Abstract
Purpose of Review
The aim of this review is to identify relevant literature reports on cochlear implantation in the elderly population; to compare the outcome of hearing rehabilitation in elderly versus younger adult cochlear implant recipients; to review reported surgical complications; to analyze possible predictive factors; and to evaluate the health-related quality of life.
Recent Findings
All elderly cohorts had a significant improvement in speech understanding and a positive impact on quality of life after cochlear implantation without an increased surgical risk. It was irrelevant if elderly was defined at the age of 60 or 80 years. Complex hearing tasks, such as hearing in background noise, may require a longer time for comprehension, and in general, the elderly population requires longer auditory therapy than the younger counterparts. Duration of deafness seems to be the most redundant predictive factor supported in most studies.
Summary
Cochlear implantation candidacy in elderly patients must be made on an individual basis, dependent on overall health as well as cognitive status. Advanced age alone is not a contraindication when determining candidacy for cochlear implantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and Limitations
The aim of this review is to summarize the results of studies on the clinical effectiveness of cochlear implantation (CI) in elderly patients. The question of the effectiveness of cochlear implantation in elderly patients has moved to the forefront as demographic changes result in an ever increasingly elderly population.
As with all established implantation technology, the question arises as to a possible limitation of use. One such possible limitation is the age at implantation for CI. The worldwide aging population has broad implications for both hearing loss and dementia. Predictions suggest that the global burden of hearing loss will approach 1.2 billion by 2050. Presbyacusis and other forms of hearing loss rise proportionately to older age. Consequences of hearing loss may be substantial because it is associated with functional decline, social isolation, poor quality of life (QOL), cognitive deficits, and depression [1,2,3].
In order to provide an adequate statement on cochlear implantation in the elderly, one must first define “elderly.” The age of 60 or 65, equivalent to retirement ages in most developed countries, is usually addressed as the beginning of old age. However, this age may not be appropriate when grouping elderly cochlear implant recipients. Some studies have shown that reduced speech perception in noise starts at the age of 70 and older [4••]. Furthermore, the worldwide average life expectancy at birth was 68.7 years (range 54.7 years (Guinea-Bissau) to 83.7 years (China, Hong Kong)) over the period 2010–2015 according to United Nations World Population Prospects 2015 Revision. Most countries in Europe and the USA have a life expectancy at birth for this period of 79–82 years. Candidacy for patients based on age as well as a definition of “elderly” may need to be defined based on the region or country under discussion. The difficulty in establishing a cutoff for the definition of elderly in cochlear implant studies is evident when reviewing the literature; some authors have set the age at 60, 65, 70, 75, and 80 years (refer to Table 1).
Another aspect that complicates this topic is how to assess the hearing results after cochlear implantation in the elderly. Is a simple comparison of the standard hearing evaluation, typical to each institution and country, compared to younger counterparts adequate for the assessment; or do any of the more difficult tasks in the test battery favor the younger patients? There are three major aspects in the central auditory nervous system that may disadvantage elderly patients. First, from a pathophysiological standpoint, there are three classic types of causes for sensorineural hearing loss in presbyacusis—sensory, strial, and neural [25]. These can occur alone or in combination. A cochlear implant can circumvent the sensory and strial damage in the cochlea, but not the neural aspect. Age-related asynchronous activity of the auditory nerve probably contributes to age-related declines in temporal resolving abilities [25]. This may affect complex hearing tasks such as auditory discrimination testing in background noise.
Second, it is widely accepted that a longer duration of deafness left untreated is disadvantageous for cochlear implantation. In other words, a degeneration of central pathways results after a long-standing loss of sensory cells in the cochlea. Such an age-related auditory processing disorder or central presbyacusis affects speed of processing and results in poorer auditory understanding in noise [25]. Fortunately, such central presbyacusis severe enough to limit rehabilitation is uncommon. In a heart study cohort (Framingham) of 1026 people aged 64–92 years using multiple central auditory tests, it was concluded that central presbyacusis is not common and that it is difficult to separate the effects of peripheral from central abnormalities [25, 26].
Lastly, cognitive function, as cognitive degeneration is more apparent in older age, must be evaluated before implantation. Although most CI centers evaluate patients preoperatively for candidacy, it is often difficult to perform a proper evaluation due to the complexity of communication with a deaf patient and the limited time for examination. In a published panel discussion on cochlear implant candidacy, elderly, and residual hearing, it was mutually agreed by all panelists that a neurophysiologist is important in the evaluation of the elderly to verify that each patient has realistic expectations and has no significant cognitive deficits [27]. Overlooked patients with cognitive deficits or unexpected dementia can also affect study results or comparisons.
The abovementioned limitations are typical aspects that one must consider when reviewing the literature on this topic. The following aspects have been evaluated in this review in considering the clinical effectiveness of cochlear implantation in elderly patients:
-
1.
Auditory rehabilitation results of elderly patients based on the ages of 60, 65, 70, 75, and 80 compared to younger adult CI recipients. The studies were grouped together based on cutoff age defining an elder recipient.
-
2.
Surgical complications compared to younger cohorts
-
3.
Possible predictive factors in elderly CI candidates
-
4.
Quality of life improvement in comparison to preoperative status
Materials and Methods
The primary search for this review was conducted in July 2017 using the MEDLINE database including the literature published from 2000 to 2017. The following search strategies were used: “cochlear implantation” [MeSH terms] OR “cochlear implants” [all fields] AND “elderly” [all fields], yielding 113 results. Abstracts and titles were screened for relevance, and full articles of the selected papers were reviewed. The reference lists of relevant papers were further examined to recognize additional papers of interest. Inclusion criteria for articles at this stage were publications in the English and German language. A comparison of elderly to younger adult cohorts was necessary for inclusion of studies reporting hearing results, surgical complications, and predictive factors. Health-related quality of life reporting required comparisons of preoperative to postoperative values. After excluding papers which did not meet the inclusion criteria, 28 articles were included in this review.
Results
Auditory Rehabilitation
Elderly 60 and Older
The first subgrouping includes studies defining elderly as patients of 60 years of age and older, or 65 years of age and older. A total of nine studies fulfilled the inclusion criteria [5–13]. There were two long-term retrospective studies, one with a follow-up of 5 years [12] and a Korean study with a follow-up of 2 years [13]. All other studies had a mean follow-up of 12–14 months. As can be seen in Table 1, the studies included various multisyllabic and monosyllabic word recognition, free-field audiometry, and sentence testing. All testing except in the long-term study of Herzog et al. [12] was done in quiet conditions. All elderly cohorts showed a significant improvement in all test batteries after implantation and activation. The elderly cohorts never outperformed the younger counterparts, but mostly showed an insignificant slightly lower performance score. In the study of Mahmoud et al. [7], the elderly group performed significantly worse in the AzBio sentence testing, also revealing a significant correlation between age at implantation and AzBio scores. In the study of Roberts et al. [9], the elderly group performed significantly worse in the consonant-nucleus-consonant (CNC) test for monosyllables. It was further shown that the octagenarian subgroup was significantly worse than the younger elders in the elderly group.
In the study of Di Nardo et al. [5], a significant difference was shown in the Italian Turrini bisyllabic test and Burdo-Orsi sentence recognition test, showing better results in the younger control group. Only the last audiometric evaluation was used for the study with time of CI use ranging from 6 months to 15 years.
The only other study with a significant difference was by Lee et al. [13] showing a better performance for the younger group in the Korean Glendonald auditory screening and monosyllabic word test at 3 months and 1 and 2 years. The other tests performed—categories of auditory performance and bisyllabic word recognition—showed no significant difference.
The long-term study of Herzog et al. [12] showed no significant difference in the Freiburg monosyllable test at all test intervals; the Hochmair-Schulz-Moser (HSM) sentence test in quiet results was also similar at 1 year post implantation. The interesting finding, however, was that the elderly patients could only begin with the sentence test with a signal-to-noise ratio (SNR) of 10 or 15 dB after 2 years, and the difference between the groups was negligible only after 3 years. The older patients required 2–3 years longer to plateau in the HSM sentence test with noise in comparison to the younger adult group.
One study reported residual hearing results in electro-acoustic stimulation candidates, reporting that older adults over 65 years lost hearing in 16.12% of cases postoperatively, while it was only 1.95% in the younger adults [28].
Elderly 70 and Older
The second subgrouping includes studies defining elderly as patients of 70 years of age and older, as well as 75 years of age and older. A total of 11 studies fulfilled the inclusion criteria [3, 4, 14,22,16, 17••, 18,17,20,21, 22•]. As can be seen in Table 1, the studies included various multisyllabic and monosyllabic word recognition, free-field audiometry, and sentence testing. All elderly cohorts showed a significant improvement in all test batteries after implantation and activation. In most test results, the elderly cohorts showed an insignificant slightly lower performance score. Only in the study of Chatelin et al. [14] was there a significant better performance in the CNC test for the younger group at 12 months. A peculiar result in this study is that both groups reached a near maximal benefit in speech understanding after 3 months of implantation.
In three studies with sentence testing in noise, the speech understanding was similar in comparing groups; there were no significant differences for speech perception in noise with age: Hochmair-Schulz-Moser sentence test in noise (+ 15 dB SNR) with a mean follow-up of 21 months [3]; Göttingen sentence test in noise (+ 5 dB SNR) with a mean follow-up of 2.6–4 years [22•]; and HINT with speech spectrum noise (+ 10 dB SNR) with a mean follow-up of 21 months [16].
In the long-term studies, Jolink et al. [17••] reported on 20 elderly patients with a mean follow-up of 4.4 years. There was no significant difference in average speech discrimination between the elderly and control groups. The speech discrimination was stable over time, although the elderly had a larger intra-subject variability. In comparison, the study of Hilly et al. [18] divided the patients into three age groups (< 61, 61–70, > 70 years), and showed a significant difference in HINT scores in quiet at 1 year (p = 0.039) and at the last mean follow-up of 6.8 years (p = 0.054). Hearing scores were stable over a follow-up period of 6.8 years in all age groups. None of the elderly patients had a drop in hearing score of more than 20%.
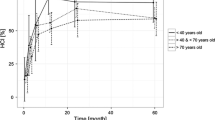
There was a similar age division in the study of Lenarz et al. [4••] (< 40, 40–59, 60–69, ≥ 70) in a cohort of 1005 postlingually deafened adults. There were similar learning curves among the groups over a 24-month period in the speech tracking test, Freiburger monosyllabic test, and HSM sentence test in quiet. There was a significant difference at 1 and 2 years only in the HSM sentence test in noise (− 10 dB SNR) when comparing the over 70-year-olds to the younger groups. An interesting finding in the study was that speech perception in noise for the 60–69-year-old group was comparable to the younger adults. A reduced speech perception in noise seemed to start from the age of 70 years in the cohort.
Elderly 79 and Older
The third subgrouping includes studies defining elderly as patients of 79 years of age and older. A total of two studies fulfilled the inclusion criteria. As can be seen in Table 1, the studies included various multisyllabic and monosyllabic word recognition, free-field audiometry, and sentence testing. Both elderly cohorts showed a significant improvement in speech perception after implantation and activation. In the study of Lundin et al. [23], the younger patients showed significantly better results in the monosyllabic word testing and a tendency toward better results in the bisyllabic testing. The results were for a postoperative interval of 6–12 months with no mean follow-up time reported. In addition, a comparison of the social environment showed no improvement in speech understanding when patients lived with one or several persons providing a better opportunity for oral communication.
In the study of Carlson et al. [24], with a mean follow-up of 1.6–2.3 years, there was only a significant difference in the AzBio sentence recognition score; the younger patients scored 6.5 percentage points better. Otherwise, there were no statistical differences in preoperative and postoperative speech perception scores between age groups.
Surgical and Anesthestic Risks
Many studies have also reported and compared perioperative and postoperative surgical and anesthetic-related complications. In the comparative studies of younger to older CI recipients, ten studies also reported complication rates [7, 9, 13, 14, 16, 19, 21, 23, 24, 29]. One further study was entirely devoted to this subject matter [30••]. Most studies showed a relatively low risk of surgical or anesthetic-related complications.
Surgical complications (flap necrosis, infection, dizziness, facial nerve injury, taste disturbance, etc.) were relatively similar when comparing the elderly to younger cohorts. In the studies of Chen et al. [29] and Rohloff et al. [21], there was a slightly higher prevalence of vestibular symptoms and dysgeusia.
In the study of Carlson et al. [24], patients 80 years or older experienced a small but statistically increased risk of perioperative anesthetic complication, requiring postoperative hospital admission and SICU monitoring more frequently. New or worsening perioperative dizziness was similar in both groups, occurring 20% in younger patients and 16% in the older group. No increased risk of poor wound healing, flap breakdown, or infection was found. Older patients did not experience a higher incidence of postoperative taste disorder or facial nerve weakness compared with the control group.
The study of Coelho et al. [30••] retrospectively divided patients older than 70 years into anesthetic risk groups based on the American Society of Anesthesiologists Physical Status Classification (ASA) in two groups, ASA l/ll and ASA lll/lV. There was no long-term morbidity and mortality, but there were three anesthesia-related complications in the latter group (4% overall): delayed extubation, postoperative congestive heart failure, and urinary retention. In general, anesthesia was well tolerated without risk in the majority of patients.
Predictive Factors
Although one may assume that predictive factors must be the same irrespective of age in the adult CI population, there are some intricacies. The elderly patients are more susceptible to cognitive deterioration and have more health risk factors. The duration of deafness may be substantially longer in the elderly, thereby affecting hearing outcome. Two studies focused on determining predictive factors of cochlear implant outcomes in the elderly.
In the study of Mosnier et al. [31], multivariate analysis of 94 implanted patients aged 65–85 years found better speech perception scores in patients with shorter duration of hearing deprivation, persistence of residual hearing for the low frequencies, the use of hearing aid before implantation, the absence of cardiovascular risk factors, and implantation in the right ear. The effect of age was only seen in difficult noisy conditions at an SNR 0 dB.
In the study of Lenarz et al. [4••], a factor analysis of 1005 postlingually deafened adults found no significant difference in the evaluation of duration of deafness, level of preoperative hearing, and type of implant system as three potential cofounders beyond age.
In the study of Leung et al. [8], a national cohort study of 749 cochlear implant recipients aged 14–91 years, as well as a multivariate regression analysis of preoperative and postoperative performance variables, was carried out. The study showed that age has a minimal effect on postoperative outcomes in the elderly. A more significant factor was the ratio of duration of deafness to age at implantation. Beyond a duration of deafness of 25 years, the older cohort demonstrated better performance than the younger cohort. A shorter percentage of life spent in deafness or near deafness is more important for auditory processing than the age at implantation.
Impact on Quality of Life
A further aspect in evaluating the impact of cochlear implantation in elderly patients is the benefit of implantation in terms of satisfaction and quality of life (QoL). There are few studies that provide preoperative to postoperative comparisons.
In the study of Hilly et al. [18], health survey scores (short form 36—SF36) improved significantly in both elderly patients over 70 years and the younger patients in “social functioning” and “mental health.” The elderly patients also perceived their “physical role functioning” performance to be significantly improved. Olze et al. [3] also reported using the SF-36; a significant improvement was only found in “social functioning” and “mental health,” but the physical component summary decreased.
Three studies used the Nijmegen cochlear implantation questionnaire (NCIQ) to evaluate health-related quality of life. In two of the studies, there was a significant improvement in the total score as well as all six subdomains [3, 32]; in the third study, only the subdomain “speech production” did not show a significant improvement [33]. The benefit was even higher in elderly patients than in younger counterparts [3]. The results indicated that the effect of cochlear implantation on HRQoL might outweigh improvements in speech perception, although the results differed among the studies if a correlation between NCIQ scores and speech perception exists.
Interestingly, two studies in addition to reporting changes in the QoL also studied psychopathological comorbidities [3, 33]. It was shown in both studies that the stress level (perceived stress questionnaire—PSQ), anxiety (general anxiety disorder-7 questionnaire), and depressiveness (depression scale—ADS-L) in elderly patients were on a low level preoperatively and, therefore, showed only minor improvements after CI. In a subgroup of stressed elderly patients, a reduction in the PSQ score was observed. This went along with a significantly less frequent application of the strategy “seeking support.”
A quality of life evaluation based on the Hearing Handicap Inventory for Adults (HHIA) showed a significant improvement in both subscales measuring emotional and situational impact of hearing loss [34]. A further study measured the health status based on the Health Utilities Index III showing a significant improvement for CI users [35].
Discussion
Comparison of studies on elderly cochlear implant recipients is troublesome due to different test batteries, age cutoffs, outcome measures, and language differences. The main universal agreement on outcome in this review is that all elderly cohorts had a significant improvement in speech understanding and a positive impact on quality of life after cochlear implantation without an increased surgical risk. It was irrelevant if elderly was defined at the age of 60 or 80 years.
A meta-analysis of scores on the same word and sentence tests in the various studies is perhaps feasible, but would not make much sense. There are many factors that can influence these scores, such as surgical procedure, length of electrode in the cochlea, implant manufacturer, external sound processor, cause of hearing loss, engagement with the rehabilitative program, true duration of deafness, residual hearing, and testing environment. Some of these biases are systematic biases (such as surgery, rehabilitation, or testing environment) that affect all groups being studied at a particular center. We, therefore, selected comparative studies of older to younger CI recipients to analyze hearing results, surgical complications, and quality of life assessments.
Cochlear implantation in postlingually deaf individuals greatly improves auditory recognition performance to an extent similar to that in younger patients. Although younger CI recipients plateau in their hearing recognition between 6 and 12 months, the older population may require 2–3 years of rehabilitation to have similar speech recognition especially in testing with background noise. In two studies, the elderly groups performed significantly worse in the AzBio sentence test. This may be a consequence of the higher memory and executive demands required in the test. All long-term studies showed speech discrimination performance to be stable over time in elderly CI recipients. However, the longer time required for hearing rehabilitation may also be offset by cognitive decay that can be of abrupt nature in septuagenarians and octogenarians. In a retrospective review in our cochlear implant pool, auditory therapy rehabilitation was not more time consuming in the elderly (≥ 70) compared to the younger counterparts [21].
Elderly patients, in general, show a postoperative recovery similar to younger CI patients. Nevertheless, preoperative evaluation of elderly patients is important due to increased risks for anesthetic complications such as ischemic stroke, transient ischemic attacks, and cardiac arrhythmia. The ASA score may be a better predictor of perioperative complication risk than age alone [30].
Predictive factors are contradictory, as some studies find correlations to certain factors, and others dispute the same factors. Duration of deafness seems to be the most redundant factor supported in most studies. The relative duration of deafness (ratio of duration of deafness to age at implantation) seems to be more important than the absolute duration of deafness. If the moderate-to-profound hearing loss occurs at a young age before deafness in postlingually deaf adults, this may limit language development.
It is more common to have comorbidities in the elderly population such as vision problems, onset of dementia, decrease in proprioception or motor function, and dexterity difficulties, which make therapy difficult. Extensive preoperative counseling in elderly patients is necessary not only for the candidacy evaluation but also to talk about realistic expectations after implantation.
In 2004, the UK CI Study Group concluded that cochlear implantation was cost-effective even in elderly patients with less than a 10-year predicted life span. When considering the above reviewed positive outcomes in the elderly population, age seems to be a minor factor in CI candidacy.
Conclusion
Postoperative speech recognition is, in general, on a similar level to younger adults both in quiet and noise. Elderly patients require longer periods of time for rehabilitation. Future studies should be based more on a 2–3-year evaluation period, rather than 6–12 months. Long-term speech recognition results seem to be stable over time, when cognitive decay is not apparent. There is a relatively low morbidity in the elderly CI recipients, but proper preoperative anesthiologic assessment must be made to optimize medical comorbidities and prevent perioperative anesthetic complications. CI has a positive effect on quality of life that may even outweigh improvements in hearing ability measured by speech perception tests.
CI candidacy in elderly patients must be made on an individual basis, dependant on overall health as well as cognitive status. Advanced age alone is not a contraindication when determining candidacy for cochlear implantation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Pacala JT, Yueh B. Hearing deficits in the older patient: “I didn’t notice anything”. JAMA. 2012;307(11):1185–94.
Cherko M, Hickson L, Bhutta M. Auditory deprivation and health in the elderly. Maturitas. 2016;88:52–7.
Olze H, Grabel S, Forster U, Zirke N, Huhnd LE, Haupt H, et al. Elderly patients benefit from cochlear implantation regarding auditory rehabilitation, quality of life, tinnitus, and stress. Laryngoscope. 2012;122(1):196–203.
•• Lenarz MSH, Joseph G, Büchner A, Lenarz T. Cochlear implant performance in geriatric patients. Laryngoscope. 2012;122:1361–5. High-quality study with large cohort of 1005 postlingually deafened adults with test battery in quiet and noise over a 24-month period.
Di Nardo W, Anzivino R, Giannantonio S, Schinaia L, Paludetti G. The effects of cochlear implantation on quality of life in the elderly. Eur Arch Otorhinolaryngol. 2014;271(1):65–73.
Ghiselli S, Nedic S, Montino S, Astolfi L, Bovo R. Cochlear implantation in post-lingually deafened adults and elderly patients: analysis of audiometric and speech perception outcomes during the first year of use. Acta Otorhinolaryngol Ital: Organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale. 2016;36(6):513–9.
Mahmoud AF, Ruckenstein MJ. Speech perception performance as a function of age at implantation among postlingually deaf adult cochlear implant recipients. Otology Neurotol: Off Publ Am Otological Soc Am Neurotol Soc Eur Acad Otol Neurotol. 2014;35(10):e286–91.
Leung J, Wang NY, Yeagle JD, Chinnici J, Bowditch S, Francis HW, et al. Predictive models for cochlear implantation in elderly candidates. Arch otolaryngol head neck surg. 2005;131(12):1049–54.
Roberts DS, Lin HW, Herrmann BS, Lee DJ. Differential cochlear implant outcomes in older adults. Laryngoscope. 2013;123(8):1952–6.
Haensel J, Ilgner J, Chen YS, Thuermer C, Westhofen M. Speech perception in elderly patients following cochlear implantation. Acta Otolaryngol. 2005;125(12):1272–6.
Hay-McCutcheon MJ, Pisoni DB, Kirk KI. Audiovisual speech perception in elderly cochlear implant recipients. Laryngoscope. 2005;115(10):1887–94.
Herzog M, Schon F, Muller J, Knaus C, Scholtz L, Helms J. Long term results after cochlear implantation in elderly patients. Laryngorhinootologie. 2003;82(7):490–3.
Lee S, Park HJ, Cho HH, Cho YB. Speech perception and auditory performance following cochlear implantation in elderly Koreans. Ear, nose, & throat journal. 2017;96(3):112–8.
Chatelin V, Kim EJ, Driscoll C, Larky J, Polite C, Price L, et al. Cochlear implant outcomes in the elderly. Otol neurotol: Off Publ Am Otological Soc, Am Neurotol Soc Eur Acad Otol Neurotol. 2004;25(3):298–301.
Hiel AL, Gerard JM, Decat M, Deggouj N. Is age a limiting factor for adaptation to cochlear implant? Eur Arch Otorhinolaryngol. 2016;273(9):2495–502.
Poissant SF, Beaudoin F, Huang J, Brodsky J, Lee DJ. Impact of cochlear implantation on speech understanding, depression, and loneliness in the elderly. J Otolaryngol - head & neck surgery = Le Journal d'oto-rhino-laryngologie et de chirurgie cervico-faciale. 2008;37(4):488–94.
•• Jolink C, Helleman HW, van Spronsen E, Ebbens FA, Ravesloot MJ, Dreschler WA. The long-term results of speech perception in elderly cochlear implant users. Cochlear Implants Int. 2016;17(3):146–50. Long-term study with a mean follow-up of up to 5.3 years with well-documented performance over time in elderly patients.
Hilly O, Hwang E, Smith L, Shipp D, Nedzelski JM, Chen JM, et al. Cochlear implantation in elderly patients: stability of outcome over time. J Laryngol Otol. 2016;130(8):706–11.
Buchsenschutz K, Arnolds J, Bagus H, Fahimi F, Gunnicker M, Lang S, et al. Surgical risk profile and audiological outcome in the elderly after cochlea-implantation. Laryngorhinootologie. 2015;94(10):670–5.
Budenz CLCM, Coelho DH, Birenbaum B, et al. The effects of cochlear implantation on speech perception in older adults. JAGS. 2011;59:446–53.
Rohloff K, Koopmann M, Wei D, Rudack C, Savvas E. Cochlear implantation in the elderly: does age matter? Otology & neurotology: official publication of the American Otological Society. Am Neurotol Soc Eur Acad Otol Neurotol. 2017;38(1):54–9.
• Hast A, Schlucker L, Digeser F, Liebscher T, Hoppe U. Speech perception of elderly cochlear implant users under different noise conditions. Otol Neurotol: Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol. 2015;36(10):1638–43. Study evaluating performance of eldery CI recipients in different noise conditions.
Lundin K, Nasvall A, Kobler S, Linde G, Rask-Andersen H. Cochlear implantation in the elderly. Cochlear Implants Int. 2013;14(2):92–7.
Carlson ML, Breen JT, Gifford RH, Driscoll CL, Neff BA, Beatty CW, et al. Cochlear implantation in the octogenarian and nonagenarian. Otology & neurotology: official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2010;31(8):1343–9.
Gates GA, Mills JH. Presbycusis. Lancet (London, England). 2005;366(9491):1111–20.
Cooper JCGG. Hearing in the elderly: the Framingham cohort, 1983-1985: part II. Prevalence of central auditory processing disorders. Ear Hear. 1991;12:304–11.
Backous DDDR, Manrique M, et al. Panel discussion IV: cochlear implant candidacy, elderly and residual hearing. Ear Hear. 2007;28(2):128–9.
Skarzynski PH, Olszewski L, Lorens A, Wlodarczyk AW, Skarzynski H. Cochlear implantation in the elderly. Audiol neuro-otol. 2014;19(Suppl 1):33–5.
Chen DSCD, Lingsheng L, Bowditch SP, et al. Cochlear implantation in older adults: long-term analysis of complications and device survival in a consecutive series. Otol Neurotol. 2013;34(7):1272–7.
•• Coelho DH, Yeh J, Kim JT, Lalwani AK. Cochlear implantation is associated with minimal anesthetic risk in the elderly. Laryngoscope. 2009;119(2):355–8. The retrospective study clearly identified the importance of preoperative evaluation of comorbidities to prevent anesthetic complications.
Mosnier I, Bebear JP, Marx M, Fraysse B, Truy E, Lina-Granade G, et al. Predictive factors of cochlear implant outcomes in the elderly. Audiology & neuro-otology. 2014;19(Suppl 1):15–20.
Mosnier I, Bebear JP, Marx M, Fraysse B, Truy E, Lina-Granade G, et al. Improvement of cognitive function after cochlear implantation in elderly patients. JAMA otolaryngology-- head & neck surgery. 2015;141(5):442–50.
Knopke S, Grabel S, Forster-Ruhrmann U, Mazurek B, Szczepek AJ, Olze H. Impact of cochlear implantation on quality of life and mental comorbidity in patients aged 80 years. Laryngoscope. 2016;126(12):2811–6.
Vermeire K, Brokx JP, Wuyts FL, Cochet E, Hofkens A, Van de Heyning PH. Quality-of-life benefit from cochlear implantation in the elderly. Otology & neurotology: official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2005;26(2):188–95.
Manrique-Huarte R, Calavia D, Huarte Irujo A, Giron L, Manrique-Rodriguez M. Treatment for hearing loss among the elderly: auditory outcomes and impact on quality of life. Audiol neuro-otol. 2016;21(Suppl 1):29–35.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Otology
Rights and permissions
About this article
Cite this article
Savvas, E., Rudack, C. Cochlear Implantation in the Elderly: Review on the Clinical Effectiveness. Curr Otorhinolaryngol Rep 5, 295–303 (2017). https://doi.org/10.1007/s40136-017-0166-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-017-0166-0