Abstract
Objective
To investigate the efficacy of transoral robotic surgery (TORS) in the treatment of Obstructive sleep apnoea patients (OSA).
Study design
Retrospective study performed at a tertiary referral hospital.
Methods
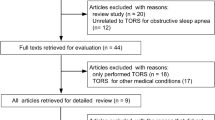
The results of 270 patients who underwent TORS procedure for OSA at our center between March 2008 and March 2017 were assessed for the change in AHI , compared to pre operative AHI and the most common complications faced intra operatively and post operatively were assessed.
Results
There was 50% reduction in AHI in 76.6% of the patients post operatively. The mean hospital stay duration was 5 days after the surgery. Post operative bleeding is the main dreaded complication , which we saw in 4.2% of our patients but only 1.7% of them required surgical intervention to stop the bleeding. The procedure is considered safe as the benefits clearly outweigh the post operative complications.
Conclusion
In selected patients, using a robot for tongue base resection or partial epiglottectomy, is really useful for treatment of patients with OSA and these areas of the human body are very difficult to visualize and operate, unless a robot is used. It was found that using a robot is not only useful , but also safe with proper training and better techniques can be developed in future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first transoral robotic surgery (TORS) for obstructive sleep apnea–hypopnea syndrome (OSAHS) was carried out in May 2008 [1••]. It was devised as a robotically assisted transoral version of Chabolle’s operation open transcervical tongue base reduction hyo-epiglottoplasty (TBRHE) for moderate-to-severe obstructive sleep apnea. After a few years, the technique was adopted with personal modifications in many ENT centers throughout the world. In 2014, the first multicenter study about TORS in which a cohort of 243 cases from 7 groups in 5 different countries was available [2]. Today, TORS is included in the surgical routine for sleep-disordered breathing (SDB) treatment in a great number of ENT departments. Although just few groups have series of more than 100 TORS cases so far, many other groups have completed more than 50 consecutive TORS for OSAHS. It is probably one of the most published techniques in tongue base area, much more popular than the open TBRHE that inspired TORS. Since March 2008 until March 2017, an overall number of 270 TORS for OSAHS were carried out in our Institution. In this chapter, we would like to summarize and present our personal experience as well as the worldwide expertise in different centers approaching OSAHS by means of robotic surgery.
Patients Selection
The oropharyngeal area, in OSAHS patients, may be considered as a unique complex anatomical entity, defined as subglosso supraglottic (SGSG) region. Its obstructive role in sleep apnea may be directly observed by awake or sedated endoscopy, as well as by imaging. Histology and geometry of the enlarged base of tongue may widely differ among different patients. If the obstructing tissue is mainly lymphoid tissue, it is a case of lingual tonsil hyperplasia and probably a simple and easy lingual tonsillectomy is the required procedure. In many other cases, a variably thin lymphoid mantle covers a true muscle enlargement, requiring a so-called tongue base debulking or reduction that, if necessary, includes the removal of a midline wedge of oral tongue. A predictable array of vessels and nerves often run inside tongue muscle mass and needs to be handled with care [3]. If the epiglottis is also considered to contribute to the airway obstruction during sleep, it may be fixed after tongue reduction. Primary or secondary obstructing epiglottis may be included in the main application of TORS. According to the patient morbid anatomy and according to the surgeon’s preference, TORS in SGSG may be included in a multi-site approach including nose surgery and palate surgery as well, in a single step setting or in pre-planned staged steps. The robot may be also be applied in palate area reshaping (palatine tonsillectomy and palate/pharyngoplasty). This approach is probably justified for training and may play a role only in case of Uvulopalatopharyngoplasty (UPPP). However, it is our opinion that palate TORS is by far less cost-effective than conventional palate surgery, and in our hands TORS was not really suitable for expansion sphincter pharyngoplasty (ESP) or barbed relocation pharyngoplasty (BRP) [4••], which is now our preferred palate procedure. It is our strong feeling that in this group of patients with severe comorbidities like high cardiovascular and neuropsychiatric risks, the use of a smart but expensive technique is justified. However, in a few cases of mild-to-moderate OSAHS but with a very huge tongue base, TORS was also used. Most of our patients are overweight males, but usually we prefer to treat patients with a pre-operative BMI less than 30. Mouth opening measured as interincisive distance of 25 mm or more is a pre-requisite for a sufficient exposure. About 70% of our cases were primary surgeries after CPAP refusal or drop out. In our center, drug-induced sedated endoscopy (DISE) is included in routine TORS work-up. It is proved to be useful for many reasons. From the strictly diagnostic point of view, DISE may offer additional information about the dynamic behaviors of base of tongue (BOT) and supraglottic area (SG). In case of significant lateral wall collapses, shown during DISE, the surgeon should avoid TORS for managing these collapses. In addition, the difficulty of the surgical exposure may also be checked.
Technique
Nasotracheal intubation must be considered the first option whenever possible. It is proved to be the most practical from the surgical point of view. In this setting, the tube is posterior to the center of the surgical field and easy to be manipulated by the head assistant. If nasal intubation is not possible, oropharyngeal intubation can be carried out. In a special group of patients, planned tracheostomy is recommended. Tracheostomy may be conventional or percutaneous, as preferred. The patient is positioned in supine position, with neck flexed and head extended (the so-called sniffing position). Routinely, a 0–0 suture is passed through the tongue body for pulling out the BOT. Our first-choice mouth-gag is Davis-Meyer or Crowe-Davis, which are preferred over FK-WO Olympus® for this type of surgery. In all but a few cases, the shortest and widest blade is preferred. We do not use teeth or soft tissue protecting devices in order to avoid any additional reduction of very narrow mouth opening as commonly observed in OSAHS patients. The next step is to insert the scope and the couple of instruments in the robotic arms. The scope is 12 mm (if available 8 mm), 30° facing up. In TORS, the bed side’s assistant is usually instructed to keep in sight the scope and instruments’ tips all the time, in order to prevent accidental tissue penetration in case of blind maneuvers. After the scope, a couple of 5 mm instruments is inserted into the arms:
-
1.
A round tip cautery.
-
2.
A Maryland forceps.
We do not routinely use any kind of LASER (Thulium or CO2) for SGSG surgery in OSAHS patients. The SGSG TORS procedure includes a couple of surgical steps in sequence:
-
1.
The Tongue Base Reduction, both sides.
-
2.
The Supra-Hyoid Horizontal Epiglottectomy.
For more details of technique, we suggest this reading: Vicini C, Hoff PT, Montevecchi F. TransOral Robotic Surgery for Obstructive Sleep Apnea, Springer, 2016 [5••].
If required the nasal obstruction is treated with septoplasty and inferior turbinoplasty or Functional Endoscopic Surgery as needed. For the surgical approach to soft palate, we currently adopted the BRP [4••].
Post-operative Management
If the patient has not undergone tracheotomy, overnight ICU stay with continued intubation can be considered per surgeon’s preference, otherwise the patient is kept under observation in the recovery room for 3–6 h after extubation, if necessary. In our Institution, we usually do not use a feeding tube, and a liquid diet is begun on first post-operative day. Continuous pulse oximetry is recommended. The patient should be monitored closely for bleeding. Post-operative intravenous steroids can help to reduce nausea, airway edema, and pain from the inflammatory response. The use of continuous intravenous analgesia with Morphine using elastomeric infuser with morphine is proved to be very useful. In our Institution, the average hospital stay is 5 days. Patients are followed closely after discharge. Diet is normalized as healing progresses, and formal therapist-directed swallowing therapy is rarely needed (<10% of cases). Post-operative polysomnography is performed once healing is complete, usually 6 months later.
Post-operative Functional Profile
In our experience, the average pain scored is below 6 measured by means of Visual Analogue Scale (VAS) in the 3 days window after the surgery. As expected in multilevel procedures, the pain is minimally higher. Our group [6] evaluated the short- and long-term swallowing outcomes following TORS for OSAHS. In the short term (1 month post-operatively), there was minimal significant impact on the swallowing function (p = 0.56) based on the MD Anderson dysphagia inventory (MDADI) questionnaire [7] (Fig. 1). The degree of dysphagia was not related to the volume of tissue removed from the BOT as demonstrated by video fluoroscopic swallow study (VFSS) (p = 0.72). There were no complaints of swallowing dysfunction in the long term (up to 32 months post-operatively), and any complaints were spontaneously resolved within 3 months post-operatively in all patients with initial abnormal findings on VFSS (Fig. 2).
Complications
The full range of complications encountered in our experience is listed in Table 1.
The safety of this approach is reasonable as the main complication (bleeding) affected 4.2% of patients (range 4.2–5.3%). However, transient dysphagia (7.2%; range 5–14%) does compromise the quality of life and must be discussed with patients preoperatively. Recently our group published a meta-analysis [8] showing also the rates of complication (Fig. 3).
Outcomes
In our meta-analysis [8], we found compelling outcomes in reducing the AHI and daytime sleepiness has been demonstrated in the current body of published studies. The rate of success, defined as 50% reduction of pre-operative AHI and an AHI <20, is achieved in up to 76.6% of patients with a range between 53.8 and 83.3% (Fig. 4). In spite of reliable predictors, the surgical response remains an area of active research.
References
References of interest which have been published recently are noted as: •• Of major importance
•• Vicini C, Dallan I, Canzi P, Frassineti S, La Pietra MG, Montevecchi F. Transoral robotic tongue base resection in obstructive sleep apnoea-hypopnoea syndrome: a preliminary report. ORL J Otorhinolaryngol Relat Spec. 2010;72(1):22–7. This paper is the first published in literature about TORS for OSAS.
Vicini C, Montevecchi F, Campanini A, Dallan I, Hoff PT, Spector ME, Thaler E, Ahn J, Baptista P, Remacle M, Lawson G, Benazzo M, Canzi P. Clinical outcomes and complications associated with TORS for OSAHS: a benchmark for evaluating an emerging surgical technology in a targeted application for benign disease. ORL J Otorhinolaryngol Relat Spec. 2014;76(2):63–9.
Vicini C, Dallan I, Canzi P, Frassineti S, Nacci A, Seccia V, Panicucci E, La Pietra MG, Montevecchi F, Tschabitscher M. Transoral robotic surgery of the tongue base in obstructive sleep Apnea-Hypopnea syndrome: anatomic considerations and clinical experience. Head Neck. 2012;34(1):15–22.
•• Vicini C, Hendawy E, Campanini A, Eesa M, Bahgat A, AlGhamdi S, Meccariello G, DeVito A, Montevecchi F, Mantovani M. Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study. “We are on the giant’s shoulders”. Eur Arch Otorhinolaryngol. 2015;272(10):3065–70. This paper explain the importance of the multilevel surgery in OSAS patients. In many cases during TORS on the tongue base is necessary to treat the palate as well.
•• Vicini C, Hoff P, Montevecchi F, eds. TransOral Robotic Surgery for Obstructive Sleep Apnea. Springer; 2016. ISBN: 978-3-319-34038-8 (Print) 978-3-319-34040-1 (Online). In this book is possible to find all the information for selection, treatment and follow-up of the patients possible candidates for robotic surgery.
Eesa M, Montevecchi F, Hendawy E, D’Agostino G, Meccariello G, Vicini C. Swallowing outcome after TORS for sleep apnea: short- and long-term evaluation. Eur Arch Otorhinolaryngol. 2015;272(6):1537–41.
Chen AY, Frankowski R, Bishop-Leone J, Hebert T, Leyk S, Lewin J, Goepfert H. The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M. D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg. 2001;127(7):870–6.
Meccariello G, Cammaroto G, Montevecchi F, Hoff PT, Spector ME, Negm H, Shams M, Bellini C, Zeccardo E, Vicini C. Transoral robotic surgery for the management of obstructive sleep apnea: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2016; doi:10.1007/s00405-016-4113-3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Robotic Surgery.
Rights and permissions
About this article
Cite this article
Vicini, C., Montevecchi, F., Dachuri, S. et al. Transoral Robotic Surgery for Obstructive Sleep Apnea Syndrome: 9 Years of Experience. Curr Surg Rep 5, 12 (2017). https://doi.org/10.1007/s40137-017-0175-4
Published:
DOI: https://doi.org/10.1007/s40137-017-0175-4