Abstract
Purpose of Review
The goal of this chapter is to educate physicians and practitioners of medicine on agents to avoid when managing patients with acute decompensated heart failure (ADHF). Through this review, we will offer explanations as to why it is necessary to refrain from the usage of certain medications, with the goal of providing optimal health care.
Recent Findings
The latest research reveals several classes of medications which should be used with caution or not at all in patients with ADHF.
Summary
We found that vasodilators (like ACE inhibitors) present the risk of hypotension, while beta- and calcium channel blockers worsen decompensation. Additionally, anti-arrhythmics were found to increase mortality, inotropes caused several deleterious effects (hypotension, arrhythmia), and glycosides offered no mortality benefit. Practitioners should be able to understand the adverse effects associated with the use of several drug classes in ADHF. With a proper understanding of these risks, they can make an educated determination as to whether they should be utilized in certain clinical scenarios.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
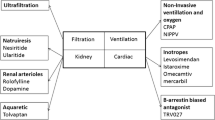
Management of acute decompensated heart failure (ADHF) has continued to evolve thanks in large part to important pharmacologic advances and improved understanding of heart failure pathophysiology. In order to optimize therapy for these patients, physicians must not only be aware of the appropriate medications to utilize but also those which should be avoided in order to guarantee the best outcomes. While diuretic agents such as furosemide, metolazone, and bumetanide are often seen as staples in heart failure treatment, a variety of other medications exist that can have deleterious effects. Here, we will explore the agents to avoid in ADHF and explain why refraining from these therapies is necessary.
Vasodilating Agents
While intravenous vasodilators are a commonly used therapy for heart failure, strong evidence demonstrating improved outcomes in the acute setting is lacking. It should be understood that although potentially beneficial, vasodilators can have detrimental effects as well and should be discontinued if symptomatic hypotension ensues. Of note, early utilization of intravenous ACE inhibitors in heart failure can be harmful as demonstrated by the CONSENSUS 2 trial. In this project, intravenous enalapril was studied and found to be associated with more adverse effects when compared to placebo, including responses such as hypotension (25.3 vs 9.6%, p < 0.001) [1]. Thus, the early utilization of intravenous ACE inhibitors in ADHF is discouraged.
As it concerns other vasodilators, evidence supporting their usage remains weak. Nitroprusside, the agent which acts via arterial and venous vasodilation to increase cardiac output, has limited data on its effectiveness and benefits in heart failure. In fact, the agent has been associated with worse outcomes in certain situations, with one study evaluating over 800 men with presumed acute myocardial infarction and finding higher mortality rates when initiated within the first 9 hours when compared to placebo (24.2 vs 12.7%, p = 0.025) [2]. Coupled with the fact that it requires close hemodynamic monitoring as the risk of hypotension is greatly increased in states of depressed cardiac functioning, nitroprusside remains an unfavorable agent to use in most heart failure scenarios and should be preserved for events like hypertensive crisis [2].
In the largest randomized placebo-controlled trial of nesiritide (the recombinant form of BNP), the Acute Study of Clinical Effectiveness of Nesiritide in Decompensated Heart Failure Trial (ASCEND-HF) studied over 7000 patients and found that although the drug had a borderline improvement in dyspnea, it was also more likely to induce symptomatic hypotension (7.2 vs 4.0%, p < 0.001) [3]. In ASCEND-HF, there was no improvement in 30-day mortality or hospitalization in patients receiving Nesiritide and in general the agent should be avoided in ADHF. A newer agent, Entresto (sacubitril/valsartan), was recently approved for use in the USA for treatment in chronic, stable, symptomatic heart failure. As no major studies exist regarding the drug’s usage in the emergency setting, it should be avoided in such circumstances until more research is performed.
Beta-Blocking Agents
Concerns about the negative inotropic effect of beta-blockers, as well as possible hemodynamic compromise, have led practitioners to avoid beta-blockers more often than not in patients with ADHF. Unsurprisingly, many patients who present with heart failure are on a medication regimen which includes beta-blockers and in those instances the drug can and should be continued, as discontinuation has been associated with both increased mortality and readmission [4••]. However, in cases where patients are not previously on a beta-blocker or are clearly decompensated with evidence of hypoperfusion, initiating beta-blocker therapy should be avoided as it carries the potential to worsen ADHF. Once these patients are stabilized, institution of a beta-blocker regimen can occur as a great deal of data confirms their beneficial effects in the long term for systolic heart failure patients.
Calcium Channel Blocking Agents
Due to the negative inotropic properties of calcium channel blockers and their association with worse outcomes in cases of ADHF, they should be avoided. Studies have shown that when compared to placebo, patients with ejection fractions under 40% who received verapamil after an acute myocardial infarction were more likely to develop clinical heart failure [5]. Moreover, hemodynamic and clinical deterioration has not only been seen in cases of verapamil usage but also with dihydropyridines (such as nifedipine) in systolic heart failure patients [6, 7].
Newer agents like clevidipine, a short acting dihydropyridine which is arterial selective and has no negative effect on myocardial contractility, are now available for use. While these properties appear to make it a more favorable selection for heart failure patients, further elucidation of its safety profile is required as there have been documented cases of reflex tachycardia and atrial fibrillation [8].
Inotropic Agents
While inotropic agents are the main stay of therapy in multiple ICU settings where patients demonstrate hypotension accompanied by signs and symptoms of end-organ hypoperperfusion and persistent pulmonary congestion despite use of diuretics, their usage should be done with discretion. Numerous studies have been performed on inotropic agents and shown them to be deleterious medications in ADHF, especially in situations of left ventricular outflow tract obstruction and tachyarrhythmias. One specific clinical trial, OPTIME-CHF (Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbation of Chronic Heart Failure), explored the effects of milrinone infusion for over 48 h in ADHF patients and found its use associated with an increase in adverse events like hypotension, as well as atrial fibrillation and flutter [9]. Another trial studied the short-term use of the agent and found it did not improve signs or symptoms, providing further evidence against routine use of the medication as an adjunct to standard heart failure therapy [10]. These events can be explained by the increase in oxygen demand caused by inotropes in general, which can worsen already existing arrhythmias or incite myocardial ischemia [11, 12].
Several trials have also shown dobutamine, a beta agonist, is associated with an increase in adverse cardiac events when used in ADHF [13, 14]. It is worth noting that both dobutamine and milrinone similarly increase cardiac output and decrease cardiac filling pressures. Although milrinone has been documented as being more effective when it comes to lowering filling pressures and decreasing systemic vascular resistance, both agents have been confirmed to promote increased myocardial oxygen demand [9].
Milrinone is preferred over dobutamine during concomitant beta-blocker therapy as its site of action is distal to the beta-adrenergic receptors [15,16,17]. However, data concerning milrinone in the setting of ischemic heart failure is worrisome and the agent should be avoided in those scenarios if possible [10, 15, 18]. Additionally, if arrhythmias (atrial or ventricular in origin) are of clinical concern, dobutamine should be avoided as it more likely to worsen existing tachyarrhythmias [19, 20].
Anti-arrhythmic Agents
Studies have shown that class I anti-arrhythmic agents should be avoided in patients with systolic heart failure as they not only offer a negative inotropic effect but also possess pro-arrhythmic qualities [21, 22]. The CAST study (Cardiac Arrhythmia Suppression Trial) revealed the association between class IC agents (such as flecainide) and increased mortality in patients who had decreased systolic functioning following an acute myocardial infarction [23••, 24]. Class IA drugs (quinidine, procainamide, disopyramide) have also been associated with increased mortality in those with decreased left ventricular systolic function [22].
Studies have been performed on class III agents and found them to be contraindicated in some cases of heart failure. In the SWORD trial (Survival with Oral D-Sotalol), it was revealed that the d-isomer of Sotalol was associated with a higher relative risk of mortality in patients with an ejection fraction under 40%. While direct studies concerning ibutilide’s performance in decompensated heart failure are limited, concerns remain regarding possible pro-arrhythmic side effects [22].
Glycosides
Digoxin remains a difficult agent to utilize in clinical practice as it provides great benefits in terms of its rate control and inotropic properties but also possesses potential drawbacks revolving around its efficacy and safety profile [25]. The drug has shown benefit in terms of rate control in atrial fibrillation and has been proven to provide symptom improvement in chronic systolic heart failure via increases in ejection fraction and cardiac output. However, digoxin has never been shown to improve death rates, a fact supported by the Digitalis Investigation group which performed a randomized study on close to 7000 heart failure patients with ejection fractions under 45% and a New York Heart Association classification of II–IV. The group found that while digoxin reduced the rate of hospitalization, it had no effect on overall mortality [25].
Additional consideration into the use of this drug should be considered in certain demographics, as studies have shown women, hypertensives, and patients who possess a preserved ejection fraction derive less benefit from digitalis therapy [25]. With these facts taken into consideration, along with the knowledge that several alternative agents exist with superior safety and efficacy profiles, digoxin cannot be recommended as a first-line agent in ADHF. However, if ideal agents are limited, digoxin remains a serviceable option for patients suffering from severe heart failure requiring temporary symptomatic relief.
Additional Agents
A variety of additional agents can exacerbate the symptoms of heart failure and should be avoided if possible. Nonsteroidal anti-inflammatory drugs are one of the most important medications of which to be aware, due in large part to their high usage rate among patients. The cardiovascular risk associated with their usage relates to the inhibition of COX-1 and COX-2 [26]. These agents promote the inhibition of prostaglandin synthesis by blocking COX-2, which causes a decrease in renal prostaglandin levels. This in turn lowers the glomerular filtration rate and can lead to sodium and water retention, thereby worsening volume status in an already compromised patient [27•]. COX-2 is more often associated with cardiotoxic effects, as the reduction of prostacyclin synthesis allows COX-1-derived thromboxane production in platelets, as well as vasoconstriction, to proceed unchecked. This process predisposes heart failure patients to further thrombosis, hypertension, or atherosclerotic buildup, all obvious unwanted potential complications [28].
Corticosteroids should also be avoided if possible in heart failure patients as they contribute to fluid retention and elevate blood pressure, mostly due to the volume expansion seen via the action of mineralocorticoids [22, 29]. The use of thiazolidinediones (such as rosiglitazone and pioglitazone) in patients with a history of heart failure is also cautioned against. Used for type 2 diabetes mellitus management, the agents are contraindicated as they can increase intravascular volume by 7% and lead to acute decompensations in heart failure patients [30, 31]. Additionally, whether used alone or in combination with other oral anti-diabetic drugs (metformin, sulfonylureas), these agents have a proven association with increased frequency of edema. Data confirms that combination usage with insulin promotes a significant increase in edema frequency as high as 16%, compared to the 7% with insulin alone [32]. Even with these facts in mind, usage of these agents remains up to the discretion of the prescribing physician but should be considered before utilization.
Cilostazol, a selective inhibitor of 3-type phosphodiesterase used in the treatment of intermittent claudication, is contraindicated in heart failure as it can increase both heart rate and cause ventricular tachycardia [33]. Anagrelide, which sometimes used in the treatment of essential thrombocytopenia, is another phosphodiesterase inhibitor which should be avoided in ADHF. Via its mechanism of increasing cyclic adenosine monophosphate (promoting calcium inflow into the myocardium) causing a positive inotropic effect, it can worsen left ventricular dysfunction and increase the risk of supraventricular arrhythmias [22].
Conclusion
Much more is known about the pathophysiology of ADHF and this knowledge provides us with the ability to appropriately manage patients in various scenarios. Use of intravenous ACE inhibitors can be harmful as demonstrated by the CONSENSUS 2 trial and its use in acute heart failure is discouraged. Additionally, the data in support of other vasodilators such as nitroprusside and nesiritide remains weak. Beta-blockers should be avoided in the setting of ADHF when there is evidence for hypoperfusion. Also, calcium channel blockers are not highly recommended due to their negative inotropic properties and their association with worse outcomes.
Inotropic agents have been shown to be deleterious in various circumstances surrounding ADHF and only should be considered in cases where temporary hemodynamic support is required, such as systemic hypoperfusion. Anti-arrhythmics not only provide a negative inotropic effect but also possess pro-arrhythmic qualities and thus their utilization should be avoided if possible. Glycosides have never been shown to improve mortality, even with their symptomatic benefits and cannot be recommended as first-line agents. Nonsteroidal anti-inflammatory drugs, corticosteroids, and thiazolidinediones can lead to exacerbation of heart failure via fluid retention, while phosphodiesterase inhibitors can potentiate arrhythmias. Many of the aforementioned medications require further investigation in order to fully understand their impact on the malfunctioning heart and to determine if any benefit can be derived from their utilization.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Swedberg K, et al. Effects of the early administration of enalapril on mortality in patients with acute myocardial infarction. Results of the Cooperative New Scandinavian Enalapril Survival Study II (CONSENSUS II). N Engl J Med. 1992;327(10):678–84.
Mullens W, et al. Sodium nitroprusside for advanced low-output heart failure. J Am Coll Cardiol. 2008;52(3):200–7.
O’conner CM, Starling RC, Hernandez AF, Armstrong PW, Dickstein K, Hasselblad V, et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med. 2011;365(1):32–43.
•• Prins KW, et al. Effects of beta-blocker withdrawal in acute decompensated heart failure: a systematic review and meta-analysis. JACC Heart Fail. 2015;3(8):647–53. Readers should take note of this relatively recent reference. They will surely encounter many patients on beta blockers and understanding the impact continuation and/or discontinuation can have in certain scenarios involving ADHF will be incredibly beneficial for practitioners
Goldstein RE, et al. Diltiazem increases late-onset congestive heart failure in post infarction patients with early reduction in ejection fraction. The Adverse Experience Committee; and the Multicenter Diltiazem Post infarction Research Group. Circulation. 1991;83(1):52–60.
Elkayam U, et al. Calcium channel blockers in heart failure. J Am Coll Cardiol. 1993;22(4 Suppl A):139a–44.
Elkayam U, et al. A prospective, randomized, double-blind, crossover study to compare the efficacy and safety of chronic nifedipine therapy with that of isosorbide dinitrate and their combination in the treatment of chronic congestive heart failure. Circulation. 1990;82(6):1954–61.
Singh A, et al. Agents with vasodilator properties in acute heart failure. Eur Heart J. 2016.
Petersen JW, Felker GM. Inotropes in the management of acute heart failure. Crit Care Med. 2008;36(1 Suppl):S106–11.
Cuffe MS, et al. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. JAMA. 2002;287(12):1541–7.
Katz AM. Potential deleterious effects of inotropic agents in the therapy of chronic heart failure. Circulation. 1986;73(3 Pt 2):III184–90.
Packer M, et al. Double-blind, placebo-controlled study of the efficacy of flosequinan in patients with chronic heart failure. Principal Investigators of the REFLECT Study. J Am Coll Cardiol. 1993;22(1):65–72.
Follath F, et al. Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low-output heart failure (the LIDO study): a randomised double-blind trial. Lancet. 2002;360(9328):196–202.
O’Connor CM, et al. Continuous intravenous dobutamine is associated with an increased risk of death in patients with advanced heart failure: insights from the Flolan International Randomized Survival Trial (FIRST). Am Heart J. 1999;138(1 Pt 1):78–86.
Loh E, et al. A randomized multicenter study comparing the efficacy and safety of intravenous milrinone and intravenous nitroglycerin in patients with advanced heart failure. J Card Fail. 2001;7(2):114–21.
Lowes BD, et al. Milrinone versus dobutamine in heart failure subjects treated chronically with carvedilol. Int J Cardiol. 2001;81(2–3):141–9.
Metra M, et al. Beta-blocker therapy influences the hemodynamic response to inotropic agents in patients with heart failure: a randomized comparison of dobutamine and enoximone before and after chronic treatment with metoprolol or carvedilol. J Am Coll Cardiol. 2002;40(7):1248–58.
Thackray S, et al. The effectiveness and relative effectiveness of intravenous inotropic drugs acting through the adrenergic pathway in patients with heart failure-a meta-regression analysis. Eur J Heart Fail. 2002;4(4):515–29.
Caldicott LD, et al. Intravenous enoximone or dobutamine for severe heart failure after acute myocardial infarction: a randomized double-blind trial. Eur Heart J. 1993;14(5):696–700.
Burger AJ, et al. Effect of nesiritide (B-type natriuretic peptide) and dobutamine on ventricular arrhythmias in the treatment of patients with acutely decompensated congestive heart failure: the PRECEDENT study. Am Heart J. 2002;144(6):1102–8.
Kottkamp H, et al. Clinical significance and management of ventricular arrhythmias in heart failure. Eur Heart J. 1994;15(Suppl D):155–63.
Amabile CM, Spencer AP. Keeping your patient with heart failure safe: a review of potentially dangerous medications. Arch Intern Med. 2004;164(7):709–20.
•• Echt DS, et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo. The Cardiac Arrhythmia Suppression Trial. N Engl J Med. 1991;324(12):781–8. A landmark study, the Cardiac Arrhythmia Suppression Trial (CAST), has come to serve as a fundamental principle in cardiac medicine. The increased mortality risks associated with class IC anti-arrhythmic use in the setting of ADHF is a basic fact, and practitioners in the acute setting must be cognizant of it in order to offer the best medical care possible
Hallstrom AP, et al. Time to arrhythmic, ischemic, and heart failure events: exploratory analyses to elucidate mechanisms of adverse drug effects in the Cardiac Arrhythmia Suppression Trial. Am Heart J. 1995;130(1):71–9.
Konstantinou DM, Karvounis H, Giannakoulas G. Digoxin in heart failure with a reduced ejection fraction: a risk factor or a risk marker? Cardiology. 2016;134(3):311–9.
Feenstra J, et al. Association of nonsteroidal anti-inflammatory drugs with first occurrence of heart failure and with relapsing heart failure: the Rotterdam Study. Arch Intern Med. 2002;162(3):265–70.
• Gislason GH, et al. Increased mortality and cardiovascular morbidity associated with use of nonsteroidal anti-inflammatory drugs in chronic heart failure. Arch Intern Med. 2009;169(2):141–9. Nonsteroidal anti-inflammatory drugs (NSAIDs) are such a popular and common medication amongst patients that their impact on those with heart failure should be understood. As their mechanism can potentially pose a threat to the stability of the discussed demographic, proper understanding of its potential impact would be beneficial for all involved medical personnel.
Funk CD, Fitzgerald GA. Cox-2 inhibitors and cardiovascular risk. J Cardiovasc Pharmacol. 2007;50(5):470–9.
Whitworth JA, et al. The nitric oxide system in glucocorticoid-induced hypertension. J Hypertens. 2002;20(6):1035–43.
Misbin RI. The phantom of lactic acidosis due to metformin in patients with diabetes. Diabetes Care. 2004;27(7):1791–3.
Kennedy FP. Do thiazolidinediones cause congestive heart failure? Mayo Clin Proc. 2003;78(9):1076–7.
Hartung DM, et al. Risk of hospitalization for heart failure associated with thiazolidinedione therapy: a medicaid claims-based case–control study. Pharmacotherapy. 2005;25(10):1329–36.
Gamssari F, et al. Rapid ventricular tachycardias associated with cilostazol use. Tex Heart Inst J. 2002;29(2):140–2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Heart Failure
Rights and permissions
About this article
Cite this article
Solomon, R., McCord, J. Medications to Avoid in Acute Decompensated Heart Failure. Curr Emerg Hosp Med Rep 5, 83–87 (2017). https://doi.org/10.1007/s40138-017-0134-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-017-0134-5