Abstract
Purpose
The length of neutropenia has a significant impact on the incidence of bloodstream infection (BSI) in cancer patients, but limited information is available about the pathogen distribution in late BSI.
Methods
Between 2002 and 2014, BSI episodes in patients with neutropenia receiving chemotherapy for hematologic malignancies were prospectively identified by multicenter, active surveillance in Germany, Switzerland and Austria. The incidence of first BSI episodes, their microbiology and time to BSI onset during the first episode of neutropenia of 15,988 patients are described.
Results
The incidence rate of BSI episodes was 14.7, 8.7, and 4.7 per 1000 patient-days in the first, second, and third week of neutropenia, respectively. BSI developed after a median of 5 days of neutropenia (interquartile range [IQR] 3–10 days). The medium duration of neutropenia to BSI onset was 4 days in Escherichia coli (IQR 3–7 days), Klebsiella spp. (2–8 days), and Staphylococcus aureus (3–6 days). In contrast, BSI due to Enterococcus faecium occurred after a median of 9 days (IQR 6–14 days; p < 0.001 vs. other BSI). Late onset of BSI (occurring after the first week of neutropenia) was also observed for Stenotrophomonas maltophilia (12 days, IQR 7–17 days; p < 0.001), and non-albicans Candida spp. (13 days, IQR 8–19 days; p < 0.001).
Conclusions
Over the course of neutropenia, the proportion of difficult to treat pathogens such as E. faecium, S. maltophilia, and Candida spp. increased. Among other factors, prior duration of neutropenia may help to guide empiric antimicrobial treatment in febrile neutropenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ten to 25% of neutropenic patients undergoing chemotherapy for acute leukemia or hematopoietic stem cell transplantation (HSCT) develop bloodstream infections (BSI) with crude mortality rates ranging from 11 to 36% [1,2,3,4]. The most frequent portal of entry for BSI in patients with neutropenia is mucosal barrier injury and central lines, with leading causes of BSI being coagulase-negative staphylococci (CoNS), Enterobacteriacea and non-fermenting Gram-negative rods [5]. Given the high case fatality rates, timely and adequate empiric antimicrobial therapy is warranted with current guidelines recommending a broad-spectrum beta-lactam with antipseudomonal activity, with or without an aminoglycoside [6, 7]. Hospital-, host- and treatment-related factors may influence the distribution of BSI pathogens during neutropenia. Such factors include the development of mucositis [8, 9], exposure to broad-spectrum antimicrobial agents [10], catheter dwell time [11], and transmission of nosocomial pathogens [12].
ONKO-KISS is an ongoing tri-national surveillance system for infections in neutropenic patients treated with induction or consolidation chemotherapy for hematologic malignancies [13,14,15]. Since 2002, primary BSI that occur in neutropenic patients receiving high-dose chemotherapy for autologous and allogeneic HSCT or for induction chemotherapy for acute leukemia, are captured prospectively by active surveillance in participating centers in Germany, Austria and Switzerland. In previous analyses of the ONKO-KISS surveillance cohort, we have described the overall characteristics of the cohort, the microbiology of BSI according to cancer treatment modalities with and without fluoroquiniolone prophylaxis, and an increase of Gram-negative BSI between 2002 and 2014 with the background of overall low rates of methicillin-resistant S. aureus, Vancomycin-resistant enterococci (VRE) and extended spectrum β-lactamase-(ESBL)-producing Enterobacteriaceae [14, 15]. In the current work, we examined changes in the incidence and distribution of BSI over the course of neutropenia in ONKO-KISS patients.
Methods
Study setting
Patients were recruited between January 2002 and December 2014 by active nosocomial infection surveillance in a median of 20 participating hematologic centers in Germany, Austria and Switzerland (ONKO-KISS) [13, 14]. ONKO-KISS surveillance includes neutropenic patients undergoing allogeneic or autologous HSCT and patients with acute leukemia receiving induction chemotherapy for hematologic malignancies [13]. Participating centers are required to treat a minimum of 20 patients with these conditions per year. The antimicrobial prophylaxis and antineoplastic treatment regimens are administered according to institutional protocols.
Data collection and definitions
The study protocol was approved by the institutional review board of the Freiburg University Medical Centre and informed consent was waived. All investigations have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
The methods for surveillance of nosocomial BSI in ONKO-KISS have been described in detail elsewhere [13, 14]. For the current study, all adult patients (aged ≥ 18 years) under surveillance who had the first episode of neutropenia were eligible for study inclusion.
Neutropenic patients were screened clinically by the treating physician on a daily basis and at least weekly for BSI by trained, dedicated staff using diagnostic criteria outlined by the Centers of Disease Control and Prevention (CDC) [16]. No surveillance blood cultures were drawn. Only primary BSI (including those originating from a central venous line or mucositis), occurring between the second day of neutropenia and 2 days following its resolution, were captured. BSI that were not considered primary were not documented by surveillance staff. Surveillance ended with the resolution of neutropenia or death, discharge or transfer to another hospital. In patients with neutropenia upon hospital admission, the day of admission was considered the first day of neutropenia. The following baseline variables were captured: demographic data, type of underlying malignancy and transplantation, chemotherapy cycle, fluoroquinolone prophylaxis (since 2009), number of previous neutropenia episodes, the beginning and end date of neutropenia, and the day of BSI onset. Information on antibiotic resistance was only available for vancomycin-resistance in Enterococcus spp., for Methicillin-resistant S. aureus, and for resistance to third-generation cephalosporins in Enterobacteriaceae (for infection surveillance purposes considered to be ESBL-positive, this information was available since 2010). Data are collected on a standardized report form and entered into a web-based database.
Neutropenia was defined either as an absolute white blood cell count of < 1000 × 109/l, as an absolute granulocyte count of < 500 × 109/l, or as an absolute granulocyte count of < 1000 × 109/l with an expected drop to < 500 × 109/l. The end of neutropenia was defined as a rise in white blood cells to > 1000 × 109/l for at least two consecutive days. BSI was defined according to CDC criteria either as growth of pathogenic bacteria from a single blood culture or as cultivation of skin commensals from a single blood culture (study period 2002–2010) or two independent blood culture sets (from 2011 onwards) in combination with patient symptoms of pyrexia ≥ 38.0 °C, shivering or hypotonia [17].
If a blood culture grew two different bacterial species and one isolate was a skin commensal, then only the pathogen that was not a skin commensal (according to CDC definitions) was included in the final analysis. The day of BSI onset was defined as the date on which the first positive blood culture was drawn. BSI occurring within the first 7 days of neutropenia were defined as early-onset BSI; BSI occurring after more than 7 days of neutropenia were defined as late-onset BSI. The duration of neutropenia was the sum of neutropenic days during the first episode of neutropenia. If a patient was neutropenic upon admission, the admission day was considered as the first day of neutropenia. Only the first BSI episodes were considered for analysis.
Statistical analysis
Differences in categorical variables were compared using the Chi-square test or Fisher’s exact test, as appropriate. Time periods of neutropenia to first BSI onset (consecutive neutropenia days) were expressed as median (interquartile range [IQR]) and were compared by use of the Kruskall–Wallis test or Dunnett’s multiple comparison test. All p values are two sided with a 0.05 level of significance. We managed and analyzed all data using of SPSS 21 software (SPSS; IBM, Chicago, IL).
Results
Study population and baseline characteristics
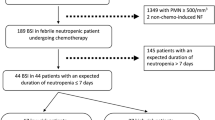
18,382 adult patients with neutropenia originating from a median of 20 participating hematology units (range 10–24) were eligible for study inclusion. A total of 15,988 patients were analyzed after excluding 476 patients with missing information on the chemotherapy cycle and 1918 patients not being in the first neutropenic phase. The baseline characteristics of the study population and information on antineoplastic treatments are summarized in Table 1 and the distribution of neutropenic days and BSI onset over time are described in Fig. 1. Overall, the median length of neutropenia was 11 days (IQR, 7–18 days) with a substantially longer duration in allogeneic HSCT patients (median 16 days; IQR 11–22 days) and in patients receiving induction chemotherapy without HSCT (median, 18 days, IQR 12–24 days) as compared to autologous HSCT recipients (median 7 days, IQR 6–9 days, p < 0.001).
Number of patients with neutropenia (black bars) or BSI (grey bars) and incidence rate of BSI per day of neutropenia (white bars): a total study cohort; b patients with allogeneic HSCT; c patients with autologous HSCT; d patients with acute leukemia treated with induction chemotherapy. BSI bloodstream infection, HSCT hematopoietic stem cell transplantation
Bloodstream infection during neutropenia
The crude incidence rate of a first BSI episode was 15.4 per 100 neutropenic patients. Overall, the median time period from the beginning of neutropenia to first BSI onset was 5 days (IQR 3–10 days; Figs. 1 , 2). The time was shortest for autologous HSCT recipients (3 days, IQR 2–5 days). It was 8 days (IQR 4–12 days) in allogeneic HSCT recipients, and 10 days (IQR 6–14 days) after induction chemotherapy in patients with acute leukemia.
Time from onset of neutropenia to BSI. a Time to BSI for first BSI episodes, b Time to BSI for all BSI episodes. Squares indicate the median, whiskers indicate the interquartile range. *p < 0.050, **p < 0.001 versus all other BSI (Kruskall-Wallis test with Dunn’s multiple comparisons test for comparison to all other BSI). BSI bloodstream infection, KES Klebsiella spp., Enterobacter spp. and Serratia spp.
A total of 1599 of the 2463 first BSI episodes (64.9%) occurred within the first week of neutropenia and were classified as early-onset BSI, while 864 (35.1%) BSI developed after the first week of neutropenia and were classified as late-onset BSI. The proportion of early-onset BSIs was higher for autologous HSCT recipients compared to allogeneic HSCT recipients and patients receiving induction chemotherapy without HSCT (853 [94.6%] versus 667 [49.7%] and 79 [35.9%], respectively). Patients who developed BSI late-onset BSI differed significantly from patients who with early-onset BSI in regards to gender, the modality of antineoplastic chemotherapy, underlying hematologic malignancy, duration of neutropenia, the proportion of patients admitted to the intensive care unit, and mortality during neutropenia (Table 1).
The incidence rate of first BSI episodes was 14.68 BSI per 1000 neutropenic days in the first week and declined with increasing duration of neutropenia to 8.71 in the second week and 4.73 in the third week (Fig. 1). In patients with autologous HSCT, the incidence rate of first BSI episodes was highest on the fourth day of neutropenia and declined rapidly thereafter. In contrast, BSI incidence rate decline was considerably slower in patients with allogeneic HSCT and patients with acute leukemia treated with induction chemotherapy (Fig. 1). Of note, the BSI incidence rate during the first week of neutropenia was higher in patients with autologous HSCT (19.77 per 1000 neutropenic days) compared to patients with allogeneic HSCT (11.77 per 1000 neutropenic days, p < 0.001) and patients receiving induction chemotherapy for acute leukemia (8.71, p < 0.001, Fig. 1b–d).
Distribution of BSI pathogens during neutropenia
BSI were more frequently caused by Gram-positive than Gram-negative bacteria (Table 2). Polymicrobial bacteremia was found in 80 patients (3.2%), and 67 patients (2.7%) had a fungemia. The most frequent Gram-positive isolates were CoNS and Enterococcus spp., while E. coli, Pseudomonas aeruginosa and Klebsiella spp. were the most frequent Gam-negative BSI isolates.
The median duration of neutropenia until onset of BSI was shorter for Gram-negative rods than for Gram-positive bacteria and fungi (Fig. 2). E. coli bacteremia developed a median 2 days earlier than other BSI, and E. faecium, S. maltophilia und non-albicans Candida spp. grew a median of 3, 6, and 7 days later, respectively (Fig. 2). No difference in the median duration of neutropenia until onset of BSI according to pathogen was found between first episodes compared to all episodes occurring during neutropenia (Fig. 2a , b).
The changes in the relative proportion of blood stream pathogens in early and late onset BSI are summarized in Fig. 3 and Table 2. Overall, the frequency of ESBL-producing Enterobacteriacea was comparably low in both early-onset BSI (50 episodes, 3.1% of early-onset BSI) and late-onset BSI (19 episodes, 2%). Similar results were found in analyses stratified by autologous and allogeneic HSCT (Online resource 1).
Discussion
In this large cohort study of patients receiving antineoplastic treatment for hematologic malignancies, we observed substantial changes in the spectrum of pathogen over the duration of neutropenia. While E. coli and CoNS were the predominant pathogen in the first week of neutropenia, a higher proportion of more difficult-to-treat organisms such as E. faecium, S. maltophilia and non-albicans Candida occurred thereafter. The most pronounced relative reduction over time was observed for E. coli as a BSI pathogen, which continuously decreased over the first 2 weeks of neutropenia. In contrast, the proportion of BSI caused by enterococci and Candida spp. increased in proportion over this time period. Of note, E. faecium BSI, which are most often resistant to beta-lactams used in the empiric therapy of febrile neutropenia, occurred later than BSI by E. faecalis, which in Germany—the country that contributes most ONKO-KISS surveillance sites—is almost universally sensitive to aminopenicillins [18]. Interestingly, the proportion of BSI caused by P. aeruginosa did not change significantly over the first 3 weeks of neutropenia.
Previously, we have have reported a higher incidence of BSI during neutropenia in patients after allogeneic hematopoetic stem cell transplantation compared to patients after autologous HSCT [14, 19]. Although during day 5 to 9 of neutropenia the cumulative incidence of BSI was in fact lower in allogeneic HSCT patients, a longer duration of neutropenia (16 days in allogeneic HSCT versus 6 days in autologous HSCT), led eventually to higher BSI incidence in this group [20].
Most factors that influence the risk for BSI in cancer patients, such as exposure to antimicrobials, a low granulocyte count, mucosal damage and the presence of central venous catheters are time-dependent. Probably the most important time-dependent variable influencing the incidence and microbiology of BSI in neutropenic patients is the exposure to therapeutic antimicrobials. Over 80% of patients with hematologic malignancies develop fever after chemotherapy and given the high mortality of BSI in neutropenic patients, prompt empirical antibiotic therapy is mandatory [7]. The proportion of BSI that likely represent breakthrough infections after initiation of empiric broad-spectrum antibiotic therapy, therefore, increases over the course of neutropenia. The presumably increasing exposure to therapeutic antimicrobials over time most likely also explains why the incidence rate of BSI in neutropenia in our cohort continuously decreases after the fourth day of neutropenia. In addition, the onset and severity of mucositis during myeloablative regimens for HSCT peaks in the first week after start of the conditioning, and strongly correlates with the risk for BSI [21].
Recent studies have highlighted the profound changes of the gut microbiome under antimicrobial exposure [10, 22, 23]. For example, a strongly reduced diversity of the gut microbiome and overgrowth by enterococci, streptococci, Enterobacteriacea associated with antibiotic treatment has been described in allogeneic HSCT patients [10] and intestinal colonization with overgrowth flora was a risk factor for subsequent BSI caused by the same strain in HSCT patients [22, 24]. In a study by Satlin et al., 101 of a total of 159 BSI in HSCT recipients occurred before the administration of antibiotics with K. pneumoniae, E. coli, viridans streptococci and P. aeruginosa being the most frequent isolates [25]. In contrast, 31 of 58 breakthrough-BSI under treatment with either piperacillin-tazobactam or meropenem were caused by VRE and the median time from transplantation until the first BSI by VRE was 18 days compared to 9 days for all BSI. Other investigators have also reported that the previous use of carbapenems and prolonged neutropenia are strong risk factors for BSI caused by vancomycin-sensitive and vancomycin-resistant E. faecium in cancer patients [26, 27]. In a retrospective analysis of 120 BSI during the pre-engraftment phase in allogeneic HSCT recipients from a Swedish cancer center, the median time to BSI was 4 days for viridans streptococci, 8 days for E. coli and 11 days for Enterococcus spp. [28]. In a small retrospective study, all BSI by S. maltophilia in HSCT recipients occurred later than 3 weeks after transplantation [29]. In a retrospective study by Marr et al. blood cultures of 30 patients with bone marrow transplantation became positive after a median of 28 days after transplantation [30]. Furthermore, prophylaxis by fluconazole or other azole antifungals have been shown to select for a gastrointestinal colonization by non-albicans Candida species [31] and a recent study reported that the majority of Candida BSI in patients hospitalized for hematologic malignancies were caused by non-albicans species [32].
Our study has several limitations. Because it was primarily designed as a surveillance program, several variables that impact the risk for BSI were not recorded. These include the timing and type of therapeutic antimicrobials, the type of antineoplastic therapy or induction regimens, or the presence and severity of mucositis, severity of neutropenia, presence of lymphopenia, and therapeutic immunosuppressive medication. For other variables, the sample size was too small to allow for stratification, such type or source of hematopoetic stems cell used for transplatation. As shown in Table 1, the time of onset of BSI during neutropenia correlated with the type of underlying malignancy and antineoplastic treatment, and, therefore, the patterns and timing of BSI may be primarily associated with cancer treatment type rather than with neutropenia duration. However, we observed similar trends in BSI distribution over time in an exploratory analysis stratified by HSCT method. Further exploratory analyses showed no relevant change in the timing of BSI during neutropenia over the study period of ONKO-KISS (data not shown). Also, our analysis may reflect the pragmatic considerations of clinicians assessing the pre-test probability for a positive blood culture result in an individual patient that may differ greatly over the course of neutropenia and which is perhaps different across participating centers. Taken together, we, therefore, did not intend to infer causality between the timing of BSI onset and respective distribution of pathogens, as a multitude of known and unknown factors and interventions may contribute to the onset of BSIs caused by specific pathogens and as the timing of BSIs can be considered as a predictor but not a causal factor. The strength of our study was that patients were prospectively identified by active surveillance from 20 study sites in three European countries using standardized surveillance definitions. In contrast, most previous studies were retrospective, single center, and had a relatively small sample size.
In summary, our study results based on a multicenter cohort of neutropenic patients demonstrates an increasing proportion of difficult to treat pathogens such as E. faecium, S. maltophilia, and Candida spp. in neutropenic patients with late-onset BSI. At least partly, these changes in BSI pathogens can be explained by different lengths of at-risk periods for colonization and infection by nosocomial pathogens. Even though most clinicians would expect such a change in pathogen distributions during neutropenia, this has so far not been confirmed in a large cohort study. Together with various other clinical and hospital-specific factors, this information may support empiric antimicrobial treatment decisions in patients with febrile neutropenia.
References
Mikulska M, Del Bono V, Raiola AM, Bruno B, Gualandi F, Occhini D, et al. Blood stream infections in allogeneic hematopoietic stem cell transplant recipients: reemergence of Gram-negative rods and increasing antibiotic resistance. Biol Blood Marrow Transpl. 2009;15:47–53. https://doi.org/10.1016/j.bbmt.2008.10.024.
Almyroudis NG, Fuller A, Jakubowski A, Sepkowitz K, Jaffe D, Small TN, et al. Pre- and post-engraftment bloodstream infection rates and associated mortality in allogeneic hematopoietic stem cell transplant recipients. Transpl Infect Dis. 2005;7:11–7. https://doi.org/10.1111/j.1399-3062.2005.00088.x.
Marin M, Gudiol C, Ardanuy C, Garcia-Vidal C, Jimenez L, Domingo-Domenech E, et al. Factors influencing mortality in neutropenic patients with haematologic malignancies or solid tumours with bloodstream infection. Clin Microbiol Infect. 2015;21:583–90. https://doi.org/10.1016/j.cmi.2015.01.029.
Wisplinghoff H, Seifert H, Wenzel RP, Edmond MB. Current trends in the epidemiology of nosocomial bloodstream infections in patients with hematological malignancies and solid neoplasms in hospitals in the United States. Clin Infect Dis. 2003;36:1103–10. https://doi.org/10.1086/374339.
Mikulska M, Viscoli C, Orasch C, Livermore DM, Averbuch D, Cordonnier C, et al. Aetiology and resistance in bacteraemias among adult and paediatric haematology and cancer patients. J Infect. 2014;68:321–31. https://doi.org/10.1016/j.jinf.2013.12.006.
Averbuch D, Orasch C, Cordonnier C, Livermore DM, Mikulska M, Viscoli C, et al. European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European Conference on Infections in Leukemia. Haematologica. 2013;98:1826–35. https://doi.org/10.3324/haematol.2013.091025.
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52:427–31. https://doi.org/10.1093/cid/ciq147.
Safdar A, Armstrong D. Infections in patients with hematologic neoplasms and hematopoietic stem cell transplantation: neutropenia, humoral, and splenic defects. Clin Infect Dis. 2011;53:798–806. https://doi.org/10.1093/cid/cir492.
Gustinetti G, Mikulska M. Bloodstream infections in neutropenic cancer patients: a practical update. Virulence. 2016;7:280–97. https://doi.org/10.1080/21505594.2016.1156821.
Taur Y, Xavier JB, Lipuma L, Ubeda C, Goldberg J, Gobourne A, et al. Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin Infect Dis. 2012;55:905–14. https://doi.org/10.1093/cid/cis580.
Safdar N, Kluger DM, Maki DG. A review of risk factors for catheter-related bloodstream infection caused by percutaneously inserted, noncuffed central venous catheters: implications for preventive strategies. Medicine (Baltimore). 2002;81:466–79.
Rosa RG, Goldani LZ, dos Santos RP. Risk factors for multidrug-resistant bacteremia in hospitalized cancer patients with febrile neutropenia: a cohort study. Am J Infect Control. 2014;42:74–6. https://doi.org/10.1016/j.ajic.2013.06.025.
Dettenkofer M, Wenzler-Rottele S, Babikir R, Bertz H, Ebner W, Meyer E, et al. Surveillance of nosocomial sepsis and pneumonia in patients with a bone marrow or peripheral blood stem cell transplant: a multicenter project. Clin Infect Dis. 2005;40:926–31. https://doi.org/10.1086/428046.
Weisser M, Theilacker C, Tschudin Sutter S, Babikir R, Bertz H, Gotting T, et al. Secular trends of bloodstream infections during neutropenia in 15 181 haematopoietic stem cell transplants: 13-year results from a European multicentre surveillance study (ONKO-KISS). Clin Microbiol Infect. 2017;23:854–9. https://doi.org/10.1016/j.cmi.2017.03.020.
Kern WV, Weber S, Dettenkofer M, Kaier K, Bertz H, Behnke M, et al. Impact of fluoroquinolone prophylaxis during neutropenia on bloodstream infection: Data from a surveillance program in 8755 patients receiving high-dose chemotherapy for haematologic malignancies between 2009 and 2014. J Infect. 2018;77:68–74. https://doi.org/10.1016/j.jinf.2018.05.004.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32. https://doi.org/10.1016/j.ajic.2008.03.002.
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128–40.
European Centre for Disease Prevention and Control. Surveillance of antimicrobial resistance in Europe 2016. Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). Stockholm: ECDC; 2017. https://ecdc.europa.eu/en/publications-data/antimicrobial-resistance-surveillance-europe-2016. Accessed 26 May 2017.
Meyer E, Beyersmann J, Bertz H, Wenzler-Rottele S, Babikir R, Schumacher M, et al. Risk factor analysis of blood stream infection and pneumonia in neutropenic patients after peripheral blood stem-cell transplantation. Bone Marrow Transpl. 2007;39:173–8. https://doi.org/10.1038/sj.bmt.1705561.
Hieke S, Bertz H, Dettenkofer M, Schumacher M, Beyersmann J. Initially fewer bloodstream infections for allogeneic vs. autologous stem-cell transplants in neutropenic patients. Epidemiol Infect. 2013;41:158–64. https://doi.org/10.1017/s0950268812000283.
Herbers AH, de Haan AF, van der Velden WJ, Donnelly JP, Blijlevens NM. Mucositis not neutropenia determines bacteremia among hematopoietic stem cell transplant recipients. Transpl Infect Dis. 2014;16:279–85. https://doi.org/10.1111/tid.12195.
Ubeda C, Taur Y, Jenq RR, Equinda MJ, Son T, Samstein M, et al. Vancomycin-resistant Enterococcus domination of intestinal microbiota is enabled by antibiotic treatment in mice and precedes bloodstream invasion in humans. J Clin Invest. 2010;120:4332–41. https://doi.org/10.1172/JCI43918.
Fan D, Coughlin LA, Neubauer MM, Kim J, Kim MS, Zhan X, et al. Activation of HIF-1alpha and LL-37 by commensal bacteria inhibits Candida albicans colonization. Nat Med. 2015;21:808–14. https://doi.org/10.1038/nm.3871.
Kamboj M, Chung D, Seo SK, Pamer EG, Sepkowitz KA, Jakubowski AA, et al. The changing epidemiology of vancomycin-resistant Enterococcus (VRE) bacteremia in allogeneic hematopoietic stem cell transplant (HSCT) recipients. Biol Blood Marrow Transpl. 2010;16:1576–81. https://doi.org/10.1016/j.bbmt.2010.05.008.
Satlin MJ, Soave R, Racanelli AC, Shore TB, van Besien K, Jenkins SG, et al. The emergence of vancomycin-resistant enterococcal bacteremia in hematopoietic stem cell transplant recipients. Leuk Lymphoma. 2014;55:2858–65. https://doi.org/10.3109/10428194.2014.896007.
Kang Y, Vicente M, Parsad S, Brielmeier B, Pisano J, Landon E, et al. Evaluation of risk factors for vancomycin-resistant Enterococcus bacteremia among previously colonized hematopoietic stem cell transplant patients. Transpl Infect Dis. 2013;15:466–73. https://doi.org/10.1111/tid.12120.
Gudiol C, Ayats J, Camoez M, Dominguez MA, Garcia-Vidal C, Bodro M, et al. Increase in bloodstream infection due to vancomycin-susceptible Enterococcus faecium in cancer patients: risk factors, molecular epidemiology and outcomes. PLoS One. 2013;8:e74734. https://doi.org/10.1371/journal.pone.0074734.
Blennow O, Ljungman P, Sparrelid E, Mattsson J, Remberger M. Incidence, risk factors, and outcome of bloodstream infections during the pre-engraftment phase in 521 allogeneic hematopoietic stem cell transplantations. Transpl Infect Dis. 2014;16:106–14. https://doi.org/10.1111/tid.12175.
Yeshurun M, Gafter-Gvili A, Thaler M, Keller N, Nagler A, Shimoni A. Clinical characteristics of Stenotrophomonas maltophilia infection in hematopoietic stem cell transplantation recipients: a single center experience. Infection. 2010;38:211–5. https://doi.org/10.1007/s15010-010-0023-2.
Marr KA, Seidel K, White TC, Bowden RA. Candidemia in allogeneic blood and marrow transplant recipients: evolution of risk factors after the adoption of prophylactic fluconazole. J Infect Dis. 2000;181:309–16. https://doi.org/10.1086/315193.
Mann PA, McNicholas PM, Chau AS, Patel R, Mendrick C, Ullmann AJ, et al. Impact of antifungal prophylaxis on colonization and azole susceptibility of Candida species. Antimicrob Agents Chemother. 2009;53:5026–34. https://doi.org/10.1128/AAC.01031-09.
Gamaletsou MN, Walsh TJ, Zaoutis T, Pagoni M, Kotsopoulou M, Voulgarelis M, et al. A prospective, cohort, multicentre study of candidaemia in hospitalized adult patients with haematological malignancies. Clin Microbiol Infect. 2014;20:O50–7. https://doi.org/10.1111/1469-0691.12312.
Acknowledgements
We would like to thank Dr. Maja Weisser and Dr. Nina Khanna for their help in infection documentation and data analysis. We also would like to thank Regina Babikir, Winfried Ebner for their support in managing the study and data collection. In addition, we would like to thank the medical staff and study nurses at all the participating centers for the invaluable support they provided to the studies over the years. This study has been presented in part at the 26th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) in Amsterdam, the Netherlands.The study was supported in part with funds from the German Federal Ministry of Health.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Widmer, A.F., Kern, W.V., Roth, J.A. et al. Early versus late onset bloodstream infection during neutropenia after high-dose chemotherapy for hematologic malignancy. Infection 47, 837–845 (2019). https://doi.org/10.1007/s15010-019-01327-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-019-01327-0