Abstract
Objective
Precise tumor alignment is vital in lung stereotactic body radiotherapy (SBRT). Differences in center of mass (COM) resulting from mixing and matching target delineation methods, and planning image datasets could introduce systematic errors.
Methods
Thirty consecutive lung SBRT patients were simulated with free-breathing CT (FBCT), maximum inhalation and exhalation breath hold CT (BHCT), and 4D-CT. Four planning target volumes (PTV) were created: 5/10-mm expansion from the gross tumor volume (GTV) in FBCT (PTVFBCT), 5-mm expansion from the internal target volume (ITV) in BHCT (PTVBHCT), 5-mm expansion from the ITV in the maximum intensity projection (PTVMIP), and 5-mm expansion from the ITV in 4D-CT (PTV4D-CT). Using average intensity projection CT (AIP-CT) or FBCT as the reference images, PTVs were transferred after bony registration to compare COMs.
Results
When AIP-CT was used as reference, the mean COM vector shifts of the PTVFBCT, PTVBHCT, and PTV4D-CT were 2.94 mm (p = 0.0094), 4.35 mm (p = 0.0001), and 1.45 mm (p = 0.57), respectively, relative to the COM of the GTV on AIP-CT. When FBCT was used as reference, the mean COM vector shifts of the PTVBHCT, PTVMIP, and PTV4D-CT were 3.6 mm (p = 0.0006), 2.78 mm (p = 0.003), and 2.94 mm (p = 0.002) relative to the GTV on FBCT, respectively.
Conclusions
Depending on the reference images used, the COMs of the PTVFBCT, PTVBHCT, and PTV4D-CT are inconsistent, exhibiting significant shifts relative to each other. To avoid possible systematic localization errors, we recommend using 4D-CT/MIP for target delineation and AIP-CT for planning and alignment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Methods used in target delineation, planning, and delivery of lung SBRT have evolved rapidly and vary among institutions. As these methods differ in the way they incorporate tumor motion, there is potential for inconsistency and systematic error that could affect treatment planning and image-guided treatment delivery.
With the exception of respiratory gating and tumor tracking, there are three major methods of target delineation in lung SBRT. The initial method applied empirical margins to the gross tumor volume on a free-breathing CT (FBCT) without considering the patient-specific tumor motion. This method was adopted in an early protocol of Radiation Therapy Oncology Group (RTOG) 0236, using fixed empiric margins of 0.5 cm radially and 1 cm in the cranio-caudal dimensions [1]. Some institutions continue to use this method today [2]. Other centers have evolved to use 4D-CT to define an individualized ITV to account for patient-specific tumor motion. However, centers lacking 4D-CT technology may resort to a third method which combines the GTV volumes from three co-registered CT scans: FBCT plus a maximum inhalation CT and a maximum exhalation CT. The combination of the three scans is used to define the full range of tumor motion to create an ITV. We refer to this method as breath-hold CT (BHCT) in the remainder of the paper [3, 4].
Each of the above methods generates a PTV with a distinct volume that associates with a center of mass (COM). The COMs of these PTVs could be either consistent or inconsistent with the COM of the tumor visible upon the planning CT. Typically, either FBCT or average intensity projection (AIP) from 4D-CT is chosen as the planning CT. Previous studies have shown potential dosimetric effects of these differences, but the COM shifts themselves have not been quantified to determine the potential impact on both treatment planning and image guidance [5]. Bradley et al. performed a spatial analysis of COM which did not reveal significant differences between COM of tumor on 4D-CT and the composite images: MIP and AIP [6]. Further studies have determined that cone beam CT (CBCT) image guidance can be precisely aligned with 4D CT generated ITV volumes [7]. Thus, for 4D-CT-based volumes, it is recommended to use AIP for both treatment planning and cone beam image guidance. For centers not equipped with 4D-CT, a quantitative analysis of COM shifts applicable to treatment planning and imaging guidance is valuable.
Here, we present a quantitative analysis of the magnitude of COM differences for four different ITV delineation methods: Two are 4D-CT-based (PTV4D-CT and PTVMIP), the third uses empirical margin (PTVFBCT), and the fourth is the BHCT (PTVBHCT). By comparing COM shifts between these PTVs and tumor on planning CT images (FBCT and AIP-CT), our goal is to describe the likelihood with which such mixing and matching could result in isocenter misalignment and introduce systematic error.
Methods and materials
Patient selection
An Internal Review Board (IRB)-approved registry of lung cancer SBRT cases was reviewed. Routine 4D-CT imaging at the time of simulation began in early 2009, and a representative sample of 30 consecutive medically inoperable lung SBRT patients with 32 lung lesions was selected. The median age was 68, median Karnofsky Performance Status (KPS) was 80, and median lesion size was 2 cm (range 0.8 to 6.5 cm). All patients had abdominal compression to restrict tumor motion.
Simulation procedure
Patients were simulated in the supine position in a vacuum bag immobilization system (BodyfixR, Elekta, Inc., Stockholm, Sweden). Abdominal compression was adjusted under fluoroscopy to restrict tumor motion to less than 1 cm. Multiple CT acquisitions, FBCT, BHCTs with the maximum exhalation and maximum inhalation, and 4D-CT, were preformed sequentially, while patient remained in the same position, using a Phillips Brilliance Big Bore CT scanner with 16 CT detector rows (Phillips Medical Systems, Cleveland, Ohio) and 3-mm slice thickness. For each patient, 4D-CT was reconstructed into 10 phases with a mean acquisition time of 100 s.
Target volume derivation
For each patient, tumors were delineated on CT with lung windowing by the same physician for consistency. Four planning target volumes (PTV) were created as follows: 5/10-mm expansion from the gross tumor volume (GTV) in FBCT consistent with RTOG 0236 protocol [1] (PTVFBCT), 5-mm expansion from the internal target volume (ITV) in BHCT (PTVBHCT), 5-mm expansion from the ITV in the maximum intensity projection (PTVMIP), and 5-mm expansion from the ITV in 4D-CT (PTV4D-CT). Pictorial representations of the four PTVs are illustrated in Fig. 1.
Shown are pictographs depicting the target volumes employed in this study. Filled circles represent gross tumor volumes that represent the GTV contoured on FBCT. Stippled ovals represent 4D-CT-derived patient-specific ITV (4D-CT and MIP). The vertical and horizontal hashed circles represent the inhale and exhale GTVs, respectively. Dashed lines surrounding GTVs or ITVs represent the PTV that results from applying superior-inferior and radial margins listed at the below each representation
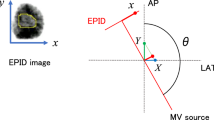
Center of mass (COM) shift determination
The COMs of the PTVs were obtained using MIMvista software (MIMvista, Cleveland OH). In order to have all COMs in the same coordinate system, all CT images were rigidly registered aligning to the spinal column and posterior rib bony anatomy. For PTVBHCT, FBCT was used as the base image set for coregistration. COMs of the GTV on the FBCT and AIP-CT were defined as two reference points to quantify the relative shifts of COMs of all PTVs.
Data management and statistical analysis
Statistical analysis was performed using JMP v.10 (SAS, Cary, NC) software. The PTV volumes relative to PTV4DCT were compared using t tests with Bonferroni corrections to adjust for multiple comparisons. Confidence levels were set to 0.05 for overall test and adjusted with Bonferroni corrections to preserve that level of significance for multiple comparisons. COM shifts were compared with ANOVA as a preliminary test to identify an overall difference between groups, and serial t tests with Bonferroni correction to preserve an overall alpha level of 0.05 were employed for individual comparisons.
Results
Volumetric differences were observed between different PTV creation methods as shown in Table 1. The PTVFBCT and PTVBHCT were on average significantly larger by 11 and 17 %, respectively (p = 0.0011 and 0.0167 – Bonferroni level p = 0.0167 for overall α = 0.05). The PTVMIP volume was not significantly different from the PTV4D-CT.
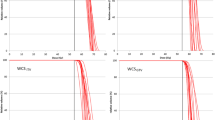
AIP-CT as a planning reference CT
When the COM of the GTV on the AIP-CT was compared to the COMs of PTV4D-CT, PTVFBCT, and PTVBHCT, significant shifts in the COM from PTVFBCT and PTVBHCT were observed (Fig. 2a). The mean magnitude shifts for PTVFBCT and PTVBHCT were 2.94 and 4.35 mm, respectively. In comparison, the mean COM shift of PTV4D-CT was 1.45 mm. Since previous studies have identified COM shifts from 4D-CT modalities to be negligible, a value of 1.5 mm was set for comparison in the t test based on the stability of COM [6]. The mean COM magnitude shifts were significantly greater than the 1.5 mm threshold for PTVFBCT and PTVBHCT (p = 0.0094 and 0.0001 respectively with Bonferroni correction p = 0.025 for an overall α = 0.05). For two patients, the COM shifts of the PTVFBCT exceeded the planning margin of 5 mm as initially defined by RTOG 0236. For five (16.7 %) patients, the COM shifts of the PTVBHCT exceeded the planning margins of 5 mm.
a The mean COM shifts in medio-lateral, anterior-posterior, superior-inferior directions, and the mean magnitude relative to COM of the tumor on AIP-CT. b The ITV on AIP-CT (green) and the PTVBHCT (blue) transferred based on bony registration are shown in sagittal and coronal views of AIP-CT. c The PTVBHCT (red) transferred based on alignment to tumor on AIP-CT are shown in sagittal and coronal views. The GTV (dark blue) from the breath hold maximum inhaled CT is shown on AIP-CT after bony alignment and is not encompassed by the displaced PTVBHCT
Figure 2b, c illustrates the implications of COM shifts on target volume positions on the AIP-CT for a selected patient with a significant shift. In Fig. 2b, the GTVAIP (green) was directly delineated on the AIP-CT. The PTVBHCT (cyan) was transferred to the AIP-CT image after bony registration between the FBCT and AIP-CT as PTVBHCT is typically drawn on the FBCT. As shown in Fig. 2b, the GTVAIP was inside the superior portion of the cyan PTVBHCT. If the registration between the FBCT and AIP-CT was changed to align to the GTVs instead of bony alignment, Fig. 2c shows the transferred PTVBHCT (red). Because of different alignment focal regions (bone vs. tumor), the COMs between the cyan PTVBHCT in Fig. 2b and the red PTVBHCT in Fig. 2c were shifted by 18 mm. This shift could translate to geometric miss of the GTV at the extreme position of the breathing cycle. To illustrate this, we transferred the GTV position (blue) onto Fig. 2c from the inhale CT scan after bony registration between the FBCT and AIP-CT.
These COM shifts of PTVFBCT and PTVBHCT relative to GTV on AIP-CT have clinical implications on image guidance. Due the slow acquisition of CBCT, the COM of the GTV on the CBCT can be considered concordant to the COM of the GTV on the AIP-CT. In contrast, when multiple breath hold CTs are acquired to define the PTVBHCT, the treatment plan is typically designed on the FBCT. However, COM of such a volume may be displaced relative to AIP CT. As a result, if the FBCT image was used as the reference CT for image-guided radiotherapy (IGRT) delivery and the two images were aligned to the tumor, the observed COM shift could be introduced during this alignment.
Free-breathing CT as a reference CT
To confirm that the above results were not due to selecting the AIP-CT as the reference CT, we chose the FBCT as the reference CT. After registering to the bony anatomy among different CTs, in relative to the COM of the GTV in the FBCT, the average magnitude shifts of the COMs of PTVBHCT, PTVMIP, and PTV4D-CT were 3.6, 2.78, and 2.94 mm respectively. The details of these shifts are shown in Fig. 3. The COM magnitude shifts for the PTVBHCT, PTVMIP, and PTV4D-CT relative to the COM of the PTVFBCT were significantly greater than 1.5 mm (p = 0.002, 0.003, and 0.0006, respectively, Bonferroni correction p = 0.0167 for overall α = 0.05). No directional trends in these shifts were observed.
a Mean COM shifts in medio-lateral, anterior-posterior, and superior-inferior directions and the mean magnitude from aligning to COM of the GTV in FBCT are shown. b For a selected patient: sagittal and coronal views of FBCT tumor (green) and PTV4D-CT aligned to the bony anatomy (blue). c The PTV4D-CT aligned to the tumor on FBCT (yellow) is shown on sagittal and coronal views of FBCT. The ITV4D-CT (red) is shown on FBCT after bony alignment and is not encompassed by the displaced PTV4D-CT
Figure 3b, c illustrates the potential implications of COM shifts for a selected patient. In Fig. 3b, the GTV (green) was directly delineated from the FBCT. After registering to the bony anatomy between the FBCT and AIP-CT, the PTV4D-CT was transferred to the FBCT as displayed blue in Fig. 3b in sagittal and coronal and views. The transferred PTV4D-CT (blue in Fig. 3b) encompassed the GTV (green in Fig. 3b) from the FBCT. If the registration focal region changed to the tumor (i.e., GTV) between the FBCT and AIP-CT, the transferred PTV4D-CT was in yellow in Fig. 3c. Because of different alignment focal regions (bone vs. tumor), the COMs between the blue PTV4D-CT in Fig. 3b and the yellow PTV4D-CT in Fig. 3c were shifted by 10 mm. This shift could translate to geometric miss of the ITV that was defined based on 4D-CT. To illustrate this, we transferred the ITV4D-CT (red in Fig. 3c) from the 4D-CT after bony registration between the FBCT and AIP-CT. As shown in Fig. 3c, the shifted yellow PTV4D-CT did not encompass the entire the ITV4D-CT (red).
Discussion
Studies have demonstrated that target volume delineation using 4D CT image datasets with planning on average intensity projection CT and cone beam CT image guidance results in minimal systematic error [5–7]. However, not all radiotherapy centers have access to this technology and may choose to employ alternative methods of target delineation including breath hold CT and empirical margins on a free-breathing CT. Without consideration of the limitations of the various methods of tumor motion delineation, the differences in COM between the PTV and the tumor apparent on FBCT and AIP CT could introduce systematic errors. Our study quantifies the COM shifts present in a series of consecutive lung SBRT patients. These errors can be introduced at two timepoints: during volume transfer between the different CT image sets and during IGRT alignment for treatment delivery.
At the time of treatment planning, the use of FBCT is problematic. Our study demonstrates significant shift magnitudes for PTVBHCT, PTVMIP, and PTV4D-CT of 3.6, 2.78, and 2.94 mm in relative to the PTVFBCT, respectively. These shifts are likely owing to fast CT acquisition, where the center of the tumor may be captured on any phase of a breathing cycle, which is not representative of the COM seen on AIP-CT. This effect is seen in Fig. 4 which shows the variable positions of the PTV4D-CT/PTVMIP (in yellow) relative to the GTVs (in cyan) from the FBCT. Since the COM of FBCT is not a reproducible estimate of tumor position, we recommend bony registration of other CT scans with the FBCT planning scan in order to avoid COM misalignment during transfer of contours.
Despite limitations, free-breathing CT is still commonly used as the reference CT for treatment planning and IGRT [7]. Some centers continue to prefer FBCT for planning because of concerns about inferior imaging quality of the 4D-CT-derived series and inability to place an iso-center directly on AIP-CT as it is synthetic CT. Others are concerned about the relationship of the CT number to electron density in AIP-CT, which may affect the dose calculation accuracy. Current RTOG protocols still allow the free-breathing CT be used as the primary planning CT while also allowing a variety of ITV creation methods [8].
By contrast, when AIP CT is used as the planning CT, PTV4D-CT or PTVMIP have no significant COM displacement, confirming that AIP-CT is a reliable planning CT [6]. The same is not true, however, for PTVFBCT and PTVBHCT, where mean COM shifts of 2.94 and 4.35 mm, respectively, were observed. Once again, to avoid COM displacement, the PTV and FBCT/BHCT to AIP-CT fusion should be performed using bony registration.
Other studies have addressed the challenges of 4D-CT-based planning and have suggested that employing AIP-CT as planning CT is feasible by applying correction parameters to achieve comparable Hounsfield units to account for tissue electron density in treatment planning [9, 10]. While differences in Hounsfield units between FBCT and AIP-CT exist, we speculate that displacement of center of mass on FBCT is likely to be more problematic for tumor coverage.
At the time of treatment delivery, selection of the appropriate reference image for CBCT delivery is crucial as similar problems of alignment can occur. If the FBCT is used as the reference image for aligning to the tumor seen on kV-CBCT at the time delivery, aligning tumor to tumor could, paradoxically, introduce an isocenter displacement. In contrast, the COM of PTVMIP and PTV4D-CT to COM of tumor on AIP-CT are consistent. Phantom studies have confirmed that the tumor projections obtained from kV-CBCT are most similar to AIP-CT [11]. Our study validates this consistency for a series of consecutive patients. By contrast, aligning PTVFBCT or PTVBHCT is problematic, and the resultant systematic error exceeded the typical ITV to PTV expansion of 5 mm for 5.6 % of the patients in our study.
While COM magnitude shifts are minimized with 4D-CT/MIP for target delineation and AIP CT for planning and IGRT alignment, larger COM magnitude shifts will not necessarily result in a target miss. When COM magnitude shifts are small, PTV margin could account for the displacement while still accounting for mechanical setup and other random error inherent in SBRT delivery. Also, the larger PTV volumes created with BHCT and FBCT could account for the increased COM displacement. Nonetheless, as illustrated in Figs. 2c and 3c, COM displacement may exceed these factors. However, even in this situation, high doses in SBRT immediately beyond the edge of the PTV could still prevent a marginal failure.
Our study is limited by its retrospective design. Also, since all contours were created by one author, the resulting ITVs and PTVs may be more similar than if contoured by different investigators. We did attempt to limit any bias by varying the order in which GTVs were contoured, but awareness of previous contours could not be completely avoided. This approach potentially minimizes differences and would be likely to minimize center of mass shifts and should not bias the study’s significant findings. Also, we accounted for slight differences in COM resulting from slight differences in contours between scans though comparison of COM between volumes on different phases of the 4D-CT. Our study does not assess the impact of aligning using 4D-CBCT, but similar principles in terms of COM are likely to apply.
Conclusions
The center of mass (COM) of the PTVFBCT, PTVBHCT, and PTV4D-CT is inconsistent, exhibiting significant shifts relative to each other. PTV4D-CT COM is consistent with GTV on AIP-CT, while PTVFBCT and PTVBHCT exhibited significant displacement. PTVBHCT, PTVMIP, and PTV4DCT are all discordant with COM of GTV on FBCT. Use of 4D-CT/MIP for target delineation and AIP CT for planning and IGRT alignment is recommended. Alternative methods of target delineation combined with AIP-CT for planning and IGRT may introduce systematic error greater than or equal to the PTV margin in over 5 % of treatments.
References
Timmerman R, Paulus R, Galvin J et al (2010) Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA 303:1070–1076
Pan H, Simpson DR, Mell LK, Mundt AJ, Lawson JD (2011) A survey of stereotactic body radiotherapy use in the United States. Cancer 117:4566–4572. doi:10.1002/cncr.26067
Hof H, Muenter M, Oetzel D, Hoess A, Debus J, Herfarth K (2007) Stereotactic single-dose radiotherapy (radiosurgery) of early stage nonsmall-cell lung cancer (NSCLC). Cancer 110:148–155. doi:10.1002/cncr.22763
Fritz P, Kraus HJ, Blaschke T et al (2008) Stereotactic, high single-dose irradiation of stage I non-small cell lung cancer (NSCLC) using four-dimensional CT scans for treatment planning. Lung Cancer 60:193–199. doi:10.1016/j.lungcan.2007.10.005
Wang L, Hayes S, Paskalev K, Jin L, Buyyounouski MK, Ma CC, Feigenberg S (2009) Dosimetric comparison of stereotactic body radiotherapy using 4D CT and multiphase CT images for treatment planning of lung cancer: evaluation of the impact on daily dose coverage. Radiother Oncol 91:314–324. doi:10.1016/j.radonc.2008.11.018
Bradley JD, Nofal AN, El Naqa IM et al (2006) Comparison of helical, maximum intensity projection (MIP), and averaged intensity (AI) 4D CT imaging for stereotactic body radiation therapy (SBRT) planning in lung cancer. Radiother Oncol 81:264–268. doi:10.1016/j.radonc.2006.10.009
Wang Z, Wu QJ, Marks LB, Larrier N, Yin FF (2007) Cone-beam CT localization of internal target volumes for stereotactic body radiotherapy of lung lesions. Int J Radiat Oncol Biol Phys 69:1618–1624
American College of Radiology Imaging Network Randomized Phase II Trial of Individualized Adaptive Radiotherapy Using During-Treatment FDG-PET/CT and Modern Technology in Locally Advanced Non-Small Cell Lung Cancer (NSCLC). http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=1106. Accessed 6/2/20142014
Admiraal MA, Schuring D, Hurkmans CW (2008) Dose calculations accounting for breathing motion in stereotactic lung radiotherapy based on 4D-CT and the internal target volume. Radiother Oncol 86:55–60. doi:10.1016/j.radonc.2007.11.022
Guckenberger M, Wilbert J, Krieger T, Richter A, Baier K, Meyer J, Flentje M (2007) Four-dimensional treatment planning for stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 69:276–285
Shirai K, Nishiyama K, Katsuda T, Teshima T, Ueda Y, Miyazaki M, Tsujii K (2014) Phantom and clinical study of differences in cone beam computed tomographic registration when aligned to maximum and average intensity projection. Int J Radiat Oncol Biol Phys 88:189–194. doi:10.1016/j.ijrobp.2013.09.031
Acknowledgments
We appreciate the assistance of Anthony Mastroianni, MD, and Lorelei Woody for their review of this manuscript.
Funding
No grant or additional financial support was received for this research.
Conflict of interest
Dr. Xia reports grants from Siemens Medical Solutions, grants from Philips Medical Systems, and grants from BrainLab, outside the submitted work. Dr. Woody, Dr. Djemil, Dr. Stephans, and Dr. Videtic declare that they have no conflicts of interest pertaining to the conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Woody, N.M., Stephans, K.L., Videtic, G.M.M. et al. Systematic errors in lung stereotactic body radiation therapy (SBRT): a caution on mixing and matching target delineation methods and planning CTs. J Radiat Oncol 4, 185–191 (2015). https://doi.org/10.1007/s13566-015-0194-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-015-0194-7