Abstract
Purpose of Review
The popularity of robotic liver surgery has vastly increased in the last decade with the aim to overcome the disadvantages of laparoscopic liver surgery using inherent advantages of robotic technology including improved dexterity, enhanced range of motion and better vision. The purpose of this review is to assess the current literature on robotic liver resection and present its perioperative outcomes, oncologic outcomes, learning curve, cost effectiveness and limitations.
Recent Findings
Several articles have been published on different aspects of robotic liver resection in the recent years. High cost associated with robotic equipment is a major drawback, however, decreased perioperative morbidity and lower costs reported in recent articles hints a trend towards acceptable cost.
Summary
In terms of perioperative outcomes, robotic liver resection was reported to be superior to open liver resection and comparable to laparoscopic liver resection. Regarding oncologic outcomes, robotic liver resection was found to be equal compared to open and laparoscopic resection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Minimally invasive surgical techniques such as laparoscopic and robotic surgery have become more popular in the last decades in accordance with the development of new technologies. In general surgery, while open procedures were preferred in the past, minimally invasive techniques have become the gold standard in several procedures, such as appendectomy, cholecystectomy and adrenalectomy. Since the first laparoscopic liver resection in 1991 by Reich et al. [1], laparoscopic technique has been widely performed and shown to be safe and feasible, offering better perioperative outcomes and similar oncologic results compared to open resection [2,3,4,5,6,7]. Nevertheless, despite all the potential it showed, laparoscopic liver resection (LLR) has inherent limitations such as lack of tactile feedback, inadequate articulation and instrument clashing. In addition to this, laparoscopic technique was found to be challenging for resecting posterosuperior lesions [8]. These drawbacks of laparoscopic technique, along with advancements in robotic equipment drew the attention to robotic liver surgeries.
Robotic surgery offers better surgeon comfort and has become popular in recent years due to its numerous advantages over laparoscopy such as 3D enhanced vision, articulated instrumentation enabling increased range of motion and decreased tremor with improved dexterity [9]. Robots have been used to assist surgeries starting with prostatectomies, cardiac surgeries and with subsequent general surgical procedures [10]. Since the first description in 2003 [11], robotic liver resection (RLR) has been proven to be safe and feasible [12, 13••]. It has shown some promise to solve the problems faced in laparoscopic surgery. Although there has been a significant increase in the number of robotic liver surgeries performed, there is still scant data in the literature on this topic. Our aim is to review the current literature on robotic liver resection and assess its perioperative outcomes, oncologic outcomes, learning curve, cost-effectiveness and limitations.
Patient Selection
Louisville statement has enabled the standardization of patient selection for LLR in 2008 [14] stating that LLR can be applied to patients with solitary lesions ≤ 5 cm in segments 2 through 6. According to the Morioka Consensus in 2015 [15], patient selection criteria for LLR has been adopted for RLR. Although in these consensus statements, patients who do not match these criteria are considered as not candidates for minimally invasive liver resection, in some reviews the indication related to location of the lesion has been expanded to include all segments of the liver [16,17,18]. These reviews consider major vessels invasion and inability to tolerate pneumoperitoneum as the only contraindications to RLR [16,17,18].
Another important aspect of minimally invasive liver surgery is that it can also be safely done in elderly patients. A propensity score-matched analysis comparing outcomes of minimally invasive liver surgery to open surgery with 4021 pairs of elderly patients in each group showed that minimally invasive liver surgery decreases the risk of major morbidity (p = 0.023), length of hospital stay (p < 0.001), bleeding (p < 0.001) and bile leak(p = 0.009) [19]. The authors in this article indicated that patient age was not a limiting criterion for selection [19].
Even though surgeons using minimally invasive techniques may face a challenge in patients with high BMI, according to current literature, this does not apply to RLR. In a study by Sucandy et al. [20], the authors found out that BMI has no effect on the outcomes on RLR. Therefore, according to this study, RLR is safe and feasible even in patients with high BMI [20].
A scoring system was developed to estimate the difficulty and complexity of an operation if laparoscopic technique was to be used for a particular patient [21]. Taking factors like location of the lesions, resection plan, tumor size, proximity to major vessels and baseline liver function into account, this system calculates the estimated difficulty and helps to choose between different operation techniques. This difficulty scoring system has also been used for robotic surgery and proven to be feasible by a later study. In this study, authors stated that estimated difficulty by this system matched with reality. In addition to this, the authors revealed that robotic surgery was successful even in most difficult cases, making minimally invasive surgery applicable to challenging cases [22].
In the literature, robotic liver surgery has been noted to be more convenient to reach some lesions on right posterior segments, particularly segment 7, which is difficult to approach and resect using laparoscopic technique [23, 24]. The main reasoning behind this superiority was reported to be that in the resection of posterosuperior segments, curved and variably angulated resection lines are needed which can only be provided by articulating robotic instruments [23, 24]. Another advantage of robots for this kind of resection is that robotic cameras allow a greater magnified view which improves dexterity [23].
Perioperative Outcomes
Perioperative outcomes, such as estimated blood loss, operative time and conversion to laparoscopic or open technique, are important for the evaluation of a surgical technique. Regarding these outcomes, there is scarce data in the literature limited to retrospective studies, reviews and few meta-analysis. A meta-analysis by Machairas et al. [13••] that compared 458 patients in robotic liver resection group with 790 patients in open liver resection (OLR) group showed that RLR resulted in lower morbidity rates (p = 0.006) and shorter duration of hospital stay (p < 0.001); whereas OLR resulted in shorter operative time (p = 0.003). According to this meta-analysis, there was no significant difference in terms of blood loss and blood transfusions [13••]. The rate of conversion to open surgery in RLR was found to be 4.6% [13••]. Furthermore, another meta-analysis by Wong et al. [25] comparing RLR and OLR found similar results. Duration of hospital stay was reported to be shorter (p < 0.001) in RLR group while operative time was found to be longer (p = 0.03) [25]. In addition to this, there was no significant difference regarding blood loss [25]. The conversion rate was noted to be 4.4% [25]. As far as perioperative outcomes are concerned, we can conclude that RLR is superior or at least not inferior to OLR.
Although there are some evidence suggesting that RLR may be superior to ORL regarding the perioperative outcomes, there is only limited number of articles showing its superiority over LLR. A recent meta-analysis by Guan et al. [26] comparing 453 patients in RLR group to 503 patients in LLR group showed that RLR causes longer operative times (p < 0.001) and higher estimated blood loss (p = 0.001). However, there was no significant difference in terms of duration of hospital stay, conversion to open surgery and complication rate [26].
Oncologic Outcomes
Despite the fact that there are several studies on perioperative and short-term outcomes of RLR, there is scant data on long-term oncologic outcomes. A propensity score-matched study containing 55 patients with liver cancer each in RLR and LLR cohorts reported no significant difference in positive resection margins (11% in RLR vs 15% in LLR, p = 0.49), short term complications and long term oncologic outcomes [27]. This study included patients with malignant primary or secondary liver tumors. Another propensity score matched study containing 115 patients in RLR and LLR group by Beard et al. [28] supported these results, showing that RLR and LLR were associated with similar positive margin rates (26.3% in RLR vs 22.6% in LLR, p = 0.18), and overall survival and disease free survival, when performed for colorectal cancer metastasis. Other studies have also proven that long-term outcomes of RLR are comparable to LLR [29, 30] and ORL [9, 31].
Although there are no studies to date comparing oncologic outcomes of RLR to OLR, several studies have compared the margin positivity of LLR to OLR. Okuno et al. found no significant difference in terms of margin positivity between LLR and OLR (13.8% in LLR vs 20.7% in OLR, p = 0.73) [32]. Another study by Li et al. revealed no significant difference between two groups [33].
Learning Curve
Learning curve is defined as the number of operations required for a surgeon to reach a level of proficiency at which the surgical results are not inferior to the gold standard technique. Learning curves need to be kept in mind, when choosing a treatment modality over another. In robotic liver surgery, learning curve changes, depending on the location and size of the lesion. There are a few studies on the learning curve of robotic liver resection. A study by Chen et al. [34••] divides the learning curve into 3 parts. In the initial phase, the operative time gets shorter and in the intermediate phase estimated blood loss is reduced, while in the advanced phase, both are improved [34••]. According to this study, 15 patients are required to overcome the initial phase and 25 are needed to overcome the intermediate phase [34••]. In a more recent study, Zhu et al. reported the learning curve for RLR to be around 30 patients [35] that is significantly less than reported for LLR, which may require up to 75 patients [36,37,38]. Another study comparing the learning curves of RLR and LLR showed that the learning curve of LLR is steeper [39]. In addition, this study recommends that a surgeon should do advanced and complex robotic liver resections only after an experience of 16 low to intermediate difficulty operations, while this cutoff for LLR is suggested to be 29 [39].
Cost
The cost of an operation is important when deciding between different treatment modalities. There are contradictory reports on the cost of robotic liver resection. Several of the earlier articles have associated RLR with higher costs compared to LLR or OLR [29, 40,41,42]. On the other hand, Daskalaki et al. [43•] claimed that total cost of RLR per patient was lower than ORL. The authors attributed this difference to lower rate of ICU admission and lower nursing and medication costs [43•]. Furthermore, Sham et al. indicated that when compared to OLR, RLR results in increased perioperative, but decreased postoperative and total costs [44•]. The latter article showing decreased costs might imply that, in the future, a high cost will not be a drawback for robotic surgery.
Technique
The initial phase of robotic liver resection is patient positioning. The patient is placed supine at 20° anti-Trendelenburg and arms are adjoined to the body, which enables the robot to be docked on either side of the patients. Placement of ports largely depend on the location of the lesion, however, in general, the camera port is inserted 20 cm away from the lesion (Fig. 1). The operation starts with induction of pneumoperitoneum, followed by trocar insertion and diagnostic laparoscopy. In total, 2 or 3 additional robotic ports are then placed which is decided based on type of surgery and availability. In addition to this, an assistant port is inserted inferior and lateral to the camera port which optimizes range of motion preventing clashing with the robotic arms (Fig. 2). This assisting port is used to aspirate blood and pass in materials required. While use of and energy device such as a vessel sealer has proved to be useful, energy can be connected to most commonly used devices like Maryland and Prograsp forceps (Fig. 3).
The surgery starts with visualization of abdominal cavity with the camera to check for any additional gross pathology. Afterwards, liver is mobilized, vascular inflow and outflow is controlled and resection of target parenchyma is done in order. Mobilization of the liver requires division of falciform and coronary ligaments (Fig. 4). To divide round ligament, one can pass a loop suture around the ligament and retract it to have a better exposure of the dissection and resection plane. Coronary ligament is divided to mobilize both right and left liver lobes and to enable better outflow control by improving exposure of hepatic veins. Following these, the hepatoduodenal ligament can be encircled to prepare for a pringle maneuver to control inflow.
During right or left hepatectomy, initially, corresponding hepatic artery and portal vein are divided and transected after being ligated, clipped and stapled. Following transection, dissection lines become demarcated on liver and dissection is performed following these lines (Fig. 5). For the dissection, various energy devices such as harmonic scalpel, bipolar energy device and the Cavitron Ultrasonic Surgical Aspirator (CUSA) can be used. The choice of whether to use of pringle maneuver to decrease blood loss depends on the surgeon preference. However, during pringle maneuver, time needs to be carefully controlled and clamping should be limited to 10–15 min each time, with 5 min or longer unclamping periods in between. As the last step, hepatic veins need to be divided using a linear stapler. After resection is completed, homeostasis should be done and the presence of a possible bile leak should be carefully checked. There is no consensus on the placement of a drain at resection plane, with the decision left to surgeon’s individual choice. The resected specimen can be removed through an extension of midline trocar incision or through an additional Pfannenstiel incision. Minor operations such as minor hepatectomies and wedge resection can be performed, following the same order as in mobilization, vascular control, and parenchymal dissection.
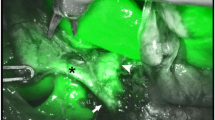
Additional helpful devices can be adapted and employed in robotic liver surgery. For example, intraoperative ultrasound can be used to investigate accompanying pathologies and determine ideal dissection planes [45]. Furthermore, use of indocyanine green (ICG) can assist in visualizing the anatomy of hepatobiliary structures and vessels so that the surgeon can find the best resection plane. There are several different methods about dosage of ICG. In a recently published article by our group, better results were obtained when 7.5 mg ICG was injected 1 day before the operation [46]. Showing tissue perfusion and lymphatic flow, ICG also helps with differentiation of healthy liver tissue from tumor [47].
Limitations
Limitations of robotic surgery include a restricted variety of instruments. Although a number of advanced instruments is available for parenchymal transection in laparoscopic and open surgery, the instruments that can be used in robotic liver surgery are restricted to vessel sealers and staplers. However, the ability to mobilize liver extensively to achieve better alignment of the port trajectory plane to resection plane in RLR may compensate for this drawback.
Conclusions
Robotic surgery has increased its penetration for minimally invasive liver resection in recent years and has the potential to offer advantages to laparoscopy. So far, it has proven to be safe and feasible and preferable to laparoscopy for the resection of posterosuperior segment lesions. In terms of perioperative outcomes, robotic liver resection was reported to be superior to open and comparable to laparoscopic liver resection. Regarding short and long-term oncologic outcomes, robotic liver resection was found to be equal compared to open and laparoscopic resection. The high cost associated with robotic equipment is a major drawback, however, decreased perioperative morbidity and lower costs reported in recent articles may help compensate for this additional cost. Although data in the literature is optimistic for RLR, to validate more promising results, the current literature is inadequate and new prospective randomized multicentric studies with larger patient numbers are needed.
References
Recently published papers of particular interest have been highlighted as: • Of importance •• Of major importance
Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991;78(5 Pt 2):956–8.
Dagher I, Di Giuro G, Dubrez J, Lainas P, Smadja C, Franco D. Laparoscopic versus open right hepatectomy: a comparative study. Am J Surg. 2009;198(2):173–7.
Khan S, Beard RE, Kingham PT, Fong Y, Boerner T, Martinie JB, et al. Long-Term oncologic outcomes following robotic liver resections for primary hepatobiliary malignancies: a multicenter study. Ann Surg Oncol. 2018;25(9):2652–60.
Morino M, Morra I, Rosso E, Miglietta C, Garrone C. Laparoscopic vs open hepatic resection: a comparative study. Surg Endosc. 2003;17(12):1914–8.
Pilgrim CH, To H, Usatoff V, Evans PM. Laparoscopic hepatectomy is a safe procedure for cancer patients. HPB. 2009;11(3):247–51.
Polignano FM, Quyn AJ, de Figueiredo RS, Henderson NA, Kulli C, Tait IS. Laparoscopic versus open liver segmentectomy: prospective, case-matched, intention-to-treat analysis of clinical outcomes and cost effectiveness. Surg Endosc. 2008;22(12):2564–70.
Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, et al. Laparoscopic versus open hepatic resections for benign and malignant neoplasms—a meta-analysis. Surgery. 2007;141(2):203–11.
Boggi U, Caniglia F, Vistoli F, Costa F, Pieroni E, Perrone VG. Laparoscopic robot-assisted resection of tumors located in posterosuperior liver segments. Updates Surg. 2015;67(2):177–83.
Ocuin LM, Tsung A. Robotic liver resection for malignancy: Current status, oncologic outcomes, comparison to laparoscopy, and future applications. J Surg Oncol. 2015;112(3):295–301.
Shah J, Vyas A, Vyas D. The history of robotics in surgical specialties. Am J Robot Surg. 2014;1(1):12–20.
Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138(7):777–84.
Sucandy I, Schlosser S, Bourdeau T, Spence J, Attili A, Ross S, et al. Robotic hepatectomy for benign and malignant liver tumors. J Robot Surg. 2019;14:75.
•• Machairas N, Papaconstantinou D, Tsilimigras DI, Moris D, Prodromidou A, Paspala A, et al. Comparison between robotic and open liver resection: a systematic review and meta-analysis of short-term outcomes. Updates Surg. 2019;71(1):39–48. Comparing outcomes of a new surgical technique with the outcomes traditionally performed surgical technique is important in analysing its advantages and weaknesses. This review and metaanalysis compares short term outcomes of robotic liver resection with open liver resection.
Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: the Louisville statement, 2008. Ann Surg. 2009;250(5):825–30.
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261(4):619–29.
Nota CL, Rinkes IHB, Molenaar IQ, van Santvoort HC, Fong Y, Hagendoorn J. Robot-assisted laparoscopic liver resection: a systematic review and pooled analysis of minor and major hepatectomies. HPB. 2016;18(2):113–20.
Qiu J, Chen S, Chengyou D. A systematic review of robotic-assisted liver resection and meta-analysis of robotic versus laparoscopic hepatectomy for hepatic neoplasms. Surg Endosc. 2016;30(3):862–75.
Salloum C, Lim C, Malek A, Compagnon P, Azoulay D. Robot-assisted laparoscopic liver resection: a review. J Visc Surg. 2016;153(6):447–56.
Tee MC, Chen L, Peightal D, Franko J, Kim PT, Brahmbhatt RD, et al. Minimally invasive hepatectomy is associated with decreased morbidity and resource utilization in the elderly. Surg Endosc. 2019. https://doi.org/10.1007/s00464-019-07298-5.
Sucandy I, Attili A, Spence J, Bordeau T, Ross S, Rosemurgy A. The impact of body mass index on perioperative outcomes after robotic liver resection. J Robot Surg. 2019;14:41.
Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y, et al. A novel difficulty scoring system for laparoscopic liver resection. J Hepato-Biliary-Pancreat Sci. 2014;21(10):745–53.
Chong CCN, Lok HT, Fung AKY, Fong AKW, Cheung YS, Wong J, et al. Robotic versus laparoscopic hepatectomy: application of the difficulty scoring system. Surg Endosc. 2020;34:2000.
Tranchart H, Ceribelli C, Ferretti S, Dagher I, Patriti A. Traditional versus robot-assisted full laparoscopic liver resection: a matched-pair comparative study. World J Surg. 2014;38(11):2904–9.
Casciola L, Patriti A, Ceccarelli G, Bartoli A, Ceribelli C, Spaziani A. Robot-assisted parenchymal-sparing liver surgery including lesions located in the posterosuperior segments. Surg Endosc. 2011;25(12):3815–24.
Wong DJ, Wong MJ, Choi GH, Wu YM, Lai PB, Goh BKP. Systematic review and meta-analysis of robotic versus open hepatectomy. ANZ J Surg. 2019;89(3):165–70.
Guan R, Chen Y, Yang K, Ma D, Gong X, Shen B, et al. Clinical efficacy of robot-assisted versus laparoscopic liver resection: a meta analysis. Asian J Surg. 2019;42(1):19–311.
Lim C, Salloum C, Tudisco A, Ricci C, Osseis M, Napoli N, et al. Short- and long-term outcomes after robotic and laparoscopic liver resection for malignancies: a propensity score-matched study. World J Surg. 2019;43(6):1594–603.
Beard RE, Khan S, Troisi RI, Montalti R, Vanlander A, Fong Y, et al. Long-term and oncologic outcomes of robotic versus laparoscopic liver resection for metastatic colorectal cancer: a multicenter, propensity score matching analysis. World J Surg. 2019;44:887.
Berber E, Akyildiz HY, Aucejo F, Gunasekaran G, Chalikonda S, Fung J. Robotic versus laparoscopic resection of liver tumours. HPB. 2010;12(8):583–6.
Lai EC, Tang CN. Long-term survival analysis of robotic versus conventional laparoscopic hepatectomy for hepatocellular carcinoma: a comparative study. Surg Laparosc Endosc Percutaneous Techn. 2016;26(2):162–6.
Chen PD, Wu CY, Hu RH, Chou WH, Lai HS, Liang JT, et al. Robotic versus open hepatectomy for hepatocellular carcinoma: a matched comparison. Ann Surg Oncol. 2017;24(4):1021–8.
Okuno M, Goumard C, Mizuno T, Omichi K, Tzeng CD, Chun YS, et al. Operative and short-term oncologic outcomes of laparoscopic versus open liver resection for colorectal liver metastases located in the posterosuperior liver: a propensity score matching analysis. Surg Endosc. 2018;32(4):1776–86.
Li N, Wu YR, Wu B, Lu MQ. Surgical and oncologic outcomes following laparoscopic versus open liver resection for hepatocellular carcinoma: a meta-analysis. Hepatol Res. 2012;42(1):51–9.
•• Chen PD, Wu CY, Hu RH, Chen CN, Yuan RH, Liang JT, et al. Robotic major hepatectomy: Is there a learning curve? Surgery. 2017;161(3):642–9. Learning curves are important aspects in the evaluation of surgical techniques as it reflects the inherent difficulty in its application. There is only scarce data about the learning curve in robotic liver resection. One of the few, this article documents the learning curve for robotic liver resection in a good number of patients.
Zhu P, Liao W, Ding ZY, Chen L, Zhang WG, Zhang BX, et al. Learning curve in robot-assisted laparoscopic liver resection. J Gastrointest Surg. 2019;23(9):1778–877.
Lin CW, Tsai TJ, Cheng TY, Wei HK, Hung CF, Chen YY, et al. The learning curve of laparoscopic liver resection after the Louisville statement 2008: Will it be more effective and smooth? Surg Endosc. 2016;30(7):2895–903.
Nomi T, Fuks D, Kawaguchi Y, Mal F, Nakajima Y, Gayet B. Learning curve for laparoscopic major hepatectomy. Br J Surg. 2015;102(7):796–804.
Vigano L, Laurent A, Tayar C, Tomatis M, Ponti A, Cherqui D. The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg. 2009;250(5):772–82.
Efanov M, Alikhanov R, Tsvirkun V, Kazakov I, Melekhina O, Kim P, et al. Comparative analysis of learning curve in complex robot-assisted and laparoscopic liver resection. HPB. 2017;19(9):818–24.
Montalti R, Berardi G, Patriti A, Vivarelli M, Troisi RI. Outcomes of robotic vs laparoscopic hepatectomy: a systematic review and meta-analysis. World J Gastroenterol. 2015;21(27):8441–51.
Packiam V, Bartlett DL, Tohme S, Reddy S, Marsh JW, Geller DA, et al. Minimally invasive liver resection: robotic versus laparoscopic left lateral sectionectomy. J Gastrointest Surg. 2012;16(12):2233–8.
Yu YD, Kim KH, Jung DH, Namkoong JM, Yoon SY, Jung SW, et al. Robotic versus laparoscopic liver resection: a comparative study from a single center. Langenbeck's Arch Surg. 2014;399(8):1039–45.
• Daskalaki D, Gonzalez-Heredia R, Brown M, Bianco FM, Tzvetanov I, Davis M, et al. Financial impact of the robotic approach in liver surgery: a comparative study of clinical outcomes and costs between the robotic and open technique in a single institution. J Laparoendosc Adv Surg Techn A. 2017;27(4):375–82. Cost of a surgical technique is important and commonly debated as it affects its accessability of the technique. Robotic surgery has always been criticised due to high cost. This article opposes the previous articles on this topic stating that robotic liver surgery has lower cost than traditional open liver resection.
• Sham JG, Richards MK, Seo YD, Pillarisetty VG, Yeung RS, Park JO. Efficacy and cost of robotic hepatectomy: is the robot cost-prohibitive? J Robot Surg. 2016;10(4):307–13. Cost of a surgical technique is important and commonly debated as it affects its accessability of the technique. Robotic surgery has always been criticised due to high cost. This article opposes the previous articles on this topic stating that robotic liver surgery has lower cost than traditional open liver resection.
Guerra F, Amore Bonapasta S, Annecchiarico M, Bongiolatti S, Coratti A. Robot-integrated intraoperative ultrasound: Initial experience with hepatic malignancies. Minim Invas Therapy Allied Technol. 2015;24(6):345–9.
Kose E, Kahramangil B, Aydin H, Donmez M, Takahashi H, Acevedo-Moreno LA, et al. A comparison of indocyanine green fluorescence and laparoscopic ultrasound for detection of liver tumors. HPB. 2019. https://doi.org/10.1016/j.hpb.2019.10.005.
Fahrner R, Rauchfuss F, Bauschke A, Kissler H, Settmacher U, Zanow J. Robotic hepatic surgery in malignancy: review of the current literature. J Robot Surg. 2019;13(4):533–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interests with respect to authorship or publication of this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Robotic Surgery.
Rights and permissions
About this article
Cite this article
Kose, E., Karahan, S.N. & Berber, E. Robotic Liver Resection: Recent Developments. Curr Surg Rep 8, 9 (2020). https://doi.org/10.1007/s40137-020-00254-6
Published:
DOI: https://doi.org/10.1007/s40137-020-00254-6