Abstract
Purpose of Review
The purpose of this article is to present a more recent radiological review to pulmonologists, radiologists and other clinicians of: typical and atypical manifestations of intrathoracic sarcoidosis, and highlighting its mimic-drug induced sarcoid like reaction.
Recent Findings
There is an association between immunotherapy and the development of sarcoid-like reactions. Clinicians and radiologists should be aware of this entity.
Summary
Sarcoidosis is a multisystem inflammatory disease, of unknown etiology that is characterized by non caseating granulomas. It most commonly involves the lungs and lymph nodes. The common features of this entity have been extensively described in literature; however, 25–30% of cases present with atypical features. This review addresses the different manifestations of pulmonary sarcoidosis, highlighting the atypical appearances, which maybe misdiagnosed in the absence of tissue diagnosis. Radiologists should not hesitate to recommend tissue sampling in the setting of atypical findings and for definite diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sarcoidosis is a multisystem inflammatory disease of unknown etiology characterized by non caseating granulomas [1, 2]. It typically involves the lymph nodes and lungs. However, it can involve virtually any organ, including the central nervous system, heart, bones, and skin. Sarcoidosis can affect all patients irrespective of age, sex, or race. In the USA, it is seen predominantly in the African American population [3]. The annual incidence of sarcoidosis is 10.0 per 100,000 population [4]. Reported peak incidence in both sexes is between the ages of 20 and 34, with a second peak in older women [5]. The accumulated lifetime risk of sarcoidosis has been reported as 1.3% for women and almost 1% for men [5].
In this review, we will discuss parenchymal and mediastinal manifestations of sarcoidosis with special focus on atypical appearances of sarcoid, which can occasionally pose a dilemma for the clinician and radiologist. There is no noninvasive confirmatory laboratory exam for sarcoid. Tissue pathology is necessary to demonstrate presence of non caseating granulomas. However, other granulomatous disorders have to be excluded prior to its diagnosis.
The Siltzbach/Scadding staging system introduced in 1961 classifies sarcoid into five stages and continues to be used even today. These are the following:
-
Stage 0, normal appearance at chest radiography; approximately 5–10% of patients have stage 0 disease at presentation [6].
-
Stage 1, lymphadenopathy only.
-
Stage 2, lymphadenopathy and parenchymal lung disease.
-
Stage 3, parenchymal lung disease only; 10–15% of patients at presentation.
-
Stage 4, pulmonary fibrosis 5% of patients at presentation [5].
However, there are many limitations to this system. Most prominently, it has no bearing on the extra-parenchymal manifestations of disease including ocular or skin involvement. It also does not correlate with severity of pulmonary function tests [7]. Newer classification types based on phenotypic clusters are being proposed [8].
Stage 1: Hilar and Mediastinal Lymphadenopathy Only
At the time of presentation, approximately 25–65% of patients have stage 1 disease [6]. It is characterized by paratracheal and bilateral hilar adenopathy. Two view, frontal posteroanterior (PA) and lateral, radiographs are the initial study of choice. On chest X-ray, mediastinal lymphadenopathy in sarcoidosis produces a characteristic 1-2-3 sign. “1” signifies the right paratracheal lymph nodes. “2 and 3 “represent hilar adenopathy (Fig. 1a). On the lateral radiograph, there is encasement of the lucent bronchi by surrounding radiopaque lymph nodes. This is also known as the “doughnut” sign (Fig. 1b).
While IV contrast is not typically required for mediastinal adenopathy, it can help better delineate hilar lymph nodes from surrounding vessels in the hila (Fig. 2a, b). Lymph nodes in untreated sarcoidosis are typically homogenous in appearance [9]. Internal necrosis characterized by central areas of low attenuation within lymph nodes is not a typical feature of sarcoidosis. If present, other entities such as tuberculosis or neoplasms such as squamous cell carcinoma should be considered. Over time, these lymph nodes may calcify. Patterns of calcification include egg shell, punctate and popcorn calcification appearance [10].
With the recent advent of immunotherapy drugs, there is an increasing incidence of “sarcoid-like reaction” (SLR) [11••]. This is often seen on PET-CT with presence of new FDG avid mediastinal lymph nodes following treatment and represents a benign entity (Fig. 3a, b). Some helpful pointers to distinguish these lymph nodes from malignant nodal disease include the following: These lymph nodes are typically seen after initiation of treatment, may decrease in size on subsequent studies, and are seen in multiple nodal stations as opposed to being localized only in the site of lymphatic drainage of tumor. It is important for oncologists and radiologists to be aware of this entity on imaging, to avoid misdiagnosis of disease progression. Cheshire et al. reported a series of patients who developed SLR, while taking pembrolizumab, an immune-modulated checkpoint inhibitor for melanoma [11••].
a PET coronal image demonstrates sarcoid-like reaction after initiation of immunotherapy with radiotracer avid lymph nodes in bilateral hila and right paratracheal regions (arrows). Additionally seen is a hepatic metastasis in the right hepatic lobe and gastric lesion, both of which had improved following initiation of immunotherapy in comparison with prior imaging (not shown). b Fused PET CT demonstrates previously described mediastinal lymph nodes and extrathoracic disease of the liver and stomach
Stage 2: Lymphadenopathy and Active Pulmonary Disease
At the time of presentation, approximately 25–30% of patients present with stage 2 disease [6]. Besides adenopathy in the various mediastinal stations described previously, stage 2 disease manifestations include pulmonary involvement. Active pulmonary disease is characterized by perifissural and peribronchovascular lung nodules with an upper lobe predominance (Fig. 4a, b), due to spread of disease via lymphatics [12].
High-resolution CT of the chest is helpful to differentiate active disease present in stages 2 and 3 from pulmonary fibrosis in stage 4 sarcoidosis. Ground-glass opacification, nodules, and alveolar opacities seen with active disease are suggestive of reversible stage 2 or 3 disease [10]. These nodules may coalesce together and result in radiographic appearance described as “sarcoid galaxy” sign, first described by Nakatsu et al. in 2002 [13] (Fig. 5a, b). However this term “galaxy” sign can be seen in pulmonary TB as well [14].
Stage 3: Parenchymal Lung Disease Only
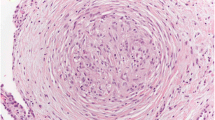
Stage 3 sarcoidosis represents involvement of the lung parenchyma, without nodal enlargement. The pulmonary nodules seen in the lung parenchyma due to sarcoidosis are composed of non caseating granulomas. These are small and vary from 1 to 10 mm, and are typically present in a perilymphatic upper lobe distribution. These small sarcoid nodules are sine qua non of sarcoidosis and are present in 80–100% of patients [9]. As they are perilymphatic, the nodules are present in the subpleural region, along the fissures and the interlobular septa. Perifissural nodules are pathognomonic of sarcoidosis. There is also thickening of the bronchovascular bundles in a perihilar distribution. Nodular thickening of the interlobular septa can be seen in up to 26–89% of patients [9]. They can take a polypoidal configuration. Lymphangitic carcinomatosis has a similar appearance but can be readily distinguished by its asymmetric pattern and involvement of the interlobular and subpleural space as compared with sarcoidosis.
The nodules can then coalesce to form larger nodules, parenchymal opacities, and lastly cavitary nodules (Fig. 6a, b). Sometimes the nodules can give rise to a pattern similar to military TB or hypersensitivity pneumonitis. Lastly, sparse pulmonary nodules can be better identified by using maximum intensity projection (MIP) images [15].
The frequency of ground-glass opacities is variable, and they can be multifocal and upper lobe predominant. Sarcoidosis with ground-glass nodules can be distinguished from interstitial lung disease such as NSIP by the presence of perifissural nodules and lymphadenopathy.
While stage 1 sarcoidosis can undergo spontaneous regression, only 1/3 of patients with stages 2 and 3 undergo regression on imaging [6].
Stage 4: Pulmonary Fibrosis
Pulmonary fibrosis is the “burnt out” and irreversible stage of sarcoidosis (Fig. 7a, b). Stage IV disease is observed in 4.7–15% of sarcoid patients [16]. One characteristic feature of this stage is the posterior displacement of the upper lobe bronchus with volume loss in the superior segment of the upper lobes [17]. This can be associated with bronchial distortion and stenosis. As the disease progresses further, the pattern resembles interstitial lung disease with traction bronchiectasis and honeycombing predominantly involving the upper lobes (Fig. 8). The three distinct patterns in this stage include - bronchial distortion, honeycombing pattern, and a linear pattern; with the bronchial distortion pattern being the commonest. Lung architectural distortion in stage IV disease is reported in 20 to 50% of patients [18]. Central conglomerate masses are seen in up to 60% of patients in stage IV disease [17]. Majority of patients with stage IV sarcoidosis die as a result of respiratory complications, mainly pulmonary hypertension. Shorr et al. analyzed patients in the US transplant registry, and reported prevalence of pulmonary hypertension in stage IV disease was 73.8% [19].
Atypical Presentations
Sarcoidosis can present in myriad ways apart from the typical manifestations described above. Some of them are described below [10].
Large Parenchymal Nodules
Large nodules in sarcoidosis represent coalescent granulomas and are formed around the pulmonary vasculature. The lesion appears as a cavitary lesion with thick walls. Differential considerations include lung carcinoma, and an important differentiating feature is extensive bilateral hilar and mediastinal lymphadenopathy in sarcoidosis which is unusual in lung carcinoma limited to a single cavitary nodule (Fig. 9a, b). Since cavitary sarcoidosis is rare, polyangiitis and superimposed infection should be excluded [9].
Mycetoma though atypical is a well-known complication of stage 4 cystic sarcoidosis. The characteristic appearance of pulmonary aspergillosis is demonstrated on the image-air crescent [10]. Mycetomas can be distinguished readily when they demonstrate the air crescent sign and contents which are seen to gravitate to the dependent portions on prone CT of the chest (Fig. 10a, b).
Ground-Glass Opacities
Ground-glass opacities in sarcoidosis are superimposed on a background of interstitial nodules and accompanied by other abnormalities [10] (Fig. 11a, b). The finding typically reflects the presence of numerous tiny granulomas and is often associated with micronodules.
Pleural Effusions and Pleural Space Lesions
Pleural abnormalities in the form of pleural effusion or thickening are relatively rare and may reflect pleural involvement in sarcoidosis. Pulmonary opacities simulating pleural plaques have also been described, termed “pleural plaque-like opacities” [20].
Tracheal Stenosis and Involvement of the Airway
Sarcoidosis can also involve the entire tracheobronchial airway—including both the large and small airways [10]. It can result in tracheal stenosis. Sarcoidosis may result in nodular bronchial wall thickening or small endobronchial lesions or granulomas, resulting in airway obstruction disease. When involved, the large airways lose their elasticity resulting in bronchiectasis. Small airway disease is manifested as mosaic attenuation and air trapping on HRCT of the chest.
Sarcoid may also result in endobronchial obstruction or extrinsic compression by enlarged lymph nodes which can result in atelectasis (Fig. 12a, b).
Atypical Enlarged Lymph Node Distribution
Atypical appearances include unilateral, solitary, and atypical locations of lymphadenopathy.
Sarcoidosis most commonly causes lymphadenopathy in the hilar, right paratracheal, and aorticopulmonary window stations. Intrathoracic lymphadenopathy without bilateral hilar lymphadenopathy or involvement of atypical locations, such as internal mammary and cardiophrenic angle lymph nodes, is highly unusual in sarcoidosis, and should prompt consideration for other entities such as lymphoma or metastatic disease [9]. Enlarged lymph nodes in sarcoidosis typically maintain shape and uncommonly coalesce while maintaining well-defined borders and preserved adjacent fat planes. Nodal disease associated with sarcoidosis is usually nonnecrotic. When lymph nodes coalesce, or if their margins are blurred, other diagnoses such as lymphoma or metastatic disease should be considered. Mediastinal lymphadenopathy involving multiple nodal stations can also be present in collagen vascular diseases, and other interstitial diseases and lymphoproliferative disorders such as lymphoma. Hence, the interpreting radiologist may rely on lung manifestations on CT of the chest to distinguish these entities from sarcoidosis.
Sarcoid-Like Reaction
The term “sarcoid-like reaction” describes localized reactions rather than the systemic processes seen with sarcoidosis. Sarcoid-like reactions are associated with checkpoint inhibitors such as pembrolizumab, ipilimumab, and nivolumab. Radiologists should be aware of the association between immunotherapy and the development of sarcoid-like reactions to avoid inaccurately ascribing new imaging findings to disease progression.
Pulmonary Hypertension
Patients with stage IV sarcoidosis manifest varying degrees of restrictive and obstructive disease and a decreased diffusing lung capacity for carbon monoxide (DLCO)] on pulmonary function tests [16]. Pulmonary hypertension is typically seen in advanced stages of the disease. On CT, presence of pulmonary hypertension maybe suggested when the main pulmonary artery measures more than 3 cm. The right heart chambers maybe enlarged on CT as well. Pulmonary hypertension in sarcoidosis has a reported prevalence between 1-28% of all patients at rest and up to 43% with exercise [21,22,23].
Conclusion
Diagnosis of sarcoidosis requires a multidisciplinary approach, including clinical, laboratory, and histopathologic correlation with imaging findings. Radiologists must be familiar with the characteristic and atypical findings in sarcoidosis and be attentive to situations that suggest alternative diagnoses. Radiologists should not hesitate to recommend tissue sampling in the setting of atypical findings and for definite diagnosis. The radiologist plays a major role in prompt diagnosis and one that may help reduce patient morbidity and mortality.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Grunewald J, Grutters JC, Arkema EV, Saketkoo LA, Moller DR, Müller-Quernheim J. Sarcoidosis. Sarcoidosis Nat Rev Dis Primers. 2019;5:45. https://doi.org/10.1038/s41572-019-0096-x.
Lashari BH, Raza A, Chan V, Ward W. Sarcoidosis presenting as acute respiratory distress syndrome. Case Reports in Medicine. 2018:Article ID 6465180 4 pages, 2018.
Baughman RP, Field S, Costabel U, Crystal RG, Culver DA, Drent M, et al. Sarcoidosis in America. Analysis based on health care use. Ann Am Thorac Soc. 2016;13:1244–52.
Ungprasert P, Carmona EM, Utz JP, Ryu JH, Crowson CS, Matteson EL. Epidemiology of sarcoidosis 1946-2013: a population-based study. Mayo Clin Proc. 2016;91(2):183–8. https://doi.org/10.1016/j.mayocp.2015.10.024.
Hillerdal G, Nöu E, Osterman K, Schmekel B. Sarcoidosis: epidemiology and prognosis—a 15-year European study. Am Rev Respir Dis. 1984;130(1):29–32.
Siltzbach LE, James DG, Neville E, Turiaf J, Battesti JP, Sharma OP, et al. Course and prognosis of sarcoidosis around the world. Am J Med. 1974;57(6):847–52.
Levy A, Hamzeh N, Maier LA. Is it time to scrap Scadding and adopt computed tomography for initial evaluation of sarcoidosis? F1000Res. 2018;7:F1000 Faculty Rev-600. Published 2018 May 16. https://doi.org/10.12688/f1000research.11068.1.
Culver DA, Baughman RP. It’s time to evolve from Scadding: phenotyping sarcoidosis. The European respiratory journal. 2018;51:1800050. https://doi.org/10.1183/13993003.00050-2018.
Nunes H, Uzunhan Y, Gille T, Lamberto C, Valeyre D, Brillet PY. Imaging of sarcoidosis of the airways and lung parenchyma and correlation with lung function. European Respiratory Journal Sep. 2012;40(3):750–65. https://doi.org/10.1183/09031936.00025212.
Criado E, Sánchez M, Ramírez J, Arguis P, Caralt T, Perea R, et al. Pulmonary sarcoidosis: typical and atypical manifestations at high-resolution CT with pathologic correlation. Radiographics: a review publication of the Radiological Society of North America, Inc. 2010;30:1567–86. https://doi.org/10.1148/rg.306105512.
•• Cheshire SC, Board RE, Lewis AR, Gudur LD, Dobson MJ. Pembrolizumab-induced sarcoid-like reactions during treatment of metastatic melanoma. Radiology. 2018;289(2):564–7. https://doi.org/10.1148/radiol.2018180572This study shows the association between immunotherapy and the development of sarcoid-like reactions, pembrolizumab-induced sarcoid-like reactions during treatment of metastatic melanoma.
Nishimura K, Itoh H, Kitaichi M, Nagai S, Izumi T. Pulmonary sarcoidosis: correlation of CT and histopathologic findings. Radiology. 1993;189:105–9.
Nakatsu M, Hatabu H, Morikawa K, Uematsu H, Ohno Y, Nishimura K, et al. Large coalescent parenchymal nodules in pulmonary sarcoidosis: “sarcoid galaxy” sign. American Journal of Roentgenology. 2002;178(6):1389–93.
Koide T, Tea S. Clinical significance of the “galaxy sign” in a Japanese single-center cohort. Sarcoidosis Vasc Diffuse Lung Dis. 2016;33:247–52.
Gruden J, Ouanounou S, Tigges S, Norris S, Klausner T. Incremental benefit of maximum-intensity-projection images on observer detection of small pulmonary nodules revealed by multidetector CT. American Journal of Roentgenology. 2002;179(1):149–57.
Baughman RP, Teirstein AS, Judson MA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. 2001;164:1885–9.
Abehsera M, Valeyre D, Grenier P et al. Sarcoidosis with pulmonary fibrosis: CT patterns and correlation with pulmonary function. AJR Am J Roentgenol. 2000;174:1751–7.
Akira M, Kozuka T, Inoue Y, Sakatani M. Long-term follow-up CT scan evaluation in patients with pulmonary sarcoidosis. Chest. 2005;127:185–191.
Shorr AF, Davies DB, Nathan SD. Predicting mortality in patients with sarcoidosis awaiting lung transplantation. Chest. 2003;124:922–8.
Lee GM, Pope K, Meek L, Chung JH, Hobbs SB, Walker CM. Sarcoidosis: a diagnosis of exclusion. AJR Am J Roentgenol. 2020;214(1):50–8. https://doi.org/10.2214/AJR.19.21436.
Sulica R, Teirstein AS, Kakarla S, et al. Distinctive clinical, radiographic and functional characteristics of patients with sarcoidosis-related pulmonary hypertension. Chest. 2005;128:1483–9.
Handa T, Nagai S, Miki S, et al. Incidence of pulmonary hypertension and its clinical relevance in patients with sarcoidosis. Chest. 2006;129:1246–52.
Gluskowski J, Hawrylkiewicz I, Zych D, et al. Pulmonary haemodynamics at rest and during exercise in patients with sarcoidosis. Respiration. 1984;46:26–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Maansi Parekh, Rashmi Balasubramanya, and Achala Donuru declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pulmonary Radiology
Rights and permissions
About this article
Cite this article
Parekh, M., Balasubramanya, R., Kumaran, M. et al. Intrathoracic Manifestations of Sarcoidosis: an Imaging Review Highlighting Atypical Features. Curr Pulmonol Rep 9, 74–81 (2020). https://doi.org/10.1007/s13665-020-00255-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-020-00255-x