Abstract
Asthma and chronic obstructive pulmonary disease (COPD) are highly prevalent chronic diseases in the general population. Both are characterized by heterogeneous chronic airway inflammation and airway obstruction. Airway obstruction is typically intermittent and reversible in asthma but is progressive and largely irreversible in COPD. However, there is a considerable pathologic and functional overlap between these two heterogeneous disorders, particularly among the elderly, who may have components of both diseases (asthma–COPD overlap syndrome, ACOS). A new chapter about ACOS is written in Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2014 and Global Initiative for Asthma (GINA) 2014. Here, we review the updates of ACOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Asthma and chronic obstructive pulmonary disease (COPD) are two common diseases in clinical practice, usually COPD is easy to distinguish from asthma, but sometimes the distinction from late-onset asthma in older patients, particularly in ones who smoke, is difficult and may be impossible [1]. We are often confused and bewildered when some older patients with obvious emphysema still have a reversible component of airway obstruction and that some confirmed asthmatic patients might already have lung function loss even when they are young [2]. How to diagnose and treat these patients who share the features both asthma and COPD (asthma–COPD overlap syndrome, ACOS) is a hot debate. Here, we review the updates of ACOS.
British hypothesis and Dutch hypothesis
The controversy on how to distinguish asthma from COPD has lasted for decades, debating whether it is asthma or COPD alone, or if there is another possibility that links to above two diseases. The well-known hypotheses are British hypothesis and Dutch hypothesis, but neither was confirmed nor refused to date [3]. British hypothesis states that asthma and COPD are distinct entities that are developed by distinct mechanisms [4]. They have different types of inflammation (primary differences are lymphocyte subsets, i.e., CD4+ vs CD8+ cells) and structural changes [5] supporting the hypothesis. However, recent study suggested NF-κB play a vital role in the inflammatory response indicating the same underlying genes of two diseases [6], which was not in favor of the hypothesis.
Dutch hypothesis, which was put forward during the first bronchitis symposium in 1961 by Orie and Sluiter, was suggested to use by Fletcher et al. at the Third International Bronchitis Symposium in the Netherlands in September 1969 [2]. Dutch hypothesis holds the primary viewpoints as follows: (1) asthma and COPD are different expressions of obstructive lung disease; (2) airway hyperresponsiveness (AHR) is a conjunction risk factor for both asthma and COPD; and (3) different exposed environments (for instance, endogenous factors (e.g., sex and age), and exogenous factors (e.g., allergens, infections, and smoking)) and time play an important role in the development to different diseases [2]. Further research needs to be done to test the hypothesis.
ACOS or CAOS
Although both Global Initiative for Chronic Obstructive Lung Disease (GOLD) and Global Initiative for Asthma (GINA) published a joint project about the diagnosis and treatment of ACOS [7, 8•], but we found large amount of literatures also termed as COPD and asthma overlap syndrome (CAOS) [9–15]. Furthermore, the Spanish COPD guideline also defined “mixed COPD–asthma” as one of the phenotypes of COPD [16]. Then comes the question that which should be the first, COPD or asthma. Some people think it does not matter, while someone consider it should name according to the order of English letters. In our opinion, the two similar terms may have different meanings and emphases. CAOS should be the phenotype of COPD. These patients usually have smoking history, older, often first been diagnosed as COPD who have allergy and wheeze symptoms in later years [17], and positive bronchodilation test [18]. ACOS should be the subtype of asthma. Some asthmatic patients usually have no smoking history, been diagnosed asthma when they are young, and may have incompletely reversible airflow limitation in later years. Asthma patients who smoke might easily have fixed airflow limitation in later years [19]. In general, ACOS and CAOS have different clinical manifestations. Large sample clinical research needs to be done in the future to clarify the difference of treatment and prognosis of ACOS and CAOS.
Real-world clinical practice
Zeki et al. defined the ACOS as one of two clinical phenotypes: (1) allergic disease consistent with asthma, that is, variable air flow obstruction or AHR that is incompletely reversible (with or without emphysema or reduced carbon monoxide diffusion capacity (DLCO)) or (2) COPD with emphysema accompanied by reversible or partially reversible airflow obstruction (with or without an allergic syndrome or reduced DLCO) [20•]. It appears partial because a comprehensive clinical phenotype should be composed by evaluation of multiple clinical variables, molecular biomarkers, physiologic and radiologic data, and factors associated with disease progression and frequent exacerbations [21]. Obviously, in real clinical practice diagnosis of ACOS is remain difficult because of the overlapping of symptoms, the lack of a gold standard, and the existence of confounding factors, such as the degree of reversibility in airflow, older age, and smoking habits, contribute to misdiagnosis of these conditions [22]. Inevitably from the treatment point, there are lack of an individualized approach to the treatment and management of patients with ACOS especially in older people in real-world clinical practice [23].
The incidence of ACOS
The incidence of ACOS remains unclear due to no definite diagnostic criteria or using different inclusion and exclusion criteria, so there is a significant variability among the reported incidence of ACOS. The incidence of ACOS is about 10–55 % by prior study stratified by age and sex [24]. Data from the US National Health and Nutrition Examination (NHANES) III survey reported that the incidence of asthma plus chronic bronchitis is 55.8 %; asthma plus emphysema, 48.7 %; and asthma plus chronic bronchitis plus emphysema, 49.0 % [25]. Meanwhile, combinations of two of the three obstructive lung disease (OLD) conditions occurred among 21.2, 31.4, and 14.4 %, in those patients in the age groups of 60 to 69, 70 to 79, and ≥80 years, respectively [25]. Apparently, the incidence of ACOS increases with advancing age. Present reports showed doctor-diagnosed asthma/COPD was 15–20 % [7, 8•]. Cross-sectional, multicenter, noninterventional study published indeterminate patients account for 19.8 % [22] which coincides to recent generally consider the ACOS accounts for approximately 15–25 % of the obstructive airway diseases [8, 20•, 26].
The pathogenesis of ACOS
The pathogenesis of ACOS remains not clear. As we described in the review above, according to the Dutch hypothesis, ACOS may be a form of obstructive lung disease (OLD) [27], as several common environmental exposures have been unequivocally identified as shared risk factors for both asthma and COPD, for instance endogenous and exogenous factors like maternal smoking, air pollution, and cigarette smoking [28]. Cigarette smoking, atopy, and possibly age as risk factors cannot been ignored because cigarette smoking may modify the small airway inflammation and remodeling associated with bronchial asthma. Atopy is a genetic predisposition for the development of an IgE-mediated response to common aeroallergens [26]. But age is disputable for lung function declines with aging [26]. Bronchial hyperresponsiveness (BHR or airway hyperreactivity) as one of the hallmark features of asthma [29] may also play a role in ACOS. Prior study reported childhood asthma is a risk factor for COPD [30]; more precisely, a recent study that proposed children with severe asthma are at increased risk of developing COPD [31] might contribute to the development of ACOS. With new molecular tools, including re-sequencing and new genotyping arrays, and genomic resources such as the 1000 Genomes project giving an opportunity to detect low frequency genetic variants, huge breakthroughs have been made in the past years [32]. Joanna Smolonska and colleagues performed a GWAS on asthma and COPD did not elucidate a common genetic background of asthma and COPD [6], while Megan Hardin et al. performed and took advantage of meta-analysis pointed out genes CSMD1 (rs11779254, p51.57610-6), SOX5 (rs59569785, p51.61610-6), and GPR65 (rs6574978, p51.18610-7) associated with ACOS [11]. Understanding of pathogenesis of ACOS is beneficial to targeted therapy.
The clinical manifestations
The clinical manifestations of ACOS seem to be more perplexing than asthma or COPD alone. Data shows that ACOS is more common in female [33], older people (>55 years), and nearly all the patients of ACOS who have the history of cigarette smoking [34]. The rate of atopy was intermediate (64 %) between that of asthma and COPD alone, and pattern of airway inflammation is more similar to COPD. In the COPDGene Study which performed a cross-sectional observational study among smoking subjects demonstrated that compared to subjects with COPD alone, subjects with COPD and asthma were younger, had fewer pack-years of smoking, more reported a history of hay fever, and more frequent exacerbations in the previous year [35]. Also, researches found that ACOS patients have a more rapid disease progression, a worse health-related quality of life, more frequent respiratory exacerbations, and increased comorbidities than those with either COPD or asthma alone [33, 35]. The study of the Latin American Project for the Investigation of Obstructive Lung Disease (PLATINO) found that overlap group has the highest number of exacerbations, hospitalizations, and the worse general health status (GHS) [10]. The PLATINO study findings are in line with patients with ACOS who have worse lung function and more respiratory symptoms than with patients with just one or the other disease [36]. Kauppi et al. evaluated patient characteristics associated with health-related quality of life (HRQoL) and found that HRQoL of ACOS patients was poorer than asthma and COPD [37]. More frequent exacerbations and severe exacerbations, worse lung function, and poorer HRQoL suggested that ACOS has a poor prognosis.
Imaging of ACOS
In early stages of ACOS, the chest X-ray or computed tomography (CT) scan may be normal [8•]. Due to the low resolution rate, chest X-ray is not commonly used as radiology examination except for excluding some obvious abnormalities. Based on chest CT scanning, subjects with overlapping features of asthma and COPD demonstrated more gas trapping, and there was no difference in the degree of pulmonary emphysema or airway wall thickness between those subjects and subjects with COPD alone [35]. Controversially, recently published study showed that subjects with both COPD and asthma show greater airway wall thickness and less emphysema than subjects with COPD alone [11]. These reports have some discrepancies possibly due to the different inclusion criteria.
The diagnostic criteria of ACOS
Although GINA 2014 put forward the term “ACOS,” it did not provide definite diagnostic criteria. In clinical practice, differentiation of asthma and COPD is based on the patient’s history and pulmonary function test. However, it is complicated to establish the diagnosis of ACOS [38]. In 2012, a consensus was published about the existence of a different clinical phenotype known as “Overlap Phenotype COPD–Asthma,” whose diagnosis is made when two major criteria and two minor criteria are met. The major criteria include very positive bronchodilator test (increase in forced expiratory volume in the first second (FEV1) ≥15 % and ≥400 ml), eosinophilia in sputum and personal history of asthma. Minor criteria include high total IgE, personal history of atopy, and positive bronchodilator test (increase in FEV1 ≥12 % and ≥200 ml) on two or more occasions [18].
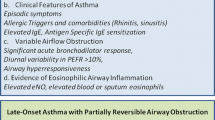
An in-depth and comprehensive elaboration of recent studies about diagnose criteria of ACOS is summarized as follow (Fig. 1): (1) clinical symptoms such as shortness of breath, wheezing, and coughing with or without sputum production [1]; (2) spirometry presents incompletely reversible airflow obstruction (postbronchodilator FEV1 <80 % predicted and FEV1/FVC <70 %); increased variability of airflow (determined by increased bronchodilator responsiveness or BHR) [34]; (3) radiologic variables demonstrate greater gas trapping on expiratory CT scan [35], less emphysema, and greater airway wall thickness compared to subjects with COPD alone [11]; and (4) airway inflammation in ACOS resembles COPD with increased airway neutrophils. Eosinophil numbers were lower compared with asthma alone [34]. However, there still a lack of a gold diagnostic criteria for ACOS.
Biomarkers of ACOS
Biomarker was defined by the National Institutes of Health as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention” [39]. Some researchers evaluated the usefulness of FeNO in predicting ACOS [40], which also been recommend in the diagnosis of GOLD and GINA [7, 8•]. Iwamoto et al. investigated four potential biomarkers of COPD: surfactant protein A (SP-A), soluble receptor for advanced glycation end products (sRAGE), myeloperoxidase (MPO), and neutrophil gelatinase-associated lipocalin (NGAL). They proposed increased induced sputum levels of NGAL might be a characteristic feature of ACOS [41•]. ACOS resembled COPD in terms of systemic inflammation, and IL-6 is a pivotal inflammatory mediator associated with ACOS in elderly people [42]. But the biomarkers of ACOS as “evidence-based” diagnosis and treatment for ACOS is really scarce [43].
Treatment of ACOS
There are guidelines or expert consensus documents about treatment strategy of ACOS. GINA pointed out while when diagnosed ACOS, COPD, and asthma are equivalent, whereas for the therapy, the default position should be to start accordingly for asthma: treatments will include an inhaled corticosteroid (ICS) (dose depends on symptoms); a long-acting beta2-agonist (LABA) should also be continued (if already prescribed), or added. If the syndromic assessment suggests COPD, appropriate symptomatic treatment with bronchodilators or combination therapy should be commenced, but not ICS alone. Other therapeutic strategies include smoking cessation, pulmonary rehabilitation, vaccinations, and treatment of comorbidities, as advised in the respective GINA and GOLD reports [8•]. Previously, also some researches divided the treatment of asthma, COPD, and ACOS into narrow-spectrum and broad-spectrum [26], which is easily confused and difficult to remember to those who are not specialist physician. Refer to complex patients emerging treatments consider using FeNO to endotype, bronchial thermoplast [26] can be taken into consideration. The Spanish COPD guidelines recommend treatment of the mixed COPD–asthma phenotype with ICS and a long-acting bronchodilator (LABD) as a first option, and with greater clinical severity, they recommend using the “triple therapy” that is a long-acting muscarinic receptor antagonists (LAMA) + ICS + LABA [16].
Future direction
This review is the updated summary about new clinical phenotype “ACOS” from pathogenesis, clinical manifestations, diagnostic criteria, therapy, etc. However, there still has a long way to go. Standardized definitions of ACOS, molecular mechanisms of ACOS like the gene and rare variant, accurate mortality, the response to therapy, and prognosis are still not fully reported. In clinical trials, such patients are often excluded from the study. For example, smokers are not included in asthma clinical study, while in COPD study, asthma are often excluded. Future research will be done to investigate the important clinical phenotype in real-world clinical practice.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Tzortzaki EG, Proklou A, Siafakas NM. Asthma in the elderly: can we distinguish it from COPD? J Allergy. 2011;2011:843543.
Dirkje S, Postma HMB. Rationale for the Dutch Hypothesis. Allergy and airway hyperresponsiveness as genetic factors and their interaction with environment in the development of asthma and COPD. Chest. 2004;126:96S–104.
Barnes PJ. Against the Dutch hypothesis: asthma and chronic obstructive pulmonary disease are distinct diseases. Am J Respir Crit Care Med. 2006;174(3):240–3. discussion 3–4.
Elias J. The relationship between asthma and COPD. Lessons from transgenic mice. Chest. 2004;126:111S–6.
Jeffery PK. Comparison of the structural and inflammatory features of COPD and asthma. Giles F. Filley Lecture. Chest. 2000;117(5 Suppl 1):251S–60.
Smolonska J et al. Common genes underlying asthma and COPD? Genome-wide analysis on the Dutch hypothesis. Eur Respir J. 2014;44(4):860–72.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for diagnosis, management and prevention of COPD. Available from www.goldcopd.org. 2014.
Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. Available from www.ginasthma.org. 2014. The report includes a new chapter which is on diagnosis of the asthma-COPD overlap syndrome (ACOS). The first time described about the diagnosis ACOS in detail. It gives us the basis when treat with the patients of ACOS.
Rhee CK et al. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. COPD. 2014;11(2):163–70.
Menezes AM et al. Increased risk of exacerbation and hospitalization in subjects with an overlap phenotype: COPD-asthma. Chest. 2014;145(2):297–304.
Hardin M et al. The clinical and genetic features of COPD-asthma overlap syndrome. Eur Respir J. 2014;44(2):341–50.
Miravitlles M et al. Characterisation of the overlap COPD-asthma phenotype. Focus on physical activity and health status. Respir Med. 2013;107(7):1053–60.
Wildman MJ et al. Survival and quality of life for patients with COPD or asthma admitted to intensive care in a UK multicentre cohort: the COPD and Asthma Outcome Study (CAOS). Thorax. 2009;64(2):128–32.
Wildman MJ et al. Predicting mortality for patients with exacerbations of COPD and Asthma in the COPD and Asthma Outcome Study (CAOS). QJM: Mon J Assoc Phys. 2009;102(6):389–99.
Wildman MJ et al. Implications of prognostic pessimism in patients with chronic obstructive pulmonary disease (COPD) or asthma admitted to intensive care in the UK within the COPD and asthma outcome study (CAOS): multicentre observational cohort study. BMJ. 2007;335(7630):1132.
Miravitlles M et al. Spanish COPD Guidelines (GesEPOC): pharmacological treatment of stable COPD. Aten Primaria/Soc Esp Med Fam Comunitaria. 2012;44(7):425–37.
Jamieson DB et al. Effects of allergic phenotype on respiratory symptoms and exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;188(2):187–92.
Soler-Cataluña JJ, Cosío B, et al. Consensus document on the overlap phenotype COPD–asthma in COPD. Arch Bronconeumol. 2012;48(9):331–7.
Perret JL et al. The independent and combined effects of lifetime smoke exposures and asthma as they relate to COPD. Exp Rev Respir Med. 2014;8(4):503–14.
Zeki AA et al. The asthma-COPD overlap syndrome: a common clinical problem in the elderly. J Allergy. 2011;2011:861926. In clinical, distinguishing asthma from COPD is difficult. The article compared asthma, COPD and asthma-COPD overlap syndrome with the similarities and differences comprehensively in clinical characteristics, and their physiologic and inflammatory profiles within the context of the aging patient. It also proposed guideline-recommended drug therapy about ACOS.
Carolan BJ, Sutherland ER. Clinical phenotypes of chronic obstructive pulmonary disease and asthma: recent advances. J Allergy Clin Immunol. 2013;131(3):627–34. quiz 35.
Miravitlles M et al. Difficulties in differential diagnosis of COPD and asthma in primary care. Br J Gen Prac: J R Coll Gen Pract. 2012;62(595):e68–75.
McDonald VM, Higgins I, Gibson PG. Insight into older people’s healthcare experiences with managing COPD, asthma, and asthma-COPD overlap. J Asthma: Off Assoc Care Asthma. 2013;50(5):497–504.
David M, Mannino. Obstructive lung disease and low lung function in adults in the United States. Data from the National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2000;160:1683–9.
Joan B, Soriano KJD, et al. The proportional Venn diagram of obstructive lung disease; two approximations from the United States and the United Kingdom. Chest. 2003;124:474–81.
Samuel Louie AAZ et al. The asthma–chronic obstructive pulmonary disease overlap syndrome: pharmacotherapeutic considerations. Expert Rev Clin Pharmacol. 2013;6(2):197–219.
Bleecker ER. Similarities and differences in asthma and COPD. Chest. 2004;126:93S–5.
Postma DS et al. Asthma and chronic obstructive pulmonary disease: common genes, common environments? Am J Respir Crit Care Med. 2011;183(12):1588–94.
de Marco R et al. Risk factors for chronic obstructive pulmonary disease in a European cohort of young adults. Am J Respir Crit Care Med. 2011;183(7):891–7.
Shirtcliffe P et al. Childhood asthma and GOLD-defined chronic obstructive pulmonary disease. Int Med J. 2012;42(1):83–8.
Tai A et al. The association between childhood asthma and adult chronic obstructive pulmonary disease. Thorax. 2014;69(9):805–10.
Wain LV, Artigas S. Tobin. What can genetics tell us about the cause of fixed airflow obstruction? Clin Exp Allergy: J Bri Soc Allergy Clin Immunol. 2012;42(8):1176–82.
de Marco R et al. The coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle-aged and elderly people from the general population. PLoS One. 2013;8(5):e62985.
Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009;64(8):728–35.
Hardin M et al. The clinical features of the overlap between COPD and asthma. Respir Res. 2011;12:127.
Mannino DM, Gognon R, et al. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2000;160:1683–9.
Kauppi P et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma: Off J Assoc Care Asthma. 2011;48(3):279–85.
Diaz-Guzman EM, Mannino E, David M. Airway obstructive diseases in older adults: from detection to treatment. J Allergy Clin Immunol. 2010;126(4):702–9.
Atkinson Jr AJ, Colburn WA, et al. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69(3):89–95.
Donohue JF et al. Characterization of airway inflammation in patients with COPD using fractional exhaled nitric oxide levels: a pilot study. Int J Chron Obstructive Pulm Dis. 2014;9:745–51.
Iwamoto H et al. Differences in plasma and sputum biomarkers between COPD and COPD-asthma overlap. Eur Respir J. 2014;43(2):421–9. There has been no study of plasma or sputum biomarkers in asthma-COPD overlap syndrome (ACOS) patients. The literature points out that sputum levels of neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker might be a characteristic feature of asthma-COPD overlap syndrome. NGAL could be taken into account when considered ACOS.
Fu JJ et al. Systemic inflammation in older adults with asthma-COPD overlap syndrome. Allergy Asthma Immunol Res. 2014;6(4):316–24.
Herland K et al. How representative are clinical study patients with asthma or COPD for a larger “real life” population of patients with obstructive lung disease? Respir Med. 2005;99(1):11–9.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Dr. Li and Dr. Chen both state that they received grant support from the Capital Health Development Research Fund (2011-1004-01)
Human and Animal Rights and Informed Consent
This article contains no studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on COPD
Rights and permissions
About this article
Cite this article
Li, M., Chen, Y. The updates of overlapping syndrome: asthma and COPD. Curr Pulmonol Rep 4, 105–110 (2015). https://doi.org/10.1007/s13665-015-0117-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-015-0117-5