Abstract
Purpose
Diagnosis of tuberculous uveitis (TBU) is often challenging and is usually made after excluding other causes of uveitis. We analysed the characteristics of TBU and variables associated with visual outcome.
Methods
A retrospective, observational analysis was performed in patients with presumptive TBU who were started on specific TB treatment between January 2006 and June 2016. Demographic, clinical, radiological, analytical and ophthalmic examination variables were studied. After completing TB treatment, a follow-up of at least 9 months was performed. A univariate and logistic regression analysis was applied to identify the variables associated with visual acuity and recurrences of uveitis.
Results
Forty affected eyes of 24 individuals were identified; 79% of patients were diagnosed during the last 3 years of the study period. Median delay from onset of symptoms to diagnosis was 12 weeks. Loss of visual acuity was the most frequent symptom (87.5%). Posterior uveitis was the most frequent localization (72.9%); 19 patients (79.2%) presented at least one of the Gupta signs predictive of TBU, but there were no confirmed diagnoses.
Outcome
There was improvement in visual acuity in 74.4% of the eyes, but a complete response was achieved only in 56.4%. There was recurrence in two patients. The initiation of treatment ≥ 24 weeks after onset of symptoms was significantly associated with no improvement (p = 0.026).
Conclusion
TBU can cause permanent damage to visual acuity, particularly in patients with delayed diagnosis. A prompt initiation of systemic TB treatment is essential to improve visual prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculous uveitis (TBU) is a form of extrapulmonary tuberculosis (TB) of growing interest in recent years. Its pathogenesis presents particular features that contrast with other forms of TB such as the decisive involvement of an immune response in clinical presentation and the difficulty, or even impossibility of demonstrating M. tuberculosis in ocular tissues [1]. Therefore, TBU is a diagnostic challenge to both ophthalmologists and infectious diseases specialists, and even for those experienced in TB diagnosis and treatment [2, 3]. The decision to initiate TB treatment is usually empiric, based on a combination of suggestive ocular signs associated with clinical, analytical and radiological findings [4, 5]. Despite growing interest, there are few TBU studies carried out in countries with low and moderate prevalence of TB.
The purpose of this study is to determine the characteristics associated with diagnosis, evolution and response to treatment of presumptive TBU patients referred from the ophthalmology’s uveitis unit to the TB specialist unit in our centre.
Materials and methods
Patients
An observational, descriptive cohort study was carried out on patients with presumptive TBU diagnosis. They were referred from the Ophthalmology department, between January 2006 and June 2016, to the TB specialist unit for establishing TB treatment. A chart review was performed and information on demographic data, clinical findings, blood and serum analysis, radiologic findings, tuberculin skin test (TST) and/or interferon-gamma release assays (IGRA) was collected. All patients were treated with at least 3 drugs and were jointly monitored by an ophthalmologist expert in uveitis and an experienced clinician in TB. Patients were monitored for at least 9 months after completing anti-tuberculosis treatment, with special focus on visual symptom changes, residual inflammatory signs and recurrences.
Other possible causes of uveitis were ruled out in all patients based on ocular findings, negativity of autoimmune tests (rheumatoid factor, antinuclear antibodies), serologies (toxoplasmosis, syphilis, B. henselae among others), angiotensin-converting enzyme and absence of other possible uveitis aetiologies. In pursuit of efficiency, ancillary tests were performed according to clinical findings, instead of performing the same battery of tests to each patient. Fluorescein angiographies were not performed routinely.
Definitions
In order to evaluate treatment response, the “best corrected visual acuity” in each affected eye was compared at diagnosis, upon completion of TB treatment, and after the follow-up period [6]. SUN (Standard Uveitis Nomenclature) classification was used to quantify inflammatory activity in patients with anterior or intermediate uveitis (ranging from 0 to 4, where 0 stands for absence of inflammation and 4 is the maximum grade) [7]. Classification of TBU was based on the Gupta revised criteria. According to these criteria, patients can be considered as confirmed TBU (patients with microbiological confirmation of M. tuberculosis in an ocular specimen), probable TBU (presence of compatible ocular findings, evidence of extraocular TB and a positive TST/IGRA) or possible TBU (presence of compatible ocular findings and a positive TST/IGRA, without extraocular TB evidence) [8].
Treatment response was classified into three groups [9]:
-
Complete response: complete visual acuity resolution, absence of inflammatory signs and recurrences during follow-up.
-
Partial response: partial visual acuity improvement, and absence of inflammatory signs or recurrences during follow-up.
-
Treatment failure: any of these scenarios: absence of visual acuity improvement, persistence of ocular inflammatory signs or recurrence after having completed TB treatment.
Statistical analysis
The Statistical Package for Social Sciences (v19, IBM SPSS Incl, Chicago, IL, USA) was used. Qualitative variables are presented in absolute numbers and percentages. Continuous variables are presented as mean and standard deviation (SD) or median and interquartile range. Student’s t test or Mann–Whitney test was used to study quantitative variables associated with visual prognosis, while the Chi square or Fisher’s exact test was used for qualitative variables. A value of p < 0.05 was considered to be statistically significant. Binary logistic regression multivariate analysis for treatment response was performed on variables that were statistically significant or with p ≤ 0.10 and clinically relevant in prior univariate analysis.
Ethical considerations
An Institutional Review Board approval was obtained from the Comité Ético de Investigación Galicia Sur (registration code: 2017/007).
Results
Initially, 29 patients were recruited, of whom 5 were excluded from further analysis: 3 due to incomplete clinical records and 2 due to another aetiology for uveitis being finally considered. Therefore, 24 patients with 40 affected eyes (16 patients with bilateral disease) were enrolled in the study. Each patient had a positive TST (induration ≥ 10 mm) and/or positive IGRA (Quantiferon®-TB Gold in-Tube, Cellestis Ltd). There was no patient with compatible ocular findings of TBU with a negative TST/IGRA and a documented exposure to a TB patient; 79% of patients were diagnosed in the last 3 years of the study period (January 2013 to June 2016).
All patients were of Spanish origin; 62% were males. Mean age was 48.3 ± 10.6 years. Serology for human immunodeficiency virus was negative in all patients. Only one patient had leucocytosis at the time of diagnosis and 82.6% of patients had normal erythrocyte sedimentation rate (ESR < 25 mm/h). Other clinical features are shown in Table 1.
Chest radiography was normal in 20 patients (83.3%); 2 had suggestive old scar healing TB findings, while 2 others showed signs of active extraocular TB (one pulmonary TB and the other pleural TB).
Aqueous humour mycobacterial culture and polymerase chain reaction (PCR) were done in two patients, with negative results. Extraocular microbiologically confirmed TB was present in only one patient with pulmonary TB. Another patient received a pleural TB diagnosis, but without microbiological confirmation. Therefore, not a single patient had confirmed TBU; 2 patients had probable TBU, and the other 22 (91.7%) had possible TBU.
The most frequent uveitis presenting symptom, affecting 87.5% of patients, was loss of visual acuity, followed by painful red-eye in 25% of patients and myodesopsias in 20.8%. Posterior uveitis was the most frequent location (72.9% of eyes) followed by intermediate (37.5%) and anterior (31.2%) uveitis. 19 eyes were affected in ≥ 2 locations. 19 patients (79.2%) presented at least 1 of the 3 predictive signs of TBU according to the Gupta criteria (posterior synechiae, retinal vasculitis or serpiginous choroiditis) [10], retinal vasculitis being the most frequent of the three (50% of patients, Fig. 1). Median duration from the onset of symptoms to anti-tuberculosis treatment initiation was 12 weeks (interquartile range 3–28 weeks).
Retinal vasculitis at presentation and after anti-tuberculosis treatment. Patient with active retinal vasculitis, with periphlebitis, retinal haemorrhagies and vascular occlusion (a, b). After completing anti-tuberculosis treatment, inflammatory signs were absent. The patient developed an epiretinal membrane (c) and peripheral affected vessels showed cicatrisation (d)
All patients were started on anti-tuberculosis treatment with three or four drugs, and 41.7% of patients were given oral corticosteroids. One patient failed to complete treatment (although he came for follow-up controls), while another was lost to follow-up after the end of treatment.
Follow-up: 23 patients were followed up for a median of 41 months (range 9–124). The SUN value fell to 0 (absence of inflammatory signs) in all patients with anterior or intermediate uveitis. All choroiditis cases showed cicatrisation of lesions. All of them were in remission at the end of the follow-up period (at least 9 months without activity after completing treatment), except for two patients who had a recurrence with a new episode of uveitis after completing anti-tuberculosis therapy.
Visual acuity improvement and absence of recurrence was achieved in 65.2% of patients, even though only 39.1% achieved complete resolution (20/20 best-corrected visual acuity in both eyes).
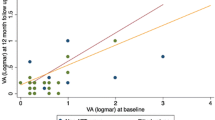
A partial or complete response was observed in 74.4% of the affected eyes, with complete visual acuity recovery in 56.4% (Fig. 2).
In the analysis of patients, treatment failure (recurrence or absence of any visual acuity improvement in at least one eye) was associated with poor visual acuity at the time of diagnosis (0.28 vs 0.57; difference of means 0.29; IC95% = 0.23–0.55). Absence of complete response was also associated with symptoms lasting more than 12 weeks prior to starting anti-tuberculosis treatment.
In the analysis of affected eyes, treatment failure was associated with symptoms lasting more than 24 weeks prior to start of treatment (p = 0.017). Absence of complete response was related to duration of symptoms prior to start of therapy (p = 0.004), serpiginous choroiditis (p = 0.048) and visual acuity loss in the affected eye (p = 0.026).
Discussion
The characteristics and evolution of a cohort of presumptive TBU patients were analysed. Clinical aspects, ocular findings and evolution of patients share common features with other series described in low or intermediate TB prevalence settings. Predominance of posterior uveitis, relatively young age of patients, slightly higher percentage of male, bilateral disease or uveitis in two or more locations in nearly half the affected eyes are common features in other series [11,12,13,14]. Recovery of symptoms (mainly visual acuity) or parameters of ocular inflammation also present partial or complete response values similar to those presented by other authors [15].
This study collected clinical parameters that are not usually analysed in other series that are directed to an ophthalmologic target audience. This is essentially to highlight the absence of systemic inflammatory markers such as normal leucocyte count in the vast majority of patients and normal ESR values.
The three main findings of this study are: (a) the lack of TB diagnosis confirmation in all our patients, (b) the importance of early diagnosis and early treatment for visual prognosis, and (c) the increasing number of TBU cases diagnosed in recent years.
Demonstration of M. tuberculosis in TBU has been observed to be null or very low in prior series [16,17,18]. Microbiological diagnosis is tricky because ocular damage is caused by immune reaction in a high number of cases. However, in other cases M. tuberculosis was detected in intraocular fluids, usually with a low bacillary load. Moreover, vitreous or anterior chamber puncture is not free of risks [19] and sensitivity of microbiological tests is low with conventional methods [16]. It is therefore a non-suitable technique for everyday practice. The use of primers, other than those commercially available to amplify nucleic acids of M. tuberculosis, have shown promising results, but unfortunately have not been validated in clinical practice [20]. In our cohort, anterior chamber samples were obtained in two patients, and both PCR and culture were negative. Altogether, no patient had a confirmed diagnosis; just two were probable TBU cases, while the other 22 patients were possible TBU cases. The number of patients with probable TBU in our study is lower than in other studies. This may be due to (a) lower prevalence of TB in Spain than in other countries where these studies were conducted [16] and (b) the fact that all our patients were referred from the Ophthalmology Department. Other authors have analysed the prevalence of TBU in patients with extraocular TB diagnosis, and logically the percentage of patients with probable TBU is higher, even in patients without ocular symptoms [17, 21].
The most relevant finding of this study is the importance of a prompt diagnosis and treatment. Even though the need for specific TB medication therapy has been questioned [22], and despite isoniazid monotherapy being a standard practice in the past [23], starting of TB specific therapy in patients with active TBU has provided good results with regard to prognosis and absence of recurrences [9, 18, 24]. Although randomized clinical trials comparing prognosis of treated vs untreated patients are missing, there is nowadays a general consensus on its appropriate indication [1, 15].
The direct relationship between prognosis and early treatment found in our study reinforces the need for specific TB therapy in presumptive TBU [25]. Patients in our clinic are normally prescribed a standard 6-month treatment in accordance with Spanish national guidelines [26]. Some authors propose extending the length of treatment to more than 6 months, based on indirect data that suggest lower recurrence rates [1, 11, 18, 27, 28]. Nevertheless, the results obtained in the present study indicate that a conventional 6-month therapy is probably adequate in patients with correct adherence to the treatment.
Remarkably, almost 80% of the cases were diagnosed in the last 3 years of the study. Until the 1960s, TB was the main cause of uveitis in developed countries. The efficacy of TB control programmes in the following decades led to a dramatic decrease of incidence and a progressive oblivion of TB, especially for physicians unrelated to infectious diseases or respiratory departments. However, in recent years, the description of highly specific ocular findings [10] and acknowledgement of the efficacy of systemic anti-tuberculosis therapy [5, 24], has contributed to greater awareness of TB among ophthalmologist, as is the case in our study and other studies in similar settings [13, 29].
Our study has some limitations that warrant further consideration. Firstly, we have analysed a relatively small number of geographically limited patients and hence conclusions might not be widely applicable to other populations. Secondly, despite positive TST or IGRAs in all patients, over-diagnosis cannot be ruled out, since no patient had confirmed TBU and only two cases were considered to have probable TBU. Positive TST or IGRA results are only suggestive of M. tuberculosis infection, and are never a definitive diagnosis test, meaning that in theory, some patients could have uveitis of another etiology [14, 16, 30]. Moreover, systemic corticosteroids associated with anti-tuberculosis therapy might initially contribute to decrease inflammatory signs and add confusion to diagnosis, because a positive clinical response could be attributed to TB medication rather than to the corticosteroids [31]. Nevertheless, we consider this to be unlikely, since other aetiologies of uveitis were thoroughly ruled out, statistical analysis did not relate corticosteroids to visual prognosis and in those cases that had early improvement related to anti-inflammatory effect of corticoids, this would have been only transitory and recurrences during follow-up would have been detected [28].
To conclude, TBU is a disease of uncertain diagnosis that requires early treatment in order to improve visual prognosis.
References
Cordero-Coma M, Salazar R, Costales F. Tuberculous uveitis: an update. Expert Rev Ophthalmol. 2014;9:125–37. https://doi.org/10.1586/17469899.2014.897228.
Lee C, Agrawal R, Pavesio C. Ocular tuberculosis. A clinical conundrum. Ocul Immunol Inflamm. 2016;24:237–42. https://doi.org/10.3109/09273948.2014.985387.
Lou SM, Larkin KL, Winthrop K, Rosenbaum JT, Group USS. Lack of consensus in the diagnosis and treatment for ocular tuberculosis among uveitis specialists. Ocul Immunol Inflamm. 2015;23:25–31. https://doi.org/10.3109/09273948.2014.926936.
Alvarez GG, Roth VR, Hodge W. Ocular tuberculosis: diagnostic and treatment challenges. Int J Infect Dis. 2009;13:432–5. https://doi.org/10.1016/j.ijid.2008.09.018.
Ang M, Chee SP. Controversies in ocular tuberculosis. Br J Ophthalmol. 2017;101:6–9. https://doi.org/10.1136/bjophthalmol-2016-309531.
Levenson JH, Kozarsky K. Visual Acuity. In: Walker HK, Hall WD, Hurst JW, editors. Clinical methods: the history, physical, and laboratory examinations. 3rd ed. Boston: Butterworths; 1990, pp. 563–4.
Jabs DA, Nussenblatt RB, Rosenbaum JT, Group SoUNSW. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–16.
Gupta A, Sharma A, Bansal R, Sharma K. Classification of intraocular tuberculosis. Ocul Immunol Inflamm. 2015;23:7–13. https://doi.org/10.3109/09273948.2014.967358.
Ang L, Kee A, Yeo TH, Dinesh VG, Ho SL, Teoh SC, et al. Treatment outcome in patients with presumed tubercular uveitis at a tertiary referral eye care centre in Singapore. Int Ophthalmol. 2016. https://doi.org/10.1007/s10792-016-0401-6.
Gupta A, Bansal R, Gupta V, Sharma A, Bambery P. Ocular signs predictive of tubercular uveitis. Am J Ophthalmol. 2010;149:562–70. https://doi.org/10.1016/j.ajo.2009.11.020.
Agrawal R, Gupta B, Gonzalez-Lopez JJ, Rahman F, Phatak S, Triantafyllopoulou I, et al. The role of anti-tubercular therapy in patients with presumed ocular tuberculosis. Ocul Immunol Inflamm. 2015;23:40–6. https://doi.org/10.3109/09273948.2014.986584.
Bajema KL, Pakzad-Vaezi K, Hawn T, Pepple KL. Tuberculous uveitis: association between anti-tuberculous therapy and clinical response in a non-endemic country. J Ophthalmic Inflamm Infect. 2017;7:19. https://doi.org/10.1186/s12348-017-0137-0.
Mora P, Ghirardini S, Héron E, Sedira N, Olcelli F, Gandolfi S, et al. Ocular tuberculosis: experience of an Italian and French cohort. Acta Ophthalmol. 2015;93:e403-4. https://doi.org/10.1111/aos.12602.
Agrawal R, Gunasekeran DV, Grant R, Agarwal A, Kon OM, Nguyen QD, et al. Clinical features and outcomes of patients with tubercular uveitis treated with antitubercular therapy in the collaborative ocular tuberculosis study (COTS)-1. JAMA Ophthalmol. 2017;135:1318–27. https://doi.org/10.1001/jamaophthalmol.2017.4485.
Kee AR, Gonzalez-Lopez JJ, Al-Hity A, Gupta B, Lee CS, Gunasekeran DV, et al. Anti-tubercular therapy for intraocular tuberculosis: a systematic review and meta-analysis. Surv Ophthalmol. 2016;61:628–53. https://doi.org/10.1016/j.survophthal.2016.03.001.
Smit DP, Esterhuizen TM, Meyer D. The prevalence of intraocular tuberculosis in HIV-positive and HIV-negative patients in south africa using a revised classification system. Ocul Immunol Inflamm. 2016;23:1–8. https://doi.org/10.1080/09273948.2016.1263342.
Tognon MS, Fiscon M, Mirabelli P, Graziani G, Peracchi M, Sattin A, et al. Tuberculosis of the eye in Italy: a forgotten extrapulmonary localization. Infection. 2014;42:335–42. https://doi.org/10.1007/s15010-013-0554-4.
Cordero-Coma M, Garzo I, Salazar R, Franco M, Calleja S, Ruiz de Morales JM. Treatment of presumed tuberculous uveitis affecting the posterior segment: diagnostic confirmation and long term outcomes. Arch Soc Esp Oftalmol. 2013;88:339–44. https://doi.org/10.1016/j.oftal.2012.11.011.
Li KK, Chan WM, Tam BS, Ng JS, Lam DS. Needle tap in the diagnosis of inflammation. Ophthalmology. 2004;111:609. https://doi.org/10.1016/j.ophtha.2003.12.036 (author reply—10).
Sharma K, Gupta V, Bansal R, Sharma A, Sharma M, Gupta A. Novel multi-targeted polymerase chain reaction for diagnosis of presumed tubercular uveitis. J Ophthalmic Inflamm Infect. 2013;3:25. https://doi.org/10.1186/1869-5760-3-25.
Bouza E, Merino P, Muñoz P, Sanchez-Carrillo C, Yáñez J, Cortés C. Ocular tuberculosis. A prospective study in a general hospital. Medicine (Baltimore). 1997;76:53–61.
Troutbeck R, Lim LL. Clinical controversy: to treat, or not to treat? That is the tuberculosis question. Clin Exp Ophthalmol. 2012;40:653–4. https://doi.org/10.1111/j.1442-9071.2012.02855.x.
Abrams J, Schlaegel TF. The role of the isoniazid therapeutic test in tuberculous uveitis. Am J Ophthalmol. 1982;94:511–5.
Bansal R, Gupta A, Gupta V, Dogra MR, Bambery P, Arora SK. Role of anti-tubercular therapy in uveitis with latent/manifest tuberculosis. Am J Ophthalmol. 2008;146:772–9. https://doi.org/10.1016/j.ajo.2008.06.011.
Patel SS, Saraiya NV, Tessler HH, Goldstein DA. Mycobacterial ocular inflammation: delay in diagnosis and other factors impacting morbidity. JAMA Ophthalmol. 2013;131:752–8. https://doi.org/10.1001/jamaophthalmol.2013.71.
González-Martín J, García-García J, Anibarro L, Vidal R, Esteban J, Blanquer R, et al. Consensus document on the diagnosis, treatment and prevention of tuberculosis. Enferm Infecc Microbiol Clin. 2010;28:297.e1-20. https://doi.org/10.1016/j.eimc.2010.02.006.
Ang M, Hedayatfar A, Wong W, Chee SP. Duration of anti-tubercular therapy in uveitis associated with latent tuberculosis: a case–control study. Br J Ophthalmol. 2012;96:332–6. https://doi.org/10.1136/bjophthalmol-2011-300209.
Ng KK, Nisbet M, Damato EM, Sims JL. Presumed tuberculous uveitis in non-endemic country for tuberculosis: case series from a New Zealand tertiary uveitis clinic. Clin Exp Ophthalmol. 2017;45:357–65. https://doi.org/10.1111/ceo.12881.
Krassas N, Wells J, Bell C, Woodhead M, Jones N. Presumed tuberculosis-associated uveitis: rising incidence and widening criteria for diagnosis in a non-endemic area. Eye (Lond). 2018;32:87–92. https://doi.org/10.1038/eye.2017.152.
La Distia Nora R, van Velthoven ME, Ten Dam-van Loon NH, Misotten T, Bakker M, van Hagen MP, et al. Clinical manifestations of patients with intraocular inflammation and positive QuantiFERON-TB gold in-tube test in a country nonendemic for tuberculosis. Am J Ophthalmol. 2014;157:754 – 61. https://doi.org/10.1016/j.ajo.2013.11.013.
Trad S, Bodaghi B, Saadoun D. Update on immunological test (Quantiferon-TB Gold) contribution in the management of tuberculosis-related ocular inflammation. Ocul Immunol Inflamm. 2017. https://doi.org/10.1080/09273948.2017.1332232.
Acknowledgements
Fundación Galicia Sur Statistics Foundation for statistical support.
Funding
Without financing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
An institucional Review Board approval was obtained from the Comité Ético de Investigación Galicia Sur (registration code 2017/007.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Anibarro, L., Cortés, E., Chouza, A. et al. Early treatment of tuberculous uveitis improves visual outcome: a 10-year cohort study. Infection 46, 549–554 (2018). https://doi.org/10.1007/s15010-018-1161-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1161-1