Abstract
Purpose
While bariatric surgery has been shown to be the most effective treatment for type-2 diabetes (T2D), recurrence following an initial period of remission is a known phenomenon. The purpose of this review is to better characterize the incidence and management of recurrent diabetes following bariatric surgery.
Recent Findings
The durability of T2D remission is heavily influenced on the severity of baseline disease, adherence to prescribed life-style modifications, and to a lesser extent, procedure type.
Summary
Recurrent diabetes following bariatric surgery is significant and challenging to manage. Therapeutic options range from medical management to revisional surgery. Treatment algorithms should follow a tiered approach, starting with the least invasive modality. Thus, a multidisciplinary approach is essential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obesity and obesity-related comorbidities (ORC) continues to increase in every region of the world with current data suggesting that an estimated 50 million girls, 74 million boys, 390 million women, and 281 million men worldwide have obesity [1]. In the United States, obesity has increased from 30.5% in 2000 to 42.4% in 2018, with severe obesity climbing to 9.2% from 4.7% [2]. Unsurprisingly, elevated body mass index (BMI) significantly increases one’s risk for the development of diabetes such that the prevalence of type-2 diabetes (T2D) has risen in lockstep with obesity [3]. Currently, the worldwide prevalence of T2D is estimated to be 9.3% (463 million people), climbing to 10.9% (700 million) by 2045 [4, 5]. Thirty-one million people are presently living with T2D in the United States [5]. The magnitude of these figures is of global pandemic status and the economic consequences and impact on personal health cannot be overstated. T2D is among the top 10 causes of death in adults with a global health expenditure estimated to be USD 727 billion [6].
Compared to medical management, bariatric surgery is more effective in treating T2D in patients with severe obesity and, in fact, it has been proposed as a potential option even for moderately obese individuals patients with mild obesity and poorly controlled T2D [7,8,9,10,11,12,13]. That said, there are a myriad of factors that influence outcomes, and response to bariatric surgery spans the continuum from attenuation to remission of T2D.
Defining Remission
Given that T2D is a chronic disease, the term ‘remission’ rather than ‘cure’ is more appropriate when describing the maximum attainable effect of any given intervention. While there is considerable heterogeneity in defining diabetes remission in the literature, the most commonly used definition for remission comes from a 2009 consensus statement by a panel of endocrinologists including experts in pediatric/adult endocrinology, diabetes education, transplantation, metabolism, bariatric/metabolic surgery, and hematology/oncology. Per the consensus statement, partial remission is defined as hyperglycemia below diagnostic thresholds for diabetes, at least 1 year’s duration, and no active pharmacologic therapy or ongoing procedures; complete remission is defined as normal glycemic measures, at least 1 year’s duration, and no active pharmacologic therapy or ongoing procedures; and prolonged remission is complete remission of at least 5 years’ duration [14].
Predicting Remission of T2D Following Metabolic Surgery
As previously mentioned, metabolic surgery has been shown to be the most effective and durable treatment for T2D. Nevertheless, not all patients with diabetes achieve remission after metabolic surgery. Acknowledgment that responder rates vary and procedure type may influence remission rates has spurred extensive research into the matter.
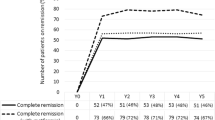
One of the most comprehensive and long-term studies providing information on the effects of bariatric surgery is the Swedish Obese Subject (SOS) study. The study prospectively followed 2010 obese subjects who underwent bariatric surgery and 2037 matched controls [15]. Patients were followed for 12–25 years starting from 1987. At 2 years, remission of diabetes was found in 72% in the surgery group versus 16.4% in controls and decreased to 30.4% and 6.5% at 15 years, respectively [15, 16]. However, the majority of patients in the SOS study underwent procedures that are no longer offered or rarely performed (i.e., vertical banded gastroplasty, non-adjustable gastric banding) [16]. The Seven-Year Weight Trajectories and Health Outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) study followed 2348 participants for 7 years. Of the participants, 1738 (74%) underwent laparoscopic Roux-en-Y gastric bypass (RYGB) and 610 (26%) underwent laparoscopic adjustable gastric banding (AGB). Remission rates of diabetes for RYGB at 1, 5, and 7 years were 71.2%, 64.6%, and 60.2%, and for AGB, 30.7%, 29.2%, and 20.3%, respectively [17]. Currently however, AGB accounts for only 1.1% of all metabolic surgery types and the most common procedures performed are the laparoscopic sleeve gastrectomy (SG) and the RYGB at 61.4% and 17%, respectively. [18].
While SG has replaced the RYGB as the most commonly performed bariatric surgery, the latter is still considered the most effective for achieving T2D remission by many experts [19]. The evidence to support this, however, has been mixed. An early randomized controlled trial involving small numbers of patients showed remission rates of 93% in patients undergoing RYGB versus 47% in LSG at 1 year [20]. In a prospectively collected cohort (PCORnet Bariatric Study (PBS)) study, investigators followed 9710 patients of which 6233 (64.2%) underwent RYGB, and 3477 (35.8%) had SG. Diabetes remission occurred in 59.2% of patients who had RYGB vs 55.9% of those who had SG at 1 year, 84.3% vs 81.5% at 3 years, and 86.1% vs 83.5% at 5 years [21∙]. In contrast, a non-randomized cohort study of 504 patients, of which 390 underwent RYGB and 134 SG, showed no significant effect of surgery type on T2D remission at 10 years [22]. Similarly, a recent meta-analysis of four randomized control trials (RCTs) compared diabetes remission in patients with mild obesity who underwent RGB or SG. There were 151 patients in the RYGB group and 145 in the SG group. Follow-up ranged from 24 to 60 months. T2D remission rates, partial and complete, were not statistically different between the two groups with 54.0% in the RYGB group and 56.7% in the SG group achieving remission [23].
As demonstrated by the above studies, variability in patient factors, remission parameters, and follow-up intervals contribute to the heterogeneity in outcomes after metabolic surgery and support the concept of a tailored approach to patient care rather than a ‘one-size fits all’ strategy. Recognition that patient factors (e.g., age, baseline BMI, severity of diabetes) significantly impact diabetes response following metabolic surgery has led to the development of several scoring systems aimed at optimizing patient selection.
Based on results of a large prospective study, the ABCD score is multidimensional grading system that calculates a score from 0 to 10 based on age, body mass index (BMI), C-peptide level, and duration of T2D. A 1-point increase in the ABCD score translates to an absolute 6.7% in the success rate of diabetes remission [24, 25]. The DiaRem (Diabetes Remission) score is an externally validated scoring model based on a retrospective study of 690 patients with diabetes that consider four preoperative clinical variables: insulin use, age, glycated hemoglobin (HbA1c), and type of antidiabetic drugs used. Scores range from 0 to 22 and are partitioned into five groups corresponding to five probability ranges for T2D remission: 0–2 (88–99%), 3–7 (64–88%), 8–12 (23–49%), 13–17 (11–33%), 18–22 (2–16%) [26, 27].
However, the predictive power of the DiaRem score is limited in patients with severe disease [28, 29]. The individualized metabolic surgery (IMS) score is a more recent prediction model based on the largest reported cohort (n = 900) with long-term (median = 7 years) postoperative glycemic follow-up. The score is based on four preoperative variables including duration of T2D, number of diabetes medications, insulin use, and glycemic control (HbA1c< 7%). The IMS score categorizes T2D into three severity stages for evidence-based procedure selection. Using this calculator, patients with milder disease severity have a similar high probability of long-term T2D remission after either procedure (RYGB or SG). In this group, the procedure choice does not need to hinge solely on the chances of T2D remission as both operations are powerful enough to achieve remission in the majority of these patients. Patients with long-standing T2D and other risk factors such as insulin use at the time of surgery and advanced age have significantly lower rates of long-term remission with either procedure. Since these patients are often higher risk surgical candidates, SG should strongly be considered since the additional risk of RYGB may not be justified based on T2D outcomes. In the moderate severity group, though, the rate long-term remission after RYGB is significantly higher than with SG and RYGB is the recommended procedure in terms of T2D outcomes. Of course, there are other patient factors that may impact the procedure choice and these must be considered alongside the benefits of T2D remission [30, 31∙∙].
Incidence of Recurrent T2D Following Metabolic Surgery
The fact that some bariatric surgery patients will experience recurrence of T2D following an initial period of regression is a known phenomenon. Like obesity, T2D is a chronic, unremitting disease and even some patients who undergo a powerful intervention such as surgery will have recurrent disease [32]. Despite recurrence of T2D in some patients, though, there is metabolic benefit from a period of tight glycemic control. This “legacy” effect results in lower long-term risk of micro- and macro-vascular complications, even in patients who have recurrent disease [33, 34∙∙].
However, attempts to capture the precise incidence of relapse are exceedingly difficult for various reasons. Many of the studies investigating the effects of bariatric surgery on T2D focus on remission of diabetes rather than relapse and those that have data regarding recurrence often report outcomes of the total cohort rather than describing only those patients who experience remission [8, 9, 11, 32, 35]. Furthermore, differences in follow-up intervals, procedure type, and definitions of recurrence make the precise incidence of relapse difficult to characterize.
The current literature shows that the durability of T2D remission following bariatric surgery is highly variable [36]. In a study of 178 patients undergoing RYGB followed for at least 10 years, 15.4% of patients were found to have recurrence [37]. A study of 1111 Danish patients with T2D treated with RYGB reported 27% recurrence at 5 years [38]. Aminian et al. reviewed outcomes in 134 patients who underwent SG followed for a median of 6 years. Relapse of T2DM after initial remission occurred in 44% [39]. A multi-institutional review of 4434 patients with uncontrolled or medication-controlled T2D who had gastric bypass reported a 35.1% rate of recurrence within 5 years [40]. In a small retrospective study, DiGiorgi et al. found that 26% of the RYGB patients who achieved remission relapsed within a mean of 6.1 years [41]. In a single-institution study of 177 patients, 89% initially achieved T2D remission after RYGB and 43% of these patients had recurrent disease at a mean of 8.6-year follow-up [42]. In a much larger retrospective review of 736 patients with T2D who underwent RYGB or SG, investigators reported a relapse rate of 32% with a median follow-up of 8 years [32].
Overall, the above studies show significant variability in the rate of T2D recurrence following bariatric surgery. Of those studies that investigated risk factors for recurrence however, predictors of relapse appear to be more consistent. In general, preoperative disease characteristics that indicate a greater severity of T2D (i.e., duration of T2D, number of diabetes medications, insulin use, higher HbA1c) portend a greater risk for recurrence over time [32, 36, 42,43,44]. A natural corollary to this observation is that patients with less severe diabetes are more likely to realize more durable remission following surgery. Furthermore, some studies indicate an association between recurrence of T2D and suboptimal weight loss and/or weight regain after surgery [41, 42, 45].
Management of Recurrent T2D Following Metabolic Surgery
While the definition varies, recurrence of T2D, most often defined as HbA1c ≥ 6.5% or need for antidiabetic medication after any period of remission, represents a therapeutic challenge [32, 46]. As is often the case in medicine, ‘prevention is the best cure’ and identifying at-risk patients for relapse is the first step in management. The aim of such a strategy is to delay diabetes relapse by attenuating risk factors. These patients, as discussed above, are likely those with more advanced diabetes and/or those that experience less than expected weight loss or even weight gain in the postoperative period. In addition to an annual HbA1c level, continued regular self-monitoring of fasting blood glucose levels should be encouraged. Moreover, strict adherence to a low-carbohydrate, low-fat, and high-fiber diet with structured exercise training is indispensable for staving off weight gain and optimizing serum glucose levels [47, 48]. As bariatric surgery patients experience significant changes in digestive physiology, appropriate screening and supplementation must be practiced to avoid micronutrient deficiencies, particularly those associated with glucose metabolism or beta-cell function such as vitamin D and chromium [49, 50].
For those patients that do recur, antidiabetic medications should ideally support weight neutrality or weight loss and avoid hypoglycemia. In this context, Metformin would be the first-line medication [51]. Glucagon-like peptide 1 (GLP-1) agonists and the newer class of sodium-glucose co-transporter 2 (SGLT2) inhibitors are also associated with weight loss, but have not been studied in post bariatric surgery patients [52, 53].
Finally, if all non-surgical attempts have been exhausted, revisional bariatric surgery for recurrent T2D should be considered in select patients. Depending on the primary procedure, revisional surgery or conversion to a bypass procedure can be as effective as primary surgery [54, 55]. Specifically, conversion of gastric operations like AGB or SG to RYGB yields improvement in diabetes in 62–79% and remission in 23–40% of patients depending on the original surgery; and revision of pouch/stoma after RYGB yields improvement of T2D in 50–79% and remission in 23% of patients [55, 56].
Conclusion
Bariatric surgery has consistently been shown to be more effective that medical management alone in the treatment of type-2 diabetes. Effectiveness of surgery, however, varies with procedure type and baseline disease severity. While remission of diabetes has been described with all bariatric procedures, the RYGB remains the gold standard. Still, recurrence rates are significant and management starts with prevention. This strategy entails identifying patients that are high risk for relapse, vigilant surveillance of serum glucose levels and weight fluctuations, adherence to life-style modifications such as diet and exercise and avoidance of nutritional deficiencies, particularly those associated with glucose metabolism.
For those patients that relapse and require pharmacotherapy, antidiabetic medications should be geared towards weight neutrality or better yet, weight loss. Medication choice, dosage, and management should be conducted by an expert. When all non-surgical strategies have been exhausted, patients should be carefully considered for revisional surgery. Specifically, those patients whose indexed procedure was restrictive (e.g., vertical banded gastroplasty, adjustable gastric band, sleeve gastrectomy) can be converted to RYGB and those patients with RYGB should be considered for stoma or pouch revision if appropriate.
In short, recurrent diabetes after initial remission following bariatric surgery is challenging. More studies are needed to identify the optimal surgical and non-surgical treatment modalities.
References
Papers of particular interest, published recently, have been highlighted as: ∙ Of importance ∙∙ Of major importance
National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Food and Nutrition Board, Roundtable on Obesity Solutions, Callahan EA. Current status and response to the global obesity pandemic: proceedings of a workshop. Callahan EA, editor. Washington (DC): National Academies Press (US); 2019 Jun 25.
National Center for Health Statistics. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. Hyattsville: National Center for Health Statistics; 2020. p. 1–8.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9(1):1197–220.
Unnikrishnan R, Pradeepa R, Joshi SR, Mohan V. Type 2 diabetes: demystifying the global epidemic. Diabetes. 2017;66(6):1432–42.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843.
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Khorgami Z, Shoar S, Saber AA, Howard CA, Danaei G, Sclabas GM. Outcomes of bariatric surgery versus medical management for type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Obes Surg. 2018;29(3):964–74.
Jakobsen GS, Småstuen MC, Sandbu R, Nordstrand N, Hofsø D, Lindberg M, et al. Association of bariatric surgery vs medical obesity treatment with long-term medical complications and obesity-related comorbidities. JAMA. 2018;319(3):291–311.
Simonson DC, Halperin F, Foster K, Vernon A, Goldfine AB. Clinical and patient-centered outcomes in obese patients with type 2 diabetes 3 years after randomization to Roux-en-Y gastric bypass surgery versus intensive lifestyle management: the SLIMM-T2D Study. Diabetes Care. 2018;41(4):670–9.
Courcoulas AP, Gallagher JW, Neiberg RH, Eagleton EB, DeLany JP, Lang W, et al. Bariatric surgery vs. lifestyle intervention for diabetes treatment: five year outcomes from a randomized trial. J Clin Endocrinol Metab. 2020;105(3):866–76.
American Diabetes Association. 8. Obesity management for the treatment of type 2 diabetes: standards of medical care in diabetes—2019. Diabetes Care. 2018;42(Supplement 1):S81–S8989.
Buse JB, Caprio S, Cefalu WT, Ceriello A, Del Prato S, Inzucchi SE, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial—a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Park JY. Prediction of type 2 diabetes remission after bariatric or metabolic surgery. JOMES. 2018;27(4):213–22.
Courcoulas AP, King WC, Belle SH, Berk P, Flum DR, Garcia L, et al. Seven-year weight trajectories and health outcomes in the longitudinal assessment of bariatric surgery (LABS) study. JAMA Surg. 2018;153(5):427–8.
American Society for Metabolic and Bariatric Surgery (2018). Estimate of Bariatric Surgery Numbers, 2011–2018. Retrieved from https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers.
Madadi F, Jawad R, Mousati I, Plaeke P, Hubens G. Remission of type 2 diabetes and sleeve gastrectomy in morbid obesity: a comparative systematic review and meta-analysis. Obes Surg. 2019;29:4066–76.
Lee W-J, Chong K, Ser K-H, Lee Y-C, Chen S-C, Chen J-C, et al. Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg. 2011;146(2):143–8.
∙ McTigue KM, Wellman R, Nauman E, Anau J, Coley RY, Odor A, et al. Comparing the 5-year diabetes outcomes of sleeve gastrectomy and gastric bypass. JAMA Surg. 2020;155:e200087–e200112200112. (Establishes the superiority of gastric bypass over sleeve gastrectomy for remission of T2D in a randomized control trial).
Jimenez A, Ibarzabal A, Moizé V, Pané A, Andreu A, Molero J, et al. Ten-year outcomes after Roux-en-Y gastric bypass and sleeve gastrectomy: an observational nonrandomized cohort study. Surg Obes Relat Dis. 2019;15(3):382–8.
Sha Y, Huang X, Ke P, Wang B, Yuan H, Yuan W, et al. Laparoscopic Roux-en-Y gastric bypass versus sleeve gastrectomy for type 2 diabetes mellitus in nonseverely obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Surg. 2020;15(5):288–311.
Lee W-J, Hur KY, Lakadawala M, Kasama K, Wong SKH, Chen S-C, et al. Predicting success of metabolic surgery: age, body mass index, C-peptide, and duration score. SOARD. 2013;9(3):379–84.
Lee W-J, Almulaifi A, Tsou JJ, Ser K-H, Lee Y-C, Chen S-C. Laparoscopic sleeve gastrectomy for type 2 diabetes mellitus: predicting the success by ABCD score. SOARD. 2015;11(5):991–6.
Still CD, Wood GC, Benotti P, Petrick AT, Gabrielsen J, Strodel WE, et al. Preoperative prediction of type 2 diabetes remission after Roux-en-Y gastric bypass surgery: a retrospective cohort study. Lancet Diabetes Endocrinol. 2014;2(1):38–45.
Aminian A, Brethauer SA, Kashyap SR, Kirwan JP, Schauer PR. DiaRem score: external validation. Lancet Diabetes Endocrinol. 2013;2(1):12–3.
Wood GC, Mirshahi T, Still CD, Hirsch AG. Association of DiaRem score with cure of type 2 diabetes following bariatric surgery. JAMA Surg. 2016;151(8):779–81.
Lee W-J, Chong K, Chen S-C, Zachariah J, Ser K-H, Lee Y-C, et al. Preoperative prediction of type 2 diabetes remission after gastric bypass surgery: a comparison of DiaRem Scores and ABCD Scores. Obes Surg. 2016;26(10):2418–24.
Aminian A, Brethauer SA, Andalib A, Nowacki AS, Jimenez A, Corcelles R, et al. Individualized metabolic surgery score. Ann Surg. 2017;266(4):650–7.
∙∙ Chen J-C, Hsu N-Y, Lee W-J, Chen S-C, Ser K-H, Lee Y-C. Prediction of type 2 diabetes remission after metabolic surgery: a comparison of the individualized metabolic surgery score and the ABCD score. Surg Obes Relat Dis. 2018;14(5):640–5. (Clarifies the importance of patient factors in determining who will benefit most from a particular type of surgery (i.e. gastric bypass vs. sleeve gastrectomy)).
Aminian A, Vidal J, Salminen P, Still CD, Nor Hanipah Z, Sharma G, et al. Late relapse of diabetes after bariatric surgery: not rare, but not a failure. Diabetes Care. 2020;43(3):534–40.
Coleman KJ, Haneuse S, Johnson E, Bogart A, Fisher D, O’Connor PJ, et al. Long-term microvascular disease outcomes in patients with type 2 diabetes after bariatric surgery: evidence for the legacy effect of surgery. Diabetes Care. 2016;39(8):1400–7.
∙∙ Sjöström L, Peltonen M, Jacobson P, Ahlin S, Andersson-Assarsson J, Anveden Å, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014;311(22):2297–8. (Highlights the importance of bariatric surgery in the role of attenuating the effects of micro and macro-vascular disease. Provides an argument that earlier surgical intervention at a lower BMI should be considered).
Dicker D, Yahalom R, Comaneshter DS, Vinker S. Long-term outcomes of three types of bariatric surgery on obesity and type 2 diabetes control and remission. Obes Surg. 2016;26(8):1814–20.
Shah A, Laferrère B. Diabetes after bariatric surgery. Can J Diabetes. 2017;41(4):401–6.
Chen Y, Corsino L, Shantavasinkul PC, Grant J, Portenier D, Ding L, et al. Gastric bypass surgery leads to long-term remission or improvement of type 2 diabetes and significant decrease of microvascular and macrovascular complications. Ann Surg. 2016;263(6):1138–42.
Madsen LR, Baggesen LM, Richelsen B, Thomsen RW. Effect of Roux-en-Y gastric bypass surgery on diabetes remission and complications in individuals with type 2 diabetes: a Danish population-based matched cohort study. Diabetologia. 2019;62(4):611–20.
Aminian A, Brethauer SA, Andalib A, Punchai S, Mackey J, Rodriguez J, et al. Can sleeve gastrectomy “cure” diabetes? Long-term metabolic effects of sleeve gastrectomy in patients with type 2 diabetes. Ann Surg. 2016;264(4):674–81.
Arterburn DE, Bogart A, Sherwood NE, Sidney S, Coleman KJ, Haneuse S, et al. A multisite study of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass. Obes Surg. 2012;23(1):93–102.
DiGiorgi M, Rosen DJ, Choi JJ, Milone L, Schrope B, Olivero-Rivera L, et al. Re-emergence of diabetes after gastric bypass in patients with mid- to long-term follow-up. SOARD. 2020;6(3):249–53.
Chikunguwo SM, Wolfe LG, Dodson P, Meador JG, Baugh N, Clore JN, et al. Analysis of factors associated with durable remission of diabetes after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2010;6(3):254–9.
Debédat J, Sokolovska N, Coupaye M, Panunzi S, Chakaroun R, Genser L, et al. Long-term relapse of type 2 diabetes after Roux-en-Y gastric bypass: prediction and clinical relevance. Diabetes Care. 2018;41(10):2086–95.
Oliveira VLP, Martins GP, Mottin CC, Rizzolli J, Friedman R. Predictors of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass in severely obese patients. Obes Surg. 2017;28(1):195–203.
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Nanni G, et al. Bariatric–metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. The Lancet. 2015;386(9997):964–73.
Pessoa BM, Browning MG, Mazzini GS, Wolfe L, Kaplan A, Khoraki J, et al. Factors mediating type 2 diabetes remission and relapse after gastric bypass surgery. J Am Coll Surg. 2020;230(1):7–16.
Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. The Lancet. 2009;374(9702):1677–86.
Umpierre D, Ribeiro PAB, Kramer CK, Leitão CB, Zucatti ATN, Azevedo MJ, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2011;305(17):1790–9.
Sacerdote A, Dave P, Lokshin V, Bahtiyar G. Type 2 diabetes mellitus, insulin resistance, and vitamin D. Curr Diab Rep. 2019;19(10):101–12.
Schlienger JL, Pradignac A, Luca F, Meyer L, Rohr S. Medical management of diabetes after bariatric surgery. Diabetes Metab. 2009;35(P2):558–61.
Stanford FC, Alfaris N, Gomez G, Ricks ET, Shukla AP, Corey KE, et al. The utility of weight loss medications after bariatric surgery for weight regain or inadequate weight loss: a multi-center study. Surg Obes Relat Dis. 2017;13(3):491–500.
O'Neil PM, Birkenfeld AL, McGowan B, Mosenzon O, Pedersen SD, Wharton S, et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. The Lancet. 2018;392(10148):637–49.
Pereira MJ, Eriksson JW. Emerging role of SGLT-2 inhibitors for the treatment of obesity. Drugs. 2019;79(3):219–30.
Daigle CR, Chaudhry R, Boules M, Corcelles R, Kroh M, Schauer PR, et al. Revisional bariatric surgery can improve refractory metabolic disease. SOARD. 2016;12(2):392–7.
Yan J, Cohen R, Aminian A. Reoperative bariatric surgery for treatment of type 2 diabetes mellitus. SOARD. 2017;13(8):1412–21.
Aleassa EM. Effect of revisional bariatric surgery on type 2 diabetes mellitus. Surg Endosc. 2019;33(8):2642–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SB reports personal fees from Speaker honoraria Medtronic, personal fees from Consultant GI Windows, outside the submitted work. JC declares no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Bariatric Surgery.
Rights and permissions
About this article
Cite this article
Chen, J., Brethauer, S. Recurrent Diabetes Following Bariatric Surgery: Incidence and Management. Curr Surg Rep 8, 24 (2020). https://doi.org/10.1007/s40137-020-00268-0
Published:
DOI: https://doi.org/10.1007/s40137-020-00268-0