Abstract
Purpose of Review
The purpose of the review is to highlight some of the new findings on phototherapy treatment for psoriasis and present clinical pearls for the practitioner.
Recent Findings
Recent research has helped to further elucidate the molecular mechanisms of UV light in the treatment of psoriasis. New evidence regarding the combination of phototherapy with biologic agents and phototherapy’s effect on quality of life is also highlighted.
Summary
Phototherapy remains an effective and viable option for patients seeking non-invasive and safe treatment of psoriasis. Further research is still needed to understand the exact immunological effects and molecular pathways regarding the response of the skin to UV light. Further research is also needed with combination treatment phototherapy and the newest biologic agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Phototherapy represents one of the oldest treatment modalities in dermatology. Over 3000 years ago, the ancient Egyptians were the first to use natural light in combination with herbal extracts in the treatment of skin disease[1]. Centuries later, the development of phototherapy for psoriasis was based on the observation that sunlight improved the symptoms of the disease. The use of phototherapy has now expanded to treat various other inflammatory and non-inflammatory skin conditions such as eczema, vitiligo, mycosis fungoides, and idiopathic pruritis. The regimen involves short, repeated exposure of the skin to ultraviolet (UV) light at very specific wavelengths. Given its excellent safety profile and non-invasive nature, phototherapy continues to be a preferred treatment by dermatologists[2]. Even though it has been used for many years, research into phototherapy and photomedicine is still in progress. The precise molecular mechanism of action of the skin’s response to UV radiation along with ways to best maximize effectiveness for patients are the two areas of current investigation. The goal of this review article is to present recent advances in phototherapy along with treatment pearls for clinical practice.
Types of Phototherapy
Three main types of phototherapy are used for the treatment of psoriasis: psoralen plus ultraviolet A (PUVA), broadband ultraviolet-B (BB-UVB), and narrowband ultraviolet B (NB-UVB). The associated wavelengths of these modalities are summarized in Table 1.
Traditionally, BB-UVB therapy was the treatment of choice for psoriasis, but in the past years, NB-UVB has surpassed its use due to its increased effectiveness[3]. A 2019 study demonstrated that NB-UVB therapy improves the quality of life in patients with psoriasis, with its beneficial effects lasting for months after the treatment has ceased[4]. Given its ease of use, good safety profile, and wide variety of applications, NB-UVB is the most common phototherapy modality used today[5].
PUVA phototherapy involves treatment with ultraviolet A (UVA) and psoralen, a photosensitizing medication. PUVA can be administered as a topical cream/soak or taken orally in systemic therapy[6]. Topical/soak PUVA allows patients to treat only limited areas of skin such as in palmoplantar psoriasis. Although very effective, PUVA is less readily available as compared with NB-UVB. The toxicity of systemic PUVA including photoaging and increased risk of non-melanoma skin cancer in the long term also limits its use.
Recent Advances
The Immunoregulatory Mechanisms of Phototherapy
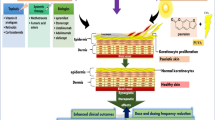
The pathophysiology of psoriasis is a complex cascade of aberrant signaling and cellular interactions leading to excessive activation of the immune system. Specifically, this disproportionate activation leads to immune responses in the T helper cell type 1 (Th1)/T helper cell type 17 (Th17) pathways. Th1/Th17 activation leads to the secretion of TNF-alpha, IL-12, IL-17, and IL-23—the key mediators of inflammation involved in the pathogenesis of psoriasis. These cytokines lead to downstream proliferation of keratinocytes, increased expression of angiogenic mediators and endothelial adhesion molecules, and infiltration of immune cells into the skin lesions[7].
Phototherapy directly combats psoriasis through multiple mechanisms. It modifies the inflammatory pathway, shifting the immune response from the Th1/Th17 pathway towards the opposite Th2 pathway[8]. This reduces key proinflammatory cytokines, including IL-12, IL-17, IL-20, IL-22, and IL-23[9]. Locally, UV light also causes apoptosis of keratinocytes and T cells in the epidermis and dermis, promotes migration of Langerhans cells out of the epidermis, and decreases histamine release and mast cell degranulation[10,11,12]. In combination, these changes support epidermal remodeling and histological normalization of psoriatic skin.
UVB
Recent research has dived further into the specific cellular pathways and cytokines that are affected by UVB treatment such as the functionality of regulatory T cells (Tregs). Typically, Tregs are key suppressors of the autoimmune response[13•]. In the pathogenic state of psorasis, Treg cells hold the potential to perpetuate this proinflammatory disease state by differentiating into Th17 cells. The greater levels of IL-17A seen in severe psoriasis have recently been shown to result from the increased propensity of Tregs to convert into IL-17A producing Th17 cells through the loss of forkhead box p3 (Foxp3) 20[14]. Because UVB increases Foxp3-positive Treg cells in psoriatic skin lesions, it improves Treg cell stability and reduces pro-inflammatory Th1/Th17 cytokines in psoriasis[15].
Additionally, an isoform of Protein Kinase C (PKCε) has recently been shown to be a mediator of Th-17 cell differentiation, which aids in the progression of psoriasis. Overexpression of PKCε was noted in the circulating CD4+-T cells of psoriasis patients. Following NB-UVB phototherapy, a decrease was noted in the amount of PKCε expressed within CD4+-T cells in peripheral blood, which correlated with disease severity before and after treatment. This research identifies PKCε’s role as a potential biomarker of treatment response to UVB therapy[16•].
UVA
New research has helped elucidate the exact mechanism of how PUVA contributes to cell death of keratinocytes in hyperprolific psoriatic plaques. Studies suggest that the mechanism of apoptosis is multifactorial. Prior research noted that PUVA creates UV-induced photoadducts, which inhibit cell proliferation[17]. More recently, PUVA was found to also induce the innate immune sensor retinoic acid inducible gene 1 (RIG-1), which leads to tumor protein p53 (p53) activation, ultimately inducing apoptosis[18, 19•]. Expanding our understanding of this signaling pathway identifies RIG-1 or p53 as potential therapeutic targets in psoriasis.
Home Phototherapy
Many patients find phototherapy treatment inconvenient and burdensome given the frequency of visits, transportation issues, and high insurance co-pays.[20] Patients need as many as 3 treatment sessions per week, and even though a typical NB-UVB phototherapy session lasts only 15 min, transportation, parking, and office wait times may require the patient to commit several hours for one treatment session.
To address these issues, home phototherapy units have been developed and popularized. A Swedish study from 1979 was the first to report the efficacy and practicality of home phototherapy. This study showed that out of the 28 patients utilizing the home phototherapy units, 20 patients had complete clearance and 6 patients showed marked clinical improvement. Although the number of treatments to complete clearance varied, the median amount of time to achieve healing was 45 treatments or 6 ½ weeks of therapy[21]. While the effectiveness of home phototherapy for psoriasis has been documented for many years, a randomized controlled study in 2009 showed equal efficacy and no increased safety risks associated with home treatment when compared with outpatient phototherapy[22]. Additionally, home phototherapy was associated with a lower burden of treatment and increased patient satisfaction, making it a very popular treatment option for patients[22].
More recently, smaller and more convenient machines are being designed to make home therapy more convenient and efficient. New devices have been modified to be handheld as opposed to the bulkier, older counterparts. Not only are these handheld devices useful for recalcitrant localized psoriatic plaques, but they also offer a practical means of enhancing NB-UVB exposure to the scalp. This is important as the scalp represents one of the most difficult areas of the body to treat effectively. One such example, the Clarify home phototherapy device, is a handheld device allowing for targeted treatment with NB-UVB phototherapy. The device is coupled to a smartphone application, allowing physicians to control and monitor treatments, and incorporates built-in reminders and scheduling for patients, improving adherence to treatment[23]. Ultimately, these home phototherapy units allow patients to target and treat recalcitrant and difficult-to-reach disease areas in the comfort of the their home, without losing the efficacy of clinic-based phototherapy.
Phototherapy and Biologic Agents: Combination Therapy for Recalcitrant Psoriasis
Despite the fact that multiple new biologic agents have shown excellent efficacy and safety, phototherapy still plays an important role in a cohort of patients with severe and treatment-resistant disease. These complex patients may require phototherapy in addition to biologic therapy. For example, several studies have exhibited the efficacy of using etanercept and NB-UVB in combination[24, 25]. These studies evaluated this combination therapy in patients who had not previously received treatment, had a poor response with etanercept alone, or had a poor response to NB-UVB alone. Overall, combination therapy was superior in efficacy and led to a reduction in the amount of time to clearance of psoriatic disease. A recent review article summarized the evidence for the combination of etanercept and NB-UVB phototherapy and graded it as B on the Grading for Recommendation and Evidence by Robinson et al. The combination of adalimumab and phototherapy was given the same designation of evidence as level B, while combination of ustekinumab and phototherapy was rated as level C for level of evidence[26].
Another recent review article evaluated the use of a combination of a biologics (e.g., etanercept, adalimumab, infliximab, ustekinumab) and phototherapy for the treatment of moderate-to-severe psoriasis through 2016. Researchers found that 9 out of 10 studies examined demonstrated favorable efficacy and safety of combination therapy, although the degrees of therapeutic enhancement varied[27]. The benefits of combination therapy were demonstrated across many different study designs, which suggests that combining a biologic with phototherapy is reasonable when efficacy of either therapy alone is inadequate. Recent data from the PSONET registry reviewed nearly 10,000 patients on biologic treatment and about 1000 patients were identified as receiving combination treatment. While infrequently used, UVB phototherapy plus biologics was the second most common combination treatment identified in the study.[28]
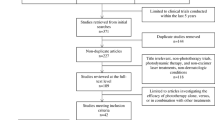
Cutaneous Malignancy Risk of UVB and PUVA Phototherapy
It is well known UVA and UVB from natural sunlight is carcinogenic. Therefore, the risk of skin malignancy from phototherapy is often questioned by patients and providers alike. Over the last several decades, many articles have been published investigating this potential concern. One of the most recent, and comprehensive, reviews of this subject was published in 2015 and assessed the cutaneous malignancy risks of NB-UVB, BB-UVB, and PUVA in all skin types including both Caucasian and non-Caucasian patients[29].
The authors found, after reviewing 61 original articles from 1980 to 2015, that the only conclusive evidence regarding cutaneous malignancy was an increased risk of squamous cell carcinoma with systemic PUVA in Caucasian patients above a threshold of 250 treatments. Risk of melanoma with systemic PUVA in Caucasians was uncertain due to conflicting results so caution is advised. In both Caucasian and non-Caucasian patients, UVB phototherapy (irrespective of UVB type[30]) does not increase the risk of cutaneous malignancy. More studies are still warranted, however, to further confirm the long-term safety of phototherapy.
Conclusions
Phototherapy is a useful and adaptable tool for the dermatologist who treats psoriasis and other inflammatory skin diseases. Research on the exact mechanisms of phototherapy is ongoing, but recent data suggests phototherapy can alter both the dysfunctional pathway and downstream effects that lead to hyperkeratotic psoriatic plaques. Home phototherapy devices also respresent a more convenient, time-efficient option for psoriasis treatment. Despite greater efficacy of the newest biologic agents, phototherapy still maintains one of the best safety profiles of any treatment, given its non-invasive nature. Also, combining phototherapy with biologic agents serves as a useful treatment option for patients with resistant disease. Given these reasons above, phototherapy should be considered and discussed for every patient who presents for treatment of psoriasis.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Racz E, Prens EP. Phototherapy and photochemotherapy for psoriasis. Dermatol Clin. 2015;33(1):79–89. https://doi.org/10.1016/j.det.2014.09.007.
Joy Wan, Katrina Abuabara, Andrea B. Troxel, Daniel B. Shin, Abby S. Van Voorhees, Bruce F. Bebo Jr., et al. Dermatologist preferences for first-line therapy of moderate to severe psoriasis in healthy adult patients. Journal of the American Academy of Dermatology, Volume 66, Issue 3, 376 - 386. https://doi.org/10.1016/j.jaad.2011.03.012
Zhang P, Wu MX. A clinical review of phototherapy for psoriasis. Lasers Med Sci. 2018;33(1):173–80. https://doi.org/10.1007/s10103-017-2360-1.
Väkevä L, Niemelä S, Lauha M, Pasternack R, Hannuksela-Svahn A, Hjerppe A, et al. Narrowband ultraviolet B phototherapy improves quality of life of psoriasis and atopic dermatitis patients up to 3 months: results from an observational multicenter study. Photodermatol Photoimmunol Photomed. 2019;35(5):332–8. https://doi.org/10.1111/phpp.12479.
Hönigsmann H. Phototherapy for psoriasis. Clin Exp Dermatol. 2001;26(4):343–50. https://doi.org/10.1046/j.1365-2230.2001.00828.x.
Stern RS. Psoralen and ultraviolet a light therapy for psoriasis. N Engl J Med. 2007;357(7):682–90. https://doi.org/10.1056/NEJMct072317.
Nestle FO, Kaplan DH, Barker J. Psoriasis. N Engl J Med. 2009;361(5):496–509. https://doi.org/10.1056/NEJMra0804595.
Enk CD, Sredni D, Blauvelt A, Katz SI. Induction of IL-10 gene expression in human keratinocytes by UVB exposure in vivo and in vitro. J Immunol. 1995;154(9):4851–6.
Johnson-Huang LM, Suárez-Fariñas M, Sullivan-Whalen M, Gilleaudeau P, Krueger JG, Lowes MA. Effective narrow-band UVB radiation therapy suppresses the IL-23/IL-17 axis in normalized psoriasis plaques. J Invest Dermatol. 2010;130(11):2654–63. https://doi.org/10.1038/jid.2010.166.
DeSilva B, McKenzie RC, Hunter JAA, Norval M. Local effects of TL01 phototherapy in psoriasis. Photodermatol Photoimmunol Photomed. 2008;24(5):268–9. https://doi.org/10.1111/j.1600-0781.2008.00366.x.
Weatherhead SC, Farr PM, Jamieson D, Hallinan JS, Lloyd JJ, Wipat A, et al. Keratinocyte apoptosis in epidermal remodeling and clearance of psoriasis induced by UV radiation. J Invest Dermatol. 2011;131(9):1916–26. https://doi.org/10.1038/jid.2011.134.
Danno K, Toda K, Horio T. Ultraviolet-B radiation suppresses mast cell degranulation induced by compound 48/80. J Invest Dermatol. 1986;87(6):775–8. https://doi.org/10.1111/1523-1747.ep12458843.
• Nussbaum L, Chen YL, Ogg GS. Role of regulatory T cells in psoriasis pathogenesis and treatment. British Journal of Dermatology. 2020. https://doi.org/10.1111/bjd.19380In this review, the authors discuss recent insights into Tregs in the setting of psoriasis with an emphasis on the effect of current treatments on Tregs and how already available therapeutics that modulate Treg frequency or functionality could be exploited for treatment of psoriasis.
Bovenschen HJ, van de Kerkhof PC, van Erp PE, Woestenenk R, Joosten I, Koenen HJPM. Foxp3+ regulatory T cells of psoriasis patients easily differentiate into IL-17A-producing cells and are found in Lesional skin. J Invest Dermatol. 2011;131(9):1853–60. https://doi.org/10.1038/jid.2011.139.
Zhang D, Chen Y, Chen L, Yang R, Wang L, Liu W, et al. Ultraviolet irradiation promotes FOXP3 transcription via p53 in psoriasis. Exp Dermatol. 2016;25(7):513–8. https://doi.org/10.1111/exd.12942.
• Martini S, Pozzi G, Carubbi C, et al. PKCε promotes human Th17 differentiation: Implications in the pathophysiology of psoriasis. European Journal of Immunology. 2018;48(4):644–54. https://doi.org/10.1002/eji.201747102In this study, the authors provide a novel insight into the molecular mechanisms of Th17 cell polarization that is known to play a crucial role in autoimmunity, pinpointing PKCε as a potential target in Th17-mediated diseases.
Lüftl M, Röcken M, Plewig G, Degitz K. PUVA inhibits DNA replication, but not gene transcription at nonlethal dosages. J Investig Dermatol. 1998;111(3):399–405. https://doi.org/10.1046/j.1523-1747.1998.00316.x.
El-Domyati M, Moftah NH, Nasif GA, Abdel-Wahab HM, Barakat MT, Abdel-Aziz RT. Evaluation of apoptosis regulatory proteins in response to PUVA therapy for psoriasis. Photodermatol Photoimmunol Photomed. 2013;29(1):18–26. https://doi.org/10.1111/phpp.12012.
• Chowdhari S, Saini N. Gene expression profiling reveals the role of RIG1 like receptor signaling in p53 dependent apoptosis induced by PUVA in keratinocytes. Cellular Signalling. 2016;28(1):25–33. https://doi.org/10.1016/j.cellsig.2015.10.015This study highlights a potential novel mechanism of action of PUVA photochemotherapy treatment providing a possible new strategy for targeting proapoptotic function of RIG-1, a regulator of innate immune response or p53 for psoriasis therapy.
Rajpara AN, O’Neill JL, Nolan BV, Yentzer BA, Feldman SR. Review of home phototherapy. Dermatol Online J. 2010;16(12):2.
Larkö O, Swanbeck G. Home solarium treatment of psoriasis. Br J Dermatol. 1979;101(1):13–6. https://doi.org/10.1111/j.1365-2133.1979.tb15286.x.
Koek MBG, Buskens E, van Weelden H, Steegmans PHA, Bruijnzeel-Koomen CAFM, Sigurdsson V. Home versus outpatient ultraviolet B phototherapy for mild to severe psoriasis: pragmatic multicentre randomised controlled non-inferiority trial (PLUTO study). BMJ. 2009;338:b1542. https://doi.org/10.1136/bmj.b1542.
Cline A, Unrue EL, Collins A, Feldman SR. Adherence to a novel home phototherapy system with integrated features. Dermatology Online Journal. 2019;25(3) https://escholarship.org/uc/item/1rw9f75h.
Kircik L, Bagel J, Korman N, Menter A, Elmets CA, Koo J, et al. Utilization of narrow-band ultraviolet light B therapy and etanercept for the treatment of psoriasis (UNITE): efficacy, safety, and patient-reported outcomes. J Drugs Dermatol. 2008;7(3):245–53.
De Simone C, D’Agostino M, Capizzi R, Capponi A, Venier A, Caldarola G. Combined treatment with etanercept 50 mg once weekly and narrow-band ultraviolet B phototherapy in chronic plaque psoriasis. Eur J Dermatol. 2011;21(4):568–72. https://doi.org/10.1684/ejd.2011.1330.
Armstrong AW, Bagel J, Voorhees ASV, Robertson AD, Yamauchi PS. Combining biologic therapies with other systemic treatments in psoriasis: evidence-based, best-practice recommendations from the medical Board of the National Psoriasis Foundation. JAMA Dermatol. 2015;151(4):432–8. https://doi.org/10.1001/jamadermatol.2014.3456.
Farahnik B, Patel V, Beroukhim K, Hao Zhu T, Abrouk M, Nakamura M, et al. Combining biologic and phototherapy treatments for psoriasis: safety, efficacy, and patient acceptability. Psoriasis (Auckl). 2016;6:105–11. https://doi.org/10.2147/PTT.S98952.
Busard CI, Cohen AD, Wolf P, Gkalpakiotis S, Cazzaniga S, Stern RS, et al. Biologics combined with conventional systemic agents or phototherapy for the treatment of psoriasis: real-life data from PSONET registries. J Eur Acad Dermatol Venereol. 2018;32(2):245–53. https://doi.org/10.1111/jdv.14583.
Cutaneous Carcinogenic Risk of Phototherapy: An Updated Comprehensive Review - Erica Wang, Jodie Sasaki, Mio Nakamura, John Koo, 2015. . https://doi.org/10.1177/247553031500100107?journalCode=jpsa
Osmancevic A, Gillstedt M, Wennberg A-M, Larkö O. The risk of skin cancer in psoriasis patients treated with UVB therapy. Acta Derm Venereol. 2014;94(4):425–30. https://doi.org/10.2340/00015555-175313.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Psoriasis
Rights and permissions
About this article
Cite this article
Brownstone, N., Mosca, M., Hong, J. et al. Phototherapy for Psoriasis: New Research and Insights. Curr Derm Rep 10, 16–20 (2021). https://doi.org/10.1007/s13671-020-00324-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13671-020-00324-z