Abstract
Purpose of Review
To review the current state of development of fully implanted cochlear implants, including a summary of the current challenges and limitations in addition to breakthroughs in technology.
Recent Findings
Recent developments towards the realization of a fully implanted cochlear implant draw from technologies that were originally developed for middle ear implants. Advances in the field of implantable microphone technologies and sustainable energy sources have led to the development of a new and novel fully implanted cochlear implant.
Summary
Advances in fully implanted cochlear implant technology are heading towards the realization of commercially available devices. Middle ear microphone technologies provide adequate amplification of sound while avoiding some of the limitations of prior subcutaneous microphones. While a fully implantable sustainable energy source is not yet developed for implantation, several recent studies show promise for eventually eliminating the need for an external charging device.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A cochlear implant (CI) is the gold standard treatment for advanced sensorineural hearing loss. Through direct stimulation of the auditory nerve, CIs can bypass the inner ear and provide input that is interpreted as sound by the brain. Since the first iteration of CIs were implanted in the early 1960s, significant developments have been made to improve both the internal and external components to optimize patient performance. Current commercially available CIs are semi-implantable, utilizing an external sound processor that sends signals to the internal receiver and electrode. Despite the strong and long-standing desire of patients to have an “invisible” hearing solution, there are no commercially available devices that achieve this.
Over the past decade, several advancements have been made to develop a fully implanted cochlear implant (FICI), eliminating the need for an externally worn sound processor. The need for a FICI stems from many of the constraints inherent to requiring external hardware. The risk of damaging or losing the external processor precludes use under certain situations, such as sleeping, strenuous physical activity or water exposure. Discomfort can arise and even lead to skin breakdown because of the need for an internal magnet to affix the external hardware to the head. Additionally, given the need for an internal magnet, MRI scanning requires extra technical safety precautions and significant imaging artifact can arise with MR imaging, potentially limiting the ability to provide adequate diagnostic imaging. Various techniques may be employed to minimize the amount of artifact produced by the internal magnet, but constraints in visualization of a lesion of interest still apply. Lastly, adverse events such as magnet displacement, demagnetization and tilt may result from MR imaging, leading to significant pain for the patient and potential loss of external hardware retention. These events occur at a relatively common rate of around 11% of patients [1].
Fully implantable hearing rehabilitation devices have been an expanding area of research and development over the past several decades. Studies examining the rate of conventional hearing aid utilization suggest that only one-third of patients who would benefit from them actually use them [2]. To address some of the barriers to the use of conventional hearing aids, middle ear implant (MEI) devices have been developed to provide an alternative option for patients with conductive, sensorineural or mixed hearing loss. Many of the advancements in this area have contributed to the development of a FICI, primarily with the development of various microphone technologies that bypass the need for a separate external microphone.
This review will detail the current status of FICIs, and will include an overview of the recent literature regarding the development of these devices. To understand the development of fully implantable hearing rehabilitation devices, it is important to include a brief discussion on the development of MEIs, as many of the advancements in this area have contributed to the development of FICIs.
Influence of Middle Ear Implants
MEIs have been available for use in patients with conductive and/or sensorineural hearing loss for the better part of the last 3 decades. The primary devices that have received FDA approval and are used in the United States include the Envoy Esteem, Med-El Vibrant SoundBridge, and the Ototronix MAXUM system [3•]. MEIs typically utilize an electromagnetic or piezoelectric transduction mechanism, and the coupling site differs by manufacturer. The Envoy Esteem utilizes a piezoelectric sensor that is coupled to the incus, an implanted amplifying sound processor, and a piezoelectric driver that is coupled to the stapes head. The Med-El Vibrant SoundBridge utilizes a floating mass transducer to produce mechanical vibrations coupled to various middle ear structures. The Ototronix MAXUM system utilizes an electromagnetic system that transmits a mechanical signal via an implant magnet that is coupled to the stapes. The Envoy Esteem is the only fully implanted MEI currently available for commercial use. Previous studies have reported satisfactory audiologic outcomes and patient satisfaction with all three MEI devices [4••, 5, 6]. Despite this, MEIs have not gained a substantial market presence due to various factors, including need for and cost of surgery, lack of insurance coverage, and the potential need for additional procedures, particularly with the Envoy Esteem’s nonrechargeable battery.
One of the primary contributions from MEIs to FICIs is the power supply required for a fully implantable hearing rehabilitation device. The Envoy Esteem utilizes a nonchargeable lithium battery that is reported to last 4.9 years when utilized most of the day [7]. The Cochlear Carina was another MEI that stopped distribution in 2020. The device worked through transducer coupling to either the incus, stapes, or round window. This device utilized a rechargeable lithium battery that reported a battery life of at least 10 years [8]. Lithium battery technology could be used an energy source for FICIs, though the finite battery lifetime introduces the added costs and risks of additional operative procedures, including the potential for device infections. Future directions for the development of sustainable energy sources for FICIs will be discussed in more detail later in this review.
The development of implantable MEIs has resulted in advancements in technologies that are leveraged in the development of FICIs. The Envoy Acclaim is a novel FICI currently being evaluated in an early feasibility study that utilized pre-existing MEI components, namely an implantable, rechargeable battery and ossicle integrated microphone. To that end, we will next discuss developing microphone technologies for FICIs and the current developmental status of these devices.
Microphone Technologies
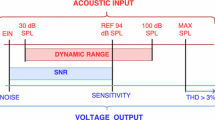
The primary challenge to developing FICIs is the need for an implantable microphone that will effectively transmit sound and speech to the receiver/stimulator. In traditional CIs, the microphone is housed in the external sound processor hardware, transmitting digitized sound signal via the transmitting coil across the skin to the internal receiver/stimulator for stimulation of the auditory nerve through the cochlear electrode. Various types of implantable microphones have been developed over the past several years to act as sensors that are capable of capturing external sounds. Different types of transduction mechanisms exist for these implantable microphones, including electromagnetic, piezoelectric and capacitive, with potential implantation subcutaneously or within the middle ear.
Calero et al. reviewed these various mechanisms and proposed a classification system of the various types of implantable microphones [9•]. Implantable microphones were first categorized into site of placement of the microphone (subcutaneous versus middle ear), then further classified based on transduction mechanism and sensor type. A comprehensive review analyzes each sensor type, with the authors’ final conclusion being that microelectromechanical systems (MEMS) technology with microphone coupling to the ossicular chain is likely to produce the best result for FICIs. Prochazka et al. have developed a packaging concept that shows promise for incorporating a MEMS microphone into a FICI, utilizing a surgically implantable titanium structure that houses the MEMS microphone [10].
The primary drawbacks for subcutaneous placement of implantable microphone technologies include microphone sensitivity due to skin thickness and implant positioning, responsiveness to physiologic noise and soft-tissue movement, overlying skin necrosis with the potential for microphone extrusion, and limitations to sound localization as a result of microphone implant location [11]. Middle ear microphone placement via coupling to ossicular chain, on the other hand, has several advantages. Placement in the middle ear allows for utilization of the ear’s natural ability amplify sounds via the pinna and ear canal, and to localize sound based on inherent directionality. Self-stimulation of the microphone by physiologic sounds would also be limited because of the middle ear reflex. Additionally, given the location of placement within the middle ear, the risks of skin necrosis and microphone extrusion would be eliminated. Mitchell-Innes et al. published a review on implantable microphone systems in 2017, within which a summary of the benefits and drawbacks to location of microphone placement is provided based on foundational studies on the topic [11].
Expanding on the benefits of a middle ear microphone system for use in FICIs, Craddock et al. recently performed a pilot study comparing audiologic performance between a traditional external CI microphone to a middle ear microphone coupled to the incus body [12•]. The middle ear microphone system demonstrated comparable results to the external microphone in sound-field testing, loudness scales, and speech reception, particularly in the lower frequencies. Notably, the middle ear microphone system demonstrated poorer performance in higher frequencies, but the authors found that study participants still found clinical benefits, highlighting the potentials of utilizing a middle ear microphone for FICIs.
More recently, a handful of studies have evaluated the use of piezoelectric middle ear microphone systems for use in FICIs. Xu et al. describe a floating piezoelectric microphone that was coupled to the ossicular chain in both cats and humans [13•]. Intraoperative testing of this microphone confirmed effective conversion of acoustic vibrations of the ossicular chain to electrical signals. Zhang et al. describe a piezofilm microphone system referred to as DrumMic that is coupled to the umbo [14•]. In this cadaveric study, the DrumMic system showed promising results with regards to sound amplification, but further development is needed towards a prototype that will be implantable in humans. Yeiser et al. describe another piezoelectric microphone that is coupled to the umbo, referred to as UmboMic, that demonstrated promising amplification results in their cadaveric study [15•].
The development of an implantable microphone system for use in FICIs is an active area of research, with most of the literature pointing towards the use of a middle ear microphone system. Various transduction mechanisms and sensor types are being explored, with the most ideal configuration yet to be determined.
Status of Fully Implanted Cochlear Implants
FICIs have been in development for many years, but as of the time of this review, there is not a commercially available device ready for implantation. There are several benefits to a FICI, as outlined earlier, that would make these devices superior to current semi-implantable CIs. In their recent review, Trudel and Morris outline the fundamental requirements to designing a FICI [16•]. The primary challenges include the development of an effective implantable microphone and a sustainable source of energy.
The status of implantable microphones was discussed in detail in the prior section. Regarding sustainable sources of energy, Trudel and Morris discuss the possibility of utilizing implantable energy harvesters as a potential source of energy. These devices would utilize sources of energy near the temporal bone to generate electrical signals delivered to the cochlear implant electrode array. Piezoelectric energy harvesters have previously been described as potential solutions, designed to convert vibrations via the tympanic membrane or basilar membrane into energy without the need for an external source [17,18,19,20]. Endocochlear potential has also been described as a potential source of energy, though current technologies do not allow for long-term, sustainable energy generation [21]. Advancements in implantable energy harvester technologies are necessary prior to the development of a self-powered FICI, but there appears to be promise in the area of piezoelectric energy harvesters.
As of today, little has been published on the design or use of an actual FICI in human recipients. The cochlear TIKI described by Briggs et al. represents the first such attempt at a commercially feasible device [22•]. Three adults with severe-profound sensorineural hearing loss were implanted with the device. The device offered the option of using a conventional external sound processor or an “invisible hearing” mode, allowing the implant recipient to continue to use the device without any external hardware. Per the report, patients received expected benefits from the implant; however, the “invisible hearing” mode relied on a subcutaneous microphone that unfortunately attenuated external sounds while amplifying body sounds, limiting its use in the fully implanted mode.
The Envoy Acclaim is the most recent FICI to have been implanted in human subjects. Dornhoffer et al. describe implantation of the device in a recently published early feasibility study [23••]. The Envoy Acclaim utilizes a middle ear microphone system that has been used in the Envoy Esteem MEI. The device’s sensor converts vibrations of the ossicular chain to an electrical signal that is delivered via a standard cochlear electrode array. The device requires an external energy source, as it employs a rechargeable internal battery placed in the chest like a pacemaker. The battery is recharged with an external charger. The report by Dornhoffer et al. focuses primarily on implantation technique and challenges, and further studies are required to determine if the Envoy Acclaim’s performance is equivalent or superior to a traditional semi-implantable CI. Patients have not reported any bothersome body sounds related to the microphone, a finding that limited the use of the TIKI. This is not surprising as the Envoy Acclaim utilizes the same system as the Envoy Esteem that has been previously implanted in many patients.
Conclusions
Several limitations to the traditional semi-implantable CI have driven the development of FICIs. MEIs have been commercially available for years, and lessons learned from the technologies incorporated into them can help drive the development of FICIs. The primary limitations to developing FICIs include 1) the need for an implantable microphone that can compete with the external hardware currently being utilized by semi-implantable CIs, and 2) the need for an implantable power supply. Several configurations for implantable microphone technologies currently exist, with the most promising being those that are implanted in the middle ear with coupling to the ossicular chain. Developing technologies for a sustainable source of energy that does not require external charging seem to be heading in the direction of energy harvesters. The Envoy Acclaim is the most recently developed FICI to have published reports on the feasibility of implantation in adults. While further studies are needed to determine its full audiological benefit, initial experiences are reportedly favorable. While FICIs have been in development for years, recent breakthroughs suggest that we are now close to having FICIs commercially available as a hearing rehabilitation option for patients with advanced sensorineural hearing loss, a solution long sought by patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fussell WL, Patel NS, Carlson ML, Neff BA, Watson RE, Lane JI, et al. Cochlear implants and magnetic resonance imaging: experience with over 100 studies performed with magnets in place. Otol Neurotol. 2021;42(1):51–8. https://doi.org/10.1097/MAO.0000000000002866.
Bainbridge KE, Ramachandran V. Hearing aid use among older U.S. adults. Ear Hear. 2014;35(3):289–94. https://doi.org/10.1097/01.aud.0000441036.40169.29.
• BanakisHartl RM, Jenkins HA. Implantable Hearing Aids: Where are we in 2020? Laryngoscope Investig Otolaryngol. 2020;5(6):1184–91. https://doi.org/10.1002/lio2.495. This manuscript reviews the state of various middle ear implants. Notably, it offers insight into various techniques for sound collection (e.g. sensor location), battery life, and challenges to the development of these technologies. Notable challenges have been issues related to feedback or body sounds from middle ear sensors and often equivocal outcomes compared to traditional hearing aids.
•• Shohet JA, Gende DM, Tanita CS. Totally implantable active middle ear implant: Hearing and safety results in a large series. Laryngoscope. 2018;128(12):2872–8. https://doi.org/10.1002/lary.27246. This study reviews results from 166 patients that underwent placement of the Envoy Esteem middle ear implant. Patients were followed an average of 35.7 months after implantation. Audiological outcomes are generally favorable. Germane to the discussion of fully-implanted cochlear implants, is that the authors report a low surgical and long-term risk profile.
McRackan TR, Clinkscales WB, Ahlstrom JB, Nguyen SA, Dubno JR. Factors associated with benefit of active middle ear implants compared to conventional hearing aids. Laryngoscope. 2018;128(9):2133–8. https://doi.org/10.1002/lary.27109.
Spiegel JL, Kutsch L, Jakob M, Weiss BG, Canis M, Ihler F. Long-term stability and functional outcome of an active middle ear implant regarding different coupling sites. Otol Neurotol. 2020;41(1):60–7. https://doi.org/10.1097/MAO.0000000000002418.
Kraus EM, Shohet JA, Catalano PJ. Envoy Esteem Totally Implantable Hearing System: phase 2 trial, 1-year hearing results. Otolaryngol Head Neck Surg. 2011;145(1):100–9. https://doi.org/10.1177/0194599811401709.
Pulcherio JOB, Bittencourt AG, Burke PR, Monsanto RDC, De Brito R, Tsuji RK, et al. Carina® and Esteem®: A Systematic Review of Fully Implantable Hearing Devices. PLoS ONE. 2014;9(10): e110636. https://doi.org/10.1371/journal.pone.0110636.
• Calero D, Paul S, Gesing A, Alves F, Cordioli JA. A technical review and evaluation of implantable sensors for hearing devices. Biomed Eng Online. 2018;17(1). https://doi.org/10.1186/s12938-018-0454-z. This article offers a technical review of existing implantable sensor technologies. It considers both sensor effectiveness and complexity of implantation. In general, middle ear sensors outperform subcutaneous sensors in both gain and lowered background or body noises. However, these benefits do come at the cost of greater complexity of implantation, with theoretically increased perioperative risk to neuroanatomical structures.
Prochazka L, Huber A, Dobrev I, Harris F, Dalbert A, Röösli C, et al. Packaging technology for an implantable inner ear MEMS microphone. Sensors. 2019;19(20):4487. https://doi.org/10.3390/s19204487.
Mitchell-Innes A, Morse R, Irving R, Begg P. Implantable microphones as an alternative to external microphones for cochlear implants. Cochlear Implants Int. 2017;18(6):304–13. https://doi.org/10.1080/14670100.2017.1371974.
• Craddock LC, Hodson J, Gosling A, Cooper S, Morse RP, Begg P, et al. Comparison of an implantable middle ear microphone and conventional external microphone for cochlear implants: A clinical feasibility study. Otol Neurotol. 2022;43(10):1162–9. https://doi.org/10.1097/MAO.0000000000003713. This study compared the effectiveness of external and implantable middle ear microphones for cochlear implants. Six implant users had middle ear microphones implanted to compare efficacy between the two microphone locations. Speech recognition at conversational levels was equivalent between the two conditions. However, the middle ear microphones underperformed with soft-level speech and at high tone thresholds.
• Xu XD, Zhang WX, Jia XH, Wu YZ, Kang HY, Chi FL, et al. A new floating piezoelectric microphone for fully implantable cochlear implants in middle ear. Laryngoscope. 2024;134(2):937–44. https://doi.org/10.1002/lary.30861. This study describes the efficacy of a newly developed floating piezoelectric microphone using in vivo testing of both cat and human patients. The results of the study show promising results with regards to the microphone’s feasibility for use in fully implanted cochlear implants.
• Zhang JZ, Graf L, Banerjee A, Yeiser A, McHugh CI, Kymissis I, et al. An implantable piezofilm middle ear microphone: performance in human cadaveric temporal bones. J Assoc Res Otolaryngol. 2024. https://doi.org/10.1007/s10162-024-00927-4. This study examines the conceptual efficacy of the DrumMic, a new piezofilm microphone under development, through testing in cadaveric temporal bones. Continued work is needed prior to in vivo testing in humans, but the approach is a promising option given the audiometric performance determined in this study.
• Yeiser AJ, Wawrzynek EF, Zhang JZ, Graf L, McHugh CI, Kymissis I, et al. The UmboMic: A PVDF cantilever microphone. ArXiv. 2023. https://doi.org/10.48550/arXiv.2312.14339. This study describes the UmboMic, a new piezoelectric cantilever microphone made of polyvinylidene difluoride (PVDF) that is designed specifically for use in fully implanted cochlear implants. The reported audiometric performance—as measured through cadaveric temporal bone studies--shows that this microphone technology may be promising option for use in fully implanted cochlear implants.
• Trudel M, Morris DP. The remaining obstacles for a totally implantable cochlear implant. Curr Opin Otolaryngol Head Neck Surg. 2022;30(5):298–302. https://doi.org/10.1097/MOO.0000000000000840. This review examines the challenges that have prevented the development of a fully implantable cochlear implant up until this point. Per the article, recent breakthroughs in both energy supply and implantable microphone technology have made the development of a fully implanted cochlear implant more feasible than ever before.
İlik B, Koyuncuoğlu A, Şardan-Sukas Ö, Külah H. Thin film piezoelectric acoustic transducer for fully implantable cochlear implants. Sens Actuators A Phys. 2018;280:38–46. https://doi.org/10.1016/j.sna.2018.07.020.
Lee HS, Chung J, Hwang GT, Jeong CK, Jung Y, Kwak JH, et al. Flexible inorganic piezoelectric acoustic nanosensors for biomimetic artificial hair cells. Adv Funct Mater. 2014;24(44):6914–21. https://doi.org/10.1002/adfm.201402270.
Jang J, Lee J, Woo S, Sly DJ, Campbell LJ, Cho J-H, et al. A microelectromechanical system artificial basilar membrane based on a piezoelectric cantilever array and its characterization using an animal model. Sci Rep. 2015;5(1):12447. https://doi.org/10.1038/srep12447.
Koyuncuoğlu A, İlik B, Chamanian S, Uluşan H, Ashrafi P, Işık D, Külah H. Bulk PZT cantilever based MEMS acoustic transducer for cochlear implant applications. Proceedings. 2017;1(4). https://doi.org/10.3390/proceedings1040584.
Mercier PP, Lysaght AC, Bandyopadhyay S, Chandrakasan AP, Stankovic KM. Energy extraction from the biologic battery in the inner ear. Nat Biotechnol. 2012;30(12):1240–3. https://doi.org/10.1038/nbt.2394.
• Briggs RJ, Eder HC, Seligman PM, Cowan RS, Plant KL, Dalton J, et al. Initial clinical experience with a totally implantable cochlear implant research device. Otol Neurotol. 2008;29(2):114–9. https://doi.org/10.1097/MAO.0b013e31814b242f. This study details the implantation of three adult patients with an experimental FICI that utilized a subcutaneous microphone for sound capture without an external device. Patients obtained open-set speech benefits, but attenuation from the subcutaneous microphone and chronic body sounds limited use of the device in the intended fully implantable mode.
•• Dornhoffer JR, Lawlor SK, Saoji AA, Driscoll CLW. Initial Experiences with the Envoy Acclaim((R)) Fully Implanted Cochlear Implant. J Clin Med. 2023;12(18). https://doi.org/10.3390/jcm12185875. This study details the implantation of 3 adult patients with the Envoy Esteem FICI. This device utilizes modular parts including an implantable rechargeable battery pack, a sensor coupled to the ossicular chain, and a sixteen electrode cochlear implant. In this manner, it obviates the need for any external components.
Funding
None.
Author information
Authors and Affiliations
Contributions
E.B., J.D. and C.D. performed the literature review and wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare no conflict interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Babajanian, E.E., Dornhoffer, J.R. & Driscoll, C.L.W. Fully Implanted Cochlear Implants. Curr Otorhinolaryngol Rep 12, 61–65 (2024). https://doi.org/10.1007/s40136-024-00507-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-024-00507-3