Abstract
Purpose of Review
This paper aims to describe the available in vitro and in vivo models of different sinonasal cancer subtypes as tools both for improving our knowledge of the signaling pathways involved in tumorigenesis and for evaluating the response to candidate therapeutic inhibitors in a preclinical setting.
Recent Findings
Starting as far back as 1981, in vitro tumor models have been established from sinonasal malignancies. However, especially in the last decade, new cell lines have been presented fully annotated with clinical and genetic data, making them ideal for testing candidate anti-cancer agents targeting specific oncogenic signaling pathways. In addition, first attempts have been made to create three-dimensional organoid cultures and mouse models, which may better reflect the cellular heterogeneity and architecture of the patients’ tumors.
Summary
Experimental models representing various sinonasal cancer subtypes are available and may help to bridge the gap between laboratory investigation and clinical application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The nasal and paranasal cavities harbor a great histological diversity of cancer types, the most frequent include squamous cell carcinoma (SNSCC), undifferentiated carcinoma (SNUC), and malignant mucosal melanoma (MMM) arsing mainly in the nasal cavity and maxillary sinus, and intestinal-type adenocarcinoma (ITAC), neuroendocrine carcinoma (SNEC), and olfactory neuroblastoma (ONB) mainly in the ethmoid sinus. The standard treatment of most sinonasal cancers is surgery followed by complementary radiotherapy. SNUC, SNEC, sarcomas, and many locoregionally advanced tumors including SNSCC and ONB are also treated with conventional chemotherapy using cisplatin, 5-FU, or Taxane [1]. Endoscopic approaches have improved patient recovery and reduced complications, while imaging and radiotherapeutic techniques have become more precise. Still, clinical management remains a challenge due to the close proximity of delicate organs as eyes and brain [2, 3].
Overall survival ranges between 20 and 60% at 5 years, depending on tumor subtype and stage. Recurrences are the main cause of death, while lymph node metastasis are infrequent. A practical approach for neoadjuvant, concomitant or adjuvant therapy would be the application of modern inhibitors of molecular targets that have shown good clinical responses in other more frequent tumor types with the same or similar genetic aberrations. Such targets can be proteins involved in signaling pathways that regulate cell proliferation, differentiation, apoptosis, invasion or response to the immune system [4, 5•]. To date, however, sinonasal cancer patients have mostly been excluded from the testing of these modern targeted therapies in clinical trials.
Several preclinical models representing various sinonasal cancer subtypes have become available and may help to bridge the gap between laboratory investigation and clinical application. In this review, we will present an overview of published cell lines and animal models with an emphasis on those that have been characterized on the genetic level. In vitro models are evolving from two-dimensional cell lines to three-dimensional organoid cultures which retain much of the cellular and genetic heterogeneity of their original tumors and are better able to predict the efficacy of inhibitory drugs targeting cellular pathways deregulated by genetic alterations. Such drugs may have cytostatic or cytotoxic effects, or may be able to induce cell maturation toward a normal adult differentiation. We will briefly point to recent, still unpublished, efforts to create organoid models of sinonasal tumors.
Sinonasal Cancers are a Histologically and Genetically Diverse Group of Rare Tumors
With a combined incidence of approximately 0.5 patients/100,000 inhabitants [6,7,8] sinonasal cancers are officially recognized as rare tumors. Moreover, there are a large number of cancer subtypes, each with their own clinical, histological, and genetic characteristics, making it difficult for clinicians to obtain experience with diagnosis and treatment [9].
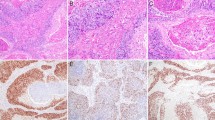
It may be speculated that the great histological variety of sinonasal tumors is related to the fact that normal stem cells in the sinonasal epithelium are capable of differentiating into various adult cell types, including squamous, glandular, mesenchymal, neuroendocrine, and even neuronal cells [10], and when transformed into malignant cells, they give rise to histologically very different tumors. Alternatively, differentiated lineage-specific cells may suffer malignant transformation and subsequently acquire stem-cell properties. Yet, another possibility is a proces of transdifferentiation. A good example is ITAC, thought to arise respiratory/olfactory mucosa changing to intestinal differentiation, possibly via a premalignant intestinal metaplasia stage [11, 12]. These tumors truly display intestinal differentiation with the same four recognized subtypes, papillary, colonic, solid and mucinous (including signet ring cells) as known in gastro-intestinal adenocarcinomas. Sinonasal tumors can also frequently display more than one histological appearance at the time of presentation, e.g., SNSCC/SNEC [13,14,15,16], human papilloma virus (HPV) positive SCC/SNEC [17], ITAC/SNEC [18, 19], ONB/ITAC [20], ONB/SCC/Adenocarcinoma [21], ONB/SNEC [22]. Perhaps most telling is teratocarcinocarcinoma (TCS), defined as an admixture of epithelial, mesenchymal, neuroendocrine and germ cell elements. In addition, premalignant inverted papilloma (ISP) has been reported in collision with SNUC and SNEC [22,23,24,25]. Finally, there are published cases where locoregional recurrences are of a different histological subtype than their corresponding primary tumors, for example ITAC recurring as SNUC, ONB or SNUC recurring as non-ITAC adenocarcinoma, or ISP recurring as SNUC [26,27,28].
From the available studies to date, we know that within the group of sinonasal cancers, individual histological subtypes are different at the genetic level. MMM show recurrent mutations in genes of the MEK pathway (e.g., NRAS, NF1), ITAC in genes of WNT (e.g., APC, CTNNB1), DNA repair (e.g., BRCA1/2, ATM), MEK (e.g., KRAS, NF1) and PI3K (e.g., PIK3CA, MTOR) pathways, SNSCC in the gene EGFR and SNUC in the gene IDH2.
Generally speaking, none of these genetic aberrations occur in high frequencies or exclusively in one tumor type. However, some tumor-specific chromosomal translocations [29] and gene mutations [5•, 30, 31] are strongly associated with specific tumor types. Examples are BRD4::NUTM1 fusion in Nuclear protein in testis (NUT) carcinoma, DEK::AFF2 fusion in Non-keratinizing SNSCC, SMARCB1 mutations/deletions in SMARCB1-deficient carcinoma and SMARCA4 mutations in TCS and subsets of SNUC and SNEC [32,33,34,35]. A few genetic alterations including mutations in TP53, CDKN2A, FANCA, and NOTCH and amplification of FGFR1 may be common in various sinonasal tumor types [36].
Poorly differentiated histology is a frequent phenomenon in sinonasal tumors [37, 38••]. Undifferentiated cells in the tumors do not mature to their normal adult function, contributing to uncontrolled cell growth. It has been shown that epigenetic events such as DNA or histone methylation often result in a block in cellular differentiation [39]. Still, few epigenetic studies have been published on sinonasal tumors, showing recurrent alterations in genes involved in epigenetic processes identified in sinonasal tumors include IDH2, SMARCB1, SMARCA4, and ARID1A [40,41,42,43,44]. A promising new application for methylation analysis is with tumor classification. Jurmeister et al. showed the diagnostic potential of unique DNA methylation profiles in a large set of sinonasal tumor types [45••].
Knowledge of genetic and epigenetic characteristics is crucial for the development of personalized therapies and for the inclusion in clinical studies testing modern treatments against molecular targets [4, 46, 47••]. A number of the above-described genetic alterations in sinonasal cancer are already used as targets for therapies in more common and better characterized cancers, and thus may also be considered for treatment of sinonasal cancer patients. Further basis for the potential efficacy of candidate therapies can be obtained from preclinical tumor models. The following paragraphs will describe the available in vitro and in vivo models of different histological sinonasal tumor subtypes, and they are summarized in Table 1.
Keratinizing Squamous Cell Carcinoma (SNSCC) and Inverted Papilloma (ISP)
This subtype is the most frequent and best-studied sinonasal tumor, arising mostly in the maxillary sinus and the lower nasal cavities. Premalignant inverted papilloma (ISP) and ISP-associated SNSCC carry frequent (30–91%) EGFR exon 20 mutations and appear to carry a better prognosis than wildtype tumors [48, 49]. HPV infection has been described in 38% of ISP and 31% of SNSCC, possibly occurring mutually exclusive with EGFR exon 20 mutation, while recent studies on ISP and SNSCC have also shown frequent inactivating mutations in CDKN2A as well as loss of p16 expression [48,49,50,51,52]. Other recurrent mutations include TP53, KRAS, PIK3CA, NF1, and NFE2L2 [50, 51].
These genetic alterations point to EGFR, PI3K-MTOR, MEK and cell cycle control signaling pathways as candidate therapeutic targets. Several drugs inhibiting the activity of these pathways are applied or being tested in clinical trials to treat more common solid cancers. Examples are EGFR exon 20 inhibitors amivantamab and mobocertinib in recurrent lung cancer, PI3K-MTOR pathway inhibitors apelisib, fulvestrant, everolimus in cutaneous melanoma, lung and breast cancer, MEK inhibitors trametinib, cobimetinib in cutaneous melanoma [53].
SNSCC is also the tumor subtype from which the largest number of cell lines have been generated. In 2014, our group presented six new cell lines named SCCNC1, SCCNC2, SCCNC4, SCCNC5, SCCNC6, and SCCNC7 from primary and previously untreated SNSCC [54]. Later, we established two additional cell lines from a local recurrence and a lymph node metastasis of the same patient as SCCNC6 who after surgery of the primary tumor had refused radio/chemotherapy. These two cell lines related to SCCNC6 were named SCCNC6REC and SCCNC6LN, respectively (unpublished results). An extensive literature search for previously published cell lines in 2014 revealed ten unique cell lines, four from treatment-naive primary tumors (cell lines MC; IMC-2,3,4; FS-1; KKM-A) and six from recurrent or metastatic tumors (cell lines KKM-B,C,D; HC-2,3,4,7,9; UT-SCC-53; AMC-HN-5; UM-SCC-33; UM-SCC-85) [54].
Udager et al. was the first to discover frequent EGFR exon 20 mutations in ISP-associated SNSCC and ISP, and demonstrated cell lines SCCNC4 and UM-SCC-112 (the latter previously unpublished) to carry the EGFR exon 20 mutations S768_D770dup and N771_H773dup, respectively [48]. Both cell lines appeared sensitive to the irreversible EGFR inhibitors neratinib, afatinib, and dacomitinib. Recently, Siegel et al. presented a new reversible small molecule inhibitor BAY2927088 with a very potent activity in SCCNC4 cells, but which also acts against EGFR exon 19 deletion [55]. Another ISP-associated SNSCC cell line named MOP-IPST-1 was created by Swenson et al. in 2020. This cell line, although being near-diploid showed a multitude of chromosomal translocations. The authors did not analyze EGFR exon 20 mutation or HPV, but did report positive immunohistochemical staining for p53 and absence of staining for p16 [56]. Finally, Nukpook et al. immortalized a ISP cell culture carrying EGFR exon 20 P772_H773insPYNP, by transduction with CCND1, mutant CDK4 and TERT [57]. The resulting cell line named IP4/K4DT showed a diploid karyotype with only one chromosomal aberration (an addition at 8q24, possibly of part of chromosome arm 5q).
In spite of the possible tumorigenic relation of HPV, no SNSCC or ISP cell lines have been described that indeed carry HPV. Other recurrent genetic abnormalities reported in series of analyzed cases SNSCC or ISP include TP53, CDKN2A with loss of p16 expression, and NF1 [50,51,52]. WES analysis of the SCCNC cell lines described by Garcia-Inclan et al. showed that all six carry mutations in TP53 (including SCCNC4 and SCCNC6 which were originally designated TP53 wildtype by PCR-sequencing), while CDKN2A and NF1 mutations are present in, respectively, SCCNC4 and SCCNC7 [54, 58]. Sequencing data can be obtained upon request.
Intestinal-Type Adenocarcinoma (ITAC)
ITAC have 40–50% TP53 mutations which may be associated with occupational exposure to wood or leather dust [59]. Nuclear expression of β‑catenin indicating Wnt pathway activation has been reported in 31–53% of cases [60], and mutations in APC and CTNNB1 (coding β-catenin) in 16% of ITAC [61,62,63]. Other recurrent mutations in ITAC include PIK3CA, KRAS, NF1, and BRCA1 [61,62,63]. Until the present moment, only one ITAC cell line has been published and it still remains the only succesful culture after a great many attempts in our laboratory.
ITAC-3 was derived from a colonic subtype ITAC from the ethmoid sinus showing scant CK20 expression and absence of nucelar β-catenin expression. It carries a homozygous TP53 exon 8 mutation with a strong nuclear p53 protein overexpression. ITAC-3 carries none of the other recurrent mutations found in ITAC [64]. A recent study identified four signaling pathways as frequently affected by genetic alterations in ITAC; aside from the already mentioned Wnt pathway, these are Homologous DNA repair, MAPK, and AKT/PI3K/mTOR [62]. We found that ITAC-3 cells indeed show elevated activity of MAPK and AKT/PI3K/mTOR while cell proliferation was greatly reduced by simultaneous exposure to selumitinib and everolimus (unpublished results). These first results indicate the possible clinical usefulness of targeted therapy against these cellular pathways for ITAC patients.
Undifferentiated Carcinoma (SNUC)
SNUC still essentially is a group of tumors classified by exclusion of other diagnosis, showing absence of squamous, glandular, and neuroendrocrine histologies. Subsets of SNUC are now recognized as separate tumor entities, with NUT carcinoma defined by > 50% NUT expression and SMARCB1-deficient and SMARCA4-deficient carcinoma defined by loss of expression of these proteins [37, 38••]. SNUC also harbors frequent (33–82%) IDH2 mutations and some authors have claimed IDH2-mutated cases to represent another separate entity. However, IDH2 mutations have also been detected in ONB, SNEC, and high-grade adenocarcinoma [65,66,67], so more investigation is needed. Very little is known on other recurrent genetic aberrations in SNUC.
In 2012, Takahashi et al. published the first and still the only SNUC cell line named MDA8788 [68]. It is derived from a maxillary sinus T4N0M0 tumor treated with induction chemotherapy with 4 cycles of etoposide and carboplatin. MDA8788 express epithelial markers E-cadherin and b-catenin but not the mesenchymal markers N-cadherin, vimentin, a-SMA or the neuroendocrine marker synaptophysin. Cytogenetic analysis showed an aneuploid karyotype with several chromosomal translocations. Later genetic analysis revealed a high-level amplification of ERBB2 and phosprylated-ERBB2 overexpression. Exposure to lapatinib was shown to reduce phosphorylated ERBB2 and downstream pathways AKT and MAPK [69]. This suggests that inhibition of these cellular pathways may be a therapeutic option for SNUC patients, similar as indicated above for ITAC.
To our knowledge, no in vitro models of sinonasal SMARCB1-deficient and SMARCA4-deficient carcinoma have been described in the literature; however, Stirnweiss et al. created a fastgrowing immortal cell line PER-909, cultured up to 13 passages, derived from a postmortum biopsy of a T4bN0M0 NUT carcinoma originating in the superior nasal cavity and ethmoid sinus with a diploid karyotype showing a BRD4-NUTM1 fusion, with BRD4 exon 15 fused to the last 124 nucleotides of NUT exon 2 [70]. Additional NUT carcinoma cell lines have been established but these are derived from other anatomical regions. Several therapies against BRD4-NUT fusion NUT carcinomas are being tested in clinical studies and include inhibitors of BET bromodomain, p300/CBP, CDK9, and CDK4/6 as well as agents targeting DNA repair [71, 72], and the PER-909 cell line will be a valuable model for preclinical testing.
Neuroendocrine Carcinoma (SNEC)
In 2004, Noguchi et al. reported the establishment of an immortal in vitro cell line derived from a lymph node metastasis of a maxillary sinus SNUC that was previously cultured in nude mice [73, 74]. The cell line was designated SNEC-MI and has been in culture over 50 passages. The neuroendocrine phenotype was confirmed by strong cytoplasmic positivity of NSE and CD56 at the membrane; however, chromogranin A and somatostatin were negative. Karyotyping showed near-triploidy with multiple chromosomal translocations. To our knowledge, no further genetic characterization of preclinical functional assays with anticancer agents have been performed with SNEC-MI cells.
SMARCA4-Deficient Carcinoma
Subsets of SNEC and also SNUC and TCS have been reported to be SMARCA4-deficient [75,76,77]. Spectral karyotyping of the above-described SNUC MDA8788 and SNEC-MI cell lines showed structural aberrations involving chromosome 19, possibly 19p13, which is the chromosomal location of the SMARCA4 gene [68, 74]. However, it is not known if MDA-6788 and SNEC-MI have lost SMARCA4 protein expression.
Our lab has recently set up in vitro cell line derived from a T4N0M0 TCS originating from the ethmoid sinus. This cell line named TCS-627 has now been in culture over 60 passages. We have characterized the cells and its original primary tumor immunohistochemically and genetically. One important feature of this cell line is SMARCA4 gene mutation, with absence of SMARCA4 as well as SMARCB1 protein expression, making it a bona fide model of TCS (unpublished results).
Mouse Models and Organoids
An important feature of sinonasal tumors is their wide histological divergence often showing loss of differentiation. Although two-dimensional cell lines are used to analyze the expression of differentiation markers, such studies do not do justice to all the cellular processes involved in these processes. This is where three-dimensional in vitro organoid models and also in vivo orthotopic mouse xenograft models can play a role. Forcing tumor cells back into normal cell differentiation and maturation is a therapeutic option alternative to killing tumor cells or reducing their proliferation with cytotoxic or cytostatic agents. The first successful differentiation therapy for cancer was all-trans retinoic acid treatment in acute promyelocytic leukemia; however, several more inhibitors have demonstrated differentiation effects in multiple solid tumors [78]. Differentiation processes are often affected by aberrant DNA and histone methylation and several genetic alterations that cause methylation changes have been reported in sinonasal tumors, including IDH2, SMARCB1, SMARCA4, KMT2A/B/C/D, SETD2, and ARID1A [45••, 66, 79]. These genes or the pathways in which they are involved can be used as target for treatment with modern inhibitors [80,81,82,83].
Three-dimensional cultures using hydrogels or scaffolds of porous forms have been shown to closely mimic tissue physiology, architecture, and microenvironment by reconstructing a true extracellular matrix. Scaffolds also allow co-culture of stromal, endothelial, and immune cells. In addition, they have the advantage of reducing the need of experimental animals [84,85,86,87]. Comparison of two- and three-dimensional preclinical models indicated significant differences in gene and protein expression, proliferation, cell differentiation, and drug response, showing 3D models to be closer to animal models [84]. The application of patient cells and biomaterial scaffolds for personalized screening in cancer is still at its infancy, and only a limited number of studies are proposed in the literature [86]. Danti and coworkers at the university of Pisa have made the first attempts of creating organoid cultures of sinonasal tumors [88, 89].
In 2012, Takahashi et al. presented a mouse model created by injecting cells of SNUC cell line MDA8788 into the muscle of the soft palate. This model showed local invasion into muscle, bone, nerve, blood vessels, lymphatic vessels, and the brain [68]. Using cell line SCCNC4, Costales et al. created an orthotopic mouse model by inoculating the cells at the level of the medial wall of maxillary sinus. This model showed invaded bone, surrounding tissues, and brain, showing the same poor differentiation as the original primary tumor from which the cell line was derived. However, genetic analysis of the cell line and the mouse xenograft tumor revealed deletions of genes CDKN2A and PTEN that were not present in the original primary tumor, indicating that in vitro or in vivo models are not always 100% representative of their original tumors [90].
Other Sinonasal Tumor Models… or No?
We have been unable to find any other sinonasal tumor models in the literature; however, we came across a few that may or may not be valid for sinonasal cancer. Back in 1988, Cavazzana et al. presented two ONB cell lines JFEN and TC-268 [91]. However, Sorensen et al. showed that both lines expressed EWS/FLIl translocation and protein fusion indicative of the Ewing sarcoma family of childhood peripheral primitive neuroectodermal tumors [92], and thus it remains unclear if these cell lines actually represent ONB.
Several cell lines have been established from skin melanoma, but we were unable to find models for sinonasal MMM in the literature. Ju et al. did create an orthotopic mouse model of maxillary sinus MMM, but for inoculation they used the cell line B16 which originally was derived from a cutaneous melanoma [93]. MMM are genetically different from cutaneous melanoma having a lower tumor mutation burden and a higher number of chromosomal rearrangements. Recurrent gene mutations in sinonasal MMM include NRAS, BRAF, NF1, KIT, SF3B1, CDKN2A, and APC mutations [94, 95]. A number of papers reported cell lines established from oral MMM [96,97,98]. It may be that oral MMM are genetically similar to sinonasal MMM; in that case, these oral MMM cell lines may be of use also as preclinical models for sinonasal MMM.
Conclusions
Many different types of tumors arise in the sinonasal cavities. Their incidence is low, a fact that has hampered molecular-genetic studies on tumorigenic pathways and the testing of alternative treatment strategies. In vitro tumor cell lines are valuable tools for functional studies on processes as proliferation, differentiation, invasion and metastasis, as well as preclinical testing of new therapeutic agents. Experimental models representing various sinonasal cancer subtypes are available and may help to bridge the gap between laboratory investigation and clinical application.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bossi P, Saba NF, Vermorken JB, Strojan P, Pala L, de Bree R, Rodrigo JP, Lopez F, Hanna EY, Haigentz M, Takes RP, Slootweg PJ, Silver CE, Rinaldo A, Ferlito A. The role of systemic therapy in the management of sinonasal cancer: a critical review. Cancer Treat Rev. 2015;41:836–43.
Orlandi E, Cavalieri S, Granata R, Nicolai P, Castelnuovo P, Piazza C, Schreiber A, Turri-Zanoni M, Quattrone P, Miceli R, Infante G, Sessa F, Facco C, Calareso G, Iacovelli NA, Mattavelli D, Paderno A, Resteghini C, Locati LD, Licitra L, Bossi P. Locally advanced epithelial sinonasal tumors: the impact of multimodal approach. Laryngoscope. 2020;130:857–65.
Llorente JL, López F, Suárez C, Hermsen MA. Sinonasal carcinoma: clinical, pathological and genetic advances for new therapeutic opportunities. Nat Rev Clin Oncol. 2014;11:460–72.
Chakravarty D, Gao J, Phillips SM, Kundra R, Zhang H, Wang J, Rudolph JE, Yaeger R, Soumerai T, Nissan MH, Chang MT, Chandarlapaty S, Traina TA, Paik PK, Ho AL, Hantash FM, Grupe A, Baxi SS, Callahan MK, Snyder A, Chi P, Danila D, Gounder M, Harding JJ, Hellmann MD, Iyer G, Janjigian Y, Kaley T, Levine DA, Lowery M, Omuro A, Postow MA, Rathkopf D, Shoushtari AN, Shukla N, Voss M, Paraiso E, Zehir A, Berger MF, Taylor BS, Saltz LB, Riely GJ, Ladanyi M, Hyman DM, Baselga J, Sabbatini P, Solit DB, Schultz N. OncoKB: a precision oncology knowledge base. JCO Precis Oncol. 2017;2017:PO.17.00011.
• Hermsen MA, Riobello C, García-Marín R, Cabal VN, Suárez-Fernández L, López F, Llorente JL. Translational genomics of sinonasal cancers. Semin Cancer Biol. 2020;61:101–9. For all major histological subtypes of sinonasal cancer, this paper presents and comments on all published genetic alterations that may serve as molecular targets for therapy with specific inhibitors.
https://www.rarecarenet.eu/. Accessed 9 Aug 2023.
Markham MJ, Wachter K, Agarwal N, Bertagnolli MM, Chang SM, Dale W, Diefenbach CSM, Rodriguez-Galindo C, George DJ, Gilligan TD, Harvey RD, Johnson ML, Kimple RJ, Knoll MA, LoConte N, Maki RG, Meisel JL, Meyerhardt JA, Pennell NA, Rocque GB, Sabel MS, Schilsky RL, Schneider BJ, Tap WD, Uzzo RG, Westin SN. Clinical Cancer Advances 2020: annual report on progress against cancer from the American Society of Clinical Oncology. J Clin Oncol. 2020;38:1081.
DeSantis CE, Kramer JL, Jemal A. The burden of rare cancers in the United States. CA Cancer J Clin. 2017;67:261–72.
Billingham L, Malottki K, Steven N. Research methods to change clinical practice for patients with rare cancers. Lancet Oncol. 2016;17:e70-80.
Hauser S, Widera D, Qunneis F, Müller J, Zander C, Greiner J, Strauss C, Lüningschrör P, Heimann P, Schwarze H, Ebmeyer J, Sudhoff H, Araúzo-Bravo MJ, Greber B, Zaehres H, Schöler H, Kaltschmidt C, Kaltschmidt B. Isolation of novel multipotent neural crest-derived stem cells from adult human inferior turbinate. Stem Cells Dev. 2012;21:742–56.
Vivanco B, Llorente JL, Perez-Escuredo J, Alvarez Marcos C, Fresno MF, Hermsen MA. Benign lesions in mucosa adjacent to intestinal-type sinonasal adenocracinoma. Patholog Res Int. 2011;2011:230147.
Franchi A, et al. Intestinal metaplasia of the sinonasal mucosa adjacent to intestinal-type adenocarcinoma. A morphologic, immunohistochemical, and molecular study. Virchows Arch. 2015;466:161–8.
Agarwal S, van Zante A, Granados ML. Combined neuroendocrine and squamous cell carcinoma of the sinonasal tract: a morphologic and immunohistochemical analysis and review of literature. Head Neck Pathol. 2022;16(4):1019–33.
Barham HP, Said S, Ramakrishnan VR. Colliding tumor of the paranasal sinus. Allergy Rhinol (Providence). 2013;4(1):e13–6.
Franchi A, Palomba A, Miligi L, Ranucci V, Innocenti DR, Simoni A, Pepi M, Santucci M. Primary combined neuroendocrine and squamous cell carcinoma of the maxillary sinus: report of a case with immunohistochemical and molecular characterization. Head Neck Pathol. 2015;9:107–13.
Sugianto I, Yanagi Y, Hisatomi M, Okada S, Takeshita Y, Bamgbose BO, Asaumi J. Collision tumor of small cell carcinoma and squamous cell carcinoma of the maxillary sinus: case report. Mol Clin Oncol. 2022;16(5):96.
Brown SJ, Thavaraj S. Human papillomavirus-associated combined neuroendocrine and squamous cell carcinoma of the sinonasal tract. Head Neck Pathol. 2022;16(4):1227–9.
Jain R, Gramigna V, Sanchez-Marull R, Perez-Ordoñez B. Composite intestinal-type adenocarcinoma and small cell carcinoma of sinonasal tract. J Clin Pathol. 2009;62(7):634–7.
La Rosa S, Furlan D, Franzi F, Battaglia P, Frattini M, Zanellato E, Marando A, Sahnane N, Turri-Zanoni M, Castelnuovo P, Capella C. Mixed exocrine-neuroendocrine carcinoma of the nasal cavity: clinico-pathologic and molecular study of a case and review of the literature. Head Neck Pathol. 2013;7:76–84.
Attwood JE, Jeyaretna DS, Sheerin F, Shah KA. Mixed olfactory neuroblastoma and adenocarcinoma with in situ neuroendocrine hyperplasia. Head Neck Pathol. 2020;14(3):792–8.
Gandhoke CS, Dewan A, Gupta D, Syal SK, Jagetia A, Saran RK, Meher R, Srivastava AK, Singh D. A rare case report of mixed olfactory neuroblastoma: carcinoma with review of literature. Surg Neurol Int. 2017;26(8):83.
Lao WP, Thompson JM, Evans L, Kim Y, Denham L, Lee SC. Mixed olfactory neuroblastoma and neuroendocrine carcinoma: an unusual case report and literature review. Surg Neurol Int. 2020;9(11):97.
Nakamura Y, Suzuki M, Ozaki S, Yokota M, Nakayama M, Hattori H, Inagaki H, Murakami S. Sinonasal inverted papilloma associated with small cell neuroendocrine carcinoma: a case report and literature review of rare malignancies associated with inverted papilloma. Auris Nasus Larynx. 2019;46(4):641–50.
Karam SD, Jay AK, Anyanwu C, Steehler MK, Davidson B, Debrito P, Harter KW. Pathologic collision of inverted papilloma with esthesioneuroblastoma. Front Oncol. 2014;14(4):44.
Orgain CA, Shibuya TY, Thompson LD, Keschner DB, Garg R, Lee JT. Long-term follow-up of a patient with malignant transformation of inverted papilloma into sinonasal undifferentiated carcinoma. Allergy Rhinol (Providence). 2017;8(3):173–7.
Kang SY, McHugh JB, Sullivan SE, Marentette LJ, McKean EL. Sinonasal undifferentiated carcinoma and esthesioneuroblastoma recurring as nonintestinal adenocarcinoma. Laryngoscope. 2013;23:1121–4.
Kim JS, Hong KH, Jang KY, Song JH. Sinonasal undifferentiated carcinoma originating from inverted papilloma: a case report. Medicine (Baltimore). 2017;96(45):e8584.
Valentini V, Giovannetti F, Cassoni A, Terenzi V, Priore P, Raponi I, Bosco S, Alesini F, Mezi S, Musio D, Tombolini V. Sinonasal undifferentiated carcinoma in a patient previously treated for an intestinal-type adenocarcinoma: metachronous neoplasms or recurrence of a different tumor type? Indian J Otolaryngol Head Neck Surg. 2019;71(Suppl 3):1779–81.
Larkin R, Hermsen MA, London NR Jr. Translocations and gene fusions in sinonasal malignancies. Curr Oncol Rep. 2023;25(4):269–78.
Taverna C, Agaimy A, Franchi A. Towards a molecular classification of sinonasal carcinomas: clinical implications and opportunities. Cancers (Basel). 2022;14(6):1463.
Turri-Zanoni M, Gravante G, Castelnuovo P. Molecular biomarkers in sinonasal cancers: new frontiers in diagnosis and treatment. Curr Oncol Rep. 2022;24(1):55–67.
French C. NUT midline carcinoma. Nat Rev Cancer. 2014;14(3):149–50.
Kuo YJ, Lewis JS, Zhai C, Chen YA, Chernock RD, Hsieh MS, et al. DEK-AFF2 fusion-associated papillary squamous cell carcinoma of the sinonasal tract: clinicopathologic characterization of seven cases with deceptively bland morphology. Mod Pathol. 2021;34(10):1820–30.
Agaimy A, Hartmann A, Antonescu CR, Chiosea SI, El-Mofty SK, Geddert H, Iro H, Lewis JS Jr, Märkl B, Mills SE, Riener MO, Robertson T, Sandison A, Semrau S, Simpson RH, Stelow E, Westra WH, Bishop JA. SMARCB1 (INI-1)-deficient sinonasal carcinoma: a series of 39 cases expanding the morphologic and clinicopathologic spectrum of a recently described entity. Am J Surg Pathol. 2017;41(4):458–71.
Rooper LM, Uddin N, Gagan J, Brosens LAA, Magliocca KR, Edgar MA, Thompson LDR, Agaimy A, Bishop JA. Recurrent loss of SMARCA4 in sinonasal teratocarcinosarcoma. Am J Surg Pathol. 2020;44(10):1331–9.
Hermsen MA. Sinonasal cancer: molecular biomarkers for tumor classification and targeted treatment. ESMO Open. 2023;8(1):101043.
El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ. WHO classification of tumors pathology and genetics of head and neck tumors. Vol 4th ed. Lyon: IARC Press, 2017.
•• Franchi A (ed). Pathology of sinonasal tumors and tumor-like lesions. Springer Nature Switzerland AG 2020. A great resource describing in detail the histological as well as immunohistochemical and genetic characteristics of all benign and malignant sinonasal tumors.
Lu C, Ward PS, Kapoor GS, Rohle D, Turcan S, Abdel-Wahab O, Edwards CR, Khanin R, Figueroa ME, Melnick A, Wellen KE, O’Rourke DM, Berger SL, Chan TA, Levine RL, Mellinghoff IK, Thompson CB. IDH mutation impairs histone demethylation and results in a block to cell differentiation. Nature. 2012;483:474–8.
Laco J, Chmelařová M, Vošmiková H, Sieglová K, Bubancová I, Dundr P, Němejcová K, Michálek J, Čelakovský P, Mottl R, Sirák I, Vošmik M, Ryška A. SMARCB1/INI1-deficient sinonasal carcinoma shows methylation of RASSF1 gene: a clinicopathological, immunohistochemical and molecular genetic study of a recently described entity. Pathol Res Pract. 2017;213(2):133–42.
Costales M, López-Hernández A, García-Inclán C, Vivanco B, López F, Llorente JL, Hermsen MA. Gene methylation profiling in sinonasal adenocarcinoma and squamous cell carcinoma. Otolaryngol Head Neck Surg. 2016;155(5):808–15.
Libera L, Ottini G, Sahnane N, Pettenon F, Turri-Zanoni M, Lambertoni A, Chiaravalli AM, Leone F, Battaglia P, Castelnuovo P, Uccella S, Furlan D, Facco C, Sessa F. Methylation drivers and prognostic implications in sinonasal poorly differentiated carcinomas. Cancers (Basel). 2021;13(19):5030.
Dogan S, Vasudevaraja V, Xu B, Serrano J, Ptashkin RN, Jung HJ, Chiang S, Jungbluth AA, Cohen MA, Ganly I, Berger MF, Momeni Boroujeni A, Ghossein RA, Ladanyi M, Chute DJ, Snuderl M. DNA methylation-based classification of sinonasal undifferentiated carcinoma. Mod Pathol. 2019;32(10):1447–59.
Sahnane N, Ottini G, Turri-Zanoni M, Furlan D, Battaglia P, Karligkiotis A, Albeni C, Cerutti R, Mura E, Chiaravalli AM, Castelnuovo P, Sessa F, Facco C. Comprehensive analysis of HPV infection, EGFR exon 20 mutations and LINE1 hypomethylation as risk factors for malignant transformation of sinonasal-inverted papilloma to squamous cell carcinoma. Int J Cancer. 2019;144(6):1313–20.
•• Jurmeister P, Glöß S, Roller R, Leitheiser M, Schmid S, Mochmann LH, Payá Capilla E, Fritz R, Dittmayer C, Friedrich C, Thieme A, Keyl P, Jarosch A, Schallenberg S, Bläker H, Hoffmann I, Vollbrecht C, Lehmann A, Hummel M, Heim D, Haji M, Harter P, Englert B, Frank S, Hench J, Paulus W, Hasselblatt M, Hartmann W, Dohmen H, Keber U, Jank P, Denkert C, Stadelmann C, Bremmer F, Richter A, Wefers A, Ribbat-Idel J, Perner S, Idel C, Chiariotti L, Della Monica R, Marinelli A, Schüller U, Bockmayr M, Liu J, Lund VJ, Forster M, Lechner M, Lorenzo-Guerra SL, Hermsen M, Johann PD, Agaimy A, Seegerer P, Koch A, Heppner F, Pfister SM, Jones DTW, Sill M, von Deimling A, Snuderl M, Müller KR, Forgó E, Howitt BE, Mertins P, Klauschen F, Capper D. DNA methylation-based classification of sinonasal tumors. Nat Commun. 2022;13(1):7148. This study provides evidence for analysis of DNA methylation profiles to aid and refine classification of all sinonasal tumor subtypes.
Mateo J. A framework to rank genomic alterations as targets for cancer precision medicine: the ESMO Scale for Clinical Actionability of molecular Targets (ESCAT). Ann Oncol. 2018;29:1895–902.
•• Martin-Romano P. Implementing the European Society for Medical Oncology Scale for Clinical Actionability of Molecular Targets in a Comprehensive Profiling Program: impact on precision medicine oncology. JCO Precis Oncol. 2022;6:e2100484. Demonstration of the usefulness of a harmonized and standardized list of actionable molecular targets, ranked according to clinical evidence, for personalized cancer treatment.
Udager AM, Rolland DC, McHugh JB, Betz BL, Murga-Zamalloa C, Carey TE, Marentette LJ, Hermsen MA, DuRoss KE, Lim MS, Elenitoba-Johnson KS, Brown NA. High-frequency targetable EGFR mutations in sinonasal squamous cell carcinomas arising from inverted sinonasal papilloma. Cancer Res. 2015;75(13):2600–6.
Cabal VN, Menendez M, Vivanco B, et al. EGFR mutation and HPV infection in sinonasal inverted papilloma and squamous cell carcinoma. Rhinol. 2020;58:368–76.
Uchi R, Jiromaru R, Yasumatsu R, Yamamoto H, Hongo T, Manako T, Sato K, Hashimoto K, Wakasaki T, Matsuo M, Nakagawa T. Genomic sequencing of cancer-related genes in sinonasal squamous cell carcinoma and coexisting inverted papilloma. Anticancer Res. 2021;41(1):71–9.
Brown NA, Plouffe KR, Yilmaz O, Weindorf SC, Betz BL, Carey TE, Seethala RR, McHugh JB, Tomlins SA, Udager AM. TP53 mutations and CDKN2A mutations/deletions are highly recurrent molecular alterations in the malignant progression of sinonasal papillomas. Mod Pathol. 2021;34(6):1133–42.
Menéndez Del Castro M, Naves Cabal V, Vivanco B, Suárez-Fernández L, López F, Llorente JL, Hermsen MA, Álvarez-Marcos C. Loss of p16 expression is a risk factor for recurrence in sinonasal inverted papilloma. Rhinology. 2022;60(6):453–61.
Esposito A, Stucchi E, Baronchelli M, Di Mauro P, Ferrari M, Lorini L, Gurizzan C, London NRJ, Hermsen M, Lechner M, Bossi P. Molecular basis and rationale for the use of targeted agents and immunotherapy in sinonasal cancers. J Clin Med. 2022;11(22):6787.
García-Inclán C, López-Hernández A, Alonso-Guervós M, Allonca E, Potes S, López F, Llorente JL, Hermsen M. Establishment and genetic characterization of six unique tumor cell lines as preclinical models for sinonasal squamous cell carcinoma. Sci Rep. 2014;4:4925.
Siegel F, Siegel S, Graham K, Kaplan B, Petersen K, Boemer U, et al. Preclinical activity of the first reversible, potent and selective inhibitor of EGFR exon 20 insertions. Cancer Res. 2023;81(13_Supplement):1470.
Swenson W, Miller KA, Wuertz B, Jungbauer WN Jr, Ondrey FG. Establishment and characterization of an inverted papilloma-associated sinonasal squamous cell carcinoma cell line. Int Forum Allergy Rhinol. 2021;11:938–40.
Nukpook T, Ekalaksananan T, Kiyono T, Kasemsiri P, Teeramatwanich W, Vatanasapt P, et al. Establishment and genetic characterization of cell lines derived from proliferating nasal polyps and sinonasal inverted papillomas. Sci Rep. 2021;11:17100.
Hieggelke L, Heydt C, Castiglione R, Rehker J, Merkelbach-Bruse S, Riobello C, Llorente JL, Hermsen MA, Buettner R. Mismatch repair deficiency and somatic mutations in human sinonasal tumors. Cancers. 2021;13(23):6081.
Pérez-Escuredo J, Martínez JG, Vivanco B, Marcos CÁ, Suárez C, Llorente JL, Hermsen MA. Wood dust-related mutational profile of TP53 in intestinal-type sinonasal adenocarcinoma. Hum Pathol. 2012;43(11):1894–901.
Díaz-Molina JP, Llorente JL, Vivanco B, Martínez-Camblor P, Fresno MF, Pérez-Escuredo J, Álvarez-Marcos C, Hermsen MA. Wnt-pathway activation in intestinal-type sinonasal adenocarcinoma. Rhinology. 2011;49(5):593–9.
Sánchez-Fernández P, Riobello C, Costales M, Vivanco B, Cabal VN, García-Marín R, Suárez-Fernández L, López F, Cabanillas R, Hermsen MA, Llorente JL. Next-generation sequencing for identification of actionable gene mutations in intestinal-type sinonasal adenocarcinoma. Sci Rep. 2021;11(1):2247.
Riobello C, Sánchez-Fernández P, Cabal VN, García-Marín R, Suárez-Fernández L, Vivanco B, Blanco-Lorenzo V, Álvarez Marcos C, López F, Llorente JL, Hermsen MA. Aberrant signaling pathways in sinonasal intestinal-type adenocarcinoma. Cancers (Basel). 2021;13(19):5022.
Sjöstedt S, Schmidt AY, Vieira FG, Willemoe GL, Agander TK, Olsen C, Nielsen FC, von Buchwald C. Major driver mutations are shared between sinonasal intestinal-type adenocarcinoma and the morphologically identical colorectal adenocarcinoma. J Cancer Res Clin Oncol. 2021;147(4):1019–27.
Pérez-Escuredo J, García Martínez J, García-Inclán C, Vivanco B, Costales M, Álvarez Marcos C, Llorente JL, Hermsen MA. Establishment and genetic characterization of an immortal tumor cell line derived from intestinal-type sinonasal adenocarcinoma. Cell Oncol (Dordr). 2011;34(1):23–31.
Riobello C, López-Hernández A, Cabal VN, García-Marín R, Suárez-Fernández L, Sánchez-Fernández P, Vivanco B, Blanco V, López F, Franchi A, Llorente JL, Hermsen MA. IDH2 Mutation analysis in undifferentiated and poorly differentiated sinonasal carcinomas for diagnosis and clinical management. Am J Surg Pathol. 2020;44(3):396–405.
Glöss S, Jurmeister P, Thieme A, Schmid S, Cai WY, Serrette RN, Perner S, Ribbat-Idel J, Pagenstecher A, Bläker H, Keber U, Stadelmann C, Zechel S, Johann PD, Hasselblatt M, Paulus W, Thomas C, Dohmen H, Baumhoer D, Frank S, Agaimy A, Schüller U, Vasudevaraja V, Snuderl M, Liu CZ, Pfister DG, Jungbluth AA, Ghossein RA, Xu B, Capper D, Dogan S. IDH2 R172 Mutations across poorly differentiated sinonasal tract malignancies: forty molecularly homogenous and histologically variable cases with favorable outcome. Am J Surg Pathol. 2021;45(9):1190–204.
Classe M, Yao H, Mouawad R, et al. Integrated multi-omic analysis of esthesioneuroblastomas identifies two subgroups linked to cell ontogeny. Cell Rep. 2018;25:811.e5-821.e5.
Takahashi Y, Kupferman ME, Bell D, Jiffar T, Lee JG, Xie TX, Li NW, Zhao M, Frederick MJ, Gelbard A, Myers JN, Hanna EY. Establishment and characterization of novel cell lines from sinonasal undifferentiated carcinoma. Clin Cancer Res. 2012;18(22):6178–87.
Takahashi Y, Lee J, Pickering C, Bell D, Jiffar TW, Myers JN, Hanna EY, Kupferman ME. Human epidermal growth factor receptor 2/neu as a novel therapeutic target in sinonasal undifferentiated carcinoma. Head Neck. 2016;38(Suppl 1):E1926–34.
Stirnweiss A, McCarthy K, Oommen J, Crook ML, Hardy K, Kees UR, Wilton SD, Anazodo A, Beesley AH. A novel BRD4-NUT fusion in an undifferentiated sinonasal tumor highlights alternative splicing as a contributing oncogenic factor in NUT midline carcinoma. Oncogenesis. 2015;4(11):e174.
Stirnweiss A, Oommen J, Kotecha RS, Kees UR, Beesley AH. Molecular-genetic profiling and high-throughput in vitro drug screening in NUT midline carcinoma-an aggressive and fatal disease. Oncotarget. 2017;8(68):112313–29.
French CA, Cheng ML, Hanna GJ, DuBois SG, Chau NG, Hann CL, Storck S, Salgia R, Trucco M, Tseng J, Stathis A, Piekarz R, Lauer UM, Massard C, Bennett K, Coker S, Tontsch-Grunt U, Sos ML, Liao S, Wu CJ, Polyak K, Piha-Paul SA, Shapiro GI. Report of the first international symposium on NUT carcinoma. Clin Cancer Res. 2022;28(12):2493–505.
Noguchi K, Urade M, Sakurai K, Nishimura N, Hashitani S, Kishimoto H. Small cell neuroendocrine carcinoma of the maxillary sinus: a case report and nude mouse transplantable model. Head Neck. 2002;24:491–6.
Noguchi K, et al. Establishment of a new cell line with neuronal differentiation derived from small cell neuroendocrine carcinoma of the maxillary sinus. Oncology. 2004;66:234–43.
Kakkar A, Ashraf SF, Rathor A, Adhya AK, Mani S, Sikka K, Jain D. SMARCA4/BRG1-deficient sinonasal carcinoma. Arch Pathol Lab Med. 2022;146(9):1122–30.
Rooper LM, Agaimy A, Gagan J, Simpson RHW, Thompson LDR, Trzcinska AM, Ud Din N, Bishop JA. Comprehensive molecular profiling of sinonasal teratocarcinosarcoma highlights recurrent SMARCA4 inactivation and CTNNB1 mutations. Am J Surg Pathol. 2023;47(2):224–33.
Agaimy A, Jain D, Uddin N, Rooper LM, Bishop JA. SMARCA4-deficient sinonasal carcinoma: a series of 10 cases expanding the genetic spectrum of SWI/SNF-driven sinonasal malignancies. Am J Surg Pathol. 2020;44(5):703–10.
Cruz FD, et al. Solid tumor differentiation therapy—is it possible? Oncotarget. 2012;3:559–67.
Capper D, Engel NW, Stichel D, Lechner M, Glöss S, Schmid S, Koelsche C, Schrimpf D, Niesen J, Wefers AK, Jones DTW, Sill M, Weigert O, Ligon KL, Olar A, Koch A, Forster M, Moran S, Tirado OM, Sáinz-Jaspeado M, Mora J, Esteller M, Alonso J, Del Muro XG, Paulus W, Felsberg J, Reifenberger G, Glatzel M, Frank S, Monoranu CM, Lund VJ, von Deimling A, Pfister S, Buslei R, Ribbat-Idel J, Perner S, Gudziol V, Meinhardt M, Schüller U. DNA methylation-based reclassification of olfactory neuroblastoma. Acta Neuropathol. 2018;136(2):255–71.
Stein E, Yen K. Targeted differentiation therapy with mutant IDH inhibitors: early experiences and parallels with other differentiation agents. Annu Rev Cancer Biol. 2017;1:379–401.
Pirozzi CJ, Reitman ZJ, Yan H. Releasing the block: setting differentiation free with mutant IDH inhibitors. Cancer Cell. 2013;23:570–2.
Turcan S, Fabius AW, Borodovsky A, Pedraza A, Brennan C, Huse J, Viale A, Riggins GJ, Chan TA. Efficient induction of differentiation and growth inhibition in IDH1 mutant glioma cells by the DNMT inhibitor decitabine. Oncotarget. 2013;4:1729–36.
Saleh K, Classe M, Nguyen F, Moya-Plana A, Even C. Tazemetostat for the treatment of INI-1-deficient sinonasal tumor. Eur J Cancer. 2022;172:329–31.
Pernik MN, Bird CE, Traylor JI, Shi DD, Richardson TE, McBrayer SK, Abdullah KG. Patient-derived cancer organoids for precision oncology treatment. JPM. 2021;11:423.
Contessi Negrini N, Franchi A, Danti S. Biomaterial-assisted 3D in vitro tumor models: from organoid towards cancer tissue engineering approaches. Cancers (Basel). 2023;15:1201.
Hasbum A, Karabulut O, Reyes RE, Ricci C, Franchi A, Danti S, Chew SA. Combined application of patient-derived cells and biomaterials as 3D in vitro tumor models. Cancers. 2022;14:2503.
Gunti S, Hoke ATK, Vu KP, London NR Jr. Organoid and spheroid tumor models: techniques and applications. Cancers. 2021;13:874.
Danti S, Ricci C, Berrettini S, Franchi A. A scaffold platform for sinonasal cancers: in-depth tumor understanding for personalized therapy. Tissue Engineering and Regenerative Medicine International Society Asia‐Pacific Conference October 5-8, 2022, ICC Jeju, South Korea. https://doi.org/10.1089/ten.tea.2022.29036.abstracts.
Danti S, Ricci C, Macchib T, Parchib P, Franchi A. 3D in vitro models of hard and soft tumours. Biomaterials and novel technologies for healthcare, 3rd International Biennial Conference BioMaH, October 18–21, 2022, Rome Italy. Proceedings ISBN 978 88 8080 500 7. https://biomah.ism.cnr.it/?page_id=665. Accessed 9 Aug 2023.
Costales M, López F, García-Inclán C, Fernández S, Llorente JL, Hermsen M. Establishment and characterization of an orthotopic sinonasal squamous cell carcinoma mouse model. Head Neck. 2015;37(12):1769–75.
Cavazzana AO, Navarro S, Noguera R, Reynolds PC, Triche TJ. Olfactory neuroblastoma is not a neuroblastoma but is related to primitive neuroectodermal tumor (PNET). Prog Clin Biol Res. 1988;271:463–73.
Sorensen PH, Wu JK, Berean KW, Lim JF, Donn W, Frierson HF, Reynolds CP, López-Terrada D, Triche TJ. Olfactory neuroblastoma is a peripheral primitive neuroectodermal tumor related to Ewing sarcoma. Proc Natl Acad Sci USA. 1996;93:1038–43.
Ju SM, Chen F, Liu J, Qin G, Xie YL, Wang ZL, Wei XM. Establishment and characterization of an orthotopic murine model of mucosal malignant melanoma of the maxillary sinus. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2017;31(20):1599–602;1605.
Riobello C, Casanueva Muruais R, Suárez-Fernández L, García-Marín R, Cabal VN, Blanco-Lorenzo V, Franchi A, Laco J, López F, Llorente JL, Hermsen MA. Intragenic NF1 deletions in sinonasal mucosal malignant melanoma. Pigment Cell Melanoma Res. 2022;35(1):88–96.
Hayward NK, et al. Whole-genome landscapes of major melanoma subtypes. Nature. 2017;545:175–80.
Lin W, Lu X, Yang H, Huang L, Huang W, Tang Y, Liu S, Wang H, Zhang Y. Metabolic heterogeneity protects metastatic mucosal melanomas cells from ferroptosis. Int J Mol Med. 2022;50(4):124.
Lyu J, Miao Y, Yu F, Chang C, Guo W, Zhu H. CDK4 and TERT amplification in head and neck mucosal melanoma. J Oral Pathol Med. 2021;50(10):971–8.
Shi C, Gu Z, Xu S, Ju H, Wu Y, Han Y, Li J, Li C, Wu J, Wang L, Li J, Zhou G, Ye W, Ren G, Zhang Z, Zhou R. Candidate therapeutic agents in a newly established triple wild-type mucosal melanoma cell line. Cancer Commun (Lond). 2022;42(7):627–47.
Acknowledgements
The authors would like to thank Dr. Lena Hieggelke and Prof. Dr. Reinhard Büttner for their longstanding collaboration and specifically for their whole exome analysis of the Oviedo cell lines published in references 54 and 64.
Funding
This study has been funded by Instituto de Salud Carlos III (ISCIII) through the project “PI19/00191” and “PI20/00383” and co-funded by the European Union, grant CB16/12/00390 from the Centro de Investigación Biomédica en Red de Cancer (CIBERONC), and grant IDI2018/155 Ayudas a Grupos PCTI Principado de Asturias. Helena Codina-Martínez is supported by Centro de Investigación Biomédica en Red de Cáncer grant CB16/12/00390 and Sara Lucila Lorenzo-Guerra is supported by Instituto de Salud Carlos III (ISCIII) grant FI20/00137.
Author information
Authors and Affiliations
Contributions
H.C-M: literature search, collection of relevant clinical and genetic data, review and editing of the manuscript. S.L.L-G: literature search, collection of relevant clinical and genetic data, review and editing of the manuscript. V.N.C: literature search, collection of relevant clinical and genetic data, review and editing of the manuscript. R.G-M: literature search, collection of relevant clinical and genetic data, review and editing of the manuscript. C.R: literature search, collection of relevant clinical and genetic data, review and editing of the manuscript. L.S-F: literature search, collection of relevant clinical and genetic data, review and editing of the manuscript. B.V: review and editing of the manuscript. V.B.L: review and editing of the manuscript. F.L: review and editing of the manuscript. P.S-F: review and editing of the manuscript. M.A.H: literature search, writing main manuscript. J.L.L: review and editing of the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
None of the authors have personal or financial competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Codina-Martínez, H., Lorenzo-Guerra, S.L., Cabal, V.N. et al. Experimental Models of Sinonasal Tumors for Preclinical Testing of Candidate Targeted Therapies. Curr Otorhinolaryngol Rep 12, 1–10 (2024). https://doi.org/10.1007/s40136-023-00496-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-023-00496-9