Abstract
Purpose of the Review
Esophageal atresia remains a complex congenital anomaly that manifests in a number of different variants ranging from pure atresia to trachea-esophageal fistula without atresia. The surgical treatment options have continued to evolve with advances in technology and innovative procedures but the results for the patients with long-gap atresia remain challenging.
Recent Findings
Documenting the outcomes from interventions in this population is difficult given the limited experience at most centers and the heterogeneity of the anomalies and the treatments. Several recent studies have provided comparison data for some newer. Studies demonstrate better results in primary procedures than secondary operations but significant morbidity remains.
Another innovation has been application of minimally invasive procedures to all forms of esophageal atresia. Reports of excellent results are encouraging with a theoretical reduction in the risk of long-term chest wall abnormalities.
Summary
Esophageal atresia remains one of the most challenging congenital abnormalities requiring surgical intervention. While some progress has been made, dramatic impact awaits advances in tissue engineering or other game changing developments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
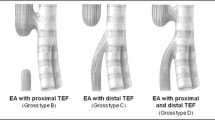
Esophageal atresia (EA) with or without tracheoesophageal fistula (TEF) is a classic surgical congenital anomaly affecting newborn infants. Three quarters of patients present with atresia of the esophagus and a fistulous connection of the distal esophagus to the airway just above the carina. The remainder presents with either pure esophageal atresia, esophageal atresia with uncommon tracheal fistulas or tracheal fistulas in the absence of esophageal atresia. The heterogeneity of these anatomical variants can have significant impact on the short- and long-term outcomes of those with the anomaly. In addition to the impact of the esophageal anomaly alone, many patients have associated congenital defects that contribute to the complexity of the long-term outcomes. While congenital cardiac defects play an important role in overall survival, associated bowel and urogenital defects contribute to long-term morbidity. The goal of surgical therapy is to establish continuity of the esophagus and separate the esophagus from the airway.
Factors Impacting Overall Survival
When the anatomy is favorable, the repair is without complication, and there are no associated anomalies, the result is usually excellent. More commonly, complications and comorbidities complicate the clinical course. Historically, prematurity, associated anomalies and low birth weight have been associated with significantly worse outcomes. Spitz et al. reported a large series of 357 infants with esophageal atresia and 15 with H-type tracheooesphageal fistula treated from 1980 through 1992. In that series reported in 1994, two criteria were found to be important predictors of outcome: birth weight of less than 1500 g and the presence of major congenital heart disease. Based on their assessment, a new classification system was proposed to replace the classic Waterston system. The proposed three groups were based on weight and associated cardiac disease. Group I: birth weight > 1500 g, without major cardiac disease (survival 97%); group II: birth weight < 1500 g, or major cardiac disease (survival 59%); and group III: birth weight < 1500 g, and major cardiac disease (survival 22%) [1].
However, a more recent series suggest that as neonatal care and treatment of congenital heart disease improves, the outcomes for patients with EA/TEF continue to improve. Hartley et al. found an overall survival of 87% with only cardiac and renal anomalies associated with an increased risk of mortality while birth weight had less significance than previously reported [2]. Okamoto proposed a revision of the Spitz criteria to create four groups using birthweight above or below 2000 g and the presence or absence of other major anomalies. Using those criteria, overall survival was increased over two consecutive time periods (Table 1) [3].
Short-Term Outcomes
The heterogeneity of EA/TEF results in a varied array of surgical interventions based on the anatomic defect and local bias for the more complex cases. Ideally, a primary repair of the atresia is completed resulting in a widely patent anastomosis and early oral feeding. Unfortunately, many cases are plagued by anatomic challenges and surgical complications. The variety of initial interventions is evident in the recent report of the French national experience reported by Sfeir et al. [4]. In that series, the diagnosis of EA/TEF was established on the first day of life in 93.5% of cases an initial procedure was performed in 83% of patients by 48 h of life. The procedures performed are listed in Table 2. The median artificial ventilation duration was 3 days (range, 0–117 days). The median length of hospital stay was 22 days (range, 2–393 days) for the series.
Surgical complications are common in the initial management of patients with EA/TEF. Lal et al. published a retrospective series of 396 patients from 11 children’s hospitals in the USA [5••]. In that series, the overall complication rate was 62% with anastomotic strictures (40%) and anastomotic leak (23%) being most common. The complications are listed by type of atresia in Table 3 [5••].
This is a large series of over 400 patients comparing surgical approaches and outcomes.
Long-Gap Esophageal Atresia
Perhaps, the most challenging cases are those in which the gap between proximal and distal esophagus prevents a primary anastomosis. One of the challenges in evaluating the literature for the surgical treatment of long-gap esophageal atresia is the lack of a uniformly accepted definition for the entity. Some have used a cutoff of a 2 cm gap to define a long gap [6] while others use 3 cm or more [7,8,9]. In addition, there is no standard for the technique by which the gap is measured. Thus, a gap measured by contrast study might be completely different than a gap measured while the esophageal ends are under tension or traction in the same patient. In the end, the definition becomes more of a functional one. Practically, long-gap esophageal atresia is one in which the ends of the esophagus cannot be brought together for a primary anastomosis without employing alternative techniques and the short- and long-term outcome for these patients is likely worse than for those in whom a primary anastomosis is achieved.
Numerous techniques have been described for bridging the gap in cases of long-gap esophageal atresia. Currently, the most common approaches include esophageal elongation, gastric transposition, jejunal interposition, and colonic interposition. There are many variations of each technique and each has associated short- and long-term complications. Gastric transposition has the advantage of a single anastomosis but concerns for long-term gastroesophageal reflux. Jejunal interpositions have tenuous blood supply but provide a better size match for the esophagus and colonic interpositions have a high leak and stricture rate acutely and problems with a redundant conduit long term. Esophageal elongation procedures have gained some popularity and an excellent review of the experience with the Foker procedure has recently been published. Esophageal continuity was achieved in 96% of primary cases and 68% of secondary cases. The overall results of the study are shown in Table 4. Successful esophageal anastomosis required 2–15 thoracotomies (mean 2 in primary and 5 in secondary repairs). Full oral nutrition was achieved in 63% of primary repairs and 9% of secondary repairs [10••].
Long-Term Outcomes
Until recently, little attention has been paid to outcomes beyond the neonatal period. However, as increasing numbers of patients survive into adulthood, there has been increasing recognition that complications continue well past the acute problems with anastomostic leaks and strictures. The chronic complications associated with EA/TEF most commonly relate to problems with gastroesophageal reflux (GERD), feeding and growth, and respiratory/airway issues.
Gastroesophageal Reflux
Gastroesophageal reflux in patients with EA/TEF is common being reported in 20–60% of patients. The ESPGHAN-NASPGHAN guidelines for the evaluation and treatment of GERD in EA/TEF have recently been published and provides an extensive literature review of the topic [11••]. The guidelines address a wide range of clinical questions regarding the work up and treatment of GERD. In general, there is strong support for aggressive diagnosis and treatment of GERD in the first year of life and a recognition the potential long-term sequelae of esophagitis, Barrett’s esophagus and the potential for malignant transformation must be monitored on a lifelong basis. The gold standard for diagnosis is pH probe or impedance testing and proton pump inhibitors are the initial therapy of choice as indicated in Fig. 1.
Additional algorithms are presented for symptomatic patients and those with strictures. Fundoplication is supported for cases of GERD refractory to medical management and is performed in 20–40% of patients. However, the quality of the evidence in the literature to support the use of fundoplication is lacking and the impact on outcomes has been challenged [12].
Feeding and Growth
Feeding issues are common and result from esophageal dysmotility, esophagitis, and potential partial obstruction. Overall, approximately half of all patients suffer from dysphagia [13•]. Both oropharyngeal and esophageal dysmotility are common and can be demonstrated in 70–80% of patients by manometry. The work up of dysphagia should include endoscopy, esophagram, and manometry to properly characterize the physiologic and mechanical factors that might contribute to the problem [14]. Dysphagia remains a lifelong problem for the majority of EA/TEF patients. In a single institution long-term follow-up survey of EA/TEF patients, the results suggest that 82% of patients have some degree of swallowing dysfunction that is worse with solids and requires sips of liquids to facilitate swallowing. However, the swallowing dysfunction was mild and did not impact daily living. In fact, a quality of life assessment did not differ from the general population [15]. Not surprisingly, patients with EA/TEF have issues with growth failure early in life but longitudinal studies have not completely characterized the amount of catch up growth that occurs later in life. Table 5 summarizes growth and neurodevelopmental data from a recent review of the literature [16].
Respiratory and Airway Issues
Evidence of the early morbidity related to respiratory problems is reflected in the French national study in which 59% of the patients required readmission during the first year of life and 48% of those readmissions were due to respiratory issues [4]. An extensive review of the literature by Mira et al. confirmed that lower respiratory tract infection is frequent, especially in the first years of life. As childhood progresses, asthma, chronic cough, and recurrent bronchitis are the most common respiratory complaints. Reported spirometry data suggests that restrictive lung disease is more common than obstructive or mixed patterns, and, overall, bronchial hyperresponsiveness can affect up to 78% of patients [17]. Unfortunately, the respiratory problems continue beyond infancy and childhood. A German study in which 58 patients more than 20 years out from EA/TEF repair identified respiratory issues characterized by chronic cough and frequent periods of bronchitis in 60%, and shortness of breath in 30% of patients [18]. Similarly, a systematic review by Conner et al. found recurrent respiratory tract infections in 24.1%, doctor diagnosed asthma in 22.3%, persistent cough in 14.6%, and wheezing in 34.7% [19].
Mechanical airway issues including recurrent tracheoesophageal fistulas and tracheomalacia undoubtedly contribute to ongoing respiratory problems. Tracheomalacia is reported in 11–33% of patients with EA/TEF and can cause long-term complications. Traditional treatment options include tracheostomy, tracheal resection, and aortopexy. More recently, posterior tracheopexy has been described as an alternative approach that can provide an improved result along a longer length of the trachea [20]. Long-term outcome data is lacking for the impact of tracheomalacia on respiratory function and risk of long-term damage to the lungs.
Recurrent tracheoesophageal fistulas occur in 5–10% of patients and can be troublesome. The diagnosis can be difficult and often requires either a careful radiographic study, a targeted bronchoscopy, or both to define the anatomy. The standard approach involves takedown of the fistula with interposition of autologous material between the trachea and the esophagus. Unfortunately, recurrences are common. More recently, excellent results for the repair of complex recurrent fistulas has been reported using two newer approaches. Jennings advocates a complete separation of the trachea and the esophagus [21] and Rutter has employed a tracheal slide procedure to close the defect [22].
Quality of Life
Finally, increasing amounts of information is accumulating regarding the long-term outcomes for patients with regard to quality of life. When considered as a group, EA/TEF patients tend to have a general quality of life comparable with the general population although the chronic health issues detailed above result in lower health-related QoL scores [23]. However, the results are not as promising when patients with more complicated clinical courses are assessed. A recent survey of a German EA/TEF group revealed a high prevalence of Gastrointestinal and respiratory symptoms [24•] (Table 6).
Adults demonstrated impaired well-being according to WHO-score and gastrointestinal function (GIQLI).
Conclusion
Survival, short- and long-term outcomes continue to improve for patients with EA/TEF. Uncomplicated cases with few or no associated anomalies can be expected to do well over time. However, there are many opportunities to improve the outcomes for the complex patients with chronic gastrointestinal and/or respiratory complications. Clearly, patients who require an esophageal replacement or extensive elongation procedures have worse outcomes than those in whom esophageal continuity can be established with the native esophagus. The potential use of regenerative medicine and a tissue engineered esophagus holds promise for the future but in the interim, new techniques are needed to improve the outcomes for the difficult esophageal and tracheal complications of EA/TEF.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Spitz L, Kiely EM, Morecroft JA, Drake DP. Oesophageal atresia: at-risk groups for the 1990s. J Ped Surg. 1994;29:723–5.
Hartley MJ, Smith NPM, Jaffray B. Statistical modelling of survival for babies with oesophageal atresia. J Ped Surg. 2016;51:1110–4.
Okamoto T, Takamizawa S, Arai H, Bitoh Y, et al. Esophageal atresia: prognostic classification revisited. Surgery. 2009;145:675–81.
Sfeir R, Khen-Dunlop N, et al. Esophageal atresia: data from a national cohort. J Ped Sur. 2013;48:1664–9.
•• Lal DR, et al. Perioperative management and outcomes of esophageal atresia and tracheoesophageal fistula. J Pediatr Surg. 2016; doi:10.1016/j.jpedsurg.2016.11.046. This is a large series of over 400 patients comparing surgical approaches and outcomes
Hands LJ, Dudley NE. A comparison between gap length and Waterson classifications as guides to mortality and morbidity after surgery for esophageal atresia. J Pediatr Surg. 1986;21(5):404–6.
Brown AK, Tam PKH. Measurement of gap length in esophageal atresia: a simple predictor of outcome. J Am Coll Surg. 1996;182(1):41–5.
Foker JE, Linden BC, Boyle EM, et al. Development of a true primary repair for the full spectrum of esophageal atresia. Ann Surg. 1997;226(4):533–43.
Coran AG. Ultra-long gap esophageal atresia: how long is long? Ann Thorac Surg. 1994;57:528–9.
•• Bairdain S, Hamilton TE, Smithers CJ, Manfredi M, Ngo P, Gallagher D, Zurakowski D, Foker JE, Jennings RW. Foker process for the correction of long gap esophageal atresia: primary treatment versus secondary treatment after prior esophageal surgery. J Pediatr Surg. 2015;50(6):933–7. The paper presents comprehensive data on the outcomes and morbidities associated with the esophageal elongation technique described by Foker
•• Krishnan U, Mousa H, Dall’Oglio L, et al. ESPGHAN-NASPGHAN guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with esophageal atresia-tracheoesophageal fistula. JPGN. 2016;63:550–70. This provides algorithms for long term monitoring of patients with a histry of esophageal atresia
Jancelewicz T, Lopez ME, Downard CD, et al. Surgical management of gastroesophageal reflux disease (GERD) in children: a systematic review. J Pediatr Surg. 2016; doi:10.1016/j.jpedsurg.2016.09.072.
• Connor MJ, Springford LR, Kapetanakis VV, Giuliani S. Esophageal atresia and transitional care-step 1: a systematic review and meta-analysis of the literature to define the prevalence of chronic long-term problems. Am J Surg. 2015;209(4):747–59. Systematic review of long term outcomes
Mahoney L, Rosen R. Feeding difficulties in children with esophageal atresia. Paediatr Respir Rev. 2016;19:34–8.
Gibreel W, Zendejas B, Antiel RM, Fasen G, Moir CR, Zarroug AE. Swallowing dysfunction and quality of life in adults with surgically corrected esophageal atresia/tracheoesophageal fistula as infants: forty years of follow-up. Ann Surg. 2016; doi:10.1097/SLA.0000000000001978.
IJsselstijn H, Gischler SJ, Toussaint L, et al. Growth and development after oesophageal atresia surgery: need for long-term multidisciplinary follow-up. Paediatr Respir Rev. 2016;19:34–8.
Mirra V, Maglione M, Di Micco LL, Montella S, Santamaria F. Longitudinal follow-up of chronic pulmonary manifestations in esophageal atresia: a clinical algorithm and review of the literature. Pediatrics and Neonatology. 2016; doi:10.1016/j.pedneo.2016.03.005.
Ure B, Slany E, Eypasch EP, et al. Quality of life more than 20 years after repair of esophageal atresia. J Ped Surg. 1998;33:51 I–515 511.
Connor MJ, Springford LR, Kapetanakis VV, Giuliani S. Esophageal atresia and transitional care step 1: a systematic review and meta-analysis of the literature to define the prevalence of chronic long-term problems. Am J Surg. 2015;209:747–59.
Fraga JC, Jennings JW, Kim PC. Pediatric tracheomalacia. Seminars Ped Surg. 2016;25:156–64.
Smithers CJ, Hamilton TE, Manfredi MA, Rhein L, Ngo P, Gallagher D, Foker JE, Jennings RW. Categorization and repair of recurrent and acquired tracheoesophageal fistulae occurring after esophageal atresia repair. J Pediatr Surg. 2016; doi:10.1016/j.jpedsurg.2016.08.012.
Provenzano MJ, Rutter MJ, von Allmen D, Manning PB, Paul Boesch R, Putnam PE, Black AP, de Alarcon A. Slide tracheoplasty for the treatment of tracheoesophogeal fistulas. J Pediatr Surg. 2014;49:910–4.
Roberts K, Karpelowsky J, Fitzgerald DA, Soundappan SS. Outcomes of oesophageal atresia and tracheo-oesophageal fistula repair. J Paediatr Child Health. 2016;52(7):694–8. doi:10.1111/jpc.13211.
• Dingemann C, Meyer A, Kircher G, Boemers TM, Bernhard V, Till H, Ure BM. Long-term health-related quality of life after complex and/or complicated esophageal atresia in adults and children registered in a German patient support group. J Pediatr Surg. 2014;49:631–8. This is important outcome data from a select patient perspective
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Daniel von Allmen has no conflict of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Surgical
Rights and permissions
About this article
Cite this article
von Allmen, D. Long- and Short-Term Outcomes of Tracheo-Oesophageal Fistula and Esophageal Atresia. Curr Pediatr Rep 5, 45–51 (2017). https://doi.org/10.1007/s40124-017-0124-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-017-0124-9