Abstract
BACKGROUND:
The extracellular matrix (ECM) has many functions, such as segregating tissues, providing support, and regulating intercellular communication. Cartilage-derived ECM (CECM) can be prepared via consecutive processes of chemical decellularization and enzyme treatment. The purpose of this study was to improve and treat osteoarthritis (OA) using porcine knee articular CECM.
METHODS:
We assessed the rheological characteristics and pH of CECM solutions. Furthermore, we determined the effects of CECM on cell proliferation and cytotoxicity in the chondrocytes of New Zealand rabbits. The inhibitory effect of CECM on tumor necrosis factor (TNF)-α-induced cellular apoptosis was assessed using New Zealand rabbit chondrocytes and human synoviocytes. Finally, we examined the in vivo effects of CECM on inflammation control and cartilage degradation in an experimental OA-induced rat model. The rat model of OA was established by injecting monosodium iodoacetate into the intra-articular knee joint. The rats were then injected with CECM solution. Inflammation control and cartilage degradation were assessed by measuring the serum levels of proinflammatory cytokines and C-telopeptide of type II collagen and performing a histomorphological analysis.
RESULTS:
CECM was found to be biocompatible and non-immunogenic, and could improve cell proliferation without inducing a toxic reaction. CECM significantly reduced cellular apoptosis due to TNF-α, significantly improved the survival of cells in inflammatory environments, and exerted anti-inflammatory effects.
CONCLUSION:
Our findings suggest that CECM is an appropriate injectable material that mediates OA-induced inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Arthritis is a term used to describe all types of inflammation that affect joints. Arthritis chronically causes non-specific inflammatory reactions in various joints, resulting in pain and stiffness [1]. Examples of arthritis include osteoarthritis (OA) and rheumatoid arthritis. These diseases progress gradually via a long process and usually cause a worsening prognosis, with severe pain-induced disabilities [2, 3]. As OA is caused by degenerative changes in the joint cartilage, this condition cannot be completely terminated [4]. Accordingly, therapies for this disease aim to provide mental stability by helping patients understand the attributes of the disease, reduce pain, maintain joint function, and prevent deformation [5, 6]. Injecting medicines into the patient’s knee should prevent the progression of OA and improve patient quality of life by controlling inflammation [7].
Extracellular matrix (ECM) has been used in various studies as a treatment for OA. Treatment with biologics comprising ECM is an important option in regenerative medicine for tissue reconstruction. Studies have reported pain relief, inflammation control, and cartilage damage suppression in OA-induced animals administered ECM [8,9,10]. Notably, the cells and genetic material contained in the ECM can be chemically and physically removed [11, 12]. The ECM has many functions, such as segregating tissues, providing support, and regulating intercellular communication. It also binds to a wide range of cell growth factors and serves as a local repository for cells [13]. The ECM thus serves as a biologically active scaffold that affects cell differentiation, proliferation, survival, polarity, and migration [14,15,16,17]. ECM derived from different tissues has distinct characteristics as the structure and function of each tissue are very specific. The cartilage tissue has a relatively high collagen and proteoglycan content and low ratio of cells-to-ECM, but brain tissue contains much little collagen and proteoglycan and much higher ratio of cells-to-ECM. [18] Porcine knee joint cartilage-derived ECM (CECM) has a high affinity and complexity with cells. The CECM consists of a variety of molecules and includes collagen family of proteins, glycosaminoglycans (GAGs), elastic fibers, adhesive glycoproteins, and proteoglycans. CECM may affect cell function through harboring growth factor-binding proteins or growth factors. Currently, various medical engineering applications of CECM are being explored [19].
Monosodium iodoacetate (MIA) is an inhibitor of glyceraldehyde-3-phosphate dehydrogenase activity. Inhibitors of glycolysis have been shown to induce chondrocyte death in vitro [20]. Previously, MIA was used to induce OA in experimental animals. Injection of MIA into the knee joint of an experimental animal causes damage to the cartilage and subchondral bone and high levels of proinflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin-(IL)1β, and IL-6, as seen in human OA joints [21, 22]. These findings indicate that proinflammatory cytokines can be used as indicators of OA induction in experimental animals. Studies are constantly being conducted to identify anti-osteoarthritic effects by analyzing proinflammatory cytokines (TNF-α, IL-1β, and IL-6) in the serum of animals. TNF-α is known to induce apoptosis and inflammation. TNF-α causes the collagen network to collapse, resulting in chondrocyte death [23].
The purpose of this study was to identify the potential of CECM solution as an injectable treatment for OA. CECM has been shown to promote the regeneration of tissue defects through several mechanisms. Furthermore, remodeling of the CECM film was demonstrated to improve hyaline cartilage tissue formation in canine models of cartilage defects [22]. Exposing chondrocytes to the CECM promotes neocartilage formation and cartilage zone-specific gene expression [24]. CECM has been used to repair cartilage by administering IL-4 [25]. CECM has also been used to inhibit blood vessel formation in rabbit corneas [26]. Notably, CECM is easily degradable in animals [19, 27].
Owing to its immunomodulatory and anti-angiogenic properties, CECM is an attractive treatment for OA because OA is now considered to progress owing to cytokine secretion, immune cell infiltration, and excessive inflammation [28,29,30]. We studied the basic properties of CECM, such as its rheological characterization, compressive syringe force, and pH, and its effects on the proliferation and cytotoxicity of chondrocytes in vitro. We also determined whether CECM could inhibit TNF-α-induced apoptosis of chondrocytes and synoviocytes in vitro, and the ability of CECM to control inflammation and protect against cartilage damage in a rat model of OA. Collectively, the results revealed a positive effect of CECM treatment on cartilage integrity in vivo and reduced expression of several proinflammatory cytokines and C-telopeptide of type II collagen (CTX-II).
2 Materials and methods
2.1 Preparation of the CECM solution
The CECM was extracted using previously described protocols [18, 30]. Briefly, porcine knee joint cartilage sections were obtained from the hind legs of market pigs under sterile conditions. After the adherent soft tissues were removed, the cartilage slices were washed with phosphate-buffered saline (PBS; WelGENE, Gyeongsan, Korea), freeze-dried, and pulverized using an auto cryogenic sample crusher at − 190 °C. For decellularization, the resultant cartilage powder was treated with hypotonic buffer (10 mM Tris–HCl, pH 8.0) for 4 h, 0.5% sodium dodecyl sulfate in Tris-buffered saline (10 mM NaCl, pH 7.6) for 2 h, and DNase (6000 U, Roche, Basel, Switzerland) for 15 h. The decellularized cartilage was treated with 0.5 M HCl and 0.1% pepsin (2500 U/mg, Sigma-Aldrich, St. Louis, MO, USA) and stirred for 24 h. The solution was neutralized to pH 7.6 and dialyzed using a 2 kD dialysis membrane for 24 h. The obtained CECM was dissolved in 0.9% saline to yield 1%, 2%, and 4% CECM solutions.
2.2 Rheological characterization
The rheological properties of the CECM solution were determined by an oscillatory frequency sweep test using a hybrid rheometer (HR-2, New Castle, DE, USA). For each sample, 0.3 mL of the CECM solutions was placed between parallel plates (80 mm in diameter) with a gap distance of 250 μm. The temperature was maintained at 37 °C using a Peltier temperature controller. Dynamic frequency sweeps of the different concentrations of the CECM solutions (1%, 2%, and 4%) were performed from 0.01 of 100 Hz. All measurements were repeated three times for each sample, and the reported data represent the average value of the replicates.
2.3 Relationship between pH and CECM concentration
The pH of the CECM solution was measured using a pH meter (HORIBA Scientific, Kyoto, Japan). After filling each chamber with the CECM solution, the electrode was immersed in the solution to ensure electrical contact. All measurements were repeated three times for each sample, and the reported data represent the average value of the replicates.
2.4 Cell culture
New Zealand rabbit chondrocytes (CLOUD-CLONE CORP, Houston, TX, USA) and human synoviocytes (SW982; ATCC, Manassas, VA, USA) were used in this study. The cells were maintained in Dulbecco’s modified Eagle’s medium (DMEM; Grand Island, NY, USA) containing 10% fetal bovine serum (FBS; Grand Island, NY, USA) and antibiotic–antimycotic at 37 °C in a 5% CO2 incubator. The cells were then maintained and grown in 150 mm cell culture dishes at 80–90% confluence before cell detachment and subculture. After washing with PBS, the cells were incubated in 3 mL trypsin-ethylenediaminetetraacetic acid (trypsin, EDTA) for 5 min at 37 °C in a CO2 incubator. Thereafter, the cell suspensions were centrifuged for 10 min at 4 °C and 1000 rpm. Subsequently, the cell pellet was resuspended in DMEM, and the seed density was controlled using a hemocytometer and a microscope.
2.5 Live/dead assay
The cytotoxicity of CECM was determined using a viability kit assay (Live/Dead® Viability/Cytotoxicity Kit, Invitrogen, Carlsbad, CA, USA). Briefly, 200 μL of the chondrocyte cell suspension was seeded into each confocal dish (SPL, Pocheon, Korea) at a final concentration of approximately 5 × 104 cells/mL. After 48 h of cell stabilization, media containing 1%, 2%, and 4% CECM were added to the dishes for 7 days. At the end of the treatment period, the dishes were washed with PBS. Thereafter, 1 μL calcein acetoxymethyl (Calcein AM) and 2 μL ethidium homodimer-1 (EthD-1) were added. After a brief incubation of 1 h at 37 °C, the cells were visualized using a laser scanning confocal microscope. The live cells showed green fluorescence owing to calcein AM dye, whereas dead cells showed red fluorescence owing to EthD-1 staining.
2.6 Cell proliferation assay
The effects of CECM on chondrocyte proliferation were investigated using a water-soluble tetrazolium salt (WST) assay (EZ-cytox, DoGenBio, Seoul, Korea). Approximately 5 × 103 cells/well were seeded in 48-well plates at 48 h before treatment and exposed to 1%, 2%, and 4% CECM for different time periods (ranging from 1 to 7 days). After treatment completion, each well was washed with PBS and fresh DMEM, and 20 μL of WST-assay reagent was added. After incubation for 1 h at 37 °C, the absorbance was measured at 450 nm.
2.7 Treatment with TNF-α and CECM
The effects of CECM on the inhibition of chondrocyte and synoviocyte apoptosis induced by rabbit TNF-α (R&D Systems, Minneapolis, MN, USA) and human TNF-α (R&D Systems, Minneapolis, MN, USA), respectively, were investigated using WST-assay. Approximately, 5 × 103 cells/well were seeded in 48-well plates at 48 h before treatment with 1%, 2%, and 4% CECM and a range of concentrations (from 0.6 to 60 ng/mL) of three TNF-α for the next 7 days. After treatment completion, each well was washed with PBS and fresh DMEM, and 20 μL of WST-assay reagent was added. After incubation for 1 h at 37 °C, the absorbance was measured at 450 nm.
2.8 Animals and injection of CECM
Sprague Dawley rats (male, 6 weeks old) were used in this study. The rats were provided by the Institutional Animal House and reared under standard environmental conditions, with a 12 h light/dark cycle at 20 ± 3 °C and 55 ± 10% humidity. All rats were fed a standard diet and water ad libitum. To reduce any potential stress, the animals were reared in solid bottom cages (three per cage). All rats underwent a 7-day adaptation period. The rats were randomly divided into normal (n = 4), OA control (n = 6), and OA control injected with 1%, 2%, and 4% CECM (n = 6 each) groups.
To induce OA, the right hind knees of the rats were shaved following anesthesia using isoflurane. For all groups of rats, except for Group I, a single injection of MIA (3 mg/50 μL) was administered into the articular cavity on day 7. Group I rats received an equivalent volume of saline via injection. All rats in Groups III–V received 100 μL of CECM via injection 2 weeks after MIA injection. Rats in Groups I and II received an equivalent volume of saline via injection. All rats were sacrificed using carbon dioxide gas 28 days after the first MIA or saline injection.
2.9 Measurement of the proinflammatory cytokines and CTX-II levels in serum
Rats were anesthetized with isoflurane and blood samples were collected from the heart. The blood samples were allowed to clot for 1 h on ice and centrifuged at 1,200 × g for 10 min at 4 °C. The supernatant was obtained and stored at − 20 °C until use. The serum levels of proinflammatory cytokines, including TNF-α (Invitrogen), IL-1β (R&D Systems), and IL-6 (Invitrogen), and cartilage degeneration mediators, such as CTX-II (MyBioSource, San Diego, CA, USA), were determined using enzyme-linked immunosorbent assay (ELISA) kits, according to the manufacturer’s recommendations.
2.9.1 Histological examination
Histological changes were investigated to confirm the effects of CECM on cartilage damage in the knee joints of MIA-induced OA rats. Knee samples were fixed in 10% formalin for 5 days at 4 °C and decalcified in 5% nitric acid for 2 days at 4 °C. Following decalcification, the samples were dehydrated and embedded in paraffin. Micro-Sects. (10 μm) were stained with hematoxylin and eosin (H&E) and safranin O-fast green. Terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay was performed manufacturer’s protocol (Abbkine, Wuhan, China).
2.9.2 Statistical analysis
The results are expressed as mean ± standard deviation for at least three separate data points for each group. The statistical significance of the differences between two groups was evaluated using the Student’s t-test for pairwise comparisons or one-way analysis of variance (ANOVA) followed by a Tukey post hoc test. Statistical significance was set at p < 0.05.
3 Results
3.1 Characterization of the CECM solution
Flow behavior is important for fabricating injectable OA therapies as is the characterizing of these solutions, including their long-term behavior in the knee and injectability. Figure 1 shows the η* for CECM solutions as a function of the oscillation frequency (0.01–100 Hz). All CECM solutions were found to display a shear thinning flow behavior as η* decreased approximately linearly with increasing frequency. At 0.01 Hz, the η* values of the 1%, 2%, and 4% CECM solutions were 1.95, 20.26, and 73.73 Pa.s, respectively. Therefore, a high concentration of the CECM solution resulted in a high η*. Similar observations were obtained under other selected frequencies, such as 0.1, 1, 10, and 100 Hz. The results for the pH of the CECM solutions are shown in Table 1. The pH values of the 1%, 2%, and 4% CECM solutions were 6.86, 6.95, and 7.03, respectively. Thus, the higher the concentration of CECM, the slightly higher was the pH value.
3.2 Cytotoxic effects of CECM on the proliferation of chondrocytes
The microscopic images of cells on a confocal dish following treatment with fluorescent dyes are presented in Fig. 2A–D. The images show live (green)/dead (red) cells staining results with (A) fresh media, (B) CECM 1%, (C) CECM 2%, and (D) CECM 4% at 7 days. Figure 2E shows the percentage of live cells after 7 days of incubation with fresh media with or without various concentrations of CECM. The percentages of live cells in the media (only fresh media), CECM 1%, 2%, and 4% groups were 86.5%, 87.2%, 84.7%, and 87.6%, respectively. When the percentages of live cells in the control and 1%, 2%, and 4% CECM solutions were compared, no significant differences were found. The proliferation results revealed significant increases in proliferation rates after 7 days of exposure to CECM with respect to the media group (only fresh media). The proliferation rate was found to be dependent on the concentration of CECM. In addition, the proliferation rate of the 4% CECM solution increased by 70.0% compared to that of the media group on day 7 (Fig. 3).
Cell viability fluorescent images by treated CECM solutions. Cells stained green owing to the “Live” calcein AM dye and those stained red owing to the “Dead” ethidium homodimer-1 dye were recorded after excitation with laser light. Chondrocytes after incubation for 7 days in A 0%, B 1%, C 2%, and D 4% 0% A, 1% B, 2% C, and 4% D CECM media. E The black portion of each bar represents the percentage of live cells. Scale bars, 100 μm
3.3 Effects of CECM on the TNF-α-induced apoptosis of chondrocytes and synoviocytes
As shown in Fig. 4A and B, various doses of TNF-α were initially used to induce a dose-dependent cell death response in the media group (only fresh media). When 60 ng/mL TNF-α was administered, the cell viability of chondrocytes and synoviocytes was 72.7% and 85.4%, respectively. Under similar conditions, 1%, 2%, and 4% CECM solutions inhibited TNF-α-induced apoptosis of chondrocytes. However, CECM did not exhibit an inhibitory effect on the TNF-induced apoptosis of synoviocytes.
Effect of CECM concentration in TNF-α. Chondrocytes A and synoviocytes B were treated with different concentrations of TNF-α (0.6–60 ng/mL) and CECM (1%, 2%, and 4%) for 36 h. The p-value is based on a comparison between the media group (non-treated CECM) and the CECM 1%, 2%, and 4% groups treated with the same concentration of TNF-α (*p < 0.05, **p < 0.01, and ***p < 0.001, using one-way ANOVA)
3.4 Expression of proinflammatory cytokines and degenerative marker in animals with OA
The effects of CECM on proinflammatory cytokines and degenerative marker levels in the serum of OA-induced rats were determined using ELISA. As shown in Fig. 5, the serum levels of TNF-α, IL-1β, IL-6, and CTX-II in rats injected with MIA increased by 184.3%, 1144.9%, 141.6%, and 53.6%, respectively, compared to those in rats injected with the control. This result suggests that MIA-induced inflammation and cartilage degeneration occur in the joint. The MIA-induced increase in proinflammatory cytokines and CTX-II levels was effectively suppressed by CECM treatment. In fact, the levels of TNF-α, IL-1β, IL-6, and CTX-II were decreased by 29 − 36.5%, 33.8 − 40.6%, 29.4 − 41.7%, and 20.9 − 31.4%, respectively, in the CECM-treated groups compared to the MIA-injected groups. However, dose-dependent differences were not observed. The serum level of IL-6 was also found to significantly decrease in the 2% CECM group.
Effects of CECM on the cytokines of serum. A TNF-α, B IL-1β, C IL-6, and D CTX-II in rats with MIA-induced (OA). TNF-α, IL-1β, IL-6 and CTX-II levels were measured using enzyme-linked immunosorbent assay (ELISA). The p-value is based on a comparison between the control and MIA, and MIA and CECM groups (*,# p < 0.05, **,## p < 0.01, and ***,### p < 0.001, versus MIA (*) or control group (#) calculated using one-way)
3.5 Histological analysis of knee cartilage
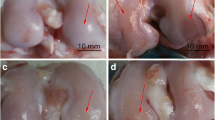
To assess the chondroprotective effect of CECM, knee joints from each treatment group were isolated after the animals were sacrificed for microscopic analysis. Staining revealed normal cellularity and smooth articular cartilage in the control group. However, the knee joints from MIA-induced OA rats exhibited apparent hypocellularity and massive proteoglycan loss. These histomorphological changes in the knee joint were significantly reduced in the CECM-treated OA rats. H&E and safranin O-fast green staining revealed that CECM prevented MIA-induced cartilage surface irregularity (Fig. 6A–D). TUNEL assay results indicate that the control group did not detect chondrocyte death. In contrast, the MIA-induced OA model showed the clear cell death in the cartilage area. Interestingly, the 2% and 4% CECM groups exhibited few positive fluorescence signals, although the 1% CECM group marginally detected cell death in the cartilage area. (Fig. 6E).
Effect of CECM on the histological change. A, B Representative H&E and C, D safranin O-fast green staining images. The prevention effect of cartilage destruction and massive proteoglycan loss by CECM in rat osteoarthritis model. Several shrunken nuclei and hypocellularity (black arrows) were observed in the MIA group. E TUNEL assay. Fluorescent results indicate cell death (red arrows). (B: bone, C: cartilage, MZ: meniscus zone). Scale bars, A, C 1000 μm, B, D 200 μm, and E 50 μm
4 Discussion
ECM biomaterials, such as CECM, are an attractive therapy for OA disease modification owing to their demonstrated regenerative capabilities in canine models [22]. As a suitable treatment for OA is currently unavailable and because CECM has shown promise in other degenerative diseases and musculoskeletal defects, we sought to explore its potential to treat OA in a rat model and in rabbit and human cells.
The rheological properties of a material are crucial for its administration via injection, its residence time within the articular cavity, and the appropriate function of the joint after injection. The shear response of the three CECM concentrations revealed the shear thinning flow behavior. Walking motion and running motion are appropriate for frequencies of 0.5 and 2.5 Hz, respectively [31]. Based on the rheological characterization of CECM compared to currently available hyaluronic acid products in the USA, 1%, 2%, and 4% CECM solutions are similar to Hyalgan®, Supartz®, and Monovisc®, respectively, at 0.5 and 2.5 Hz [31, 32]. The safe pH range for injection into the body, providing the solutions are not appropriately buffered, is 4.5–8.0. The closer the pH of a material is to the upper and lower limits of this pH range, the more likely it is to cause irritation and discomfort at the injection site [33]. As the pH of the CECM is very close to neutral, side effects, owing to pH, will be very unlikely.
As a naturally sourced ECM that is intended for use as a biomaterial, the cytotoxicity and immunogenicity of CECM may be of concern as heterologous proteins may be cytotoxic and immunogenic and can be accompanied by serious consequences. Collagen accounts for the highest proportion of CECM [19]. The immunogenicity and antigenicity of collagen are closely related to its purity and structure. Structurally, the telopeptides located in the immunodominant epitope and non-helical terminal regions within the α chain may result in irregular immune responses [34]. However, the telopeptides can be removed using the pepsin digestion method, and the epitope is determined by a specific amino acid sequence. The 258–272 amino acids of human type II collagen have been demonstrated to behave as important immunodominant epitopes [35, 36], and they can be perceived immunologically when treated under pathological conditions. Nevertheless, if there is any change in the above-mentioned amino acid sequence, the immunodominant epitope is destroyed [37]. In addition to the risk of creating a pathological immune response, some animals have been found to share the same immunodominant epitope in this sequence as human type II collagen [35, 38]. The breakdown of cartilage tissue during OA is related to the loss of ECM and chondrocyte death [39]. Our results indicated that CECM has low cytotoxicity to chondrocytes. In addition, CECM positively affected chondrocyte proliferation. However, LIVE/DEAD proliferation assays showed only chondrocytes derived from a rabbit; therefore, different species, specifically human cells, should be assessed to delineate the effects of CECM.
Cell death is a basic cellular response that plays an important role in regulating tissue homeostasis by removing unwanted cells and shaping most animals during development. Three main types of death have been reported based on cell morphology: autophagic cell death, apoptosis, and necroptosis or necrosis. Most previous studies on the effect of TNF-α on cell death have shown that TNF-α induces cell death via apoptosis [40,41,42]. The basic function of chondrocytes and synoviocytes is to produce cartilage and synovial fluid, respectively [43, 44]. Therefore, if TNF-α inhibits the death of chondrocytes and synoviocytes, it will slow the progression of OA, such as cartilage damage. All the tested concentrations of CECM had a suppressive effect on TNF-α-induced chondrocyte death; however, CECM had no inhibitory effect on the death of synoviocytes.
Although CECM is employed in a variety of tissue engineering applications, no study has sought to demonstrate its protective effect in the treatment of OA. Therefore, the present in vivo investigation was performed to assess the anti-inflammatory and anti-OA effects of CECM in an MIA-induced OA rat model. Several OA incidences have shown that inflammatory mediators play an important role in the expansion and progression of cartilage destruction [45]. Proinflammatory cytokines and inflammatory mediators display potential catabolic properties that cause the pathophysiological progression of OA [46]. Various parameters were used to evaluate the anti-OA effect of CECM in a rat model of MIA-induced OA, including proinflammatory cytokines, cartilage degradation mediators, and histopathological features. Our results showed that CECM significantly relieved inflammation in the MIA-induced OA rat model. Several studies have shown that inflammation plays an important role in the progression of arthritis and have confirmed the chondroprotective effect of inflammation. Proinflammatory cytokines such as IL-1 beta, TNF control the degeneration of knee joint cartilage matrix, which makes them targets for therapeutic strategies. [47, 48] The present study showed that CECM affects the chondroprotective effects in OA and MIA-induced OA rat models by inhibiting proinflammatory cytokines and cartilage degradation mediators in serum.
In our animal model, H&E and safranin O-fast green staining revealed the hypocellularity of knee joint cartilage in the tibia, including massive proteoglycan loss, and the cell survival result, the number of chondrocytes in the MIA group was lower than that in the sham-treated control group. Hypocellularity and proteoglycan loss are the result of OA induction, which was achieved by injecting MIA into the knee joint [49, 50]. Injection of CECM increased the number of chondrocytes markedly and alleviated proteoglycan loss. Injecting CECM might mitigate OA symptoms by inhibiting the death of chondrocytes and controlling the inflammatory environment of the knee articular cavity.
Inflammation plays a key role in OA progression and damage to the articular cartilage structure. Proinflammatory cytokines are reflected throughout OA expansion and break the balance between CECM degradation and repair [51, 52]. These indications aggravate cartilage degradation and the clinical symptoms of OA. Thus, targeting the inflammatory reaction may be a valuable approach for treating the expansion and progression of OA. In the present study, CECM was confirmed to be a suitable material for injection and had low cytotoxicity and a positive effect on cell proliferation. In addition, CECM inhibited apoptosis caused by TNF-α, prevented the progression of OA remarkably, and reduced inflammatory reactions. Lastly, by assessing the histopathology of the knee joint, the protective effect of CECM against damage to chondrocytes was revealed in relation to that observed in the MIA group. Our results clearly indicate that CECM may be an effective therapeutic agent for the treatment of OA or OA-associated symptoms. However, we still do not know the mechanism of CECM efficacy on OA disease. It is expected that the factors and components present in CECM may decrease or control related inflammation environments. We are planning to do an analysis of potential key components in CECM to elucidate its mechanism in future studies.
References
Hunter DJ, Guermazi A, Roemer F, Zhang Y, Neogi T. Structural correlates of pain in joints with osteoarthritis. Osteoarthritis Cartilage. 2013;21:1170–8.
Chapple CM, Nicholson H, Baxter GD, Abbott JH. Patient characteristics that predict progression of knee osteoarthritis: a systematic review of prognostic studies. Arthritis Care Res (Hoboken). 2011;63:1115–25.
Laasila K, Laasonen L, Leirisalo-Repo M. Antibiotic treatment and long term prognosis of reactive arthritis. Ann Rheum Dis. 2003;62:655–8.
Pelletier JP, Martel-Pelletier J, Abramson SB. Osteoarthritis, an inflammatory disease: potential implication for the selection of new therapeutic targets. Arthritis Rheum. 2001;44:1237–47.
Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. Lancet. 2005;365:965–73.
Bhatia D, Bejarano T, Novo M. Current interventions in the management of knee osteoarthritis. J Pharm Bioallied Sci. 2013;5:30–8.
Billesberger LM, Fisher KM, Qadri YJ, Boortz-Marx RL. Procedural treatments for knee osteoarthritis: a review of current injectable therapies. Pain Res Manag. 2020;2020:3873098.
Jacobs HN, Rathod S, Wolf MT, Elisseeff JH. Intra-articular injection of urinary bladder matrix reduces osteoarthritis development. AAPS J. 2017;19:141–9.
Li Y, Cao J, Han S, Liang Y, Zhang T, Zhao H, et al. ECM based injectable thermo-sensitive hydrogel on the recovery of injured cartilage induced by osteoarthritis. Artif Cells Nanomed Biotechnol. 2018;46:152–60.
Proffen BL, Sieker JT, Murray MM, Akelman MR, Chin KE, Perrone GS, et al. Extracellular matrix-blood composite injection reduces post-traumatic osteoarthritis after anterior cruciate ligament injury in the rat. J Orthop Res. 2016;34:995–1003.
Gilbert TW, Sellaro TL, Badylak SF. Decellularization of tissues and organs. Biomaterials. 2006;27:3675–83.
Crapo PM, Gilbert TW, Badylak SF. An overview of tissue and whole organ decellularization processes. Biomaterials. 2011;32:3233–43.
Kumar V, Abbas AK, Fausto N, Aster JC. Robbins and Cotran pathologic basis of disease. 9th edition. Professional edition e-book. Amsterdam: Elsevier health sciences; 2014.
Lo CM, Wang HB, Dembo M, Wang Y. Cell movement is guided by the rigidity of the substrate. Biophys J. 2000;79:144–52.
Hadjipanayi E, Mudera V, Brown RA. Close dependence of fibroblast proliferation on collagen scaffold matrix stiffness. J Tissue Eng Regen Med. 2009;3:77–84.
Engler AJ, Sen S, Sweeney HL, Discher DE. Matrix elasticity directs stem cell lineage specification. Cell. 2006;126:677–89.
Wang HB, Dembo M, Wang YL. Substrate flexibility regulates growth and apoptosis of normal but not transformed cells. Am J Physiol Cell Physiol. 2000;279:C1345–50.
Beachley VZ, Wolf MT, Sadtler K, Manda SS, Jacobs H, et al. Tissue matrix arrays for high-throughput screening and systems analysis of cell function. Nat Methods. 2015;12:1197–204.
Kim HJ, Lee S, Yun HW, Yin XY, Kim SH, Choi BH, et al. In vivo degradation profile of porcine cartilage-derived extracellular matrix powder scaffolds using a non-invasive fluorescence imaging method. J Biomater Sci Polym Ed. 2016;27:177–90.
Jhun J, Lee SH, Na HS, Seo HB, Kim EK, Moon SJ, et al. The chicken combs extract alleviates pain and cartilage degradation in rat model osteoarthritis. Tissue Eng Regen Med. 2015;12:352–61.
Imamura M, Ezquerro F, Marcon Alfieri F, Vilas Boas L, Tozetto-Mendoza TR, Chen J, et al. Serum levels of proinflammatory cytokines in painful knee osteoarthritis and sensitization. Int J Inflamm. 2015;2015:1–8.
Li TZ, Jin CZ, Choi BH, Kim MS, Kim YJ, Park SR, et al. Using cartilage extracellular matrix (CECM) membrane to enhance the reparability of the bone marrow stimulation technique for articular cartilage defect in canine model. Adv Func Mater. 2012;22:4292–300.
Aigner T, Kim HA. Apoptosis and cellular vitality: issues in osteoarthritic cartilage degeneration. Arthritis Rheum. 2002;46:1986–96.
Grogan SP, Chen X, Sovani S, Taniguchi N, Colwell CW Jr, Lotz MK, et al. Influence of cartilage extracellular matrix molecules on cell phenotype and neocartilage formation. Tissue Eng Part A. 2014;20:264–74.
Tian G, Jiang S, Li J, Wei F, Li X, Ding Y, et al. Cell-free decellularized cartilage extracellular matrix scaffolds combined with interleukin 4 promote osteochondral repair through immunomodulatory macrophages: in vitro and in vivo preclinical study. Acta Biomater. 2021;127:131–45.
Choi BH, Choi KH, Lee HS, Song BR, Park SR, Yang JW, et al. Inhibition of blood vessel formation by a chondrocyte-derived extracellular matrix. Biomaterials. 2014;35:5711–20.
Kwon JS, Yoon SM, Shim SW, Park JH, Min KJ, Oh HJ, et al. Injectable extracellular matrix hydrogel developed using porcine articular cartilage. Int J Pharm. 2013;454:183–91.
De Lange-Brokaar BJ, Ioan-Facsinay A, Van Osch GJ, Zuurmond A-M, Schoones J, Toes RE, et al. Synovial inflammation, immune cells and their cytokines in osteoarthritis: a review. Osteoarthritis Cartilage. 2012;20:1484–99.
Revell PA, Mayston V, Lalor P, Mapp P. The synovial membrane in osteoarthritis: a histological study including the characterisation of the cellular infiltrate present in inflammatory osteoarthritis using monoclonal antibodies. Ann Rheum Dis. 1988;47:300–7.
Benito MJ, Veale DJ, FitzGerald O, van den Berg WB, Bresnihan B. Synovial tissue inflammation in early and late osteoarthritis. Ann Rheum Dis. 2005;64:1263–7.
Bhuanantanondh P, Grecov D, Kwok E. Rheological study of viscosupplements and synovial fluid in patients with osteoarthritis. CMBES Proc. 2010;33:522.
Park DY, Yun HW, Lim S, Truong MD, Yin XY, Park J, et al. Cross-linked cartilage acellular matrix film decreases postsurgical peritendinous adhesions. Artif Organs. 2020;44:E136–49.
Nicholls M, Manjoo A, Shaw P, Niazi F, Rosen J. Rheological properties of commercially available hyaluronic acid products in the United States for the treatment of osteoarthritis knee pain. Clin Med Insights Arthritis Musculoskelet Disord. 2018;11:1179544117751622.
Lynn AK, Yannas IV, Bonfield W. Antigenicity and immunogenicity of collagen. J Biomed Mater Res Part B: Appl Biomater Off J Soc Biomater Japan Soc Biomater Aust Soc Biomater Korean Soc Biomater. 2004;71:343–54.
Kim HY, Kim WU, Cho ML, Lee SK, Youn J, Kim SI, et al. Enhanced T cell proliferative response to type II collagen and synthetic peptide CII (255–274) in patients with rheumatoid arthritis. Arthritis Rheum. 1999;42:2085–93.
Ria F, Penitente R, De Santis M, Nicolò C, Di Sante G, Orsini M, et al. Collagen-specific T-cell repertoire in blood and synovial fluid varies with disease activity in early rheumatoid arthritis. Arthritis Res Ther. 2008;10:R135.
Myers LK, Tang B, Rosioniec EF, Stuart JM, Kang AH. PART III Autoimmunity an altered peptide ligand of type ii collagen suppresses autoimmune arthritis. Crit RevTM Immunol. 2007;27:345–56.
Cremer MA, Xiu JY, Myers LK, Brand DD, Rosloniec EF, Kang AH. T cell immunity to type II collagen in the biobreeding rat: The identification and characterization of RT1u-restricted T cell epitopes on α1 (II). J Immunol. 2004;173:1795–801.
Im G-I. Perspective on intra-articular injection cell therapy for osteoarthritis treatment. Tissue Eng Regen Med. 2019;16:357–63.
Lee SW, Lee HJ, Chung WT, Choi SM, Rhyu SH, Kim DK, et al. TRAIL induces apoptosis of chondrocytes and influences the pathogenesis of experimentally induced rat osteoarthritis. Arthritis Rheum. 2004;50:534–42.
Lee SW, Song YS, Lee SY, Yoon YG, Lee SH, Park BS, et al. Downregulation of protein kinase CK2 activity facilitates tumor necrosis factor-α-mediated chondrocyte death through apoptosis and autophagy. PLoS One. 2011;6:e19163.
Coustry F, Posey KL, Liu P, Alcorn JL, Hecht JT. D469del-COMP retention in chondrocytes stimulates caspase-independent necroptosis. Am J Pathol. 2012;180:738–48.
Akkiraju H, Nohe A. Role of chondrocytes in cartilage formation, progression of osteoarthritis and cartilage regeneration. J dev biol. 2015;3:177–92.
Toshihiko I, Mitsumori S, Hiroko K, Haruko Y, Kayoko NI. Morphology and functional roles of synoviocytes in the joint. Arch Histol Cytol. 2000;63:17–31.
Lee SG, Lee EJ, Park WD, Kim JB, Kim EO, Choi SW. Anti-inflammatory and anti-osteoarthritis effects of fermented Achyranthes japonica Nakai. J Ethnopharmacol. 2012;142:634–41.
Mobasheri A. Intersection of inflammation and herbal medicine in the treatment of osteoarthritis. Curr Rheumatol Rep. 2012;14:604–16.
Ferrero-Miliani L, Nielsen OH, Andersen PS, Girardin S. Chronic inflammation: importance of NOD2 and NALP3 in interleukin-1β generation. Clin Exp Immunol. 2007;147:227–35.
Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol. 2011;7:33–42.
Jeong JH, Moon SJ, Jhun JY, Yang EJ, Cho ML, Min JK. Eupatilin exerts antinociceptive and chondroprotective properties in a rat model of osteoarthritis by downregulating oxidative damage and catabolic activity in chondrocytes. PLoS One. 2015;10:e0130882.
Khodir SA, Al-Gholam MA, Salem HR. L-Carnitine potentiates the anti-inflammatory and antinociceptive effects of diclofenac sodium in an experimentally-induced knee osteoarthritis rat model. Iran J Basic Med Sci. 2020;23:1035-44.
Mobasheri A. Osteoarthritis year 2012 in review: biomarkers. Osteoarthritis Cartilage. 2012;20:1451–64.
Felson DT. Developments in the clinical understanding of osteoarthritis. Arthritis Res Ther. 2009;11:203.
Acknowledgements
Everyone who contributed significantly to the work has been listed. This research was supported by the National Research Foundation Grant (NRF- 2019M3E5D1A02070861.)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical statement
All animal studies were approved by the Institutional Review Board at the Pukyong National University (PKNUIACUC-2020–03).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, SH., Jo, SH., Kim, SH. et al. Anti-Osteoarthritic Effects of Cartilage-Derived Extracellular Matrix in a Rat Osteoarthritis Model. Tissue Eng Regen Med 20, 83–92 (2023). https://doi.org/10.1007/s13770-022-00508-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-022-00508-7