Abstract
Purpose of Review
The purpose of this literature review is to appraise the current research surrounding the impact of mobility for geriatric patients presenting with orthopedic conditions in the acute care setting.
Recent Findings
A literature search in the PubMed database yielded 53 results which underwent a title and abstract screening to reveal a total of 22 articles eligible for full-text review. Two authors screened each article and a third author was responsible for reconciling any conflicts. Following the full-text screen, 10 total articles were extracted and evaluated to determine what the current literature has concluded about the impact of mobilization for geriatric patients with orthopedic conditions in the acute care setting. Studies are inconsistent in their dosage parameters of mobility for geriatric orthopedic patients and range in initiating protocols 6 to 24 h following surgery. Protocols and activity standards vary from 1.8 to 8.3 METs, 0 to 1000 steps per day, 15 min walks, or a 5-day mobility protocol focused on functional and strengthening activities. Studies range in reported length of stay (LOS) but infer that the earlier mobility is initiated the risk of prolonged LOS is decreased. Finally, studies report greater success with mobility protocols when multiple disciplines are educated and involved in implementation.
Summary
Despite the limitations of this study and existing literature, it is clear that integrating mobility within the first 24 h following the injury or surgical intervention does not produce additional adverse effects or increase pain intensity. This review suggests that emphasizing interprofessional collaboration when implementing a mobility protocol is vital to the success and safety of patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mobilization of patients in the hospital is a factor in short-term and long-term functional outcomes, length of stay (LOS), discharge recommendations, and hospital readmission rates. Immobility during hospitalization is widely recognized as a contributor of deconditioning, functional loss, and increased demand for transition to sub-acute care facilities [1]. Evidence has emerged supporting increasing the amount of physical activity performed by patients in the hospital to reduce the risk for adverse events and prevent functional decline. Early rehabilitation can optimize patient management, allowing early discharge from the acute ward and reducing risk of hospital-acquired complications like hospital-acquired infections and thromboembolic events [2•]. The amount of physical activity performed postoperatively negatively correlates with the LOS in the hospital [3]. Additionally, ambulatory status is a fundamental factor in management of the postoperative surgical inpatient and has been linked to positive outcomes in reducing deep venous thromboembolisms (DVT), cost of care, and LOS [4•]. Mobility in this review is defined by the authors as any form of activity or exercise in which the patient provides effort in movement within the first 24 h of admission in the acute care setting, meaning that passive mobility by hospital staff is not consistent with this definition.
Total joint arthroplasty (TJA) surgeries and fractures are among some of the most common reasons for hospitalization for older adults today. The rates of TJA of the hip and knee have increased in North America over the last decade [5]. Additionally, falls often account for many injuries in older adults. An estimated 1.64 million older adults were treated in emergency departments for unintentional fall injuries, with fractures, contusions, and lacerations accounting for greater than three quarters of all injuries [6]. The number of fractures among older adults continues to be a concern in coming years. In fact, the number of hip fractures is projected to be 289,000 in 2030 [7]. The orthopedic conditions that bring older adults into the hospital often have mobility considerations (weight bearing status, pain, strength, range of motion (ROM) limitations, immobilization of a specific body region) regarding LOS and the achievement of functional outcomes with recovery. There is a lack of consensus among research on the impact mobility has on older adults with orthopedic conditions in the hospital regarding their functional outcomes [8]. Therefore, the primary aim of this paper is to review and summarize the current literature about the impact of mobilization for geriatric patients with orthopedic conditions in the hospital setting.
Methods
A literature search was carried out using the PubMed search engine between April 10, 2015 and April 10, 2020. The following search algorithm was used to gain a broad spectrum of evidence surrounding mobility interventions for the geriatric population recovering from orthopedic conditions in the acute care setting: ((((Exercis* OR Ambulat* OR mobil*)) AND (“acute care” OR “inpatient”))) AND (Geriatric OR Elderly OR “Older Adults”)) AND (Orthopedics OR “Orthopedic Surgery” OR Joint Arthroplasty OR Fracture). The exclusion criteria included non-human subjects, articles without a free full-text available, and any setting other than acute care. The inclusion criteria included older adult population defined by mean age greater than 50 years old, an orthopedic diagnosis or surgery, and an intervention of active mobility in the acute care setting. Level of evidence for included articles was appraised and established by the Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence criteria [9].
Results
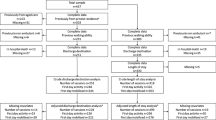
The search strategy resulted in 53 articles eligible for a title and abstract screening. Following the title and abstract review, 31 articles were excluded and 22 articles were moved into a full-text screening for further examination of inclusion and exclusion criteria. In each phase, the article eligibility was reviewed by two authors and any conflict in the screening process was resolved by a third author. The full-text review phase resulted in 10 articles eligible for inclusion in this review which is seen in Fig. 1. Upon the final appraisal of articles, an additional two articles were excluded from this review. One article by Asplin et al. was excluded due to the setting of a Comprehensive Geriatric Care (CGC) unit resembling an inpatient rehabilitation model of care which was missed during the initial rounds of excluding articles [10]. Another article written by Soeters et al. was excluded due to the lack of mobility intervention following the surgical intervention and instead focused on education prior to surgery which does not fit the inclusion criteria [11]. All authors collaborated and agreed on the final articles in this review, which were all appraised to be Level II–III evidence.
Following a complete review of all studies seen in Table 1, the authors established recurring themes in which articles could be categorized and grouped together to establish a consensus in the evidence. The following themes emerged in the review: dosage of mobility, interdisciplinary collaboration, and length of stay (LOS) related to mobility in acute care.
Dosage of Mobility
Despite the common occurrence of orthopedic surgeries, there is no consensus in existing evidence regarding optimal dosage of rehabilitative mobility in the early stages of recovery to maximize function and participation. Many studies included in this review examined various rehabilitative regimens following common orthopedic surgeries to examine their effectiveness in making gains across the various components of the International Classification of Functioning, Disability, and Health (ICF) model.
A total knee arthroplasty (TKA) is one of the most commonly performed orthopedic surgeries in response to severe osteoarthritis to relieve pain and restore function [2•, 12•]. Mobility guidelines following this surgical procedure have changed over the years in response to the evolving procedure itself involving more technology and less invasive techniques. In an observational study published in 2017 by Lisi et al., a sample of 215 TKA patients underwent a rehabilitation protocol within 24 h after surgery including continuous passive motion, active ankle ROM, and isometrics that progressed quickly to functional bed mobility and ambulation tasks as tolerated and appropriate [2•]. The exact dosage of these exercises was not provided but the protocol progressed over 5 days following the day of surgery with an average time of 2.3 (SD = 0.7) days to reach sitting position, 2.6 (SD = 1.0) to reach standing, and 2.9 (SD = 1.0) to achieve walking with assistance [2•]. Additionally, this study observed pain intensity was not increased and the pain intensity continued to decrease following the day of surgery despite progression of mobility protocol [2•]. Knowing mobility and exercise have been found to have analgesic effects and greater functional gains following TKA, another study done by Zietek et al. sought to understand if adding two 15-min walks at least 3 h apart beginning 6 h following surgery would be more advantageous than one 15-min walk on the day of surgery [12•]. Sixty-three patients recovering from a TKA received intensive muscle strengthening, isometric and ROM exercises, and functional activities and were then randomly assigned to receive either two 15-min walks or one 15-min walk on the day of surgery [12•]. The results suggested adding the additional walk did not increase pain at rest (p = 0.83) or while walking (p = 0.68) but it also did not facilitate any greater functional improvement (p = 0.42) shown by similar scores on the Knee Society Function score and visual analog scale (VAS) for both groups [12•]. Despite the lack of change between the intervention and control group in this study, there were limitations to note including the lack of neuromuscular electrical stimulation (NMES) that is a standard implementation in both early rehabilitation and standard rehabilitation following TKA surgery [12•].
Due to the ever-changing environment in the hospital, measuring and quantifying dosage of mobility in acute care is often a barrier to implementing standardized protocols. A recent study published in 2019 by Daskivich et al. provided wearable activity monitors to 100 patients recovering from various surgical procedures including total hip arthroplasty (THA) to attempt to measure step counts, assess the accuracy of physician assessment and ordering of ambulation status, and quantify the association of step counts with LOS [4•]. Patients recovering from THA comprised 15% of the total subjects in this study with the remaining subjects recovering from more gastrointestinal surgical interventions; yet, the findings are beneficial and should be considered for all patients recovering from orthopedic interventions [4•]. This study found there was a statistically significant increase in daily step count with successive postoperative days in aggregate and across individual operations [4•]. Those with an ambulation order of “ambulate with assistance” were more likely to take a higher number of steps each day compared to the orders of “out of bed to chair” which is to be suspected [4•]. The dosage of mobility in this study that indicated lower odds of prolonged LOS (p = .003) was 1000 steps a day, but there was no further decrease in odds after 1000 steps [4•]. This study provides insight into the need for wearable activity monitors in the acute care setting in order to improve the accuracy of daily step count over vague assumptions in their level of mobility to better identify patients at risk for poor efficiency outcomes [4•].
Another common orthopedic injury is a vertebral compression fracture (VCF) due to the higher incidence of osteoporosis in the geriatric population [13•]. Katoka et al. sought to measure early physical activity time (EPAT) and investigate these effects on pain following acute VCFs and recovery of the ability to perform ADLs [13•]. Using activity monitors during the acute phase of this injury, the authors retrospectively divided 69 patients into a standardized group or EPAT group based on their median EPAT. The groups were different at baseline in their motor Functional Independence Measure (mFIM) score, Barthel Index (BI) score, and time required to complete the Trial Making Test Part A (TMT-A) with the sedentary group performing worse at baseline but patient reported pain intensity at rest was not different between the groups at baseline [13•]. The results of this observational study found the completion times for TMT-A (p = 0.019), mFIM (p < 0.001) scores at baseline, and relative functional gains of mFIM from baseline to week 2 or 4 were significantly associated with EPAT [13•]. Additionally, pain at rest and during standing and walking were not significantly different between the groups at week 2 and 4 (p = 0.116) [13•]. Katoka et al. defined their mobility as activity 1.8 to 8.3 METs which includes a range of light to high intensity activities, but there were no reports on specific activities performed and frequency of activities throughout the day [13•].
Interdisciplinary Collaboration
A number of studies incorporated interdisciplinary collaboration in the hospital to provide care and improve functional outcomes for patients with orthopedic conditions. Although physical therapy and occupational therapy are commonly the main disciplines involved in mobilizing patients in the hospital, other disciplines can play a key role in improving functional outcomes for patients by facilitating activities to increase a patient’s mobility. Nursing staff, in particular, often spend increased time with patients compared to other disciplines and can facilitate mobilization activities within their scope of practice.
A study by Resnick et al., assessed the feasibility and efficacy of Function-Focused Care in Acute Care (FFC-AC) for orthopedic trauma patients. FCC-AC addresses many of the barriers that prevent physical activity for patients in the hospital by establishing motivational interventions to change beliefs and incorporate physical activity into routine care [14•]. This model includes activities such as nurses engaging patients in bed mobility during care so the patient performs the movement with cueing rather than passively moving the patient, facilitating performance of ADLs, and ambulating patients to the bathroom or in the hallway and engaging families to do likewise when appropriate. FCC-AC in this study was coordinated and implemented by a Research Function-Focused Care Nurse who implemented the three components of FCC-AC: (1) education of nurses, (2) environmental and policy assessments, and (3) ongoing training and motivation of nurses [14•]. Outcome measures used to assess function, performance and physical activity were measured using the Physical Performance and Mobility Examination, The Physical Activity Survey, and FFC Behavior Checklist for Patients and Actigraphy. Pain was assessed by a verbal report of pain (yes or no) and the patient’s description of the pain intensity using the Pain Verbal Descriptor Scale [14•]. At discharge, there were no significant differences between groups with regard to function (p = .14) or verbal reports of time spent in mobility (p = .13); however, physical activity at discharge showed a trend toward the treatment group spending more time in overall counts of activity based on 24 h recording of Actigraphy [14•]. At 30 days post discharge, there was a greater improvement in function (p = 0.04) and physical resilience (p = 0.04) among those in the treatment versus control group, and no differences were found between the groups regarding having pain or intensity of pain [14•]. This suggests implementation of the FCC-AC can improve functional status for patients after being discharged from the hospital. Additionally, the findings of this study suggest working with nursing staff to engage patients in physical activity during the acute care stay may help patients’ maintain function and engage in physical activity [14•].
When considering the discharge recommendations to the next level of care, a patient’s physical function is an important component for all providers to be aware of. Physical therapists in the hospital make discharge recommendations regarding the maintenance of patient safety, the assistance required for mobility, and the use of assistive devices. These recommendations help drive the continued progress toward the desired functional outcomes for patients upon discharge from the hospital; therefore, providers at the next level of care should take these recommendations into consideration when providing care to these patients. A study by Polnaszek et al. evaluated the omission of physical therapy recommendations for high-risk patients transitioning from the hospital to sub-acute care facilities [15•]. The results of the study found that omission of recommendations for patient safety restrictions/precautions occurred in 54% (316/584) patients, for level of assistance with sitting to standing in greater than 99% (535/537) of patients, and for medical assistive devices in 77% (409/532) patients [15•]. Additionally, Medicare beneficiaries with such omissions demonstrated a trend toward more negative 30-day outcomes as compared to those without patient safety restriction/precaution omissions (26% versus 18%; p = .10) [15•]. These findings show the alarming rate at which PT recommendations are omitted from the patient’s discharge summary and suggest the omission of PT recommendations leads to more negative outcomes following discharge from the hospital. This reiterates the importance of interdisciplinary collaboration between levels of care regarding the improvement of functional outcomes for patients.
Length of Stay
Reducing LOS in the hospital has been a main focus of many programs recently due to the ability to reduce overall cost to the hospital and the patients, as well as reducing the risk for hospital-acquired infections. Despite this claim, few studies are able to report parameters of mobility or functional milestone goals that translate to a shorter LOS, especially for the geriatric population recovering from an orthopedic condition. This review looked at recent studies and how they were able to relate their mobility interventions to the LOS if it was reported.
The study mentioned previously by Lisi et al. initiated their post TKA protocol within 24 h after surgery and continued to progress mobility tasks over 5 days and observed the average LOS to be 4.6 days (SD = 1.8) [2•]. This LOS was found to be comparable to existing evidence regarding LOS for fast-track rehabilitation programs following a TKA [2•, 16]. Despite the claim to reduce LOS, this study did not report on frequency, intensity, or duration of the exercises which makes the results hard to draw conclusions from [2•]. Another study mentioned by Daskivich et al. monitored activity level of individuals recovering from major surgeries using daily step counts and ambulation orders by physicians [4•]. This study found patients who engaged in 0 to 1000 steps a day including postoperative day 1 were associated with a lower probability of a prolonged LOS, but any steps above 1000 did not further impact predicted LOS [4•]. Daskivich also reported that for every 100 steps taken, a 3.7% reduction of an operation specific prolonged LOS was achieved (p = 0.003) [4•]. This study gives insight into specific dosage of mobility parameters when implementing early mobility, but is limited in generalization to the geriatric orthopedic population due to only 15% of the participants recovering from an orthopedic condition in this study [4•].
In the same capacity that mobility has reduced LOS following orthopedic surgical interventions, the newer advances and minimally invasive techniques have also played a role in decreasing LOS and even moving these interventions into a same day surgery category. Due to the lack of high-quality research regarding the effectiveness of same day surgery compared to an overnight stay in the hospital, Goyal et al. sought to understand if patients undergoing a THA had differences in postoperative pain, complications, readmission rates, and relative work effort from the office staff depending on if their discharge happened within 12 h after surgery or stayed in the hospital at least one night [17•]. What this study found was individuals who were discharged on the same day had higher VAS of pain than inpatients (p = 0.005) with no differences in readmission rates, complications, or burden to the outpatient staff [17•]. Another study done by Gromov et al. was also interested in discharging the same day of surgery and utilized specific criteria including < 500 mL of blood loss, received instruction from a PT and is safely instructed in mobility, has pain < 3 while resting and < 5 during activity, and has support at home for 24 h following discharge [18•]. The patients eligible also had to reach functional milestones prior to discharge including independent dressing, bed mobility, sit to stand transfers, and personal care as well as able to ambulate > 70 m with an assistive device [18•]. The patients eligible for discharging the hospital on the same day are automatically getting a more intense dosage of mobility immediately following their surgery in order to discharge within 12 h. This study reported that the readmission rates in these patients were similar to matched patients with at least one overnight stay, indicating there may not be safety issues with same-day discharge pending all criteria are met [18•]. In addition, this article draws attention to the need for facilities to have the ability to remain overnight pending the discharge criteria are not met to ensure safety and an appropriate progression of mobility and functional tasks are met prior to returning home [18•].
Discussion
Based on the review of the most current literature, it is clear evidence remains to be emerging and inconsistent regarding the development of standardized mobility protocols, specifically for the geriatric population recovering from orthopedic conditions and surgical interventions. The majority of available evidence and current standard of practice suggest mobility in the acute care setting is beneficial for prophylaxis of deep venous thrombosis (DVT) occurrence, decreasing risk of postoperative infections, reducing LOS and subsequently cost to both patients and hospital systems, and accelerating functional return [1, 2•, 3, 4•]. Additionally, patients in the hospital have a decreased risk for medical complications, including prosthetic infections and DVT, when a rehabilitation program is started within 2 weeks after TKA surgery, which concludes that timing of rehabilitation is a factor affecting TKA complications [19].
This review is unable to suggest an exact mobility protocol for the geriatric orthopedic population and there is a need for more evidence for guidelines to exist. Evidence in this review suggests that by implementing mobility protocols following a TKA within the first 24 h following surgery and as soon as 6 h after surgery, there are advantages in facilitating return to functional tasks within their short LOS averaging 4 days [2•, 12•]. Studies in this review also mention that mobility may only be beneficial up to a certain dosage before the advantages plateau. Zietek et al. found that an additional 15-min walk to their standard protocol with an existing 15-min walk did not impact pain or return to function. Daskivich et al. found walking 0 to 1000 steps a day including the day of surgery can decrease the LOS, but walking greater than 1000 steps does not reduce the LOS any further [4•, 12•]. Another factor to consider is the discharge time frame and if the discharge is occurring on the same day, the mobility and functional milestones that must be performed safely on the same day of surgery are much more advanced than an individual would receive with a pending 4-day stay in the hospital for recovery. Same-day surgery discharges are becoming more popular and if patients are eligible with certain criteria following the surgical intervention primarily for THA and TKA, they are experiencing the same recovery timeline as those hospitalized longer and have a reduced cost [17•, 18•]. Another inconsistency in the studies included in this review is how dosage is recorded and implemented, making the results harder to generalize to the population in question. One study found implementing mobility activities requiring 1.8 to 8.3 METs measured by an activity monitor was significant enough to improve time to complete motor speed tasks measured by the TMT-A and motor functional tasks measured by the mFIM [13•]. Despite these findings, the study did not report how frequent or in what context these METs were being performed which makes this study hard to replicate and draw conclusions from.
When mobility is implemented efficiently and effectively in the hospital, it is most commonly done in an interdisciplinary format where each discipline holds responsibility for monitoring the status of the patient and safely implementing mobility tasks. When considering disciplines involved in performing mobility activities with patients, it is necessary to involve the physician, nurses, physical and occupational therapists in decision making in addition to nursing staff for training in safe mobility to reduce the risk of falls. One study implemented a theory of Function-Focused Care in Acute Care (FFC-AC) for orthopedic trauma patients and was able to infer nurses who were more educated and involved in consistent communication regarding the mobility and functional status of their patients were more likely to show greater functional improvements and display greater physical resilience at 30 days post discharge compared to standard education of the nurses [14•]. This study emphasizes the need to engage all staff in safe handling and benefits of frequent mobility and function-focused activities for patients recovering from orthopedic trauma. Another study in this review emphasizes the clinical expertise of PTs regarding recommendations for assistance for mobility, need for assistive devices, and optimal discharge setting to achieve the most ideal positive outcomes following recovery from an orthopedic condition [15•]. This study again emphasizes the vital importance for interdisciplinary collaboration when establishing mobility protocols and recommendations for patients.
Limitations of this study include using only one search engine to scan for existing evidence, potentially limiting the number of studies available to screen for inclusion criteria in this review. Other limitations in this research include inconsistent outcome measures across the board but specifically those to measure activity intensity, pain, and functional gains. The articles in this review were not consistent or clear in their dosage of activity performed, making their studies impossible to replicate. In addition, this study reviews a small sample of orthopedic conditions and surgical interventions, so the recommendations for safe mobility may differ for each of those.
A more comprehensive and broad review of the literature may provide more insight into the available evidence in order to make stronger recommendations regarding when and how to prescribe mobility interventions for a geriatric patient recovering from an orthopedic condition. In addition, developing guidelines for mobility for a specific orthopedic population may provide more consistent dosage and outcome measures to ensure more generalizable results with a review of the literature.
Conclusion
Despite the limitations of this study and existing literature, it is clear integrating mobility within the first 24 h following the injury or surgical intervention does not produce additional adverse effects or increase pain intensity. Due to the lack of research regarding dosage of mobility in the hospital setting, it may be advisable to implement activity monitors in subsequent studies to better quantify the results. This review suggests emphasizing interprofessional collaboration with nurses, physicians, PTs, and OTs when implementing a mobility protocol is vital to the success and safety of patients.
Abbreviations
- LOS:
-
Length of stay
- DVT:
-
Deep venous thromboembolism
- TJA:
-
Total joint arthroplasty
- ROM:
-
Range of motion
- TKA:
-
Total knee arthroplasty
- THA:
-
Total hip arthroplasty
- VCF:
-
Vertebral vompression fracture
- VAS:
-
Visual analog scale
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Hastings SN, Choate AL, Mahanna EP, et al. Early mobility in the hospital: lessons learned from the STRIDE Program. Geriatr Basel Switz. 2018;3(4). https://doi.org/10.3390/geriatrics3040061.
Lisi C, Caspani P, Bruggi M, et al. Early rehabilitation after elective total knee arthroplasty. Published online 2017:6. This study provided data that confirms the benefit of rehabilitation started as soon as 24 h after minimally invasive surgery on the achievement of early recovery of walking controlling pain.
Abeles A, Kwasnicki RM, Pettengell C, Murphy J, Darzi A. The relationship between physical activity and post-operative length of hospital stay: a systematic review. Int J Surg Lond Engl. 2017;44:295–302. https://doi.org/10.1016/j.ijsu.2017.06.085.
Daskivich TJ, Houman J, Lopez M, et al. Association of wearable activity monitors with assessment of daily ambulation and length of stay among patients undergoing major surgery. JAMA Netw Open. 2019;2(2):e187673. https://doi.org/10.1001/jamanetworkopen.2018.7673This study provided data about dosage of ambulation during hospitalization and the impact the amount of steps taken has on functional outcomes and length of stay.
Ravi B, Croxford R, Reichmann WM, Losina E, Katz JN, Hawker GA. The changing demographics of total joint arthroplasty recipients in the United States and Ontario from 2001 to 2007. Best Pract Res Clin Rheumatol. 2012;26(5):637–47. https://doi.org/10.1016/j.berh.2012.07.014.
Stevens JA, Rudd RA. The impact of decreasing U.S. hip fracture rates on future hip fracture estimates. Osteoporos Int. 2013;24(10):2725–8. https://doi.org/10.1007/s00198-013-2375-9.
Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev. 2005;11(2):115–9. https://doi.org/10.1136/ip.2004.005835.
Scheerman K, Raaijmakers K, Otten RHJ, Meskers CGM, Maier AB. Effect of physical interventions on physical performance and physical activity in older patients during hospitalization: a systematic review. BMC Geriatr. 2018;18(1):288. https://doi.org/10.1186/s12877-018-0965-2.
Oxford Centre for Evidence-based Medicine - Levels of evidence (March 2009). CEBM. Published June 11, 2009. Accessed June 14, 2020. https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/.
Asplin G, Carlsson G, Zidén L, Kjellby-Wendt G. Early coordinated rehabilitation in acute phase after hip fracture – a model for increased patient participation. BMC Geriatr. 2017;17(1). https://doi.org/10.1186/s12877-017-0640-z.
Soeters R, White PB, Murray-Weir M, Koltsov JCB, Alexiades MM, Ranawat AS. Preoperative physical therapy education reduces time to meet functional milestones after total joint arthroplasty. Clin Orthop. 2018;476(1):40–8. https://doi.org/10.1007/s11999.0000000000000010.
Zietek P, Zietek J, Szczypior K, Safranow K. Effect of adding one 15-minute-walk on the day of surgery to fast-track rehabilitation after total knee arthroplasty: a randomized, single-blind study. Eur J Phys Rehabil Med. 2015;51(3):8 This study provided data that suggests more intense exercise during the hospitalization period may improve functional recovery without increasing pain for patients following TKA.
Kataoka H, Ikemoto T, Yoshimura A, et al. Association of early physical activity time with pain, activities of daily living, and progression of vertebral body collapse in patients with vertebral compression fractures. Eur J Phys Rehabil Med. 2017;53(3):11 This article was able to draw the conclusions that coordinated, intensive rehabilitation compared to standard protocols, improved reports of higher levels of perceived participation, greater levels of independence with P-ADL activities of lower body hygiene and dressing at discharge, and decreased help required for walking outdoors and ascend/descend stairs at 1 month follow-up.
Resnick B, Wells C, Galik E, et al. Feasibility and efficacy of function-focused care for orthopedic trauma patients. J Trauma Nurs. 2016;23(3):144–55. https://doi.org/10.1097/JTN.0000000000000203This article provided insight into how disciplines other than PT and OT can play a key role in the mobilization of patients in the hospital to improve functional outcomes for patients by using the Function-Focused Care in Acute Care (FCC-AC) framework.
Polnaszek B, Mirr J, Roiland R, Gilmore-Bykovskyi A, Hovanes M, Kind A. Omission of physical therapy recommendations for high-risk patients transitioning from the hospital to subacute care facilities. Arch Phys Med Rehabil. 2015;96(11):1966–1972.e3. https://doi.org/10.1016/j.apmr.2015.07.013This article included data that showed the rate at which PT recommendations are omitted from the patient’s discharge summary from the hospital for patients transitioning to a sub-acute care facility. Such omissions were shown to lead to negative functional outcomes at a 30-day follow up. This suggests the importance of including PT recommendations into the patient’s discharge summary from hospital for providers at the next level of care, which emphasizes the need for increased intradisciplinary and interdisciplinary collaboration across levels of care.
Isaac D, Falode T, Liu P, I’Anson H, Dillow K, Gill P. Accelerated rehabilitation after total knee replacement. Knee. 2005;12(5):346–50. https://doi.org/10.1016/j.knee.2004.11.007.
Goyal N, Chen AF, Padgett SE, et al. Otto Aufranc Award: a multicenter, randomized study of outpatient versus inpatient total hip arthroplasty. Clin Orthop Relat Res. 2017;475(2):364–72. https://doi.org/10.1007/s11999-016-4915-zThis study provided data that shows a difference in VAS pain scores among those who discharge home on DOS versus those who stay overnight in the hospital. The cause of the increased pain for those who discharge home is unclear; improved counseling on pain management at home (when to take medications, which medications to take, modalities to reduce pain) may be warranted or the increase in pain could be due to the increased mobility required to transition from the hospital to the patient’s home.
Gromov K, Jørgensen CC, Petersen PB, et al. Complications and readmissions following outpatient total hip and knee arthroplasty: a prospective 2-center study with matched controls. Acta Orthop. 2019;90(3):281–5. https://doi.org/10.1080/17453674.2019.1577049This study provided data comparing readmission rates in patients with either a THA or TKA who were discharged on DOS versus patients with at least 1 overnight stay. No statistical significant differences were found between groups.
Chen H, Chen H, Wang Y, Chen P, Chien C. Association between rehabilitation timing and major complications of total knee arthroplatsy. J Rehabil Med. 2012;44(7):588–92. https://doi.org/10.2340/16501977-0971.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Geriatric Orthopedics
Rights and permissions
About this article
Cite this article
Peck, M., Holthaus, A., Kingsbury, K. et al. Mobility in Acute Care for Geriatric Patients with Orthopedic Conditions: a Review of Recent Literature. Curr Geri Rep 9, 300–310 (2020). https://doi.org/10.1007/s13670-020-00347-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-020-00347-1