outcomes or increased opioid use, although the tool assesses the risk for alcohol rather than opioid misuse. We consider the CAGE Adapted to Include Drugs (CAGE-AID) substance abuse screening tool a useful alternative, since this tool includes both alcoholism and illicit drug use. One study [10•] observed a CAGE-AID score of 1 out of 4 was the cutoff for patients with a high risk of aberrant opioid use behavior defined as Screener and Opioid Assessment for Patients with Pain (SOAPP-14) scores ≥ 7. Oncology patients at risk of aberrant opioid use scored high on the SOAPP questionnaire items concerning mood swings and alcohol or drug problems in family members or close friends.
A brief version of the 14-item SOAPP, the SOAPP–Short Form (SF), is a promising 5-item questionnaire. The SOAPP-SF cutoffs associated with prescription noncompliance among oncology patients were reported as ≥ 4 or ≥ 3 [13] from two different centers. Other factors associated with non-adherence to treatment (confirmed by UDT) included higher MEDD and a history of alcohol, smoking, or illicit drug use [14].
Recently, a nomogram [15••] estimated the probability of risk (defined as a SOAPP-14 score of ≥ 7) based on routinely collected clinical data and two brief questionnaires (ESAS and CAGE-AID) in patients referred to a supportive care clinic. Other relevant factors, such as genetics (e.g., opioids and their metabolism), may be added in the future. The nomogram is accessible online at https://is.gd/soappnomogram.
Urine Drug Tests (UDT)
UDT may detect the use of undisclosed medications, the nonuse of prescribed medications, and the use of illicit drugs. Although UDT is a key element in numerous opioid prescribing guidelines, UDTs are not widespread in oncology clinics, and large studies showing improved clinical outcomes are lacking. Of 323 patients in a palliative care clinic, fewer than 5% had UDT, with 56% having aberrant results. In an outpatient study at another NCI cancer center, clinicians ordered UDT in about 40% of patients based on clinical judgment of substance misuse risk. Seventy percent of those tested had an inappropriate UDT result, with about half showing non-prescribed opioids, benzodiazepines, or potent illicit drugs such as heroin or cocaine. Thirty-nine percent of UDTs were inappropriately negative, raising concerns about diversion or non-adherence and suggesting a wider role for UDT among oncology patients [16].
Before adopting a broader role for UDT, we should consider some of the drawbacks in testing patients with cancer-related pain. UDTs can impair the physician–patient relationship, especially if patients perceive the test as punitive or if the clinician misinterprets false-negative or false-positive results as accurate. Solutions to decrease the stigma associated with UDTs include standardizing periodic UDTs on all patients (not just high-risk patients), but the cost of such standardization may be prohibitive. There are generally two types of tests used: screening tests or immunoassays and confirmatory tests. Screening tests are fast, less expensive, and used as point-of-care tests. The limitations of immunoassays include the inability to detect synthetic opioids, low sensitivity and high false negativity rates, and cross reactivity with opioids and other substances (low specificity and high false positivity) [17•]. Confirmatory tests typically use mass spectrometry (MS) to identify opioids and their metabolites. They are highly sensitive, specific, and identify specific natural or synthetic opioids; however, confirmatory tests are more expensive, have a longer turnaround time, and require knowledge about opioids and their metabolites for accurate interpretation. We use MS for most oncology patients because accuracy is crucial to avoid false assumptions when interpreting the results, because the longer turnaround time is acceptable and because our patients are frequently prescribed synthetic opioids such as fentanyl or methadone.
Prescription Drug Monitoring Program (PMP)
PMPs are available in all 50 states, allowing providers (prescribers, pharmacists, and regulators) to access prescription data. Many states require providers to review PMP data prior to prescribing opioids. Integrating electronic medical records (EMR) and PMPs will be necessary to increase PMP adoption by providers in order to identify “physician shopping” and concomitant benzodiazepine [18] and gabapentinoid use. Although the evidence [19] is not conclusive [20], preliminary studies suggest that the use of PMP is associated with decreased prescriptions, opioid prescription overdoses, and deaths in some states [21•]. Unfortunately, PMP implementation may be associated with unintended consequences such as increased heroin overdoses [22].
Management
The fundamentals of managing patients—whether they are at high or low risk for NMOU—are included in the universal precautions (UP) (Table 1).
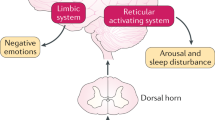
Originally developed for non-cancer pain, UP [23] are the standard of care for all patients, not only for those at high risk [24]. Management strategies for patients at high risk must include UP as well as additional measures to enhance education, promote harm reduction, mitigate risk, and address psychological and spiritual distress (Fig. 1). Existing guidelines should be updated; a recent appraisal of opioid prescribing for chronic non-cancer pain concluded that guidelines were at risk of bias because of pervasive conflicts of interest with the pharmaceutical industry [25].
Harm Reduction
The specific opioid, route of administration, co-administration of other drugs, and identification of the type and quality of pain are important factors in reducing harm [5]. Although the data for naloxone improving clinical outcomes in cancer pain are limited, it seems prudent to follow some Centers for Disease Control and Prevention(CDC) recommendations for non-malignant chronic pain, such as considering co-prescription of naloxone in patients who have a history of overdose or substance use disorder, and in those receiving benzodiazepines [26].
Co-medications
Polypharmacy increases the risk of adverse events; this is especially true for combinations of muscle relaxers, anti-histamines, gabapentinoids, anti-cholinergics [27], and benzodiazepines. De-prescribing is an important countermeasure, since these medications are associated with increased ED visits among the elderly [28], and concurrent benzodiazepine use is associated with a fivefold increase of opioid-related overdose [29•]. A Norwegian national cohort study reported that cancer survivors who are persistent or high-dose users of opioids are more likely to receive prescriptions of high-dose benzodiazepines and/or benzodiazepine-related hypnotics than among persistent opioid users in the general population [30]. The authors suggested the mechanism for addictive behavior towards both substances is explained by preclinical work showing benzodiazepines increase the rewarding and reinforcing effects of opioids [31].
Identifying the type of pain, such as neuropathic pain, can assist in mitigating the escalation of opioid doses. For example, duloxetine is the drug of choice for chemotherapy-induced peripheral neuropathy (CIPN), and although duloxetine has not yet been shown to be “opioid sparing,” neuropathic pain is less responsive to opioids and is associated with a higher MEDD [32]. We avoid some adjuvant analgesics such as gabapentinoids, given the limited evidence for their efficacy and the increased risk of mortality when combined with opioids or sedatives [33]. Currently, we counsel patients that the role of medical cannabis (MC) in cancer pain management is unclear and is supported by conflicting evidence. A systematic review indicated a likelihood of reduced opioid dose when used in combination with MC but also stated that a causal inference was not possible [34]. However, a recent narrative review concluded that controlled clinical data do not support the role of cannabinoids for opioid replacement or opioid-sparing effects when treating opioid use disorder or chronic pain [35]. Rather than demonstrating an opioid-sparing effect, there are also concerns about MC increasing NMOU. The confidential responses of over 57,000 US household residents indicated that MC users were more likely to report nonmedical use of any prescription drug, including opioids, stimulants, and tranquilizers [36].
Route
The route and speed of opioid administration may increase risk [37•]. Faster infusions of morphine in healthy volunteers produce greater effects than slower infusions on measures of good drug effect, drug liking, and “high” [38]. An anonymous survey of oncology nurses indicated that rapid opioid infusions might be increasing risk more often than expected. More than half of the nurses reported administering intravenous opioids too fast (< 120 s). In the inpatient oncology setting, the use of patient-controlled analgesia (PCA) with a continuous basal opioid infusion and no demand dosing may result in better pain control and fewer opioid side effects than intermittent dosing. We typically avoid demand dosing in an attempt to decrease the likelihood of patients with chemical coping or delirium self-administering IV opioids. Preclinical data supports this strategy, in that intermittent IV boluses of morphine facilitated subsequent morphine self-administration in comparison with continuous infusions [39].
Scheduled Administration and Extended Release
Similarly, in the outpatient setting, extended release rather than immediate release opioids may be preferable for cancer-related pain. A retrospective study from the Veterans Administration (VA) reported more overdose-related deaths for as-needed oral opioids compared with patients on scheduled opioids or those patients receiving both as-needed and regularly scheduled doses [40]. A contradictory conclusion from another VA study limited to patients with chronic non-cancer pain reported that patients on long-acting opioids had a significantly higher rate of overdose than those receiving short-acting opioids, particularly during the first 2 weeks after the initiation of treatment [41]. The reasons for the discrepancy between the two studies are unclear; however, patients with cancer taking regularly scheduled opioids may benefit by developing tolerance to respiratory depression.
Dose
In patients with non-malignant pain, the adverse effects of opioids (including overdose) increase with higher opioid doses. Although CDC guidelines regarding dose limits are not applicable to oncology patients undergoing active cancer treatment, clinicians should nevertheless avoid unnecessary dose escalation, given the risk for side effects such as sedation, delirium, and myoclonus.
Methadone or Buprenorphine for Pain and Opioid Use Disorder
Buprenorphine and methadone [42] are effective analgesics, indicated for opioid use disorder, and therefore may have an important role in patients with cancer-related pain and NMOU. Canadian guidelines for the management of patients with chronic non-cancer-related pain and substance use disorder recommend opioid agonist treatment with buprenorphine–naloxone as the preferred treatment; however, methadone is also acceptable [43].
Opioid Rotation
When patients develop tolerance, pain expression typically increases, and an opioid dose escalation with increased risk of adverse effects is a likely consequence. An alternative strategy to a dose increase is an opioid rotation or switch aimed at improving analgesia while simultaneously reducing MEDD. Opioid rotation is safe [44] and successful in about two thirds of patients with cancer, resulting in a decreased MEDD, and accompanied by improved pain, depression, overall well-being, and survival [45].
Aberrant Deterrent Opioid Formulations (ADF)
The high cost of these medications is often prohibitive, and their effectiveness in decreasing opioid abuse is unclear. There are fears that ADFs may increase opioid prescribing, facilitating a false sense of security among physicians, and some evidence suggests the advent of ADF prescriptions may be associated with increased heroin use [46].
Interdisciplinary Management of Psychological and Spiritual Distress
A multidisciplinary, non-judgmental, and compassionate approach to mitigating aberrant opioid-related behavior decreased the MEDD and median number of aberrant opioid-related behaviors among patients in a supportive care clinic when compared with a control group [47•]. When an interdisciplinary team is not available because of limited resources, clinicians should be familiar with Brief Motivational Interviewing (BMI), an objective, non-judgmental, and empathic interview style that includes personalized feedback, especially about markers of risk or harm. BMI [48] employs 5 general principles: (1) express empathy through reflective listening; (2) develop discrepancy between clients' goals or values and their current behavior; (3) avoid argument and direct confrontation; (4) roll with resistance rather than opposing it directly; and (5) support self-efficacy and optimism.
Education
The education of clinicians and patients plays an important role in mitigating opioid risk and decreasing harm. A study of 300 oncology patients attending a supportive care clinic found only 1 out of 10 patients locked up their opioids, and three out of four were unaware of proper opioid disposal methods [49]. A subsequent educational program using an information pamphlet along with personalized education and counseling improved patient-reported safe opioid use, storage, and disposal [50•]. Expanding low-cost programs such as an educational pamphlet to a digital intervention program may reach even more patients and families. Clinicians also benefit from education programs; however, their gained knowledge may not necessarily improve all clinical outcomes. A cluster-randomized clinical trial among 53 primary care clinicians and their 985 patients receiving long-term opioid therapy found improved guideline-concordant care, dose reduction, or opioid treatment discontinuation, but it found no difference in early opioid refills compared to controls [51].
Conclusion
The estimated prevalence of non-medical opioid use is about one in five patients and is likely higher in specific cancers (e.g., esophageal and lung cancers) associated with prior alcohol or tobacco use. Refining the assessment of risk with a nomogram that incorporates readily available patient data and simple clinical tools is a useful advance for daily practice. There are preliminary studies showing that education measures and interdisciplinary team intervention are effective management strategies in oncology. Adopting low-cost screening measures such as prescription drug monitoring programs appears straightforward given the minimal burden; however, the role of urine drug tests remains unclear because of concerns about implied mistrust, cost, and the expertise required for interpreting the results. Finally, further research is required to guide primary care clinicians in identifying and referring complex patients that require specialist palliative care or pain management.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hahn KL. Strategies to prevent opioid misuse, abuse, and diversion that may also reduce the associated costs. Am Health Drug Benefits. 2011;4(2):107–14.
Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999-2018. NCHS Data Brief. 2020;356:1–8.
•• Wiffen PJ, Wee B, Derry S, Bell RF, Moore RA. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;7(7):CD012592. https://doi.org/10.1002/14651858.CD012592.pub2Few randomized controlled trials are available, however the evidence for opioids reducing severe cancer pain is compelling.
Yennurajalingam S, Kang JH, Hui D, Kang DH, Kim SH, Bruera E. Clinical response to an outpatient palliative care consultation in patients with advanced cancer and cancer pain. J Pain Symptom Manage. 2012 Sep;44(3):340–50. https://doi.org/10.1016/j.jpainsymman.2011.09.014.
Vargovich AM, Schumann ME, Xiang J, Ginsberg AD, Palmer BA, Sperry JA. Difficult conversations: training medical students to assess, educate, and treat the patient with chronic pain. Acad Psychiatry. 2019 Oct;43(5):494–8. https://doi.org/10.1007/s40596-019-01072-4.
Arthur J, Edwards T, Lu Z, Hui D, Fellman B, Bruera E. Health care provider attitudes, beliefs, and perceived confidence in managing patients with cancer pain and nonmedical opioid use. J Pain Symptom Manage. 2020;S0885-3924(20):30584-4. https://doi.org/10.1016/j.jpainsymman.2020.06.040 Epub ahead of print.
Voon P, Kerr T. “Nonmedical” prescription opioid use in North America: a call for priority action. Subst Abuse Treat Prev Policy. 2013;8:39. https://doi.org/10.1186/1747-597X-8-39.
•• Moride Y, Lemieux-Uresandi D, Castillon G, de Moura CS, Pilote L, Faure M, et al. A systematic review of interventions and programs targeting appropriate prescribing of opioids. Pain Physician. 2019;22(3):229–40 Evidence is lacking for effective interventions.
Andersson V, Bergman S, Henoch I, Simonsson H, Ahlberg K. Benefits of using the Brief Pain Inventory in patients with cancer pain: an intervention study conducted in Swedish hospitals. Support Care Cancer. 2020;28(8):3721–9. https://doi.org/10.1007/s00520-019-05200-6.
• Klimas J, Gorfinkel L, Fairbairn N, Amato L, Ahamad K, Nolan S, et al. Strategies to identify patient risks of prescription opioid addiction when initiating opioids for pain: a systematic review. JAMA Netw Open. 2019;2(5):e193365. https://doi.org/10.1001/jamanetworkopen.2019.3365Risk factors obtained from readily available clinical information.
Yennurajalingam S, Edwards T, Arthur JA, Lu Z, Najera J, Nguyen K, et al. Predicting the risk for aberrant opioid use behavior in patients receiving outpatient supportive care consultation at a comprehensive cancer center. Cancer. 2018;124(19):3942–9. https://doi.org/10.1002/cncr.31670.
Carmichael AN, Morgan L, Del Fabbro E. Identifying and assessing the risk of opioid abuse in patients with cancer: an integrative review. Subst Abuse Rehabil. 2016;7:71–9. https://doi.org/10.2147/SAR.S85409.
Greiner RS, Boselli D, Patel JN, Salib M, Edelen C, Walsh D. Opioid risk screening in an oncology palliative medicine clinic. JCO Oncol Pract. 2020;30:OP2000043. https://doi.org/10.1200/OP.20.00043 Epub ahead of print.
Koyyalagunta D, Bruera E, Engle MP, Driver L, Dong W, Demaree C, et al. Compliance with opioid therapy: distinguishing clinical characteristics and demographics among patients with cancer pain. Pain Med. 2018;19(7):1469–77. https://doi.org/10.1093/pm/pnx178.
•• Yennurajalingam S, Edwards T, Arthur J, Lu Z, Erdogan E, Malik JS, et al. The development of a nomogram to determine the frequency of elevated risk for non-medical opioid use in cancer patients. Palliat Support Care. 2020:1–8. https://doi.org/10.1017/S1478951520000322Accessible online, requiring clinical data and two brief questionnaires.
Rauenzahn S, Sima A, Cassel B, Noreika D, Gomez TH, Ryan L, et al. Urine drug screen findings among ambulatory oncology patients in a supportive care clinic. Support Care Cancer. 2017 Jun;25(6):1859–64. https://doi.org/10.1007/s00520-017-3575-1.
• Arthur JA. Urine drug testing in cancer pain management. Oncologist. 2020;25(2):99–104. https://doi.org/10.1634/theoncologist.2019-0525A comprehensive review, including interpretation of UDT.
Liang D, Guo H, Shi Y. Mandatory use of prescription drug monitoring program and benzodiazepine prescribing among U.S. Medicaid enrollees. Subst Abus. 2019:1–8. https://doi.org/10.1080/08897077.2019.1686722 Epub ahead of print. PMCID: PMC7202951.
Rhodes E, Wilson M, Robinson A, Hayden JA, Asbridge M. The effectiveness of prescription drug monitoring programs at reducing opioid-related harms and consequences: a systematic review. BMC Health Serv Res. 2019;19(1):784. https://doi.org/10.1186/s12913-019-4642-8.
Liang D, Shi Y. The association between pain clinic laws and prescription opioid exposures: New evidence from multi-state comparisons. Drug Alcohol Depend. 2020;206:107754. https://doi.org/10.1016/j.drugalcdep.2019.107754.
• Pauly NJ, Slavova S, Delcher C, Freeman PR, Talbert J. Features of prescription drug monitoring programs associated with reduced rates of prescription opioid-related poisonings. Drug Alcohol Depend. 2018;184:26–32. https://doi.org/10.1016/j.drugalcdep.2017.12.002Highlights features associated with PMP success, important, given the relative lack of efficacy.
Fink DS, Schleimer JP, Sarvet A, Grover KK, Delcher C, Castillo-Carniglia A, et al. Association between prescription drug monitoring programs and nonfatal and fatal drug overdoses: a systematic review. Ann Intern Med. 168(11):783–90. https://doi.org/10.7326/M17-3074.
Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107–12. https://doi.org/10.1111/j.1526-4637.2005.05031.x.
Del Fabbro E. Assessment and management of chemical coping in patients with cancer. J Clin Oncol. 2014;32(16):1734–8. https://doi.org/10.1200/JCO.2013.52.5170.
Spithoff S, Leece P, Sullivan F, Persaud N, Belesiotis P, Steiner L. Drivers of the opioid crisis: an appraisal of financial conflicts of interest in clinical practice guideline panels at the peak of opioid prescribing. PLoS One. 2020;15(1):e0227045. https://doi.org/10.1371/journal.pone.0227045.
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 2016;315(15):1624–45. https://doi.org/10.1001/jama.2016.1464.
Green AR, Reifler LM, Bayliss EA, Weffald LA, Boyd CM. Drugs contributing to anticholinergic burden and risk of fall or fall-related injury among older adults with mild cognitive impairment, dementia and multiple chronic conditions: a retrospective cohort study. Drugs Aging. 2019;36(3):289–97. https://doi.org/10.1007/s40266-018-00630-z.
Alvarez CA, Mortensen EM, Makris UE, Berlowitz DR, Copeland LA, Good CB, et al. Association of skeletal muscle relaxers and antihistamines on mortality, hospitalizations, and emergency department visits in elderly patients: a nationwide retrospective cohort study. BMC Geriatr. 2015;15:2. https://doi.org/10.1186/1471-2318-15-2.
• Hernandez I, He M, Brooks MM, Zhang Y. Exposure-response association between concurrent opioid and benzodiazepine use and risk of opioid-related overdose in Medicare part D beneficiaries. JAMA Netw Open. 2018;1(2):e180919. https://doi.org/10.1001/jamanetworkopen.2018.0919Elevated risk of co-medications.
Fredheim OM, Skurtveit S, Loge JH, Sjøgren P, Handal M, Hjellvik V. Prescription of analgesics to long-term survivors of cancer in early adulthood, adolescence, and childhood in Norway: a national cohort study. Pain. 2020;161(5):1083–91. https://doi.org/10.1097/j.pain.0000000000001800.
Walker BM, Ettenberg A. Benzodiazepine modulation of opiate reward. Exp Clin Psychopharmacol. 2001;9(2):191–7. https://doi.org/10.1037//1064-1297.9.2.191.
Walsh D, Perin ML, McIver B. Parenteral morphine prescribing patterns among inpatients with pain from advanced cancer: a prospective survey of intravenous and subcutaneous use. Am J Hosp Palliat Care. 2006;23(5):353–9. https://doi.org/10.1177/1049909106292170.
Chincholkar M. Gabapentinoids: pharmacokinetics, pharmacodynamics and considerations for clinical practice. Br J Pain. 2020;14(2):104–14. https://doi.org/10.1177/2049463720912496.
Okusanya BO, Asaolu IO, Ehiri JE, Kimaru LJ, Okechukwu A, Rosales C. Medical cannabis for the reduction of opioid dosage in the treatment of non-cancer chronic pain: a systematic review. Syst Rev. 2020;9(1):167. https://doi.org/10.1186/s13643-020-01425-3.
Babalonis S, Walsh SL. Therapeutic potential of opioid/cannabinoid combinations in humans: review of the evidence. Eur Neuropsychopharmacol. 2020;36:206–16. https://doi.org/10.1016/j.euroneuro.2020.03.002.
Caputi TL, Humphreys K. Medical marijuana users are more likely to use prescription drugs medically and nonmedically. J Addict Med. 2018;12(4):295–9. https://doi.org/10.1097/ADM.0000000000000405.
• Arthur JA, Reddy A, Smith U, Hui D, Park M, Liu D, et al. Practices and perceptions regarding intravenous opioid infusion and cancer pain management. Cancer. 2019;125(21):3882–9. https://doi.org/10.1002/cncr.32380Underappreciated risk related to rapid administration of intravenous opioids.
Marsch LA, Bickel WK, Badger GJ, Rathmell JP, Swedberg MD, Jonzon B, et al. Effects of infusion rate of intravenously administered morphine on physiological, psychomotor, and self-reported measures in humans. J Pharmacol Exp Ther. 2001;299(3):1056–65.
Yu G, Zhang FQ, Tang SE, Lai MJ, Su RB, Gong ZH. Continuous infusion versus intermittent bolus dosing of morphine: a comparison of analgesia, tolerance, and subsequent voluntary morphine intake. J Psychiatr Res. 2014;59:161–6. https://doi.org/10.1016/j.jpsychires.2014.08.009.
Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–21. https://doi.org/10.1001/jama.2011.370.
Miller M, Barber CW, Leatherman S, Fonda J, Hermos JA, Cho K, et al. Prescription opioid duration of action and the risk of unintentional overdose among patients receiving opioid therapy. JAMA Intern Med. 2015;175(4):608–15. https://doi.org/10.1001/jamainternmed.2014.8071.
Fürst P, Lundström S, Klepstad P, Strang P. The use of low-dose methadone as add-on to regular opioid therapy in cancer-related pain at end of life: a national Swedish survey in specialized palliative care. J Palliat Med. 2020;23(2):226–32. https://doi.org/10.1089/jpm.2019.0253.
Furlan AD, Reardon R, Weppler C. National opioid use guideline group. Opioids for chronic noncancer pain: a new Canadian practice guideline. CMAJ. 2010;182(9):923–30. https://doi.org/10.1503/cmaj.100187.
Parsons HA, de la Cruz M, El Osta B, Li Z, Calderon B, Palmer JL, et al. Methadone initiation and rotation in the outpatient setting for patients with cancer pain. Cancer. 2010;116(2):520–8. https://doi.org/10.1002/cncr.24754.
Reddy A, Yennurajalingam S, Pulivarthi K, Palla SL, Wang X, Kwon JH, et al. Frequency, outcome, and predictors of success within 6 weeks of an opioid rotation among outpatients with cancer receiving strong opioids. Oncologist. 2013;18(2):212–20. https://doi.org/10.1634/theoncologist.2012-0269.
Alpert A, Powell D, Pacula RL. Supply-side drug policy in the presence of substitutes: evidence from the Introduction of abuse-deterrent opioids. Am Econ J: Economic Policy. 2018;10(4):1–35. https://doi.org/10.1257/pol.20170082.
• Arthur J, Edwards T, Reddy S, Nguyen K, Hui D, Yennu S, et al. Outcomes of a specialized interdisciplinary approach for patients with cancer with aberrant opioid-related behavior. Oncologist. 2018;23(2):263–70. https://doi.org/10.1634/theoncologist.2017-0248Effective Interdisciplinary team approach to high risk patients.
Center for Substance Abuse Treatment. Enhancing motivation for change in substance abuse treatment. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1999. (Treatment Improvement Protocol (TIP) Series, No. 35.) Chapter 3—Motivational Interviewing as a Counseling Style. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64964/
Reddy A, de la Cruz M, Rodriguez EM, Thames J, Wu J, Chisholm G, et al. Patterns of storage, use, and disposal of opioids among cancer outpatients. Oncologist. 2014;19(7):780–5. https://doi.org/10.1634/theoncologist.2014-0071.
• de la Cruz M, Reddy A, Balankari V, Epner M, Frisbee-Hume S, Wu J, et al. The impact of an educational program on patient practices for safe use, storage, and disposal of opioids at a comprehensive cancer center. Oncologist. 2017;22(1):115–21. https://doi.org/10.1634/theoncologist.2016-0266Simple educational pamphlet improves patient care.
Liebschutz JM, Xuan Z, Shanahan CW, LaRochelle M, Keosaian J, Beers D, et al. Improving adherence to long-term opioid therapy guidelines to reduce opioid misuse in primary care: a cluster-randomized clinical trial. JAMA Intern Med. 2017;177(9):1265–72. https://doi.org/10.1001/jamainternmed.2017.2468.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Opioid Use in an Opioid Epidemic
Rights and permissions
About this article
Cite this article
Granina, E., Kuzhiyil, A. & Del Fabbro, E. A Practical Approach to Assessment and Management of Patients at Risk for Non-medical Opioid Use: a Focus on the Patient with Cancer-Related Pain. Curr Anesthesiol Rep 10, 396–403 (2020). https://doi.org/10.1007/s40140-020-00417-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-020-00417-2