Abstract
Purpose of Review
Pulmonary tuberculosis (TB) remains a diagnostic challenge, particularly in low endemic settings with ageing populations. The impact has both individual and infection control implications.
Recent Findings
Over the past 20 years, progress has been made in trying to improve TB diagnostics. International recommendations for investigation however still rely heavily on the index of suspicion, imaging and ultimately culturing Mycobacterium tuberculosis which remains the gold standard for diagnosing TB disease. Recent advances include molecular diagnostics with the ability to rapidly identify TB disease and drug resistance and whole-genome sequencing.
Summary
In this review, we explore the validity of TB diagnostics in the elderly to assist the practicing clinician in the diagnostic workup in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis (TB) is the leading cause of death from a single infectious agent worldwide [1]. The elderly (defined for this review as individuals > 65 years) are a particularly vulnerable population in both developing and developed countries, with higher mortality rates and adverse reactions to treatment.
Further diagnosing TB can be challenging and is often delayed in this population, being compounded by higher levels of comorbidity and frailty. In this review, we summarize how advancing age may affect the diagnosis of TB.
Background
The overall TB notification rate in the UK in 2017–2018 was 9.1 per 100,000 population. When stratified by age group, notifications were highest among those aged 30–39 years (14.4 per 100,000 population) [2]. When restricted to UK-born citizens alone, TB notification rates were highest among those over 65 years, with those over 80 years having the highest incidence (3.9 [95% CI 3.1–4.8] per 100,000 population). Despite this, nearly 40% of TB cases among those over 65 years experienced a diagnostic delay of more than 4 months. Evidence also suggests that time from symptom onset to treatment in patients with pulmonary TB is significantly longer in those over 65 years compared with those aged 18–64 years (92.5 versus 61 days; p = 0.003) [3].
Infection with Mycobacterium tuberculosis results in either the elimination of infection or the persistence of the pathogen. When the pathogen persists, a dynamic relationship is thought to exist between the host and M. tuberculosis, resulting in a continuous spectrum between TB infection and disease. Within this spectrum, broad clinical states have been described (Table 1) [4••].
While active lung parenchymal infection with M. tuberculosis (active pulmonary TB disease, henceforth called TB disease) is the focus of this review, laryngeal, tracheal and endobronchial TB may co-exist. Another common incidental finding in the elderly is tuberculoma; this asymptomatic rounded lesion occurs following primary infection and is frequently managed as indeterminate pulmonary nodules. While usually static, on occasion, it can cavitate and lead to TB disease. The main differential diagnosis for tuberculomas in developed countries is malignant disease. An outline of the recommended investigations for patients with suspected TB disease is summarized in Table 2.
Confirming a diagnosis of TB disease prior to commencing treatment is especially important in the elderly, as polypharmacy, comorbidities and physiological changes in this age group can lead to an increased risk of adverse events from TB treatment. Hepatotoxicity is the most common adverse reaction and the risk is significantly higher in patients over 65 years of age [8,9,10]. Although less common, renal impairment secondary to rifamycins also significantly increases with age, especially in diabetics [11]. However, with TB disease, the benefit of treatment outweighs these risks. But, they should be taken into account when deciding on drug regimens and monitoring frequency. When treating latent TB infection (LTBI) in the elderly population, the risk of hepatotoxicity may be even higher [10, 12], possibly due to less rigorous monitoring regimes. Therefore, treating LTBI is not recommended in this age group unless there is a strong indication to do so.
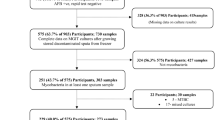
Methods
Using subject headings and keywords (Appendix), Medline and EMBASE were searched from inception to the 30th of October 2019 for original research studies. Bibliographies of identified studies were searched for additional studies or sources of data. The subject headings and keywords used covered the domains of (1) TB diagnostic tests; (2) diagnostic test validity; and (3) the elderly population. The expressions were combined using the Boolean operator AND to generate a final output of studies.
In all the study designs, the validity of tests for TB diagnosis was investigated and comparisons were made between the different tests which were eligible for inclusion. The study population was elderly. The TB diagnostics of interest were symptoms, CXR, sputum microscopy, culture and nucleic acid amplification tests. Only English-language articles were included; all other languages were excluded. Primary articles were restricted to human studies only.
Study selection was undertaken by two independent reviewers. Any disagreements were resolved through discussion or, if required, consultation with a third reviewer. Studies were initially shortlisted based on the title and abstract. The definite selection was based on screening the full texts of shortlisted studies for eligibility. All relevant data were entered onto standardized case report forms by a single reviewer. Findings are summarized qualitatively.
Clinical Features
Individuals may be at risk of TB disease due to host factors such as malnutrition, immunosuppression, untreated HIV infection, smoking, alcohol and drug abuse and comorbid conditions such as diabetes mellitus [13, 14]. Tuberculosis is more common in patients with malignancy, with the highest risk in patients with haematological and head and neck cancers [15,16,17]. Further individuals in congregate settings such as prisons or long-term care facilities are also at increased risk. [18, 19].
TB disease should be suspected in individuals with risk factors for TB, who present with a prolonged cough of more than 2 weeks duration, haemoptysis, lymphadenopathy and B-type symptoms such as fever, night sweats and weight loss. These symptoms are not diagnostic for TB disease; their sensitivity and specificity are variables depending on patient risk factors and whether the patient is in a high or low TB endemic region [13]. Physical examination findings are usually non-specific. Previous evidence of TB treatment may be present, particularly in the elderly, who may have signs of cervical lymph node resection, thoracoplasty, induced pneumothoraces and phrenic nerve injuries. However, there are no studies that compare the findings on clinical examination among the elderly and the young.
Several studies have attempted to establish if there is a difference in the clinical presentation of TB disease between younger and older adults. However, most of these studies have a small sample size and used varying and arbitrary cut-offs between age groups, making comparisons between studies difficult. Some small early studies suggested there was no difference in presenting symptoms between younger and older patients [20] whereas others found older patients were more likely to present with anorexia and weight loss and less likely to present with cough, fever and haemoptysis [21, 22]. A meta-analysis by Perez-Guzman and colleagues found that patients over 60 years of age were less likely to have fever, sweating and haemoptysis and had lower serum albumin concentrations and leukocyte counts [23]. This atypical presentation in older adults has also been shown in several more recent studies. In an Indian study, elderly patients (> 60 years of age) were less likely to present with respiratory or constitutional symptoms and had a longer duration of symptoms prior to diagnosis [24]. Similar results were found in a cohort of patients > 65 years in Mexico [25••]. However, contrary to these findings, a Korean study found that patients > 65 years of age were more likely to present with dyspnoea, but, after adjusting for gender, smoking and comorbid conditions, no significant difference in symptoms were found between older and younger patients [26]. As expected, a higher proportion of comorbid conditions were found in older patients in nearly all studies, which may be a confounding factor. Nevertheless, it appears that TB disease is more likely to present atypically in older patients and therefore, a low index of suspicion is required to make the diagnosis.
In a study of elderly patients with TB disease and non-TB respiratory infection, cough was less common in the latter group (p = 0.003). Diabetes mellitus was more common among TB disease patients and previous TB was reported equally in both groups [5].
Radiology
Chest Radiography
Chest radiographs (CXR) are the first line of imaging to aid the diagnosis of TB disease [6, 7, 27] and are recommended by most authorities as part of the diagnostic workup in suspected TB disease cases (Table 1). CXRs may display an array of features including nodules, infiltrates, consolidation, cavities, mediastinal lymphadenopathy and effusions (see Fig. 1). Traditionally, findings are divided into typical and atypical features. Typical features occur in immunocompetent individuals and include upper lobe infiltrates or cavitatory lesions. Atypical features occur in immunocompromised individuals and include lower lobe disease, lymphadenopathy, miliary TB and pleural effusions. [28].
Radiographic features of tuberculosis (TB) disease. Figure shows chest radiographs and respective coronal CT scans demonstrating typical features of patients with TB. Panels a and b demonstrate right upper lobe mass like consolidation (small white arrow) and loss of the right paratracheal stripe (fat white arrow) indicative of paratracheal lymphadenopathy. Furthermore, the white dotted arrow in panel b shows nodular changes. Panels c and d demonstrate right upper lobe consolidation—visible on the chest radiograph, but clearer on the CT scan, with tree in-bud-changes (dotted arrow) adjacent to consolidation (small white arrow)
However, even with typical CXR changes, CXR specificity for TB disease is low, ranging from 46 to 89% [29]. Furthermore, there is also inter-observer variability in interpreting CXRs from TB disease patients [10].
There is evidence that the radiological appearance of TB disease in the elderly differs from that of younger adults. CXRs are less likely to show cavitation [23] and more likely to demonstrate middle or lower zone infiltrates and multifocal disease [30, 31] in the elderly. They are also more likely to show a mass like or consolidative lesion and therefore are often initially misdiagnosed as bacterial pneumonia or cancer [30]. In a study of patients presenting with unilateral lower lobe pneumonia, 10% were diagnosed with TB disease, which occurred more frequently in the elderly on univariate analysis although no association was found on multivariable analysis [32].
Computed Tomography
Thoracic computed tomography (CT) has a higher sensitivity than CXRs in the detection of both subtle parenchymal abnormalities and mediastinal lymphadenopathy in TB disease. Further, it is better at differentiating active TB from old TB [1]. It is the most common second-line imaging modality but is usually reserved for cases with equivocal CXR changes.
The data for CT findings in the elderly is mixed. One study suggested little difference in CT findings between younger and older patients except for a higher proportion with miliary TB in older patients (0.7% vs 6.7%) [21]. Another study found that CT in older patients was less likely to show nodules, micronodules and cavitation and more likely to show consolidation [26], similar to the findings on CXRs.
In the elderly with respiratory infections, consolidation (96% versus 70%), cavitation (73% versus 9.8%), nodules/masses (72% versus 2%), tree-in-bud changes (93% versus 25%), centrilobular nodules (80% versus 57%) and fibrosis (23% versus 14%) were more common in TB disease than other respiratory infections [5]. Among the elderly with TB disease, there was a higher proportion with consolidation in the superior segment of the lower lobe, tree-in-bud changes, calcification and fibrosis compared with younger patients. Furthermore, a lower proportion had clusters of nodules/masses and there was no difference in cavitation between the groups.
CT changes in those with smear-positive and smear-negative TB disease has also been studied [33•]. While no difference in findings by age group was identified, the median age of the study group was 63 years with 25% of patients being older than 76 years [33•]. Compared with smear-negative patients, smear-positive patients were more likely to have consolidation, cavitation, bronchiectasis, upper lobe involvement and lymphadenopathy.
A common finding in the workup for patients with suspected TB disease is that of non-tuberculous mycobacterial (NTM) diseases. Kim et al. compared radiographic appearances (CXR and CT) in patients with TB and NTM [34]. As expected, a considerable overlap in radiographic appearance was found between the two groups. However, patients with NTM were more likely to be elderly (> 65 years), and a higher proportion of those with TB disease had consolidative appearances on imaging (88% versus 67%) [34]. This emphasizes the importance of culture confirmation and speciation of all suspected TB disease cases, even when smear is positive, to guide treatment and infection control measures.
PET-CT
Positron emission tomography (PET) can be used to assess the metabolic activity of lesions via the uptake of radio-nuclides such as 18-fluorodeoxyglucose (FDG). PET has traditionally aided diagnostic processes and is said to be highly sensitive and specific at discerning malignant from benign conditions in low endemic infectious areas. However, sensitivity and specificity of PET in diagnosing lung cancer in high endemic infectious areas is poor [35], and a recent review highlighted the limited role of PET in discerning tuberculous and cancerous lesions due to the variable metabolic activity of TB disease and/or the host inflammatory response [36].
Research has focused on various techniques to reliably distinguish cancerous from tuberculous lesions using PET including innovative radionuclides, use of dual radionuclides [37], arbitrary cut-offs in standardized uptake values [38] and delayed imaging or dual time point imaging, with various success. Others have focused on using PET to predict TB disease versus latent TB infection [39].
Although retrospective analysis of PET scans of individuals with confirmed TB has demonstrated useful information in tuberculous lesion characteristics, findings described are not diagnostic of TB disease [36, 40]. Furthermore, even in high TB prevalence settings, TB disease cases are misclassified as cancerous despite the use of PET-CT [38]. No studies were identified that compared the PET scan characteristics of TB disease patients by age.
Therefore, PET currently has a limited role in TB diagnosis [41] confined to cases where histological and bacterial diagnosis is unfavourable [37].
Summary
As with clinical features, elderly patients with TB disease are more likely to demonstrate atypical radiology. Therefore, a low index of suspicion is required to identify cases. It has been suggested that all older adults who present with pneumonia or a lung mass should have at least one sputum sent for microscopy and culture [42]. Indeed, in developed countries, it is not uncommon for patients with lung lesions to undergo pulmonary resection as part of their diagnostic/therapeutic workup; to find a benign lesion has been resected. Granulomatous disease constitutes the commonest aetiology of these benign lesions: a proportion of these represent TB disease [43].
Microbiological Confirmation
Sputum analysis is the cornerstone of diagnosis in patients with suspected TB disease. Conventional culture remains the gold standard but is technically difficult to perform and takes several weeks to get a result. Smear microscopy provides a much quicker result but has a low sensitivity (around 65%) [2]. Single cartridge nucleic acid amplification tests (NAATs) such as the Xpert MTB/RIF which has been endorsed by the World Health Organization (WHO) since 2011 have a sensitivity of 85% and specificity of 98% [2] and can provide a result within hours, while also guiding management by identifying common drug resistance genotypes. In patients who are unable to provide sputum, samples can be obtained by either flexible bronchoscopy or induced sputum with both methods providing similar yields [3].
Sputum Smear and Culture
It is unclear whether sputum microscopy and culture results differ between younger and older patients. Some studies have reported a lower proportion of sputum smear positivity in older patients [44, 45] whereas others have found no differences [21, 23, 24, 30]. When positive smears have been differentiated into low grade and high grade, significantly more low-grade positive sputum smears have been found in the older population [46, 47], although this shows a significant geographical variation [47]. There is some evidence that nursing home residents are more likely to have smear-negative, culture-positive TB disease compared with community dwelling older people [48]. The proportion with positive cultures was similar between older and younger patients in most studies, with only one study showing higher culture positivity in the older population; however, this included samples taken during bronchoscopy which occurred more frequently in the older population [26]. Therefore, sputum analysis with microscopy and culture remains the first-line investigation in elderly patients suspected to have TB disease. Data from the national surveillance system in the USA shows that older patients (including those diagnosed at post mortem) were less likely to have sputum smear and culture results recorded [49].
Nucleic Acid Amplification Tests
Nucleic acid amplification tests (NAATs) have become commonplace since they were recommended by the WHO in 2011, with some guidelines recommending their use in all cases whereas others suggest using them in selected patients (Table 1). A number of methods including polymerase chain reaction (PCR), real-time PCR and loop-mediated isothermal amplification (LAMP) can detect TB and selected drug resistance within 2 h of sampling compared with weeks for traditional culture, helping to reduce unnecessary or ineffectual courses of treatment. Perhaps the most used system worldwide is the Cepheid Xpert MTB/RIF system; a Cochrane review found it had a sensitivity of 85% and a specificity of 98% for detecting TB disease. A newer version of the test, the Xpert ULTRA, has a higher sensitivity but lower specificity (88% and 95%, respectively) [50]. The sensitivity and specificity for rifampicin resistance were 96% and 98% for Xpert MTB/RIF and 95% and 98% for Xpert ULTRA, respectively [50]. Its role in detecting TB in elderly patients has not been a focus of studies. But awareness of the test is important, for those in whom there is a high degree of suspicion and time is critical or drug resistance is a possibility.
Whole-Genome Sequencing
Once mycobacterium is isolated, whole-genome sequencing (WGS) and next-generation sequencing (NGS) can be performed. There are currently no studies investigating the sensitivity or specificity of these tests in older patients and given this is pathogen-dependent, it is unlikely to be affected.
Obtaining Samples in Non-sputum Producers
Approximately a quarter of patients with TB disease are unable to produce sputum. Sputum induction is a procedure where hypertonic saline (usually 3%) is administered via a nebulizer to provoke coughing and sputum collection. It is an option for patients who are unable to produce sputum spontaneously or are not suitable for bronchoscopy. It has been shown to perform similarly to bronchoscopy and maybe more cost-effective [51, 52], with a sensitivity for smear and culture being 34% and 67%, respectively [52].
In patients who are unable to provide sputum (spontaneous or induced), flexible bronchoscopy can be considered with a view to performing a bronchoalveolar lavage (BAL) [53]. BAL fluid is positive in 50–60% of culture-confirmed TB disease patients [54, 55]. Post bronchoscopy, patients will expectorate over the following days, so it is worth collecting further sputum samples as these too are frequently confirmatory [54]. In a large study of 1539 patients with sputum smear-negative suspected TB disease, BAL fluid showed a higher sensitivity than sputum for culture and NAAT (63% versus 43%). In 20% of those with negative sputum culture and NAAT and 40% unable to produce sputum samples, positive results were obtained from a BAL [56•]. Factors associated with positive BAL included younger age, pulmonary cavitation and a positive interferon-gamma release assay (IGRA).
Other Sampling Methods
There are several other sampling methods including gastric aspiration, stool sampling and tissue biopsies. All can be considered in difficult cases when standard approaches cannot be achieved or remain unsuccessful in confirming a diagnosis.
If invasive testing is contraindicated, evaluation of stool samples may be used in elderly patients, with molecular testing having a higher positive rate than microscopy and culture (68% versus 13% versus 41% respectively) for detecting TB disease [57].
CT-guided core biopsies can also be considered, and in one large case series of patients with suspected TB disease, the sensitivity and specificity were 80% and 100%, respectively [58]. The positive predictive value and negative predictive value were 100% and 89%. Complications included pneumothorax (9%), bleeding at biopsy site (11%) and haemoptysis (8%). Such biopsies may show mycobacterium, chronic inflammation, necrosis or benign-appearing tissue.
Other Tests of Variable Utility
Tuberculin Skin Testing
It has long been established that tuberculin skin test (TST) reactivity decreases with advancing age [59, 60], with positivity falling from 15% in the over 70s to less than 3% in the over 90s [61]. A negative TST does not rule out disease in this population and has even lower sensitivity in patients with a low BMI (< 18.5 kg/m2) [62]. TST becomes increasingly positive with retesting, the so-called booster effect. This increasing response is more profound in older patients [63]; thus, caution must be taken when interpreting a test that goes from negative to positive on retesting as may be due to the booster effect. For these reasons, there is a limited clinical use of TST in the elderly.
Interferon-Gamma Release Assays (IGRAS)
There are two main tests that are currently in widespread use: the QuantiFERON - TB Gold (QFT –G) and T-SPOT test. These tests indicate a host’s cell-mediated immune response to Mycobacterium tuberculosis antigens. It is a tool for detecting TB exposure, but it is important to note that it does not indicate TB disease and can be negative in TB disease. These tests rely upon a CD4-mediated immune response.
In TB disease, IGRAs demonstrate a better sensitivity and specificity than TST in elderly patients [64]. But the proportion of positivity by IGRA varies with age; 79% of elderly patients with TB disease had a positive IGRA versus 86–92% in the younger age groups in one study, which was associated with a lower lymphocyte count.
In TB disease, T-SPOT has a higher sensitivity and specificity than the QFT-G test [65, 66]. Furthermore, the sensitivity of QFT-G test reduces with age while the T-SPOT shows no significant decrease [65]. However, T-SPOT is associated with higher false-positive results in those over 65 years [66]. Since IGRAs do not distinguish between TB infection and disease [67], their role in TB disease diagnosis is limited. But, they are frequently performed in low TB prevalence settings. Recent developments to the QFT-G test, the QuantiFERON - TB Gold Plus, include a CD8 component which may have a role in TB disease diagnosis.
Conclusions
The elderly population has various risk factors for TB, through a lifelong risk of exposure to comorbidities that are associated with TB disease. Clinical phenotypes are often non-specific and imaging may appear atypical. Differential diagnoses include other infections, malignancy and non-tuberculous mycobacterium. While obtaining samples for microbiology and performance of microbiological tests do not differ by age, the risks of invasive procedures may influence the level to which tests are performed in the elderly. Urgent innovation is required to identify robust methods to definitively diagnose TB disease in a timely way in patients where imaging and standard approaches fail or lead to a drawn-out process with a risk of onward TB transmission.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organisation. Global tuberculosis report 2019 https://www.who.int/tb/publications/global_report/en/2019.
Public Health England. Tuberculosis in England: 2019 Report. PHE Publications; 2019.
Abbara A, Collin SM, Kon OM, Buell K, Sullivan A, Barrett J, et al. Time to diagnosis of tuberculosis is greater in older patients: a retrospective cohort review. ERJ Open Res. 2019;5(4):00228–2018.
•• Drain PK, Bajema KL, Dowdy D, Dheda K, Naidoo K, Schumacher SG, et al. Incipient and Subclinical Tuberculosis: a Clinical Review of Early Stages and Progression of Infection. Clin Microbiol Rev. 2018;31(4). An excellent review of the spectrum of TB infection, highlighting the different stages of infection with elimination, latent TB, incipient TB, subclinical and active disease. The literature around these stages of disease is reviewed giving insight into contemporary understanding of this complex disease.
Yeh JJ, Chen SC, Chen CR, Yeh TC, Lin HK, Hong JB, et al. A high-resolution computed tomography-based scoring system to differentiate the most infectious active pulmonary tuberculosis from community-acquired pneumonia in elderly and non-elderly patients. Eur Radiol. 24(10):2372–84.
Lewinsohn DM, Leonard MK, LoBue PA, Cohn DL, Daley CL, Desmond E, et al. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention clinical practice guidelines: diagnosis of tuberculosis in adults and children. Clin Infect Dis. 2017;64(2):111–5.
NICE. guidelines. Tuberculosis. 2016; NICE guidelines NG33. UK.
Schluger NW. Tuberculosis and nontuberculous mycobacterial infections in older adults. Clin Chest Med. 2007;28(4):773–81 vi.
Pande JN, Singh SP, Khilnani GC, Khilnani S, Tandon RK. Risk factors for hepatotoxicity from antituberculosis drugs: a case-control study. Thorax. 1996;51(2):132–6.
Hosford JD, von Fricken ME, Lauzardo M, Chang M, Dai Y, Lyon JA, et al. Hepatotoxicity from antituberculous therapy in the elderly: a systematic review. Tuberculosis (Edinb). 2015;95(2):112–22.
Chang CH, Chen YF, Wu VC, Shu CC, Lee CH, Wang JY, et al. Acute kidney injury due to anti-tuberculosis drugs: a five-year experience in an aging population. BMC Infect Dis. 2014;14:23.
Smith BM, Schwartzman K, Bartlett G, Menzies D. Adverse events associated with treatment of latent tuberculosis in the general population. CMAJ. 2011;183(3):E173–9.
Cudahy P, Shenoi SV. Diagnostics for pulmonary tuberculosis. Postgrad Med J. 2016;92(1086):187–93.
Ferrara G, Murray M, Winthrop K, Centis R, Sotgiu G, Migliori GB, et al. Risk factors associated with pulmonary tuberculosis: smoking, diabetes and anti-TNFalpha drugs. Curr Opin Pulm Med. 2012;18(3):233–40.
Teng CJ, Huon LK, Zheng YM, Yeh CM, Tsai CK, Liu JH, et al. Increased risk of tuberculosis in oral cancer patients in an endemic area: a nationwide population-based study. Clin Oral Investig. 2019;23(12):4223–31.
Ganzel C, Silverman B, Chemtob D, Ben Shoham A, Wiener-Well Y. The risk of tuberculosis in cancer patients is greatest in lymphoma and myelodysplastic syndrome/myeloproliferative neoplasm: a large population-based cohort study. Leuk Lymphoma. 2019;60(3):720–5.
Cheng MP, Abou Chakra CN, Yansouni CP, Cnossen S, Shrier I, Menzies D, et al. Risk of active tuberculosis in patients with Cancer: a systematic review and meta-analysis. Clin Infect Dis. 2017;64(5):635–44.
Nardell EA. Tuberculosis in homeless, residential care facilities, prisons, nursing homes, and other close communities. Semin Respir Infect. 1989;4(3):206–15.
Narasimhan P, Wood J, Macintyre CR, Mathai D. Risk factors for tuberculosis. Pulm Med. 2013;2013:828939.
Katz PR, Reichman W, Dube D, Feather J. Clinical features of pulmonary tuberculosis in young and old veterans. J Am Geriatr Soc. 1987;35(6):512–5.
Korzeniewska-Kosela M, Krysl J, Müller N, Black W, Allen E, FitzGerald JM. Tuberculosis in young adults and the elderly: a prospective comparison study. CHEST. 1994;106(1):28–32.
Van Dijk JM, Rosin AJ. A comparison of clinical features of mycobacterial infections in young and elderly patients. Neth J Med. 1993;42(1):12–5.
Perez-Guzman C, Vargas MH, Torres-Cruz A, Villarreal-Velarde H. Does aging modify pulmonary tuberculosis?: a meta-analytical review. Chest. 1999;116(4):961–7.
Bhushan B, Kajal NC, Maske A, Singh SP. Manifestations of tuberculosis in elderly versus young hospitalised patients in Amritsar, India. Int J Tuberc Lung Dis. 2012;16(9):1210–3.
•• Cruz-Hervert LP, Garcia-Garcia L, Ferreyra-Reyes L, Bobadilla-del-Valle M, Cano-Arellano B, Canizales-Quintero S, et al. Tuberculosis in ageing: high rates, complex diagnosis and poor clinical outcomes. Age Ageing. 2012;41(4):488–95. This prospective study is specific to the aging population and describes the clinical spectrum and compares to younger age groups.
Kwon YS, Chi SY, Oh IJ, Kim KS, Kim YI, Lim SC, et al. Clinical characteristics and treatment outcomes of tuberculosis in the elderly: a case control study. BMC Infect Dis. 2013;13(1):121.
Migliori GB, Sotgiu G, Rosales-Klintz S, Centis R, D'Ambrosio L, Abubakar I, et al. ERS/ECDC Statement: European Union standards for tuberculosis care, 2017 update. Eur Respir J. 2018;51(5).
Rozenshtein A, Hao F, Starc MT, Pearson GD. Radiographic appearance of pulmonary tuberculosis: dogma disproved. AJR Am J Roentgenol. 2015;204(5):974–8.
Cohen R, Muzaffar S, Capellan J, Azar H, Chinikamwala M. The validity of classic symptoms and chest radiographic configuration in predicting pulmonary tuberculosis. Chest. 1996;109(2):420–3.
Lee JH, Han DH, Song JW, Chung HS. Diagnostic and therapeutic problems of pulmonary tuberculosis in elderly patients. J Korean Med Sci. 2005;20(5):784–9.
Morris CD, Nell H. Epidemic of pulmonary tuberculosis in geriatric homes. S Afr Med J Suid-Afrikaanse Tydskrif Vir Geneeskunde. 1988;74(3):117–20.
Lin CH, Chen TM, Chang CC, Tsai CH, Chai WH, Wen JH. Unilateral lower lung field opacities on chest radiography: a comparison of the clinical manifestations of tuberculosis and pneumonia. Eur J Radiol. 2011;81(4):e426–30.
• Kim JH, Kim MJ, Ham SY. Clinical characteristics and chest computed tomography findings of smear-positive and smear-negative pulmonary tuberculosis in hospitalized adult patients. Medicine. 2019;98(34):e16921. A useful contemporary study for clinicians describing the different radiographical features in smear positive and negative patients.
Kim YK, Hahn S, Uh Y, Im DJ, Lim YL, Choi HK, et al. Comparable characteristics of tuberculous and non-tuberculous mycobacterial cavitary lung diseases. International Journal of Tuberculosis & Lung Disease. 2014;18(6):725–9.
Deppen SA, Blume JD, Kensinger CD, Morgan AM, Aldrich MC, Massion PP, et al. Accuracy of FDG-PET to diagnose lung cancer in areas with infectious lung disease: a meta-analysis. JAMA. 2014;312(12):1227–36.
Ankrah AO, Glaudemans A, Maes A, Van de Wiele C, Dierckx R, Vorster M, et al. Tuberculosis. Semin Nucl Med. 2018;48(2):108–30.
Hara T, Kosaka N, Suzuki T, Kudo K, Niino H. Uptake rates of 18F-fluorodeoxyglucose and 11C-choline in lung cancer and pulmonary tuberculosis: a positron emission tomography study. Chest. 2003;124(3):893–901.
Lang S, Sun J, Wang X, Xiao Y, Wang J, Zhang M, et al. Asymptomatic pulmonary tuberculosis mimicking lung cancer on imaging: a retrospective study. Exp Ther Med. 2017;14(3):2180–8.
Kim IJ, Lee JS, Kim SJ, Kim YK, Jeong YJ, Jun S, et al. Double-phase 18F-FDG PET-CT for determination of pulmonary tuberculoma activity. Eur J Nucl Med Mol Imaging. 2008;35(4):808–14.
Soussan M, Brillet PY, Mekinian A, Khafagy A, Nicolas P, Vessieres A, et al. Patterns of pulmonary tuberculosis on FDG-PET/CT. Eur J Radiol. 2012;81(10):2872–6.
Skoura E, Zumla A, Bomanji J. Imaging in tuberculosis. Int J Infect Dis. 2015;32:87–93.
Schaaf HS, Collins A, Bekker A, Davies PDO. Tuberculosis at extremes of age. Respirology. 2010;15(5):747–63.
Smith MA, Battafarano RJ, Meyers BF, Zoole JB, Cooper JD, Patterson GA. Prevalence of benign disease in patients undergoing resection for suspected lung cancer. Ann Thorac Surg. 2006;81(5):1824–8. discussion 8-9.
Wang C-S, Chen H-C, Yang C-J, Wang W-Y, Chong I-W, Hwang J-J, et al. The impact of age on the demographic, clinical, radiographic characteristics and treatment outcomes of pulmonary tuberculosis patients in Taiwan. Infection. 2008;36(4):335–40.
Cruz-Hervert LP, Garcia-Garcia L, Ferreyra-Reyes L, Bobadilla-del-Valle M, Cano-Arellano B, Canizales-Quintero S, et al. Tuberculosis in ageing: high rates, complex diagnosis and poor clinical outcomes. Age Ageing. 41(4):488–95.
Chinnakali P, Selvaraj K, Thekkur P, Ramasamy G, Thulasingam M, Vasudevan K. Age and sex differences in sputum smear microscopy results for acid fast bacilli in a tertiary care Centre, South India. J Respir Med. 2014;2014:5.
Rieder HL, Lauritsen JM, Naranbat N, Katamba A, Laticevschi D, Mabaera B. Quantitative differences in sputum smear microscopy results for acid-fast bacilli by age and sex in four countries. Int J Tuberc Lung Dis. 2009;13(11):1393–8.
Chitnis AS, Robsky K, Schecter GF, Westenhouse J, Barry PM. Trends in tuberculosis cases among nursing home residents, California, 2000 to 2009. J Am Geriatr Soc. 2015;63(6):1098–104.
Pratt RH, Winston CA, Kammerer JS, Armstrong LR. Tuberculosis in older adults in the United States, 1993–2008. J Am Geriatr Soc. 2011;59(5):851–7.
Horne DJ, Kohli M, Zifodya JS, Schiller I, Dendukuri N, Tollefson D, et al. Xpert MTB/RIF and Xpert MTB/RIF Ultra for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev. 2019;6.
McWilliams T, Wells AU, Harrison AC, Lindstrom S, Cameron RJ, Foskin E. Induced sputum and bronchoscopy in the diagnosis of pulmonary tuberculosis. Thorax. 2002;57(12):1010–4.
Anderson C, Inhaber N, Menzies D. Comparison of sputum induction with fiber-optic bronchoscopy in the diagnosis of tuberculosis. Am J Respir Crit Care Med. 1995;152(5 Pt 1):1570–4.
Patel YR, Mehta JB, Harvill L, Gateley K. Flexible bronchoscopy as a diagnostic tool in the evaluation of pulmonary tuberculosis in an elderly population. J Am Geriatr Soc. 1993;41(6):629–32.
Malekmohammad M, Marjani M, Tabarsi P, Baghaei P, Sadr Z, Naghan PA, et al. Diagnostic yield of post-bronchoscopy sputum smear in pulmonary tuberculosis. Scand J Infect Dis. 2012;44(5):369–73.
Mehta J, Krish G, Berro E, Harvill L. Fiberoptic bronchoscopy in the diagnosis of pulmonary tuberculosis. South Med J. 83(7):753–5.
• Liu X, Hou XF, Gao L, Deng GF, Zhang MX, Deng QY, et al. Indicators for prediction of Mycobacterium tuberculosis positivity detected with bronchoalveolar lavage fluid. Infect Dis Poverty. 2018;7(1):22. This study although retrospective reports on > 1500 smear-negative/non-sputum producers with suspected TB, reporting on the diagnostic yield of bronchoalveolar lavages.
Konno A, Narumoto O, Matsui H, Takeda K, Hirano Y, Shinfuku K, et al. The benefit of stool mycobacterial examination to diagnose pulmonary tuberculosis for adult and elderly patients. J Clin Tuberc Other Mycobact Dis. 2019;16(100106).
Chen J, Byanju S, Zhang H, Zhu D, Liao M. CT-guided percutaneous core needle biopsy of pulmonary tuberculosis: diagnostic accuracy and complications. Radiol Infect Dis. 5(2):69–75.
Beresford OD. Tuberculin skin sensitivity in old age. Am Rev Tuberc. 1958;77(2):323–8.
Dorken E, Grzybowski S, Allen EA. Significance of the tuberculin test in the elderly. Chest. 1987;92(2):237–40.
Nisar M, Williams CS, Ashby D, Davies PD. Tuberculin testing in residential homes for the elderly. Thorax. 1993;48(12):1257–60.
Chan-Yeung M, Dai DLK, Cheung AHK, Chan FHW, Kam KM, Tam CM, et al. Tuberculin skin test reaction and body mass index in old age home residents in Hong Kong. J Am Geriatr Soc. 2007;55(10):1592–7.
Holden M. Tuberculin sensitivity in elderly patients. Am Rev Respir Dis. 1972;105(5):854–5.
Kobashi Y, Mouri K, Yagi S, Obase Y, Miyashita N, Okimoto N, et al. Clinical utility of the QuantiFERON TB-2G test for elderly patients with active tuberculosis. Chest. 2008;133(5):1196–202.
Bae W, Park KU, Song EY, Kim SJ, Lee YJ, Park JS, et al. Comparison of the sensitivity of QuantiFERON-TB gold in-tube and T-SPOT. TB according to patient age. PLoS One. 2016;11.
Teramoto S, Komiya K, Ariga H, Kawashima M, Nagai H. Pitfalls of diagnostic values of the T-SPOT.TB assay to detect tuberculosis infection in elderly patients suspected with pulmonary tuberculosis (PTB) clinically. Am J Respir Crit Care Med Conference: American Thoracic Society International Conference, ATS. 2011;183(1).
Janssens JP. Clinical utility of the interferon-gamma release assay for elderly patients with active tuberculosis: a word of caution. Chest. 2008;134(2):471–2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pulmonology and Respiratory Care
Appendix
Appendix
Search terms in EMBASE
(((exp lung tuberculosis/ OR exp tuberculosis/) OR (TB or tuber*)) AND (exp diagnostic test/ OR exp diagnosis/ OR (diagnos*))) AND (exp “sensitivity and specificity”/ OR exp diagnostic accuracy/ OR exp predictive value/ OR exp validity/ OR (sensitivity or specificity or predictive value*)) AND (exp aged/ OR exp geriatrics/ OR (geriatric* OR elderly or old age))
Search terms in MEDLINE
(((exp Tuberculosis/ OR exp. Tuberculosis, Pulmonary/) OR (TB OR tuber*)) AND (exp Diagnosis/ OR exp. Diagnostic Tests, Routine/ OR (diagnos*))) AND (exp “Sensitivity and Specificity”/ OR exp “Predictive Value of Tests”/ OR (sensitivity OR specificity OR predictive value*)) AND (exp “Aged, 80 and over”/ OR exp Aged/ OR exp Geriatrics/ OR (geriatric* or elderly or old age))

Rights and permissions
About this article
Cite this article
Symes, M.J., Probyn, B., Daneshvar, C. et al. Diagnosing Pulmonary Tuberculosis in the Elderly. Curr Geri Rep 9, 30–39 (2020). https://doi.org/10.1007/s13670-020-00319-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-020-00319-5