Abstract
Treatment of pregnant women with cancer with radiation presents medical, technical, and ethical challenges. Cancer during pregnancy occurs in 1 out of 1000 cases. The most common cancers are those that are common in females of childbearing age, including breast cancer, cervical cancer, melanoma, Hodgkin lymphoma, and leukemia. The in utero radiation exposure of a developing fetus through diagnostic radiology/nuclear medicine and radiation therapy is always a concern for healthcare providers and parents. Radiation exposure to the fetus seems to be associated with increased incidences of childhood cancer at any fetal dose. However, there also seem to be threshold doses for non-cancer adverse outcomes such as intellectual disability, organ malformation, and fetal death. The fetal radiation exposure from diagnostic radiology and nuclear medicine studies is far smaller than these threshold levels. On the other hand, fetal doses from radiation therapy for treatment of maternal cancers depend largely on gestational age and distance of fetus from the treatment field. Treatment of cancers in head and neck or extremities is relatively safe, while that of pelvic organs, such as cervical cancer, is not compatible with pregnancy. It is important to note that the “threshold” doses were calculated based on observational data and therefore should be used with careful considerations in individual clinical scenarios. Ultimately, it is the frank discussion between the pregnant mother and her family with the entire medical team, including her oncologist, the obstetrician, the neonatologist, the psychologist, and the social worker, that will lead to the best individualized management plan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer complicates in 1 out of 1000 pregnancies [1, 2]. The most common cancers are those that are common in females of childbearing age, including breast cancer, cervical cancer, melanoma, Hodgkin lymphoma, and leukemia [2]. The in utero radiation exposure of a developing fetus through diagnostic radiology/nuclear medicine and radiation therapy is always a concern for healthcare providers. The potential adverse effects of radiation on the fetus include death, organ malformation, microcephaly, growth and intellectual disability, and childhood cancers. Such effects largely depend on the gestational age and the dose of radiation exposed. This review article intends to assist patients, families, and providers in evaluating fetal risk associated with ionizing radiation during diagnostic and therapeutic measures for pregnant patients.
Adverse effects of radiation on the fetus
The adverse effects of fetal radiation exposure depend largely on the gestational age (GA), as detailed in Table 1. Gestational age is defined as the number of weeks since the first day of last menstrual period (LMP), which is approximately 2 weeks earlier than the date of ovulation/conception. Implantation of the conceptus occurs between 2 and 3-week GA [9]. During this period, the effect of radiation on the fetus is an all-or-none phenomenon; that is, if the embryo survives the insult, it will likely suffer no other adverse effects except the increased risk for childhood cancers. Organogenesis coincides with a GA of approximately 5 to 10 weeks. An insult during this period results in organ malformations, among which microcephaly is the most common [1].
Interestingly, although the development of neural tissue begins around 4-week GA, no cases of severe intellectual disability (formerly mental retardation) were seen in the children exposed during 5–10-week GA period by atomic bomb explosions in Hiroshima and Nagasaki [1]. Severe intellectual disability is a main risk with radiation administered after 10-week GA. The risk per gray (Gy) from exposure between 10 and 17-week GA is four times higher than that for exposure between 18 and 27-week GA (Table 1). The former group also has a lower threshold dose for severe intellectual disability. The severity of intellectual disability increases with the amount of radiation exposure, with 25–31 points and 12–21 points of intelligence quotient reduction per 1 Gy above the thresholds for 10–17-week GA and 18–27-week GA, respectively, suggesting that the brain may be most sensitive to radiation damage in the early second trimester (Table 1).
Cancer induction may occur in a person who was exposed to radiation in utero. There is no threshold dose established for this risk, as evidenced by the increase in infant leukemia across Europe due to very low dose fetal exposure to radiation from the Chernobyl accident [10]. The risk does increase with the increased fetal dose (Table 2), and it has been suggested that the risk may be highest during the first trimester [11].
The spontaneous rates of these adverse outcomes in the population should also be considered. Estimated rate of miscarriage rate is 15 to 20 % in women who know they are pregnant [12]. Major birth defects occur at the rate of about 3 %, while intellectual disability is estimated at 1 % of the population [13, 14]. For childhood cancers, the background rate is at 0.3 % (Table 2).
Fetal radiation exposure from diagnostic studies
The fetal radiation exposure from diagnostic radiology studies can vary tenfold within each imaging modality depending on a number of factors including the fetal position from the field of view, the thickness of the patient, the direction of the projection, and the gestational age of the fetus [15]. Table 3 lists the common diagnostic studies and corresponding fetal doses. The data comes from three sources, and the highest reported dose is used for each modality [15–17].
Malignancies occurring during pregnancy
The most significant risk factor for development of maternal malignant neoplasms during pregnancy is patient’s age [18]. As childbearing is increasingly postponed in the developed world, the incidence of cancer during pregnancy also has increased [19]. Types of malignancies occurring during pregnancy include breast cancer, cervical cancer, Hodgkin lymphoma, malignant melanoma, and thyroid cancers. With regards to radiation therapy, peripheral doses that are measured in phantoms are accurate for clinical use and can be used to estimate the fetal dose [20].
Radiation therapy for specific cancers during pregnancy
Fetal radiation doses from radiation therapy provoke the highest concerns for both the patient and the healthcare providers. Generally, cancers that are distant from the fetus, especially in the extremities and head and neck area, can be safely treated with careful planning. On the other hand, cancers in the pelvis cannot be adequately treated with radiation without severe consequences to the fetus, and therefore, pregnancy termination has to be considered [21]. Other cancers, such as breast cancer and those in the thorax and mediastinum, carry intermediate risk to the fetus.
Fetal doses depend on a number of factors, the most important being the distance of the fetus from the edge of the radiation field, with the doses increasing significantly as the distance decreases. The leakage of photons from the head of the linear accelerator, scatter from the collimators and modifiers, scatter within the patient, and additional dose from neutron emission (contamination) in higher energy photon beams (>10 MV) all also contribute to the fetal dose.
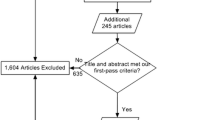
A literature search for the case reports of different cancers discussed in this article was performed by using PubMed (up to week 1, October, 2015) with a filter for human only and with words “fetal dose,” “cancer,” and “radiotherapy”. “Breast,” “Hodgkin’s,” “Cervical,” and “Head and Neck” were added for each cancer. The cases that are missing the type of cancer were excluded.
Head and neck cancers
The large distance from the head and neck to the fetus makes the treatment for these cancers most likely to result in the lowest fetal dose compared with those in the torso. Ten representative cases from the literature are reported in Table 4. Fetal doses range from 19.9 to 110 mGy. The case with the highest fetal dose is reported by Magné et al. in the patient who had a metastatic lesion in the right occipital lobe, with a primary lung lesion that was treated 15 months earlier with lobectomy and radiotherapy [22]. The patient was at 24-week GA at the beginning of the treatment for the metastatic lesion. Two lateral beams were used to radiate the whole brain to 30 Gy, and 2-cm-thick lead screens were used as shields on both sides of the patient. The patient’s neck was hyperextended on the edge of the concrete block containing 2.3 % FeO2. The patient delivered a healthy boy who was free of adverse outcomes at age 3. The only case to report an adverse outcome in brain cancer is by Luis et al. who described a 20-week GA patient with a left frontal astrocytoma [30]. Three linear beams were used to radiate the patient to 54 Gy, and her abdomen was covered in a 75-mm-thick lead shield. The radiotherapy proceeded without complication, but at routine 38-week fetal ultrasound, no heart sounds were detected. The fetal autopsy demonstrated inferior vena cava thrombus that likely occurred around full term given the fetus’s size. In three of the other cases reported in Table 4, there was no information about the fetal outcome, but the fetal doses were 19.9, <35, and 49 mGy, all well below the threshold doses for non-cancer adverse outcomes. All other cases reported no adverse outcomes. Jie-Hua et al. reported four cases of nasopharyngeal carcinoma with no adverse outcomes (fetal doses are missing, and therefore, cases were not reported in Table 4) [38]. These cases illustrate that the radiation therapy can be used fairly safely in the cancers of the head and neck. On the other hand, watchful waiting has also been utilized in slow-growing tumors. Haba et al. reported a case in which a 20-week GA patient with glioma was managed conservatively until delivery after serial MRIs showed no progression during pregnancy [39].
Breast cancer
After malignant melanoma and Hodgkin lymphoma, breast cancer is the most common cancer during pregnancy with an incidence of 1 in 3000–10,000 [2]. Breast cancer during pregnancy is generally defined as one that arises during concurrent pregnancy or within 1 year after delivery. The incidence of breast cancer during concurrent pregnancy, however, was 34 out of 100,000 maternities in a population-based study in Australia [40]. Table 5 lists the maximum fetal doses by gestational age, demonstrating a significant increase in fetal dose as the fetus grows—from only 3 cGy at 10-week GA to 143 cGy at 38-week GA. However, one should note that as the gestational age increases, the fetus is more likely to be in cephalic position, reducing the risk of radiation to the fetal brain.
There have been cases of successful radiation therapy used to treat breast cancer patients with concurrent pregnancies resulting in no adverse outcomes to the fetus [31–33]. All cases occurred in different trimesters during the treatment and showed no abnormalities to the infants. For the tumor doses of 46–50 Gy using 6 and 10 MV photon beams, fetal doses varied from 39 to 180 mGy. In the case with 2-week GA, no shield was used and the fetal dose was less than 100 mGy, the threshold dose for fetal death [31]. Nine millimeter and 4-cm lead shields were used in the other two cases that were over 15-week GA. The fetal doses were also less than the threshold dose for intellectual disability. As with cancers of the head and neck, breast cancers can also be treated with radiation with good fetal outcomes.
Hodgkin’s lymphoma
At the incidence of 1 in 1000–6000 pregnancies, Hodgkin’s lymphoma is the second most common malignant tumor among pregnant women after malignant melanoma [2]. It has a bimodal age distribution with the first peak in 20s–30s and the second in 50s, explaining the high incidence during the childbearing years. It typically presents in the neck or the mediastinum as painless lymphadenopathy or as an asymptomatic enlarged lymph node on chest X-ray [41]. Depending on the location of the nodes involved, fetal doses can vary. One previous review noted a total of three adverse outcomes in 58 cases of Hodgkin’s lymphoma of varying stages, including one perinatal death [30]. Klieger-Grossmann et al. reported an adverse outcome in a case of stage IIA Hodgkin lymphoma in the mediastinum [34]. The patient was found to be pregnant after chemotherapy and radiation therapy. GA was calculated to be 7 weeks and 4 days at the beginning of the radiation treatment. She received 42.5 Gy in 20 fractions, and fetal dose was calculated later to be between 50 and 180 mGy. A healthy baby boy was born at 39-week GA at 10th, 50th, and 20th percentiles for weight, length, and head circumference, respectively. At the age of 2, the boy was healthy and had met developmental milestones. However, his weight and length were at the fifth percentile and his head circumference at the third percentile. His gestational age during the radiotherapy overlapped with the period of organogenesis, potentially explaining his delayed growth, especially the small head size.
On the other hand, Moreau et al. reported a case with a good outcome despite a very high fetal dose [37]. The patient had Hodgkin lymphoma with extensive involvement of both supradiaphragmatic and subdiaphragmatic nodes. She received 40 Gy to the mediastinum and 36 Gy to the neck along with chemotherapy. Radiotherapy for subdiaphragmatic nodes was delayed for 4 weeks during which she became pregnant. Thirty-six gray to the paraaortic nodes was delivered. She was found to be pregnant only after the end of the second course of radiotherapy. Gestational age was calculated to be about 4 weeks at the beginning of the treatment and 8 weeks at the end. The fetal dose was estimated to be between 2.8 and 5 Gy. The option of termination of pregnancy was discussed, but the patient declined. A baby boy was delivered at 41-week GA. At the age of 3, he was healthy and had normal psychomotor development for his age without any hematologic disorders. These two cases demonstrate the unpredictability in adverse outcomes to the fetus from in utero radiation exposure.
Four other cases of Hodgkin lymphoma described in the Table 4 were known pregnancies at the time of treatment. The lesions in all cases were above the diaphragm, and patients also received shielding. The first case was at 23-week GA [36]. The fetus received less than 100 mGy with an outcome of a healthy infant. The second case was at 27-week GA [23]. Before the fetus was delivered through planned C-section, it received less than 420 mGy. The therapy continued after delivery. The child was healthy with no adverse effects at 8 years of age. In the other two cases, the fetuses received 46–50 mGy, and both children were healthy at 9 and 11 years of age, respectively [30]. While most of the cases of Hodgkin lymphoma described above failed to show adverse outcomes, fetal doses have proven to be significantly higher than doses to more distant lesions, particularly in the head and neck region. In addition, involvement of nodes below the diaphragm will likely push fetal doses above threshold.
Cervical cancer
Cervical cancer has an incidence of 1.2 in 10,000 pregnancies [2]. Unfortunately, radiation therapy for cervical cancer cannot be safely administered during pregnancy. Budzinski et al. reported five cases of stage IIb invasive carcinoma of the cervix during pregnancy in which spontaneous abortions/premature labor occurred after 30.6–32 Gy of irradiation was delivered through external beam and brachytherapy [42]. If pregnancy is desired, the risk to the mother from delaying the treatment should be carefully balanced with the risk to the fetus from early delivery to find the optimal gestational age for delivery. For early delivery, the fetus is generally not viable in the first trimester, but viability improves after 23 weeks of gestation. Cautious delay in treatment may be an option if pregnancy is still early and the disease is also in early stage [43]. However, a disastrous outcome to the mother after such a delay has also been reported [44]. The following topic discusses the survival of preterm deliveries. If the treatment is postponed until after delivery, vaginal birth is contraindicated due to the risk of recurrence in episiotomy scars [45].
Considerations in pregnancy management for pregnant women with cancer requiring radiotherapy
When the risk of radiation to fetus is considered, one alternate solution is to consider early delivery. The decision for the delivery should be guided by the risk of mortality and morbidity to the newborn due to prematurity. The data adapted from the study by Stoll et al. (Table 6) shows the survival rate of preterm delivery [46]. This data came from 20 US academic centers across the nation from 2003 to 2007 and studied children born between 22 and 28 weeks of gestation. This study highlights the fact that although greater than 75 % of infants with gestation age over 26 weeks survive, many of those who survive will have morbidities due to prematurity, including respiratory distress syndrome, bronchopulmonary dysplasia, intraventricular hemorrhage, periventricular leukomalacia, early onset and late-onset sepsis, necrotizing enterocolitis, infections, patent ductus arteriosus, and retinopathy of prematurity. These morbidities can have long-term complications and may translate into mortality after discharge. The postneonatal (defined as 29 days to 1 year after delivery) mortality rate for premature infants born before 38.0 weeks of gestation who survived the neonatal period is illustrated in Table 7.
The limitation in using Tables 6 and 7 is that the preterm deliveries in these studies are not specific for those due to medical indication from maternal cancer treatments. In fact, many are due to fetal indications (e.g., distress or abnormality) that may have different mortality risk when compared with maternal indications. Therefore, they should be used with caution when the physician discusses the data with the patient. They are intended to supplement the discussion between the patient and the providers about options for the patient. The patient will ultimately need an expert opinion from a neonatologist and an obstetrician regarding the mortality and morbidity risk due to premature delivery.
Conclusions
Radiation exposure to the fetus is associated with increased incidences of childhood cancer at any fetal dose. However, there seem to be threshold doses for non-cancer adverse outcomes such as intellectual disability, organ malformation, and fetal death. The fetal radiation exposure from diagnostic radiology and nuclear medicine studies is far smaller than the threshold levels. On the other hand, fetal doses from radiation therapy for treatment of maternal cancers depend largely on gestational age and distance of fetus from the treatment field. Treatment of cancers in head and neck or extremities is relatively safe, while that of pelvic organs, such as cervical cancer, is not compatible with pregnancy. Shielding should be used to reduce fetal dose. It is important to note that all data in this paper, collected from several sources, come from observational studies. The “threshold” doses were calculated by studies that are based on the limited number of observational cases and therefore should be used with careful considerations to individual clinical scenarios.
References
Stovall M, Blackwell CR, Cundiff J, et al. (1995) Fetal dose from radiotherapy with photon beams: report of AAPM radiation therapy committee task group no. 36. Med Phys 22(1):63–82
Pavlidis NA (2002) Coexistence of pregnancy and malignancy. Oncologist 7:279–287
Center for Disease Control and Prevention. Radiation and Pregnancy: A Fact Sheet for Clinicians. Retrieved from: https://emergency.cdc.gov/radiation/prenatalphysician.asp.
De Santis M, Cesari E, Nobili E, et al. (2007) Radiation effects on development. Birth Defects Research part C Embryo Today 81(3):177–182
Otake M, Schull WJ, Lee S (1996) Threshold for radiation-related severe mental retardation in prenatally exposed A-bomb survivors: a re-analysis. Int J Radiat Biol 70(6):755–763
Schull WJ (1995) Effects of atomic radiation, a half-century of studies from Hiroshima and Nagasaki. Wiley-Liss & Sons, Inc., New York
Bithell JF, Stewart AM (1975) Prenatal irradiation and childhood malignancy: a review of British data from the Oxford survey. Br J Cancer 31:271–287
Mole RH (1990) Childhood cancer after prenatal exposure to diagnostic X-ray examinations in Britain. Br J Cancer 62(1):152–168
Adams WE (1960) Early human development. The New Zealand Medical Journal 59:7–17
Busby CC (2009) Very low dose fetal exposure to Chernobyl contamination resulted in increases in infant leukemia in Europe and raises questions about current radiation risk models. Int J Environ Res Public Health 6(12):3105–3114
Bithell JF, Stewart AM (1971) Pre-natal irradiation and childhood malignancy: a review of British data from the Oxford survey. Br J Cancer 31(3):271–287
American College of Obstetricians and Gynecologists (2002) ACOG practice bulletin. Management of recurrent pregnancy loss. Number 24, february 2001. (replaces technical bulletin number 212, september 1995). International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics 78(2):179–190
Center for Disease Control and Prevention. Update on Overall Prevalence of Major Birth Defects – Atlanta,Georgia, 1978–2005. Retrieved from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5701a2.htm.
Szymanski L, King BH (1999) Practice parameters for the assessment and treatment of children, adolescents, and adults with intellectual disability and comorbid mental disorders. American Academy of Child and Adolescent Psychiatry working group on quality issues. J Am Acad Child Adolesc Psychiatry 38(12 Suppl):5S–31S
McCollough C, Schueler B, Atwell T, et al. (2007) Radiation exposure and pregnancy: when should we be concerned? Radiographics 27:909–917
Williams PM, Fletcher S (2010) Health effects of prenatal radiation exposure. Am Fam Physician 82(5):488–493
Osei EK, Darko J (2013) Foetal radiation dose and risk from diagnostic radiology procedures: a multinational study. ISRN Radiology 318425.
Smith LH, Dalrymple JL, Leiserowitz GS, et al. (2001) Obstetrical deliveries associated with maternal malignancy in California, 1992 through 1997. Am J Obstet Gynecol 184(7):1504–1512
Andersson TM, Johansson AL, Hsieh CC, et al. (2009) Increasing incidence of pregnancy-associated breast cancer in Sweden. Obstet Gynecol 114(3):568–572
Van der Giessen P, Bierhuizen W (1997) Comparison of measured and calculated peripheral doses in patients undergoing radiation therapy. Radiother Oncol 42:257–264
International Commission on Radiological Protection (2000) Pregnancy and medical radiation. (1-43). Ann ICRP 30:iii–viii ICRP Publication 84
Magné N, Marcié S, Pignol JP, et al. (2001) Radiotherapy for a solitary brain metastasis during pregnancy: a method for reducing fetal dose. Br J Radiol 74:638–641
Nuyttens JJ, Prado KL, Jenrette JM, et al. (2002) Fetal dose during radiotherapy: clinical implementation and review of the literature. Cancer Radiothérapie 6:352–357
Sneed PK, Albright NW, Wara WM, et al. (1995) Fetal dose estimates for radiotherapy of brain tumors during pregnancy. Int J Radiat Oncol Biol Phys 32(3):823–830
Sharma DS, Jalali R, Tambe CM, et al. (2004) Effect of tertiary multileaf collimator (MLC) on foetal dose during three-dimensional conformal radiation therapy (3DCRT) of a brain tumour during pregnancy. Radiother Oncol 70:49–54
Islam MK, Saeedi F, Al-Rajhi N (2001) A simplified shielding approach for limiting fetal dose during radiation therapy of pregnant patients. Int J Radiat Oncol Biol Phys 49:1469–1473
Josipovic M, Nystrom H, Kjaer-Kristoffersen F (2009) IMRT in a pregnant patient: how to reduce the fetal dose? Med Dosim 34:301–310
Orlandi E, Zonca G, Pignoli E, et al. (2007) Postoperative radiotherapy for synovial sarcoma of the head and neck during pregnancy: clinical and technical management and fetal dose estimates. Tumori 93(1):45–52
Moeckli R, Ozsahin M, Pache G, et al. (2004) Foetal dose reduction in head and neck radiotherapy of a pregnant woman. Z Med Phys 14(3):168–172
Luis SA, Christie DRH, Kaminski A, et al. (2009) Pregnancy and radiotherapy: management options for minimizing risk, case series and comprehensive literature review. J Medical Imaging and Radiation Oncology 53:559–568
Antypas C, Sandilos P, Kouvaris J, et al. (1998) Fetal dose evaluation during breast cancer radiotherapy. Int J Radiat Oncol Biol Phys 40(4):995–999
Ngu SL, Duval P, Collins C (1992) Foetal radiation dose in radiotherapy for breast cancer. Australasia Radiology 36:321–322
Van der Giessen PH (1997) Measurement of the peripheral dose for the tangential breast treatment technique with Co-60 gamma radiation and high-energy X-rays. Radiother Oncol 42:257–264
Klieger-Grossmann C, Djokanovic N, Chitayat D, et al. (2009) In utero exposure to therapeutic radiation for Hodgkin lymphoma. Can Fam Physician 55(10):988–991
De Wildt SN, Taquachi N, Koren G (2009) Unintended pregnancy during radiotherapy for cancer. Nat Clin Pract Oncol 6(3):175–178
Cygler J, Ding GX, Kendal W, et al. (1997) Fetal dose for a patient undergoing mantle field irradiation for Hodgkin's disease. Med Dosim 22:135–137
Moreau MV, Brunaud C, Bologna S, et al. (2007) High fetal irradiation: about one pregnant woman receiving infradiaphragmatic radiotherapy for Hodgkin lymphoma. Cancer Radiothérapie. 11(8):495–499
Jie-Hau Y, Caisen L, Yuhua H (1984) Pregnancy and nasopharyngeal carcinoma: a prognostic evaluation of 27 patients. Int J Radiat Oncol Biol Phys 10:851–855
Haba Y, Twyman N, Thomas SJ, et al. (2004) Radiotherapy for glioma during pregnancy: fetal dose estimates, risk assessment and clinical management. Clin Oncol 16:210–214
Lee YY, Roberts CL, Dobbins T, et al. (2012) Incidence and outcomes of pregnancy-associated cancer in Australia, 1994–2008: a population-based linkage study. BJOG 119(13):1572–1582
Mauch PM, Kalish LA, Kadin M, et al. (1993) Patterns of presentation of Hodgkin disease: implications for etiology and pathogenesis. Cancer 71:2062–2071
Bidzinski M, Zielinski J, Panek G (2002) Stage IIb invasive carcinoma of the cervix during pregnancy—personal experience and contemporary opinions on this topic. Ginekol Pol 73:30–34
Nguyen C, Montz F, Bristow R (2000) Management of stage I cervical cancer in pregnancy. Obstetrics and Gynecological Survey 55:633–643
Rabaiotti E, Sigismondi C, Montoli S, et al. (2010) Management of locally advanced cervical cancer in pregnancy: a case report. Tumori 96(4):623–626
Hafeez I, Lawenda BD, Schilder JM, et al. (2011) Prolonged survival after episiotomy recurrence of cervical cancer complicating pregnancy. Eur J Gynaecol Oncol 32(2):211–213
Stoll BJ, Hansen NI, Bell EF, et al. (2010) Neonatal outcomes of extremely preterm infants from the NICHD neonatal research network. Pediatrics 126:443–456
Kamath-Rayne BD, Defranco EA, Chung E, et al. (2012) Subtypes of preterm birth and the risk of postneonatal death. J Pediatr 162(1):28–34
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Funding
None.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Maung, K.K., Lucas, A., Schaner, P. et al. Considerations in radiation therapy for pregnant women with malignancy. J Radiat Oncol 5, 335–344 (2016). https://doi.org/10.1007/s13566-016-0276-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-016-0276-1