Abstract
The ethanol extract of Phyllanthus amarus (Schum and Thonn), a plant of ethnomedicinal importance, was formulated into herbal cream and ointment and evaluated using physicochemical, safety and antimicrobial properties. The extract was obtained by maceration and the antimicrobial properties tested on clinically isolated pathogenic bacteria (Staphylococcus aureus and Pseudomonas aeruginosa) and dermatophytes (Trichophyton rubrum and Candida albicans) using established methods. Cream and ointment formulations containing 1–10 % w/w extract was prepared and 4 % w/w humectant (glycerin) was incorporated into the cream while 5 % w/w surfactant (cetomacrogol 1000) was incorporated to the ointment. The results showed that the pH of the formulations was acidic and the viscosity ranged from 1250 to 4950 cP for ointments and 570–1233 cP for creams. The presence of humectant and surfactant significantly (p < 0.05) reduced the viscosities of the formulations. The results of dermal irritation showed negligible irritation index while sub-chronic toxicity tests showed that the formulations did not cause any visible lesions in the skin of the animals after application for twenty-one days. The in vitro antimicrobial properties of formulations were concentration-dependent with the creams showing higher activity. Furthermore, the in vivo activity of the cream on S. aureus showed increased antibacterial activity with increase in extract concentration and humectant presence. The herbal cream and ointment of Phyllanthus amarus extract had acceptable physicochemical and safety profiles with significant (p < 0.05) in vitro and in vivo antimicrobial activity. Thus, the formulations could be useful in the treatment of skin infections instead of using the extract for bathing and rubbing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pharmaceutical semi-solid preparations are topical products intended for application to the skin or accessible mucous membrane to provide local or sometimes systemic effects at application sites (Betageri and Prablu 2002). Topical agents like creams and ointments are more attractive than oral therapy because they reduce the potential for systemic adverse reactions. They are also suitable for self-administration of medication since no specialized appliances or personnel are required leading to improved patient compliance. Efficacy is also achieved by lower total daily dosage of drug since it is applied directly to the affected area (Martin et al. 2005).
Creams are non-greasy viscous systems with opaque appearance in contrast to ointments which are more viscous and translucent (Buhse et al. 2005). The base for creams is usually an oil-in-water emulsion or aqueous microcrystalline dispersion of long-chain fatty acids or alcohols that are water-washable and are cosmetically and aesthetically acceptable. On the other hand, ointments are greasy preparations that contains dissolved or dispersed drug (Idson and Lazarus 1991). The ointment is expected to soften or liquefy on application to the skin, so as to permit the medicament to exert the desired effect. Ointments contain fatty compounds having the consistency of butter with bases such as hydrocarbons, vegetable oils and silicones. Although creams and ointments are both semi solids, ointments have <20 % water plus volatiles compared to cream with >40 % water and volatiles (Ansel et al. 2005). Therapeutically, creams are considered to be particularly suited for application to oozing wounds while ointments are indicated for chronic, dry lesions and contraindicated in exudative lesions (Reuter et al. 2010).
The traditional treatment of dermatologic conditions using topical preparations obtained from plants is an age-long practice which remains relevant even today in industrialized countries (Brown and Dattner 1998). Herbal remedies for skin care with antibacterial and antifungal activities have been prepared from a variety of plant parts such as leaves, stem, root, bark or fruits and are topically administered as solvent extracts, creams, ointments, lotions, gels or soaps (Nebedum et al. 2009).
Phyllanthus amarus (P. amarus) Schum and Thonn (family Euphorbiaceae) is a perennial herb that is widely distributed in almost all tropical countries including America, India and Nigeria. The plant commonly called ‘stonebreaker’, ‘windbreaker’, ‘gulf leaf flower’ or ‘gala of wind’ (Adegoke et al. 2010) is ethnobotanically used in the treatment of various diseases and disorders. The leaves are used as expectorant and diaphoretic, and the fruits as carminative, laxative, astringent, diuretic, diaphoretic and tonic to the liver (Naaz et al. 2007). The plant parts have been found to exhibit antiviral activity in Hepatitis B virus infection (Xinhua 2001), antidiabetic (Moshi et al. 2001), hepatoprotective (Faremi et al. 2008), and antimicrobial activity (Mazumder et al. 2006). Furthermore, the ethanol extract of the whole plant of P. amarus has been shown to possess repository and chemotherapeutic effects against resistant strains of P. yoelii in Swiss albino mice (Ajala et al. 2011). The antiplasmodial effects of the extracts were comparable with standard chemotherapeutic and chemoprophylactic drugs used in chloroquine resistant malaria. The phytochemical constituents of P. amarus are alkaloids, flavonoids, hydrolysable tannins, polyphenols and lignans (Faremi et al. 2008). The ethanol extract of P. amarus has demonstrated significant antimicrobial activity against S. typhi (Eldeen et al. 2011) and β lactamase producing E. coli isolated from the stool samples of HIV patient (Akinjogunla et al. 2010). This indicates the usefulness of the extract in the treatment of microbial infections.
Thus in the present study, P. amarus ethanol extract has been formulated into herbal creams and ointments for use as topical antimicrobial agents. The physicochemical, safety and in vitro antimicrobial properties of the formulations against bacteria and dermatophytes were investigated. Furthermore, the formulation with optimal performance was explored for in vivo antibacterial activity by topical application on Sprague–Dawley rats infected with clinical isolates of S. aureus from skin infections.
Materials and methods
Materials
Microorganisms
The bacteria used were clinical isolates from skin infections obtained from the Department of Medical Microbiology, University College Hospital, Ibadan, Nigeria. It comprises of one gram-negative (Pseudomonas aeruginosa), and one gram-positive (Staphylococcus aureus) bacteria. The dermatophytes-Candida albicans and Trychophyton rubrum were obtained from laboratory stock of the department of Pharmaceutical Microbiology, University of Ibadan, Nigeria. S. aureus was re-isolated two times on Mannitol Salt Agar (MSA, Biowark Lab. Pune, India) and P. aeruginosa was re-isolated in Oxoid Cetrimide Agar (Thermo Fisher Scientific, Inc.,U.K), while the strains of fungi were re-isolated in Sabouraud Dextrose Agar (SDA, Biolife Laboratories, V. Le Monza, Italy). All organisms were maintained on agar slopes at 4 °C and sub-cultured for 24 h before use.
Experimental animals
All animals (rats and rabbits) used in this experiment were obtained from the Animal House of the Faculty of Veterinary Medicine, University of Ibadan, Nigeria. The animals were housed individually in standard cages and allowed to acclimatize for 14 days before the commencement of the experiments. The animals were allowed free access to both feed (Ladokun Feeds, Ibadan, Nigeria) and water ad libitum. All animal experiments followed national and institutional guidelines in accordance with the revised National Institute of Health standards for the Care and Use of Laboratory Animals (Grosblatt 1978).
Methods
Plant collection and preparation
Fresh samples of Phyllanthus amarus were collected in the morning in the months of May to August from the natural habitat in Sagamu, Ogun state, Nigeria. The plant was identified and authenticated at the Forestry Research Institute of Nigeria (FRIN), Ibadan, Nigeria with voucher number 108345. The plant was cleaned, cut and dried in the shade for 2 weeks and then in the oven (Model BS 250, GallenKamp Co., UK) at 40 °C for 4 h. The dried plant was powdered using a laboratory mill (Kenwood Ltd, Hertfordshire, UK) and kept in airtight container until needed.
Plant extraction
One kilogram of the powdered plant material was macerated for 72 h with 4 L of absolute ethanol (96 %), and then filtered using a Whatman filter paper (Whatman Plc., Kent, UK). The extract was concentrated in vacuo at 40 °C using a rotary evaporator (Buchi Model R210, Switzerland). The remaining solvent in the residue was evaporated in a vacuum dessicator.
Preparation of creams and ointment formulations
Aqueous cream BP, used as the base for the creams, was prepared using established methods (BPC 1979). Briefly, emulsifying ointment (30 % w/w) was melted on a water bath (I) and chlorocresol (0.1 % w/w) was dissolved in purified water (69.9 % w/w) with the aid of gentle heat (II). The solution (II) was added to the melted wax (I) while still hot with continuous stirring until it was cold. Cream formulations containing four different concentrations of the extract (12.5, 25, 50 and 100 mg/ml) were prepared by mixing the required quantity of extract with the cream base by continuous stirring until an elegant product was formed. Cream formulations containing humectant (4 % w/w glycerin) were prepared by mixing the appropriate quantity of glycerin with the extract before incorporating into the base.
Simple ointment BPC, used as the base for the ointment was prepared by fusion method (BPC 1979). The ingredients for the base (5 % woolfat, 5 % hard paraffin, 5 % cetostearyl alcohol and 85 % yellow soft paraffin) were all melted together and stirred gently until cold (40 °C). Phyllanthus amarus extract was gradually incorporated into the base with continuous stirring to obtain a homogeneous preparation. Ointment formulations containing cetomacrogol 1000 as surfactant was prepared by mixing Simple ointment BPC (prepared as above) and P. amarus extract (oil phase). The surfactant (aqueous phase) was melted separately and added to the oil phase at equal temperature. The mixture was then stirred gently until cold. Details of the composition of the cream and ointment formulations are presented in Table 1.
Evaluation of physicochemical parameters
The pH of the formulations was measured at 27 ± 2 °C using a pH meter (Jenway Model 3520, Essex, UK). The viscosity of the formulations was carried out using a Brookefield viscometer (VT 181, Karlsruhe, Germany) at 27 ± 2 °C using spindle number seven and the rotational speed of 100 rpm. Spreading time was done by placing 0.5 g of each formulation on a previously cleaned slide and covered with another slide. Weight (1 kg) was placed on the covered slides for 5 min for even spread. The spreading time was determined by the length of time taken to separate the two slides. The diffusion profiles of the cream and ointment formulations were studied in agar using the method of Femi-Oyewo et al. (2013) and diffusion rates were obtained from the slope of the graphs of diffusion against time.
Dermal irritation test
The rabbit irritation test was carried out using established procedure (OECD 2002) Briefly, the right and left hind limbs of 16 male New Zealand rabbits (1400 ± 220 g) were clipped free of fur 24 h before the application of the formulations. The extract and selected formulations (500 mg) of P. amarus was applied to a site of approximately 25 mm2 and covered with a patch (semi-occlusive) using a non-occlusive bandage to wrap the test areas. After 24 h, the patch and test materials were removed and the sites were examined for skin irritation. The reactions were assessed using the scoring system and response categories according to OECD test guideline 404 (OECD 2002; Kamkaen et al. 2007). The score of primary irritation was then calculated for each rabbit.
Sub-chronic toxicity test
Six groups of five male Sprague–Dawley rats were clipped free of fur at the back and daily applications of 500 mg of the cream or ointment formulations was done on 4 cm2 area of the skin. The extract, base and selected formulations (containing 10 % extract and humectant or surfactant) were applied consistently for 21 days on the fur-free areas. After the experiments, the animals were humanely sacrificed and the skin was collected for histopathological analysis by fixing a portion of tissue in formalin diluted to 10 % with normal saline. Serial sections of 5 µm thickness were made after paraffin embedding and block making. The sections were stained with heamatoxylin and eosin, and then microscopically examined.
In vitro antimicrobial studies
The antimicrobial activities of P. amarus ethanol extract were determined using the agar well diffusion method (Collins et al. 1995). Four concentrations of the extract (12.5, 25.0, 50.0 and 100.0 mg/mL) were prepared using 20 % dimethylsulphoxide (Gaylord Chemical Corporation, USA) as the solvent. The cream and ointment formulations containing equivalent quantities of extract were diluted with DMSO as well. The antibacterial activity of the extract, cream and ointment on S. aureus and P. aeruginosa was done by seeding about 0.2 mL of each diluted culture of the test organisms into 20 mL of sterile nutrient agar (Difco Laboratories, USA). The agar was transferred into plates and allowed to set. Wells (6 mm in diameter), were bored on the agar plates with the aid of a sterile cork borer. About 0.5 mL of the cream or ointment was dispensed into each well and then allowed to stand for about 30 min for diffusion to occur. The plates were then incubated at 37 °C for 24 h. The zones of inhibition were measured (in mm) as the difference between cork borer (6 mm) and the diameters of inhibition (Junaid et al. 2006).
The antifungal activity of the extracts against Trychophyton rubrum and Candida albicans was done using sterilized Saburaud dextrose agar (SDA) as the growth media. The SDA (20 mL) was transferred into sterile petri-dish, allowed to set and about 0.2 mL of a 24 h old culture of the fungal isolates in nutrient broth were streaked unto the agar plates and then the extract, cream or ointment were transferred into the wells as previously described. The dishes were incubated at 27 °C for 48 h and the zones of inhibition were then measured (in mm).
Control experiments were set up as follows: Agar plate only; agar plates and extract only; agar plate and test organisms only; agar plate, test organisms and 20 % DMSO; agar plate, test organisms and 4 % glycerin only; agar plate, test organisms and 5 % cetomacrogol 1000 only. Ciprofloxacin (30 µg/mL), neomycin-bacitracin cream and mupirocin ointment were used as the positive control (standard) for bacteria; ketoconazole (100 µg/mL), ketoconazole cream and Whitfield ointment were used as the standard for dermatophytes.
In vivo antimicrobial studies of cream on infected Sprague–Dawley rats
Staphylococcus aureus was cultured for 24 h after which dilutions were made and the organism was plated on Mannitol Salt Agar (MSA, Biowark Lab. Pune, India) and incubated for 16 h to achieve a log-phase growth. The number of organisms was enumerated using a colony counter (Stuart Scientific Co. Ltd. U.K). Seven groups of Sprague–Dawley rats (five animals per group) weighing 220 ± 25 g were randomly assigned to groups. Groups 1 and 2 were treated with 5 and 10 % w/w P. amarus cream respectively, groups 3 and 4 received 5 and 10 % w/w P. amarus cream containing 4 % w/w glycerin respectively, group five received the cream base, group six utilized the standard antibacterial cream (neomycin–bacitracyn cream) and group seven was not treated.
The animals were anaesthetized with chloroform (Sigma Aldrich Chemical Company, St Loius, USA) inhalation and their backs (2 × 2 cm) were clipped free of fur. To each shaved area, 200 µL of a log-phase culture of 10−8 dilution of S. aureus was inoculated intradermally into the shaved area. Treatment commenced 24 h post infection by which time the lesions had been formed and the bacterial count per lesion were determined (Gisby and Bryant 2000). Cream formulations (500 mg) were applied to the lesions and a second dose was applied after 6 h and then twice daily for 3 days. The lesions were observed and noted at the start and end of therapy.
The animals were humanely sacrificed 16 h after cessation of treatment. The lesions and surrounding skin were excised and homogenized in 1 mL of bacteriological peptone (Lab M Ltd., Lancashire, UK) for 20 min (Griffin and George Ltd, London, UK). The resulting homogenates were serially diluted and 20 µL volumes of each dilution was cultured on mannitol salt agar, incubated for 24 h and the viable count of S. aureus was determined.
Statistical analysis
Statistical analysis to compare the antimicrobial properties of the formulations was done with Graph-Pad Prism InStat (Graphpad Software Inc., San Diego USA), using unpaired student’s t test, analysis of variance and Turkey Kramer’s multiple comparison tests. The null hypothesis in each test was that there were no significant differences between or within the treatments. Values of p < 0.05 (i.e. 95 % confidence interval) were considered significant.
Results
Physicochemical properties
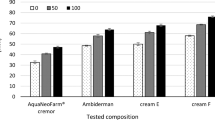
The physicochemical properties of P. amarus creams and ointments are presented in Table 2. The pH (3.61–6.04) of the cream and ointment formulations was in the acidic range. The pH and viscosity of the cream and ointment formulations reduced with increase in extract concentration with formulations having humectant or surfactant having lower viscosities. The spreading time for cream was lower than for ointment and diffusion rates of the cream were also higher than for the ointment. Figure 1 shows the diffusion profiles of the 10 % formulations, the diffusion of the formulations increased with time. The onset of diffusion for cream was faster than ointment and the presence of humectant or surfactant facilitated faster diffusion.
Safety profiles
The rabbit skin irritation tests showed that the irritation index in vivo ranged between 0.06 and 0.13 for creams and ointments. Formulations containing humectant or surfactant had lower indices of irritation. Generally, all the irritation indices for the extract, base, cream and ointment formulations were in the negligible category for primary irritation. Figure 2 shows the photomicrographs of the skin of animals subjected to sub-chronic toxicity test for 21 days. The skin sections of all the animals presented no visible lesions.
Antimicrobial properties
The results of the antimicrobial properties of P. amarus extract are presented in Table 3. The zones of inhibition of the various organisms increased significantly (p < 0.01) with increase in concentration of the extract. The antibacterial activity of the extract was significantly (p < 0.001) higher than the antifungal activity especially at low concentrations. However, there was no significant difference (p > 0.05) between the zones of inhibition for the bacteria (S. aureus and P. aeruginosa) and dermatophytes (C. albicans and Trychophyton rubrum). The in vitro antimicrobial properties of the formulations are presented in Table 4. The results showed that cream and ointment formulations containing 1.0 and 2.5 % w/w extract showed no antimicrobial effect except against P. aeruginosa. However, cream containing glycerin showed activity on S. aureus and T. rubrum at 1 % concentration while ointments containing surfactant exhibited activity on all organisms at 2.5 %. The antimicrobial properties generally increased with increase in concentration of the extracts with formulations containing humectant and surfactant exhibiting significantly higher (p < 0.05) antimicrobial properties. The formulations showed significantly (p < 0.001) larger zones of inhibition than the extract with the cream showing higher antimicrobial activity than the ointment. In addition, S. aureus was more susceptible to the extract and its formulations than the other organisms.
The results of the survival of S. aureus in Sprague–Dawley rats inoculated with clinical strains of S. aureus from skin infections are presented in Table 5. There was 100 % survival of the bacteria in the untreated animals while the animals treated with the base showed 90.6 % survival. Generally, the ranking of bacteria survival in the formulations was: 5 % P. amarus cream >5 % P. amarus cream + humectant >10 % P. amarus cream >10 % P. amarus cream + humectant. This shows that the survival of the organism decreased with increase in the concentration of the extract and with the addition of humectant.
Discussion
The pH of P. amarus cream and ointment was in the pH range of the skin. The stratum corneum is remarkably resistant to alterations in pH, tolerating a range of 3–9 (Isa et al. 2000). The absorption of creams into the skin through the stratum corneum has been shown to be affected by the pH-partition hypothesis. The ionized molecules have a much greater aqueous solubility than the unionized hence does not penetrate the lipid barrier like the former. This indicates that the cream and ointment formulations will be well tolerated on the skin and will not cause any form of irritation. Viscosity reflects the adherence property of creams when applied to the skin surface and high viscosity property helps prolong drug delivery at the application site (Adeyeye et al. 2002). Formulations containing humectants or surfactant had significantly lower (p < 0.05) viscosity than those without humectant. This indicates that humectant or surfactant reduced the viscosity of the formulations making it more fluid in consistency. Humectants are used to minimize water loss from semi-solid preparations to prevent dryness and improve the spreadability and general consistency of the product while surfactants serve as wetting agents that lower the surface tension of liquids and allowing for improved spreading characteristics. Femi-Oyewo et al. (2013) reported the improved penetration of sulphur ointments containing surfactant while humectants have also been shown to improve the effectiveness of certain herbal cream formulations (Fakeye et al. 2004).
The rabbit irritation tests have been used in previous studies to determine the irritant potential of chemicals (Hoffmann 2006). The formulations showed negligible primary irritation index in vivo and the sub-chronic toxicity tests showed no visible lesions on the animal skin indicating that the formulations are well tolerated in the animals. The biocompatibility of pharmaceutical and cosmetic products having natural compounds is evaluated by the irritation tests (OECD 2002; Kamkaen et al. 2007). The cream and ointment formulations of P. amarus can thus be regarded as safe for use.
The ethanol extract of P. amarus possess appreciable antimicrobial properties against gram-negative (P. aeruginosa) and gram-positive (S. aureus) bacteria, and the dermatophytes (C. albicans and Trychophyton rubrum). When the cream formulations containing humectant were compared with the extracts, the cream formulations showed significantly larger (p < 0.001) zones of inhibition than the plain extract. This indicates that the formulation of the extract into cream significantly (p < 0.001) increased the antimicrobial property of the extract. Thus, the cream formulation of the extract will be more effective for the treatment of skin infections than using the extract either for bathing or rubbing on the affected parts of the skin. The ointment formulations containing only the extract or with surfactant also showed significant antimicrobial activity compared to the extract though lower than the cream. The lower activity of the ointment compared to the cream may be due to the significantly higher (p < 0.01) viscosity which impeeded the diffusion rate. The diffusional speed of a molecule is affected by the state of matter, hence higher in gases and air than liquids and solids and this determines penetration (Barry 2001). Both formulations will be useful in the treatment of skin infections; while the cream will be useful for oozing wounds, the ointment will be applicable in chronic dry lesions.
There were significant differences (p < 0.05) in bacteria survival in untreated animals; those treated with the base and those treated using Phyllanthus amarus cream formulations. This implies that the cream was active and the activity was not dependent on the base. The in vivo activity of the cream was dependent on extract concentration in a similar manner to the in vitro action. This showed that the presence of formulation ingredients did not compromise the bioactivity of the phytoconstituents in the extract. In addition, formulation containing humectant yielded lower survival of the micro-organism compared to the one having no humectant. This showed that the humectant had a potentiating effect on the in vivo activity of the cream. Furthermore, the standard antibacterial agent gave a significantly (p < 0.05) lower survival than the formulations containing humectant. The reason could be because the standard agent is a compound comprising of two potent synthetic antimicrobial agents while the formulations contain a crude extract.
The study reported the successful design and formulation of the extract of Phyllanthus amarus into pharmaceutical dosage forms for topical application. The dosage forms provides a superior presentation for a plant extract that is normally used for bathing and rubbing into infected parts of the skin. The dosage forms have not reduced the biological activity of the extract showing that the formulation additives were compatible with the extract. Creams and ointments have adherent property that enables prolonged activity compared to when the extract is rubbed to the skin which may easily run off the skin surface. To enhance product elegance and presentation, humectants which conserves water was added to the cream while surfactant a penetration enhancer, was added to the ointment. Generally, this study is novel since it incorporates the formulation of an indigenous and culturally acceptable active plant extract into conventional dosage form.
Conclusion
The herbal cream and ointment of Phyllanthus amarus extract had acceptable physicochemical and safety profiles with significant in vitro antimicrobial activity. Furthermore, the in vivo activity of the cream on S. aureus showed increased antibacterial activity with increase in extract concentration and humectant presence. Thus, the cream and ointment formulations P. amarus extract could be useful in the treatment of skin infections instead of using the extract for bathing and rubbing.
References
Adegoke AA, Iberi PA, Akinpelu DA, Aiyegoro OA, Mboto CI (2010) Studies on phytochemical screening and antimicrobial potentials of Phyllanthus amarus against multiple antibiotic resistant bacteria. Int J Appl Res Nat Prod 3(3):6–12
Adeyeye MC, Jain AC, Ghorab M, Reilly WJ (2002) Viscoelastic evaluation of topical creams containing microcytalline cellulose/sodium carboxymethyl cellulose as stablizer. AAPS Pharm Sci Tech 3(2):16–25 (Article 8)
Ajala TO, Igwilo CI, Oreagba IA, Odeku OA (2011) The antiplasmodial effect of the extracts and formulated capsules of Phyllanthus amarus on Plasmodium yoelii infection in mice. Asian Pac J Trop Med 4(4):283–287
Akinjogunla OJ, Eghafona NO, Enabulele IO, Mboto CI, Ogbemudia FO (2010) Antibacterial activity of ethanolic extracts of Phyllanthus amarus against extended spectrum–lactamase producing Escherichia coli isolated from stool samples of HIV sero positive patients with or without diarrhea. Afr J Pharm Pharmacol 4(6):402–407
Ansel C, Allen LV, Popovich (2005) Disperse systems. In: Pharmaceutical dosage forms and drug delivery systems (8th edition). Lippincott Williams and Wilkins. Philadelphia, pp 387–389, 398
Barry BW (2001) Novel mechanisms and devices to enable successful transdermal drug delivery. Eur J Pharm Sci 14:101–114
Betageri G, Prabhu S (2002) Semi solid preparations. In: Swarbick J, Boylan JC (eds) Encylopedia of pharmaceutical technology, vol 3, 2nd edn. Marcel Dekker Inc, New York, pp 2436–2457
British Pharmaceutical Codex (1979) (11th Edition). The Pharmaceutical Press, London, p 55
Brown DJ, Dattner AM (1998) Phytotherapeutic approaches to common dermatologic conditions. Arch Dermatol 134:1401–1404
Buhse L, Kolinski R, Westenberger B, Wokovich A, Spencer J, Chen CW, Turujman S, Gautam-Basak M, Kang GK, Kibbe A, Heintzelman B, Wolfgang E (2005) Topical drug classification. Int J Pharm 295:101–112
Collins CH, Lynes PM, Grange JM (1995) Microbiological methods, 7th edn. Butter Worth-Heinemann Ltd, Oxford, pp 175–190
Eldeen IMS, Seow EM, Abdullah R, Sulaiman SF (2011) In vitro antibacterial, antioxidant, total phenolic contents and anti HIV-1 reverse transcriptase activities of extracts of seven Phyllanthus spp. South Afr J Bot 77(1):75–79
Fakeye TO, Itiola OA, George AO, Odelola HA (2004) Antimicrobial property of Picralima nitida stem bark extract in cream formulations. Pharm Biol 42(4–5):274–279
Faremi TY, Suru SM, Fafunso MA, Obioha UE (2008) Hepatoprotective potentials of Phyllanthus amarus against ethanol-induced oxidative stress in rats. Food Chem Toxicol 46:2658–2664
Femi-Oyewo MN, Ajala TO, Mabadeje A (2013) The evaluation of shea butter from Butyrospermum parkii as a vehicle in sulphur ointment formulations. West Afr J Pharm 24(2):58–65
Gisby J, Bryant E (2000) Efficacy of a new formulation of mupirocin: comparison with oral and topical agents in experimental skin infections. Antimicrob Agents Chemother 44(2):255–260
Grossblatt N (1978) Guide for the care and use of laboratory animals. National Academies Press. Issue 85, Part 23 DHEW, NIH Publications No. 80–23
Hoffmann RM (2006) The hair follicle and its stem cells as drug delivery targets. Expert Opin Drug Deliv 3(3):437–449
Idson B, Lazarus J (1991) Semisolids. In: Lachman L, Lieberman HA, Kanig JL (eds) The theory and practice of industrial pharmacy. Varghese Publishing House, Bombay, pp 534–563
Isa TS, Philippe B, Raymond H, Michel H, Jacques D (2000) Improved kinetic parameter estimation in pH-profile data treatment. Int J Pharm 198:38–49
Junaid SA, Olabode AO, Onwuliri FC, Okwori AEJ, Agina SE (2006) The antimicrobial properties of Ocimum gratissimum gastrointestinal isolates. Afr J Biotechnol 5(22):2315–2321
Kamkaen N, Phuntuwe W, Samee W, Boonrod A, Treesak C (2007) The investigation of the rabbit and human skin irritation of herbal anti-wrinkle cream. Thai Pharm Health Sci J 2(1):20–25
Martin A, Bustamante P, Chun AHC (2005) Physical pharmacy (4th Indian Edition). Lippincott Williams and Wilkins. B. I. Publication Pvt. Ltd. 500–501
Mazumder A, Mahato A, Mazumder R (2006) Antimicrobial potentiality of Phyllanthus amarus against drug resistant pathogens. Nat Prod Res 20(4):323–326
Moshi MJ, Lutale JK, Rimoy GH, Abbas ZG, Josiah RM, Swai ABM (2001) The effect of Phyllanthus amarus aqueous extract on blood glucose in non-insulin dependent diabetic patients. Phytother Res 15(7):577–580
Naaz F, Javed S, Abdin MZ (2007) Hepatoprotective effect of ethanolic extract of Phyllanthus amarus Schum and Thonn on aflatoxin B1-induced liver damage in mice. J Ethnopharmacol 113:503–509
Nebedum J, Ajeigbe K, Nwobodo E, Uba C, Adesanya O, Fadare O, Ofusori D (2009) Soap and ointment made from Cassia alata, Walnut-Juglan nigra, Ocimum basilicum and Aloe vera. J Med Plant 3:23–28
OECD guideline for the testing of chemicals. 2002. Test No. 404: Acute dermal irritation/corrosion. doi: 10.1787/9789264070622-en
Reuter J, Merfort I, Schempp CM (2010) Botanicals in dermatology: an evidence-based review. Am J Clin Dermatol 11(4):247–267
Xinhua WA (2001) Comparative study of Phyllanthus amarus compound and interferon in the treatment of chronic hepatitis B. Southeast Asian J Trop Med Public Health 32(1):140–142
Acknowledgments
This article does not contain any studies with human subjects performed by any of the authors and animal care use was conducted in accordance with appropriate guidelines as stated under methods section. In addition, all authors (Tolulope O. Ajala, Mbang N. Femi-Oyewo, Oluwatoyin A. Odeku, Oluwasanmi O. Aina, Adebowale B. Saba, Olayinka O. Oridupa) hereby declare that they is no conflict of interest. None of the authors received research grant from any agency for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ajala, T.O., Femi-Oyewo, M.N., Odeku, O.A. et al. The physicochemical, safety and antimicrobial properties of Phyllanthus amarus herbal cream and ointment. Journal of Pharmaceutical Investigation 46, 169–178 (2016). https://doi.org/10.1007/s40005-015-0226-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40005-015-0226-8