Abstract
Headache disorders are the most prevalent neurological conditions in the Sub-Saharan Africa and the second cause of disability. In this study, we analyze the knowledge about headache disorders and their management among Cameroonian healthcare providers. We conducted an interventional study with a prospective cohort design. Cameroonian health care providers from the whole country were invited. The evaluation was based on a questionnaire that was done before and after a 4-day educational course. The study included 42 participants, 52.4% female, aged 36.8 years. Participants treated a median of 240 monthly patients. Headache was reported as the most frequent neurological condition in their clinics (34%). Mean number of neurological patients seen per week was 69.3, among them 20 were headache patients. At baseline, only 35.8% correctly mentioned at least one primary headache, increasing to 78.6% after the course (p = 0.002). Secondary headaches were correctly identified by 19.0% at baseline and 40.5% after the course (p = 0.01). Clinical history was considered sufficient for headache diagnosis by 57.1% before and 78.6% after (p = 0.5). Correct red flags were mentioned at baseline by only 14.3% of participants, increasing to 40.5% after the course (p = 0.005). At baseline, the preferred symptomatic was paracetamol (47.6%) and Non-Steroidal Anti-Inflammatory Drugs (9.5%), changing to 23.8 and 66.7% after the course (p = 0.05 and < 0.001). Headache was reported as the most frequent neurological disorders. Knowledge about primary headache disorders and their etiology was scarce, and the clinical concept of red flags was limited. The acute drug of choice was paracetamol.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Headache is a universal experience, with a reported life-prevalence of 98.8 in women and 95.9 in men in Sub-Saharan Africa (SSA) study [1]. Epidemiology of headache in SSA is largely unexplored; however, recent studies state that African migraine prevalence is similar to western settings [2, 3]. The Global Campaign Against Headache and Lifting the Burden project promoted by the World Health Organization raised awareness about headache prevalence and impact [4, 5]. Headache is among the most frequent neurological disorders, with 1-year prevalence varying between 16.4 and 88.3% [6, 7]. It represents the second or third leading cause of disability in SSA, with stroke and meningitis, depending on the geographical area [8].
According to the Atlas of Headache Disorders [9], the percentage of African patients with headache that self-treat is the highest worldwide, while the percentage of patients that consult health professionals is three times lower than in Asia and six times lower than in Europe. In addition, despite the arrival of novel therapies, some treatments such as triptans are exceptionally used in Africa, and paracetamol is still the drug of choice [10, 11]. The data on headache prophylaxis is sparse; in a study on an Ethiopian student population, the percentage of headache patients receiving oral preventive drugs was nil [12].
Headache patients are diagnosed and classified into primary or secondary headaches according to the International Classification of Headache Disorders (ICHD) [13]; however, few African epidemiological studies use ICHD criteria properly [3]. Secondary headache disorders are underdiagnosed [14] even though the incidence of head and neck trauma and meningeal and cerebral infection is high [14, 15].
Cameroon is a SSA country located in central Africa, with a population of 24 million people [16]. The lack of specialized care, with a proportion of 0.01 neurologist per 10,000 inhabitants [17], makes healthcare depend on primary physicians and nurses, with a ratio of 1.9 and 16.0 per 10,000 people, respectively [16]. The World Atlas of Headache Disorders pointed out that worldwide, the most frequently encountered problem is the lack of professional education (34%) and the lack of headache-specific healthcare resources (33%) [9]. To detect the needs and wants of headache care in Cameroon, we analyzed the presence of headache disorders in the clinical practice of a group of healthcare providers (HCP) from Cameroon that attended an intensive course on neurology. We evaluated their general knowledge about classification, diagnosis and management of headache disorders through questionnaires, and repeated the evaluation to measure improvement after the course.
Participants and methods
Subjects
We conducted an interventional study with a prospective cohort design. The target population were a group of Cameroonian HCP, including general practitioners and nurses, both nurse practitioners and nurse assistants. HCP from the whole country (both rural and urban centers) that actively participated in a telemedicine platform in partnership with the Spanish NGO Fundación Recover Hospitales para África were invited. Participants were provided grants covering transport and housing for the course that took place in October 2017. The 4-day intensive course covered the main sub-specialties of neurology. Concerning headache, the teaching program reviewed epidemiology, diagnosis and management of headache disorders. Table 1 summarizes course curriculum. Attendees also participated in two workshops covering fundoscopy and occipital nerve blockade. The total duration of the headache disorders course was 6 h. The study was done in accordance with the Declaration of Helsinki and all the participants agreed and consented to participate.
Questionnaires
Participants provided demographic data including age, gender, professional title, years of training and years in neurology training; as well as epidemiological data on their patient population, based on their personal impression: total number of patients per month, number of headache patients per month, and the most frequent reason for consultation. If patients had been specifically trained in psychology or other specialties but that was not the main specialty, they were classified according to their background training in the analysis.
They also filled out a questionnaire on headache disorders at baseline and after course completion. To be able to analyze local needs and facts, the questionnaire included open questions and in selected cases multiple-choice questions. The full questionnaire is available in Supplementary Materials. We specifically evaluated (a) primary/secondary headache differentiation, (b) primary or secondary headache etiology, (c) presumptive causes of headache, (d) headache red flags (e) complementary tests, (f) symptomatic treatments employed, (g) preventive treatments employed and their duration. Thus, we recorded epidemiological headache data and knowledge regarding classification, diagnosis and treatment of headache disorders in our sample.
Study objectives
With the survey, we recorded if headache was a frequent reason of consult in their clinical practice, in absolute number of patients per week and in comparison, with other sub-specialties of neurology. We evaluated education in headache medicine, testing if participants were aware of the main primary and secondary headache disorders and their etiology. We assessed management and diagnosis, analyzing if participants were familiar with the main red flags and if they considered complementary exams necessary. Finally, we analyzed preferences about symptomatic and preventive treatment. Questions were both multiple-choice and open questions. When applicable, we compared results before the course and after. As exploratory analysis, we compared responses in the group of physicians versus the rest of the sample.
Statistical analyses
We present qualitative data as percentage and frequency, and quantitative variables as mean and standard deviation (SD) or median and Inter-quartile range (IQR) when applicable. Considering the size of our sample and the before and after nature of many comparisons, we employed Fisher exact test or McNemar in the evaluation of qualitative variables; and U-Mann–Whitney or Wilcoxon in the analysis of qualitative and quantitative variables. Statistical analysis was conducted with SPSS v21.0 and statistical level of signification was set to 0.05%, and multiple comparisons were adjusted by Bonferroni method. Sample size was not calculated as the number of participants was defined by the budget, as all participants were granted. Missing data were managed by complete case analysis.
Results
Forty-two healthcare providers participated in the study, 22 of them were women (52.4%), with mean age 36.8 (8.2) years. All participants were the main HCP from their centers. Twenty participants were nurse practitioners (49%), 12 physicians (28%) and 10 nurse assistants (23%). Three patients had psychological training, being two of them nurses and a physician the other one. The median duration of their professional training was 4 years (3–6.5) and median time since the completion of studies was 5 years (3–10). They reported a median of 66 h of neurology training (30–315). Education time was longer in physicians compared with the rest of participants (6.8 vs. 4.5 years, U-Mann–Whitney, p = 0.003).
Headache epidemiology
Participants assisted a median of 240 (130–400) neurological patients per month. Thirty four percent of participants reported that headache disorders were the most frequent neurological condition in their settings, 31% considered epilepsy as the most frequent neurological disorder, 21% selected cerebrovascular diseases and 7% neuromuscular disorders. Mean number of neurological patients seen per week was 69.3 (28) among physicians and 63.0 (42.5) for the rest of participants (U-Mann–Whitney, p = 0.67). Median number of headache patients per week was 20.0 (10–30), without differences between physicians and other HCPs (U-Mann–Whitney p = 0.54).
Primary headache etiology and classification
Concerning knowledge of primary headache disorders at baseline, 15 participants (35.8%) mentioned at least 1 primary headache: migraine (26.2%) and tension-type headache (11.9%). No other primary headache disorders were reported. After the course, 33 participants (78.6%) identified at least one primary headache (Fisher, p = 0.002): migraine (73.8%), tension-type headache (33.3%), cluster headache (9.5%) and trigeminal neuralgia (4.8%). Figure 1 shows the percentage of responders that described all the different causes of headache that were reported by the participants. Figure 2 represents the perceived etiology of primary headache disorders.
Secondary headache classification
When participants were asked to list secondary headache disorders, only 8 participants (19.0%) mentioned at least 1; after the course 17 (40.5%) were able to enumerate them appropriately (Wilcoxon, p = 0.014) (Fig. 2). At the baseline, two participants listed migraine as a secondary headache disorder. Supplementary table 2 summarizes the different secondary headache disorders mentioned by the participants. On the other hand, after the course, 15 participants (35.7%) wrongly listed primary headache disorders as secondary headaches, with cluster headache being the most frequent (9 times), followed by tension-headache (4 times) and migraine (3 times).
Diagnosis, red flags and management
Clinical history was considered sufficient for headache diagnosis only by 24 participants at baseline (57.1%), compared with 33 participants after the course (78.6%), (McNemar, p = 0.50). At baseline, 21 participants (50%) affirmed that neurological examination could be abnormal in primary headache patients, decreasing to 17 participants after the course (40.4%), (McNemar, p = 0.02). Neuroimaging was judged as necessary for headache diagnosis by 14 participants (33.3%) before the course and by 5 (11.9%) afterwards (McNemar, p = 0.02).
Correct red flags for secondary headache diagnosis were mentioned by 6 participants at baseline (14.3%) and 17 after the course (40.5%), (Wilcoxon, p = 0.005). When asked to spontaneously list red flags, the most frequently mentioned was photophobia by six of the participants, followed by vertigo, fever, and intensity, each mentioned by four participants.
Treatment
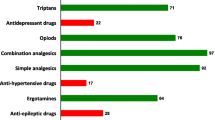
Regarding headache treatment, the preferred symptomatic drugs for migraine were paracetamol and Non-steroidal anti-inflammatory drugs (NSAIDs), for 22 (47.6%) and four (9.5%) participants, respectively; changing to 10 (23.8%) and 28 (66.7%) after the course (McNemar, p = 0.05 and p < 0.001). At baseline, two participants considered amitriptyline a symptomatic treatment and one participant affirmed to use haloperidol for migraine attacks. When asked about preventive treatment, participants mentioned an adequate preventive drug at baseline in 29.6% of the cases, increasing to 74.1% after the course (p = 0.015). Median duration of preventive treatment was 7 days before the course (5–90) and 90 days after the course (75–90) (Wilcoxon, p = 0.05).
Comparison between physicians and the rest of the sample
The only variable that showed statistically significant differences was the correct identification of red flags before the course, which was higher in the physicians’ group (41.7 vs. 10%). The full results are available in the supplementary table 1.
Discussion
Our study showed that headache was the leading neurological reason for consult in daily practice of the participants of the study. Their knowledge about headache types and their etiology was scarce. The concept of red flags and the importance of anamnesis was also very limited. The identification of red flags was incompletely understood after the course. Finally, treatment was mainly based on the use of symptomatic medication and paracetamol was the drug of choice.
Burden of headache disorders is not only related with their high prevalence and associated disability [7, 8], but also with their economic impact. Besides direct costs, the indirect costs due to absenteeism and presenteeism are also relevant in SSA countries [1]. Cost of headache disorders ranges between 1.6 and 1.9% of the total gross domestic product (GDP) in countries like Zambia [18] or Ethiopia [19], proportionally higher than in any other region in the world [5]. In the case of Cameroon, percentage of GDP expended on health was 4.1% in 2014 [20], but there are no data on headache direct and indirect costs.
The first step in headache management is proper diagnosis and classification. In our sample, the concept of primary and secondary headaches was unclear, and few participants knew of migraine or tension-type headaches. There are two possible explanations. Patients with primary headaches rarely consult, around 6.9% in some series [12], as self-treatment with over-the-counter drugs is common practice [10, 21]. Some pharmacy-based studies showed that up to 95% of the patients were directly prescribed in that setting, where only 45% of cases were asked about symptoms and 22% on previous treatments [21].
When asked about secondary headache disorders, the mentioned entities were highly variable, no more than four participants mentioned the same secondary headache and some important causes in the local setting such as headache attributed to systemic infection or headache attributed to cranial vascular disorder [14] were not even mentioned. The red flags listed differed greatly with those generally established [22] and after the course, performance on questions on alarm symptoms and signs was suboptimal. Secondary causes of headache are common in SSA clinical practice [14], and thus secondary headaches may be for HCP as normal as primary headache disorders are for western countries physicians.
On the other hand, the high demand for complementary exams was worth noting. Many participants considered that anamnesis was not enough to make a proper diagnosis even though it is well established that most of headaches can be correctly diagnosed [13]. A significant proportion aimed to have a Cranial tomography (CT) scan performed in every case. In some studies, up to 51.1% of headache patients receive an Electroencephalogram (EEG) [23]. Few participants mentioned funduscopic eye examination or lumbar puncture as possible tests, although they are available in most Cameroonian centers and highly efficient. In the setting of Cameroon, where the cost of a CT scan is one-third of the average wage [17], availability is low, with < 10 CTs in the whole country [17] and quality of imaging and reports are poor, complementary exams should be requested only when patients clearly benefit from them. Thus, the identification of secondary and primary headaches is key to guide the HCP in the request for diagnostic tests.
Pharmacological treatment was another critical point. The concept of prophylactic treatment was completely unclear at baseline, as participants only maintained treatment for a week. Paracetamol was considered the drug of choice for acute treatment, in line with other studies where 66.1–83.8% of subjects were treated with paracetamol, despite its worse efficacy profile compared with NSAIDs [24, 25]. Triptans are not available and their cost is disproportionated compared with paracetamol or NSAIDs.
Availability of oral preventive drugs is scarce in Cameroon and other SSA; however, amitriptyline and propranolol can be found in most of countries, while valproic acid is more variable [14], frequently suffering from stock interruption and irregular supply. Many other effective drugs are not available and some common drugs such as topiramate, flunarizine, metoprolol, duloxetine can seldomly be found. Cameroon is more deprived than other countries in SSA and data about availability and price of essential medicines are not even reported in the World Health Organization database.
Neurological diseases and in particular headache disorders management can be improved by education. On one hand, many diseases are chronic; on the other hand, some of them have a hyper-acute presentation. Educational initiatives can improve identification, diagnosis and treatment done by local healthcare providers [26]. By analyzing which areas were not correctly addressed after the course, we identified the weak points that should be improved in future seminars. Also, we realized that in SSA countries, health services frequently offer non-medical-doctor health personnel. Education programs should be tailored, adapting the teaching content to nurses as well.
Our study addresses a knowledge gap since there are no published data on the prevalence of headache in Cameroon, or on its management. The strengths include the evaluation of the effect, the representative nature of the sample, with HCP coming from varied backgrounds (physicians, nurses and psychologists) and urban and rural centers, as well as the combination of open and multiple-choice questions.
The main limitation to the epidemiological data reported in this study is the potential memory bias that all self-reported questionnaires entail, as HCPs reported epidemiological results based on what they remembered from daily practice. Another important limitation is the small sample size, with a possible selection bias since participants were previously involved in educational activities in a telemedicine platform, so their interest in training and education could be higher than average in the country and, therefore, less representative.
In interpreting the results of the intensive headache course, a test–retest and memory bias should be considered, as participants took the same questionnaire at baseline and at the end of the day. Definitely, future studies should re-administer the questionnaire long time after the teaching course. To this, we aim to keep in touch with participants via online platform education and we plan to do future courses and expand the material free of charge. Retention of information should also be evaluated in the clinical setting, analyzing the impact and change in the management of patients. It would be interesting to administer the questionnaire in other population or in our current settings to compare results. A confounding factor could exist, as the course was done in French and our native language is Spanish, with the subsequent potential risk of miscommunication.
Conclusions
Headache was reported as the most frequent neurological disorder in our sample. Knowledge about primary headache disorders and their etiology was scarce, and the clinical concept of red flags was very limited. The first-choice drug for acute headache was paracetamol and the correct use of preventive treatment, even when sometimes available, was unclear. Education in headache medicine should be a priority in teaching programs in Sub-Saharan Africa due to the high prevalence of headache disorders and the health burden they entail.
Data availability
Datasheets are available for other researchers upon request to the corresponding author.
Abbreviations
- SSA:
-
Sub-Saharan Africa
- HCP:
-
Healthcare provider
- ICHD:
-
The International Classification of Headache Disorders
- SD:
-
Standard deviation
- IQR:
-
Inter quartile range
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- GDP:
-
Gross domestic product
- CT:
-
Cranial tomography
- EEG:
-
Electroencephalogram
References
Mengitsu Takele G, Tekle Haimanot R, Martelletti P (2008) Prevalence and burden of primary headache in Akaki textile mill workers, Ethiopia. J Headache Pain 9:119–128
Stovner LJ, Hagen K, Jensen R et al (2007) The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 27:193–210
Woldeamanuel YW, Cowan RP (2017) Migraine affects 1 in 10 people worldwide featuring recent rise: a systematic review and meta-analysis of community-based studies involving 6 million participants. J Neurol Sci 15(372):307–315
Stovner LJ, Al Jumah M, Birbeck GL et al (2014) The methodology of population surveys of headache prevalence, burden and cost: principles and recommendations from the global campaign against headache. J Headache Pain 15:5
Saylor D, Steiner TJ (2018) The global burden of headache. Semin Neurol 38:182–190
GBD 2016 Headache Collaborators (2016) Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of disease study. Lancet Neurol 2018(17):954–976
Global Burden of Disease Neurology Collaborators (2019) Global, regional, and national burden of neurological disorders; 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 18:459–480
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study. Lancet 2018(392):1789–1858
World Health Organization (2011) Atlas of headache disorders and resources in the world. World Health Organization, Geneva
Ojini FI, Okubadejo NU, Danesi MA (2009) Prevalence and clinical characteristics of headache in medical students of the university of Lagos, Nigeria. Cephalalgia 29(4):472–477
Ofovwe GE, Ofili AN (2010) Prevalence and impact of headache and migraine among secondary school students in Nigeria. Headache 50(10):1570–1575
Birru EM, Abay Z, Abdelwuhab M et al (2016) Management of headache and associated factors among undergraduate medicine and health science students of university of Gondar, north west Ethiopia. J Headache Pain 17:56
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38(1):1–211
Woldeamanuel YW (2017) Headache in resource-limitted settings. Curr Pain Headache Rep 21(12):51
Mengitsu G, Alemayehu S (2013) Prevalence and burden of primary headache disorders among a local community in Addis Ababa, Ethiopia. J Headache Pain 14:30
World Bank (2018) Atlas of sustainable development goals 2018: from world development indicators. World bank atlas. World Bank, Washington, DC
Observatoire de ressources humaines pour la Santé de l’Afrique. Profil en ressources humanitaires pour la santé du Cameroun. Global health workforce alliance. http://www.ressma.com/Documentation/BIBLIO/RESSOURCES%20HUMAINES/RH_cameroon_profile.pdf. Accessed 7 Nov 2019
Mbewe E, Zairemthiama P, Paul R et al (2015) The burden of primary headache disorders in Zambia: national estimates from a population-based door-to-door survey. J Headache Pain 16:513
Zebenigus M, Tekle-Haimanot R, Worku DK et al (2017) The burden of headache disorders in Ethiopia: national estimates from a population-based door-to-door survey. J Headache Pain 18(01):58
Global health observatory. World Health Organization. http://apps.who.int/gho/data/?theme=main. Accessed 7 Nov 2019
Netere AK, Erku DA, Sendekie AK et al (2018) Assessment of community pharmacy professionals’ knowledge and counseling skills achievement towards headache management: a cross-sectional and simulated-client based mixed study. J Headache Pain 19:96
Do T, Remmers A, Schytz HW et al (2019) Red and orange flags for secondary headaches in clinical practice: SNOOP10 list. Neurology 92(3):134–144
Kaputu-Kalala-Malu C, Walker TD, Ntumba-Tshitenge O et al (2016) The challenge of managing headache disorders in a tertiary referral neurology clinic in Rwanda. Neurosciences 21(2):151–157
Birru EM, Abay Z, Abdelwuhab M et al (2016) Management of headache and associated factors among undergraduate medicine and health science students of university of Gondar, north west Ethipia. J Headache Pain 17:56
Onwuekwe I, Onyeka T, Aguwa E et al (2014) Headache prevalence and its characterization amongst hospital workers in Enugu, south east Nigeria. Head Face Med 10:48
Gallagher RM, Alam R, Shah S, Mueller L, Rogers JJ (2005) Headache in medical education: medical schools, neurology and family practice residencies. Headache 45(7):866–873
Acknowledgements
We want to thank Fundación Recover Hospitales para África Non-Governmental Organization for their support and all the participants and attendees of the course.
Funding
The study did not receive any private or public funding.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study design. Material preparation, data and analysis were conducted by MHGM and DG-A. The first draft was written by DG-A. All authors commented the subsequent versions, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare not to have any conflict of interest.
Ethics approval
The study was done in accordance to the Declaration of Helsinki principles. Due to the nature of the study, it was not evaluated by ethics review board.
Consent to participate
All the participants were informed about the study, agreed to participate and signed informed consent forms.
Consent for publication
Both participants and authors agreed on publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
García-Azorín, D., Molina-Sánchez, M., Gómez-Iglesias, P. et al. Headache education and management in Cameroon: a healthcare provider study. Acta Neurol Belg 122, 75–81 (2022). https://doi.org/10.1007/s13760-021-01620-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-021-01620-6