Abstract
Purpose of Review
Periprosthetic fractures (PPF) of the lower extremity are increasing as the population ages, as the number of joint replacement increases, and patients remain active. The management of PPFs is challenging because of implant and cement obstruction within the bone, poor bone quality, and limited availability of bone stock for screw purchase. Historically, they have been associated with high rates of nonunion, infection, and fixation failure. Minimally invasive osteosynthesis (MIO) has reduced complications and improved union rates compared to conventional open plating of fractures. This paper reviews the principles of treatment, implant choices, and technical challenges of MIO for PPF in the lower extremity.
Recent Findings
In recent series, PPF for the lower extremity has shown reduced complication rates, improved union, and early mobilization compared prior open treatment.
Summary
MIO for PPF is technically challenging but promising method of treatment for PPF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rate of total joint arthroplasty is growing, and by 2030, it is estimated that the number of primary total hip arthroplasty (THA) in America will grow by 174% to an annual rate of 572,000 procedures per year, while total knee arthroplasty (TKA) will grow by 673% to 3.48 million procedures per year [1]. Not surprisingly, the incidence of periprosthetic fractures (PPFs) has also been increasing in the past several decades and will inevitably rise as the number of joint replacements increases [2].
The incidence of periprosthetic fracture after THA is estimated to be 1% for primary THA and 4% after revision THA [3], while the estimated incidence of fracture after knee arthroplasty is up to 5% after primary TKA, and up to 30% for revision TKA [4,5,6]. Most frequently, PPFs occur in the femur for both THA and TKA; however, they can also occur around the tibial component in 0.1–0.4% of TKA, particularly in revision cases [3, 5]. Because of implant and cement obstruction within the bone, poor bone quality, and limited availability of bone stock for screw purchase, management of PPFs can be particularly challenging and requires a careful approach to evaluate implant integrity, patient comorbidities, and fixation options [7, 8].
Classification
The most commonly used method for describing PPF is the Vancouver classification for fractures around a femoral stem (Table 1) [9]. This system is based on three main components: the fracture location, stability of the stem, and quality of the femoral bone stock around the stem. It has substantial inter- and intra-observer reliability [10]. For type B1 and type C fractures, where the stem is stable, internal fixation is the treatment of choice. For types B2 and B3, where the stem is loose, internal fixation is combined with revision of the prosthesis to a longer stem with either a press-fit or cemented implant.
Given the complex nature of these injuries, it is critical that the surgeon evaluate the integrity of the stem-bone interface for signs of loosening such as continuous lucency around the stem-bone, cement-bone, or stem-cement interface. A fracture around a cement mantle without lucency and no prior history of functional thigh pain is usually stable in the setting of acute fracture [11]. If there is any concern intra-operatively, the surgeon can perform an arthrotomy at the time of fixation, dislocate the hip, and directly assess the stability of the implant. In virtually all cases of PPF, revision instruments and implants should be available at the time of surgery. It is critical that the surgeon is prepared for any of these possible outcomes as the radiographic findings do not always correlate with implant stability.
Other classification schemes for PPF include the Rorabeck classification for PPF for femur fractures above a TKA [12], the Felix classification system for PPF around tibial implants, and the AO/OTA-based Unified Classification System for Periprosthetic Fractures (UCPF) which has been proposed for use in all extremities [13,14,15]. All of these classifications emphasize the importance of the location of the fracture relative to the implant and the stability of the implant itself to aid with management decisions.
Evolution of Treatment
Early treatment of patients with PPFs consisted of balanced traction and prolonged immobilization followed by revision arthroplasty which often yielded poor results [7]. Early case series describing operative management of these injuries were primarily concerned with fractures around a hip stem and include a mixture techniques. These include open reduction internal fixation with allografts, cerclage wiring, or isolated screws, or internal fixation combined with revision to a longer stemmed prosthesis in cases where the stem was unstable [16,17,18,19,20]. While this allowed earlier mobilization than nonoperatively treated PPF, surgeons reported high rates of nonunion, infection, and poor functional outcome in 30–50% of cases, which was similar to patients treated nonoperatively [20, 21].
Johansson et al. reported the results of dynamic compression plating with lag screws in PPF around cemented hip stems and discussed risk factors for fixation failure. In their series, 37 patients, operatively treated patients, had unsatisfactory results in 56% of cases compared with 80% in those treated nonoperatively. They concluded that ORIF of an unstable fracture with a long stemmed prosthesis provided the best results and emphasized that internal fixation implants should extend beyond the tip of the stem to avoid a stress riser [22]. Other authors also found that rigid plate fixation could produce better outcomes than non-operative treatment or revision arthroplasty alone [23]. Nonetheless, complications remained high with rates of implant loosening and infection up to 20% [24].
Serocki et al. were the first to specifically discuss AO/ASIF techniques using broad compression plates to create long fixation constructs and achieve rigid fixation in PPF with stable implants. They reported a union rate of 90% with the majority of their patients reaching pre-injury functional outcomes. However, they were raised the concern that screws placed around cemented stems could compromise the cement mantle and stem stability [25]. Additional studies utilizing AO/ASIF techniques with or without cortical strut allograft achieved high rates of union and favorable functional outcomes either in isolation or as a supplement to revision to a longer stem [26, 27]. Sen et al. described the use of a long limited-contact dynamic compression plate (LC-DCP) with trochanteric fixation with wires or unicortical screws to achieve a greater than 80% union rate around stable hip stems. In this series, all patients were treated with open reduction, and the authors emphasized the importance of adequately spanning the fracture with long fixation both proximally into the trochanter and distally with at least 4 or 5 cortical screws. They also emphasized the importance of minimizing soft tissue stripping to preserve blood supply to the fracture [28]. Subsequent biomechanical studies evaluating single versus double plating or strut allografting with shorter constructs concluded that biplanar fixation with allograft provided the best rotational and bending support for Vancouver B1 type fractures. However, the authors raised concerns that the excessive amount of soft-tissue stripping required for 90 degree fixation could impede healing [29,30,31].
Minimally Invasive Osteosynthesis
The goal of internal fixation is to achieve a balanced fixation construct with minimal injury to the soft tissues to achieve fracture union and early functional rehabilitation [32]. Minimally invasive osteosynthesis (MIO) is a concept of biologically respectful internal fixation to achieve these goals via indirect reduction, preservation of the fracture hematoma and periosteum, and limited exposures [33, 34]. The ideal implant to achieve this in lower extremity long bone fractures is the intramedullary nail; however, the presence of a canal-occluding implant such as a hip stem or posterior-stabilized TKA femoral component necessitates plate fixation. In both the tibia and the femur, the development of indirect reduction techniques, submuscular plating, and percutaneous instrumentation have shown less impact on fracture vascularity, fewer soft-tissue complications, and improved union rates compared to conventional open plating [35,36,37,38,39,40,41,42,43,44,45,46,47]. Furthermore, the development of locking screws in conjunction with submuscular plates allows for the creation of a “internal external fixator” which achieves a long working length to span the fracture, stable fixation with both bending and rotational control, and short segment fixation in soft bone. The use of rigid unicortical screws avoids compromising the cement mantle with better preservation of the soft tissues [48]. However, these techniques are often technically challenging as the reduction and implant fixation often occur simultaneously and require a skilled assistant with heavy use of fluoroscopy [49].
Femur Fractures Around a Hip Stem
Ricci et al. reported the first large series of periprosthetic femur fractures treated with MIO techniques. Their cohort included fractures of the femur with an occluded femoral canal (i.e., THA, stemmed TKA, or prior intramedullary device). All patients were treated with indirect reduction and percutaneous submuscular placement of a locking 4.5 mm broad LC-DCP (Synthes; Paoli, PA) through the distal lateral knee and proximal lateral thigh incisions with care taken to maintain a skin bridge over the fracture site itself to respect the fracture hematoma and soft tissues. Cables were passed extraperiosteally around the implant-zone of the femur with a minimum of six screw holes and fixation into the greater trochanter using screws [50•]. They also recommended long plates that end beyond the stem to prevent a stress riser, even going as far to suggest that surgeons should consider spanning the entire length of the femur in osteoporotic patients, especially those patients with ipsilateral TKA and THA. Patients were allowed toe-touch weight bearing after surgery. All fractures united at an average of 3 months with only one acute infection and no loss of alignment. The authors attributed their success rate to preservation of the soft tissue envelope around the fracture [51].
Anatomically contoured femoral locking plates have also been increasingly utilized in the management of both Vancover B1 and C type fractures. Ehlinger et al. described the benefits and challenges of the anatomically contoured nature of the less invasive skeletal stabilization plate (LISS; Synthes, USA, Paoli, PA) to assist with reduction of Vancouver C and B1 fractures at the tip of a hip stem [52]. In their subsequent clinical series of 37 patients, 36 achieved union, 2 developed an infection, and 3 developed mechanical complications. One resulted from failure to recognize a loose hip stem, one resulted from a malreduction and inadequate fixation, and the last from a high concentration of locking screws at the fracture site [53]. Additional series using both the LISS plate and the non-contact bridging plate-distal femur (NCB-DF; Zimmer Inc., Warsaw, IN) have shown similarly high union and low infection rates [54, 55•, 56].
Femur Fractures Above A TKA
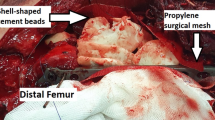
Supracondylar femoral fractures above a well-fixed posterior stabilized (PS) TKA can often be approached in the same manner as a distal femur fracture without an implant. The goal is to restore appropriate length, rotation, and alignment indirectly with skeletal traction, well-placed bumps, or even “joystick” schanz pins for more direct control of the distal fragment. Temporary external fixation or the femoral distractor can also be utilized to achieve adequate length, alignment, and rotation provisionally. The submuscular plate through a relatively small distal window followed by percutaneous insertion of diaphyseal screws (Fig. 1). It is important to avoid malrotation of the distal segment and malalignment of the plate on the bone [57]. Plates that allow for variable angle locking screw insertion and very distal placement of the plate, essentially against the prosthesis, may improve screw purchase in the short distal metaphyseal peri-implant fragment [55•, 57]. The majority of modern peri-articular locking plates are precontoured to assist with placement and reduction; however, variations in arthroplasty implant placement and prior bone cuts may have altered the patient’s native anatomy, and over-reliance on the plate contour for reduction may lead to malreductions or improper plate placement. Additionally, care must be taken to assess screw options in the distal fragment as the prosthesis may limit the options for screw placement. Knowledge of implant options and appropriate preoperative planning is critical to a successful outcome and may determine if the patient is even a candidate for fracture fixation.
Cruciate-retaining (CR) TKA may permit retrograde intramedullary nailing of PPF above a TKA as the femoral canal is not completely occluded by the implant. Despite this benefit, however, the box is often more posterior than the standard start site for a retrograde femoral nail which could result in a hyperextension or translation deformity. One can consider utilizing a bending iron to bend the distal aspect of the femoral nail to prevent the deformity. Additionally, the opening may not be large enough to accommodate an appropriately sized nail. For that reason, a detailed understanding of the femoral component specifications is crucial [58]. Some surgeons have described widening or even creation of the opening with metal-cutting tools at the expense of a large amount of metal debris [59]. Similarly, some have described cutting of the nail to move the interlocking screws more distally and maximize distal screw purchase [60].
In addition to the technical challenges related to the prosthesis, nailing of supracondylar fractures above a CR TKA is subject to the same difficulties with nailing very distal femur fractures. The wide metaphyseal fragment and poor bone quality may predispose the fracture to malalignment as the nail cannot be used as a reduction tool, and techniques such as blocking screws or joysticks may be required [61]. Furthermore, because of scarring of the fat pad, inferior location of the open box, and concern over metal debris from reaming through the box, retrograde nailing of a fracture above a CR TKA may be difficult with a small percutaneous incision at the patella and require an open approach to the notch via a medial parapatellar approach.
Bong et al. studied the biomechanical characteristics of the LISS plate and supracondylar nail for these fractures and found that while the LISS plate resisted valgus forces well, the nail ultimately had less fracture displacement to varus, medial translation, torsional, and sagittal loading [62]. In contrast, Althausen et al. found greater varus displacement in patients treated with supracondylar nails compared to LISS plating in a small clinical series of 12 patients, though all patients achieved union [63]. Ricci et al. reported on the clinical outcome of 53 patients who underwent locked platting above a well-fixed TKA and found that 75% of patients were able to achieve successful union [56]. Gliatis et al. described a small series of 10 fractures in 9 patients with supracondylar femur fractures above a stable posterior-cruciate retaining TKA treated with a retrograde nail. Of these, one patient had a malunion of 35° of valgus which was revised to a stemmed TKA, while the remaining nine fractures healed uneventfully within 12 weeks [64]. As such, while there is a paucity of reported clinical comparisons, both techniques appear to yield promising results provided that the technical challenges are appropriately addressed.
Tibial Plating
Tibial fractures below a TKA are less common than femur fractures and present some unique challenges. While the surgeon should still approach these injuries with the same methodical decision making regarding fracture location, stem fixation, and bone quality, the tibia has the added complexity of delicate skin and a less tolerant soft-tissue envelope. The tissues may not tolerate large exposures or multiple incisions on the medial side of the tibia, particularly older patients with dermal atrophy.
In a well-fixed tibial component where the fracture is very near or around the stem, the use of MIO techniques is very similar to those used in complex tibial fracture [47, 65]. Restoration of alignment is paramount to any fixation technique. This may be achieved manual traction, judicious use of bumps, external fixation, or large femoral distractor [66]. An anterolateral approach to the proximal tibia with maintenance of a distal skin bridge relative to the TKA incision that is at least half the length of the shortest incision to avoid skin necrosis (2:1 length-to-width ratio). This allows submuscular insertion of an anatomically contoured locking plate along the lateral tibial cortex [67]. Percutaneous diaphyseal fixation minimizes soft tissue trauma. If there is extensive medial comminution or concern for instability, percutaneous insertion of a medial plate may preserve the thin medial skin while providing crucial resistance against varus collapse [47]. Once again, fracture fixation must extend well beyond the tip of the tibial stem with at least eight cortices of fixation utilizing every other hole to maximize the working length of the plate.
Tibial Nailing
Diaphyseal fractures well below a primary TKA or unicondylar knee replacement can be treated with a tibial nail. Because of the location of the tibial component, especially the keel, the traditional infrapatellar nail insertion technique may have to be modified. The insertion point must be more distal, and pointed angled hand reamers are required (Fig. 2). Additionally, the surgeon must ensure careful development of the start site as well as insertion of the guidewire to avoid the deep and posterior cortex. A traditional infrapatellar approach or a semi-extended lateral parapatellar approach as described by Kubiak et al. may be used [68•]. A medial parapatellar approach may also be used. Like a retrograde nailing in a supracondylar femoral TKA PPF, if the surgeon cannot achieve an appropriate start site with a small percutaneous incision, a full arthrotomy may be required. Because of the low, anterior start site, the surgeon may use a 9 mm or smaller nail and may need to curve the distal 1/3 of the nail anteriorly with a table top bender to avoid abutment on the posterior cortex. Haller et al. reported on his technique for nailing in a small series of four patients, all of whom healed and returned to baseline function [69].
a Tibial shaft fracture below well-fixed TKA. Note that the patient has a prior distal femoral locking plate. b Awl used for semi-extended lateral parapatellar approach for tibial nailing. Note that start site has been moved slightly distal to a traditional start site to accommodate the prosthesis. c 6 weeks post-op. The patient was allowed progressive weight bearing
Biomechanical Considerations
While many would agree that preservation of the soft tissues during internal fixation is a critical factor in promoting bony union, there is continued controversy regarding the appropriate fixation construct regarding screw choice, location, and plate length. In fractures that are remote from the prosthesis, it is tempting to consider a smaller implant to avoid the fixation around the stem. In their analysis of ipsilateral stemmed arthroplasties in the femur, Soenen et al. found that an interprosthetic distance of at least 11 cm was the threshold at which strain and fracture risk increased dramatically, in four-point bending [70]. However, maintaining an interprosthetic length of 11 cm could compromise the construct length required for adequate stabilization of the fracture itself. For these reasons, we recommend that the fixation construct should always bridge the prosthesis.
In revision arthroplasty, the optimum stem length for intramedullary bypass of a defect should be 2–3 cortical diameters to minimize stress risers [71]. Prior to the development of MIO plating, the length of the fixation construct was limited by the amount of soft tissue stripping. With the advent of submuscular plate insertion, limited exposures, and percutaneous screw insertion, plate length may be increased while preserving the soft tissues, though these techniques have a steep learning curve [72]. For periprosthetic fracture fixation, many authors advocate for a longer construct transition, with at least 4–6 screw holes of fixation around a well-fixed hip stem including fixation into the greater trochanter and at least eight cortices of fixation distal to the fracture [50•, 73]. Some surgeons have suggested spanning the entire native bone in osteoporotic patients [50•].
Locking screws increase construct rigidity; however, it is less clear how much rigidity is required to achieve union. In fractures of native bone in distal femurs, all-locking constructs have been shown to significantly increase the likelihood of nonunion, and management of the fracture working length (i.e., distance between the nearest fixation points to the fracture zone) has the greatest impact on the magnitude and direction of fracture motion [74,75,76]. A screw closest to the fracture zone significantly reduces shear stresses and may promote callus formation at the fracture [74,75,76], and a nonlocking screw at that location significantly reduces plate stress [71,72,73, 77•]. For optimum fixation, Beltran et al. recommended that no more than 50% of the screw holes be filled in the diaphyseal segment and that four bicortical screws are adequate [78]. Furthermore, because of reports of thigh pain and concern for periprosthetic fracture from locking screws at the end of the plate, the last screw should have a nonlocking bicortical screw or unicortical locking screw if it is in native diaphysis [79].
A recent development in screw design that attempts to address excess rigidity and yet maintain a fixed-angle construct is the Far cortical locking screw, in which the proximal cortex is over-drilled or the screw has a reduced inner diameter proximally while the head is locked into the plate like a traditional locking screw [80]. This creates unicortical fixation at the far cortex which increases the flexibility of the construct and allows for more symmetric axial motion at the near and far cortices. Early animal studies suggest that this may improve the volume and morphology of callus formation [80,81,82]; however, there is a paucity of human clinical studies.
Functional Outcomes
The overarching goal for any fracture care is to achieve early mobilization and functional recovery. This is particularly important in geriatric patients as they are at higher risk of complication from prolonged immobilization. Early mobilization has been encouraged following most reports utilizing minimally invasive techniques for periprosthetic fracture repair; however, a variety of bracing and weight bearing protocols have been described ranging from immediate weight bearing as tolerated with crutch [28] to knee immobilization and protected weight bearing with walker for 3 months [51, 57, 63]. At our institution, patients are encouraged to begin gentle active and passive range of motion of the affected limb. They are encouraged to partially weight bear or weight bear as tolerated with walker with a goal of full weight bearing by 6–8 weeks after surgery.
Despite decreased complications and increased union rates, a full functional recovery is unlikely for most patients. Though many patients are encouraged to mobilize and bear full or partial weight on the extremity soon after surgery, the 1-year mortality for these fractures is 15–20%, with fewer than 50% of surviving patients returning to their prior level of activity and independence [54, 55, 83]. Myers, Weber et al. evaluated the mortality in a series of 283 patients with distal femur fractures at their institution and included both native and periporthestic fractures. The overall mortality at 1 year was 13.4% for all distal femur fractures. Additionally, the periprosthetic fracture patients had increased mortality with increasing delay to definitive fixation. The risk of mortality in the periprosthetic cohort was 9.7% [84]. Gitajn et al. examined the mortality of patients with Vancouver B periprosthetic femur fractures. They demonstrated a similar 1-year mortality rate of 13% and a 5-year mortality of 46% [85].
Like geriatric hip fractures, much of this is likely related to underlying frailty in addition to the stress of trauma, surgery, and rehabilitation. As such, it is important to counsel patients and their families on these outcomes so that they can be adequately prepared.
Conclusion
In summary, MIO techniques and newer implant designs have significantly improved our ability to manage periprosthetic femur and tibial fractures. Early results of this technically demanding approach, when appropriately applied, can achieve lower complication rates, improved healing, and quicker return to weight bearing. The optimal implant type, length, screw density, and screw type have not been determined, but long plates with spaced screws and overlap of the prosthesis have gained wide acceptance. Regardless of implant choice and surgical approach, a thorough evaluation of implant stability prior to surgery, respect for the soft tissues, and restoration of anatomic length, alignment, and rotation are the critical factors for successful outcomes in these complex injuries. Despite recent advances, many patients will have persistent functional deficits and the mortality risk is significant. These factors should be discussed in depth with the patient and family.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major Importance
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–5.
Lewallen DG, Berry DJ. Periprosthetic fracture of the femur after total hip arthroplasty: treatment and results to date. Instr Course Lect. 1998;47:243.
Berry DJ. Epidemiology: hip and knee. Orthop Clin. 1999;30(2):183–90.
Figgie MP, Goldberg VM, Figgie HE III, Sobel M. The results of treatment of supracondylar fracture above total knee arthroplasty. J Arthroplast. 1990;5(3):267–76.
Healy WL, Siliski JM, Incavo SJ. Operative treatment of distal femoral fractures proximal to total knee replacements. JBJS. 1993;75(1):27–34.
Ritter MA, Faris PM, Keating EM. Anterior femoral notching and ipsilateral supracondylar femur fracture in total knee arthroplasty. J Arthroplast. 1988;3(2):185–7.
Giannoudis PV, Kanakaris NK, Tsiridis E. Principles of internal fixation and selection of implants for periprosthetic femoral fractures. Injury. 2007;38(6):669–87.
Duwelius PJ, Schmidt AH, Kyle RF, Talbott V, Ellis TJ, Butler JB. A prospective, modernized treatment protocol for periprosthetic femur fractures. Orthop Clin. 2004;35(4):485–92.
Brady OH, Kerry R, Masri BA, Garbuz DS, Duncan CP. The Vancouver classification of Periprosthetic fractures of the hip: a rational approach to treatment. Tech Orthop. 1999;14(2):107–14.
Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability of validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplast. 2000;15(1):59–62.
Pike J, Davidson D, Garbuz D, Duncan CP, OʼBrien PJ, Masri BA. Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. Am Acad Orthop Surg. 2009;17(11):677–88.
Rorabeck CH, Taylor JW. Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin. 1999;30(2):209–14.
Hanssen AD, Stuart MJ. Treatment of periprosthetic tibial fractures. Clin Orthop Relat Res. 2000;380:91–8.
Duncan C, Haddad F. The unified classification system (UCS): improving our understanding of periprosthetic fractures. Bone Joint J. 2014;96(6):713–6.
Unified Classification System for Periprosthetic Fractures (UCPF). J Orthop Trauma. 2018;32:S141–4.
Scott RD, et al. Femoral fractures in conjunction with total hip replacement. J Bone Joint Surg Am. 1975;57(4):494–501.
Parrish TF, Jones JR. Fracture of the femur following prosthetic arthroplasty of the hip: report of nine cases. JBJS. 1964;46(2):241–8.
Taylor MM, Meyers MH, Harvey JJ. Intraoperative femur fractures during total hip replacement. Clin Orthop Relat Res. 1978;137:96–103.
Khan M, O'Driscoll M. Fractures of the femur during total hip replacement and their management. Bone Joint J. 1977;59(1):36–41.
Barfod G, Steen Jensen J, Hansen D, Larsen E, Menck H, Olsen B, et al. Hemi-arthroplasty of the hip followed by ipsilateral fracture of the femoral shaft. Injury. 1986;17(2):104–6.
Abdu WA, Lurie JD, Spratt KF, Tosteson ANA, Zhao W, Tosteson TD, et al. Degenerative spondylolisthesis: does fusion method influence outcome? Four-year results of the spine patient outcomes research trial. Spine (Phila Pa 1976). 2009;34(21):2351–60.
Johansson J, et al. Fracture of the ipsilateral femur in patients wih total hip replacement. J Bone Joint Surg Am. 1981;63(9):1435–42.
Cooke P, Newman J. Fractures of the femur in relation to cemented hip prostheses. J Bone Joint Surg Br. 1988;70(3):386–9.
Beals RK, Tower SS. Periprosthetic fractures of the femur: an analysis of 93 fractures. Clin Orthop Relat Res. 1996;327:238–46.
Serocki JH, Chandler RW, Dorr LD. Treatment of fractures about hip prostheses with compression plating. J Arthroplast. 1992;7(2):129–35.
Wang J-W, Wang C-J. Periprosthetic fracture of the femur after hip arthroplasty: the clinical outcome using cortical strut allografts. J Orthop Surg. 2000;8(1):27–31.
Tsiridis E, Narvani AA, Timperley JA, Gie GA. Dynamic compression plates for Vancouver type B periprosthetic femoral fractures: a 3-year follow-up of 18 cases. Acta Orthop. 2005;76(4):531–7.
Sen R, Prasad P, Kumar S, Nagi O. Periprosthetic femoral fractures around well fixed implants: a simple method of fixation using LC-DCP with trochanteric purchase. Acta Orthop Belg. 2007;73(2):200–6.
Kuptniratsaikul S, et al. Plate-screw-wiring technique for the treatment of periprosthetic fracture around the hip: a biomechanical study. J Med Assoc Thai. 2001;84:S415–22.
Wilson D, Frei H, Masri BA, Oxland TR, Duncan CP. A biomechanical study comparing cortical onlay allograft struts and plates in the treatment of periprosthetic femoral fractures. Clin Biomech. 2005;20(1):70–6.
Chandler H, Tigges R. The role of allografts in the treatment of periprosthetic femoral fractures. Instr Course Lect. 1998;47:257.
Reudi T, Buckley R, Moran C. AO Principles of Fracture Management. New York: Thieme-Verlag.; 2007.
Perren SM, Mane K, Pohler O, Predieri M, Steinemann S, Gautier E. The limited contact dynamic compression plate (LC-DCP). Arch Orthop Trauma Surg. 1990;109(6):304–10.
Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg (Br). 2002;84(8):1093–110.
Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate Osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13(6):401–6.
Collinge CA, Sanders RW. Percutaneous plating in the lower extremity. J Am Acad Orthop Surg. 2000;8(4):211–6.
Krettek C, et al. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury. 1997;28(Supplement 1):Sa20–30.
Bone LB. Indirect fracture reduction: a technique for minimizing surgical trauma. J Am Acad Orthop Surg. 1994;2(5):247–54.
Mast J, Jakob R, Ganz R. Planning and reduction technique in fracture surgery, vol. xiii. Berlin: Springer-Verlag.; 1989. 254 p.
Schutz M, et al. Use of the less invasive stabilization system (LISS) in patients with distal femoral (AO33) fractures: a prospective multicenter study. Arch Orthop Trauma Surg. 2005;125(2):102–8.
Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003;408(408):286–91.
Stannard JP, et al. Fracture stabilization of proximal tibial fractures with the proximal tibial LISS: early experience in Birmingham, Alabama (USA). Injury. 2003;34(Suppl 1):A36–42.
Gosling T, et al. Less invasive stabilization of complex tibial plateau fractures: a biomechanical evaluation of a unilateral locked screw plate and double plating. J Orthop Trauma. 2004;18(8):546–51.
Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system - surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18(8):509–20.
Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury. 2004;35(6):615–20.
Collinge C, Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma. 2010;24(1):24–9.
Krettek C, Gerich T, Miclau T. A minimally invasive medial approach for proximal tibial fractures. Injury. 2001;32(Suppl 1):SA4–13.
Fulkerson E, Koval K, Preston CF, Iesaka K, Kummer FJ, Egol KA. Fixation of periprosthetic femoral shaft fractures associated with cemented femoral stems: a biomechanical comparison of locked plating and conventional cable plates. J Orthop Trauma. 2006;20(2):89–93.
Kregor P, et al. Distal femoral fracture fixation utilizing the less invasive stabilization system (LISS): the technique and early results. Injury. 2001;32:32–47.
• Ricci WM, et al. Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. Surgical Technique. J Bone Joint Surg Am. 2006;88 Suppl 1(Pt 2):275–82. Well illustrated and described technique for peri-implant and peri-prosthetic fixation of femur fractures.
Ricci WM, et al. Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. JBJS. 2005;87(10):2240–5.
Ehlinger M, Bonnomet F, Adam P. Periprosthetic femoral fractures: the minimally invasive fixation option. Orthop Traumatol Surg Res. 2010;96(3):304–9.
Ehlinger M, Adam P, di Marco A, Arlettaz Y, Moor BK, Bonnomet F. Periprosthetic femoral fractures treated by locked plating: feasibility assessment of the mini-invasive surgical option. A prospective series of 36 fractures. Orthop Traumatol Surg Res. 2011;97(6):622–8.
O'toole RV, et al. Low complication rate of LISS for femur fractures adjacent to stable hip or knee arthroplasty. Clin Orthop Relat Res. 2006;450:203–10.
• El-Zayat B, et al. NCB-plating in the treatment of geriatric and periprosthetic femoral fractures. Orthop Traumatol Surg Res. 2012;98(7):765–72. Good technical description and clinical series using the periperosthetic-specific NCB-plate fixation system for lower extremity fractures.
Ricci WM, Loftus T, Cox C, Borrelli J. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma. 2006;20(3):190–6.
Kregor P, Hughes J, Cole P. Fixation of distal femoral fractures above total knee arthroplasty utilizing the less invasive stabilization system (LISS). Injury. 2001;32:64–75.
Su ET, DeWal H, Di Cesare PE. Periprosthetic femoral fractures above total knee replacements. Am Acad Orthop Surg. 2004;12(1):12–20.
Maniar R, et al. Supracondylar femoral fracture above a PFC posterior cruciate-substituting total knee arthroplasty treated with supracondylar nailing: a unique technical problem. J Arthroplast. 1996;11(5):637–9.
McLaren AC, Dupont JA, Schroeber DC. Open reduction internal fixation of supracondylar fractures above total knee arthroplasties using the intramedullary supracondylar rod. Clin Orthop Relat Res. 1994;302:194–8.
Ricci WM, O'Boyle M, Borrelli J, Bellabarba C, Sanders R. Fractures of the proximal third of the tibial shaft treated with intramedullary nails and blocking screws. J Orthop Trauma. 2001;15(4):264–70.
Bong MR, Egol KA, Koval KJ, Kummer FJ, Su ET, Iesaka K, et al. Comparison of the LISS and a retrograde-inserted supracondylar intramedullary nail for fixation of a periprosthetic distal femur fracture proximal to a total knee arthroplasty. J Arthroplast. 2002;17(7):876–81.
Althausen PL, Lee MA, Finkemeier CG, Meehan JP, Rodrigo JJ. Operative stabilization of supracondylar femur fractures above total knee arthroplasty: a comparison of four treatment methods. J Arthroplast. 2003;18(7):834–9.
Gliatis J, Megas P, Panagiotopoulos E, Lambiris E. Midterm results of treatment with a retrograde nail for supracondylar Periprosthetic fractures of the femur following Total knee arthroplasty. J Orthop Trauma. 2005;19(3):164–70.
Boldin C, Fankhauser F, Hofer HP, Szyszkowitz R. Three-year results of proximal tibia fractures treated with the LISS. Clin Orthop Relat Res. 2006;445:222–9.
Mast J, Jakob R, Ganz R. Planning and reduction technique in fracture surgery. Berlin: Springer-Verlag Berlin Heidelberg; 1989.
Mathes S, Nahai F. The reconstructive triangle: a paradigm for surgical descision making. In: Mathes SJ, Nahai F, editors. Reconstructive surgery: principles, anatomy, & technique. 1st ed. New York: Churchill Livingstone; 1997. p. 9–39.
• Kubiak EN, Widmer BJ, Horwitz DS. Extra-articular technique for semiextended tibial nailing. J Orthop Trauma. 2010;24(11):704–8. Practical discussion of the technique for nailing tibia fractures distal to a total knee arthroplast.
Haller JM, Kubiak EN, Spiguel A, Gardner MJ, Horwitz DS. Intramedullary nailing of tibial shaft fractures distal to total knee arthroplasty. J Orthop Trauma. 2014;28(12):e296–300.
Soenen M, Baracchi M, de Corte R, Labey L, Innocenti B. Stemmed TKA in a femur with a total hip arthroplasty: is there a safe distance between the stem tips? J Arthroplast. 2013;28(8):1437–45.
Larson J, Chao E, Fitzgerald R. Bypassing femoral cortical defects with cemented intramedullary stems. J Orthop Res. 1991;9(3):414–21.
Kregor PJ, Hughes JL, Cole PA. Fixation of distal femoral fractures above total knee arthroplasty utilizing the Less Invasive Stabilization System (L.I.S.S.). Injury. 2001;32:64–75.
Berlusconi M, et al. Locking compression plates (LCP) for treatment of periprosthetic fractures of the hip. J Orthop Trauma. 2004;18(Suppl. 9):S20–1.
Harvin WH, Oladeji LO, Della Rocca GJ, Murtha YM, Volgas DA, Stannard JP, et al. Working length and proximal screw constructs in plate osteosynthesis of distal femur fractures. Injury. 2017;48(11):2597–601.
McLachlin S, Kreder H, Ng M, Jenkinson R, Whyne C, Larouche J. Proximal screw configuration alters peak plate strain without changing construct stiffness in comminuted supracondylar femur fractures. J Orthop Trauma. 2017;31(12):e418–24.
Elkins J, Marsh JL, Lujan T, Peindl R, Kellam J, Anderson DD, et al. Motion predicts clinical callus formation: construct-specific finite element analysis of supracondylar femoral fractures. J Bone Joint Surg Am. 2016;98(4):276–84.
• Cui, S., et al., Locked plating of comminuted distal femur fractures: does unlocked screw placement affect stability and failure? J Orthop Trauma, 2014. 28(2): p. 90–6. While this article does not specifically discuss periprosthetic fractures, the techniques and pitfalls it describes for minimally invasive fixation of distal femoral fractures are very applicable.
Beltran MJ, Gary JL, Collinge CA. Management of distal femur fractures with modern plates and nails: state of the art. J Orthop Trauma. 2015;29(4):165–72.
Bottlang M, Doornink J, Byrd GD, Fitzpatrick DC, Madey SM. A nonlocking end screw can decrease fracture risk caused by locked plating in the osteoporotic diaphysis. J Bone Joint Surg Am. 2009;91(3):620–7.
Bottlang M, Feist F. Biomechanics of far cortical locking. J Orthop Trauma. 2011;25(Suppl 1):S21–8.
Bottlang, M., et al., Effects of construct stiffness on healing of fractures stabilized with locking plates. J Bone Joint Surg Am, 2010. 92 Suppl 2(Supplement_2): p. 12–22.
Bottlang M, Tsai S, Bliven EK, von Rechenberg B, Klein K, Augat P, et al. Dynamic stabilization with active locking plates delivers faster, stronger, and more symmetric fracture-healing. J Bone Joint Surg Am. 2016;98(6):466–74.
Anakwe RE, Aitken SA, Khan LA. Osteoporotic periprosthetic fractures of the femur in elderly patients: outcome after fixation with the LISS plate. Injury. 2008;39(10):1191–7.
Myers P, Laboe P, Johnson KJ, Fredericks PD, Crichlow RJ, Maar DC, et al. Patient mortality in geriatric distal femur fractures. J Orthop Trauma. 2018;32(3):111–5.
Gitajn IL, Heng M, Weaver MJ, Casemyr N, May C, Vrahas MS, et al. Mortality following surgical Management of Vancouver B Periprosthetic Fractures. J Orthop Trauma. 2017;31(1):9–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Carol Lin and Milton Little declare no conflict of interest. Charles Moon reports personal fees from Stryker as a trauma consultant, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Geriatric Orthopedics
Rights and permissions
About this article
Cite this article
Lin, C.A., Little, M.T.M. & Moon, C.N. Minimally Invasive Osteosynthes of Periprosthetic Fractures in the Lower Extremity. Curr Geri Rep 7, 256–263 (2018). https://doi.org/10.1007/s13670-018-0259-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-018-0259-8