Abstract
Background
Monogenic diabetes mellitus (MDM) represents a diverse group of uncommon form of diabetes. Based on the number of reported cases in literatures, it appears that the detection rate of MDM, even in specialized diabetes centers, remains low. This case series provides a comprehensive overview of different MDM cases observed at a single diabetes center, focusing on their clinical features, diagnostic challenges, and management considerations.
Methods and Results
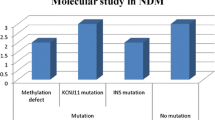
We identified 10 cases of MDM by conducting genetic analysis of 77 youth-onset diabetes cases clinically suspected to be MDM. Among these, there were 2 cases of neonatal diabetes mellitus (NDM) [a heterozygous mutation p.Arg825Trp in the ABCC8 gene (transient NDM) and a heterozygous mutation in p.Asp212Tyr in the ABCC8 gene (permanent NDM)], 3 cases of HNF4A MODY (MODY)-1 [a heterozygous promoter mutation 79C/T in the HNF4A gene, a novel heterozygous missense variant in exon 8 of the HNF4A gene that results in the amino acid substitution of serine for arginine at codon 976 (p.Arg326Ser), and a heterozygous mutation p. Arg333Cys in exon 8 of the HNF4A gene], and 4 cases of maternally inherited diabetes and deafness (MIDD) [heteroplasmic missense mutation in the MT-TL1 position (m.3243A>G) encoding for the leucine transfer RNA].
Conclusion
This case series highlights that MDM can be effectively identified in diabetes clinics through careful clinical evaluation and targeted genetic testing. Early detection allows for personalized treatment strategies, optimizing glycemic control, and pre-empt, prevent, or modify associated clinical features to improve patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monogenic diabetes mellitus (MDM) constitutes a relatively uncommon subset of non-autoimmune diabetes mellitus (DM), comprising 1–2% of all DM cases [1]. They range from 1 to 5% of the pediatric and young adult DM population [2] but remain insufficiently diagnosed pointing to the need for increasing awareness of these unique forms of diabetes.
MDM is classified into neonatal DM (NDM) characterized by early-onset DM and maturity-onset diabetes of the young [MODY] occurring in adolescents or young adults [3]. Syndromic DM, syndromes of severe insulin resistance (SSIR), and lipodystrophy are the other subtypes of MDM. The same MDM gene can contribute to different forms of DM with early or late onset, depending on the functional impact of the variant and the same pathogenic variant can produce variable DM phenotypes, even within the same family. The probability of MDM should be reliably estimated by clinical criteria and phenotype.
Diagnosing MDM within a clinical setting poses considerable challenges, primarily due to the overlapping characteristics with type 1 DM (T1D1M) or type 2 DM (T2DM), and often leads to misdiagnosis [4, 5]. The relative paucity of awareness among physicians about MDM further exacerbates this issue. Additionally, the limited accessibility and availability of genetic diagnostic centers in the region, along with the high costs involved, further complicate the situation. Moreover, the considerable time and effort required by physicians to counsel and persuade patients about the necessity of genetic testing serve as significant deterrents to its more widespread recognition.
Out of a total of 77 probands with clinical suspicion of MDM, our clinic in Kozhikode, Kerala, has successfully identified 10 cases in collaboration with a genetic testing center in Chennai. We present this case series to emphasize the importance of recognizing MDM cases in all clinical settings, as early detection can contribute to improved management and the possibility of stopping insulin and changing over to inexpensive sulphonylurea (SU) tablets in many of these cases.
Case presentations
Neonatal diabetes mellitus (NDM)
Case no. 1
This was a 60-day-old male infant with a 2.5-kg birth weight admitted for the management of neonatal hepatitis and sepsis. His blood glucose and glycated hemoglobin (HbA1C) were high. He had a C-peptide level of 0.098 ng/mL (normal, 0.5–2 ng/mL) and negative islet autoantibodies [glutamic acid decarboxylase (GAD), islet antigen-2 (IA-2), and zinc transporter 8 (ZnT8)]. No developmental delay or neurological symptoms were noted at presentation and there was no family history of DM. He was initially treated with insulin. His blood sample was sent for genetic analysis, and the result showed a heterozygous mutation in p.Asp212Tyr in the ABCC8 gene which was associated with permanent NDM. Insulin therapy was withdrawn and converted to a SU, glibenclamide 2.5 mg twice daily administered orally which yielded good control of blood glucose values. However, the patient experienced a significant increase in blood glucose values on two occasions after discontinuing SU therapy (Fig. 1). In 2016, random blood glucose (RBG) levels spiked to 450 mg/dL and HbA1c increased to 10%, and in 2021, fasting blood glucose (FBG) levels were at 273 mg/dL, postprandial blood glucose (PPBG) levels at 388 mg/dL, and HbA1C reached 11.4% (Fig. 2). These elevated values normalized when SU therapy was resumed. This provided further confirmation of the diagnosis of permanent neonatal diabetes mellitus (PNDM).
Case no. 2
The second case was a 17-year-old male presenting for the control of blood glucose. His FBG was 192 mg/dL, PPBG was 282 mg/dL, and HbA1C was 12.5%. Notably, he had a history of transient neonatal hyperglycemia during the first year of his life, which resolved spontaneously. His fasting and random C-peptide levels were 0.69 ng/mL and 1.61 ng/mL, respectively, and islet autoantibodies were negative. His BMI was 19.9 kg/m2. He had been initiated on insulin therapy at another hospital 3 days prior to this presentation. There was a history of DM in his paternal grandmother. The prior history of transient hyperglycemia in early childhood raised suspicions of neonatal DM, leading to a genetic analysis of the patient’s sample. The genetic results revealed a heterozygous mutation p.Arg825Trp in the ABCC8 gene which was associated with transient NDM. It was therefore clear that he had TNDM which was remitted by the first birthday but recurred in adolescence. His insulin treatment was discontinued, and he was switched over to oral glibenclamide 2.5 mg twice daily. His blood glucose levels remained well-controlled, except on two occasions when he skipped his medications, causing a spike in blood sugar. However, the levels returned to normal after he resumed taking the medication (Fig. 3).
HNF4A-MODY
We have three cases of HNF4A-MODY. Comparison of their clinical characteristics and laboratory data is presented in Table 1.
Case no. 3
This was a 39-year-old female who is a doctor by profession working overseas. She approached us for blood glucose control. She had a history of DM for a duration of 4 years for which she was taking metformin 1000 mg at night. She reported consistently high FBG levels with FBG of 159 mg/dL and HbA1C of 6.5% at presentation. Her highest PPBG reported was 160 mg/mL, and her random C-peptide level was 3.3 ng/mL. She had a history of gestational DM for which she was treated with insulin. She had been diagnosed with hypothyroidism with a positive anti thyroperoxidase antibody (anti-TPO antibody) of 38 IU/mL (NV < 34 IU/mL) and a negative thyroglobulin antibody level of 3.2 IU/mL (NV < 116 IU/mL) and was on levothyroxine 100 mcg once daily. Her BMI was 22.4, waist circumference was 81 cm, visceral fat was 5%, and lipid profile and liver function tests (LFT) were normal. She had a positive family history of DM in her father, paternal grandmother, and paternal uncles. She was initially suspected to have glucokinase (GCK) MODY due to her consistently high FBG despite taking metformin 1000 mg at night. However, her genetic analysis result showed a novel heterozygous missense variant in Exon 8 of the HNF4A gene (MODY-1) that resulted in the amino acid substitution of serine for arginine at codon 976 (p.Arg326Ser). The patient has switched over to gliclazide 30 mg at night and is doing well now.
Case no. 4
A 21-year-old male with a history of 4 years of DM was referred to us for blood glucose control. His BMI was 23.5 kg/m2, waist circumference was 70 cm, and visceral fat was 6%. His FBS and PPBS were 172 mg/dL and 265 mg/dl, respectively, and HbA1C was 7.8%. His random C-peptide level was 1.3 ng/mL, and islet autoantibodies were negative. The lipid profile was normal and serum glutamic oxaloacetic transaminase (SGOT) and serum glutamic pyruvic transaminase (SGPT) values were 30.8 IU/mL and 41.4 IU/mL, respectively. He had a family history of DM in his mother, father, and maternal uncle. His genetic analysis result showed a heterozygous mutation p. Arg333Cys in Exon 8 of the HNF4A gene (MODY-1). He was prescribed Gliclazide 40 mg once daily. His blood glucose and HbA1c improved and he continues to do well (Figs. 4 and 5).
Case no. 5
A 25-year-old female presented with symptoms of DM (polyuria, polydipsia, and polyphagia) over a duration of 3 months. Her FBG and PPBG were 170 mg/dL and 259 mg/dL, respectively, and her HbA1C was 11.9%. Her BMI was 27.5 kg/m2, waist circumference 86 cm, visceral fat 7%, fasting C-peptide 0.41 ng/mL, random C-peptide 0.7 ng/mL, and islet autoantibodies were negative. Her lipid profile and LFT were normal. She had a family history of DM in her father, two brothers, paternal grandparents, and maternal grandmother. Her genetic analysis results revealed a heterozygous promoter mutation 79C/T in the HNF4A gene (MODY 1). Before the genetic results were available, the patient was initially prescribed a combination of metformin and sitagliptin. Later, her treatment was switched over to glimepiride 2 mg twice daily. Unfortunately, the patient was subsequently lost to follow-up.
Case no. 6
Maternally inherited diabetes and deafness (MIDD)
We have identified a total of four cases of MIDD at our center. Among these cases, three were previously reported in a separate case series which was the largest case series of MIDD reported in India so far [6]. Here, we present a detailed clinical profile of the fourth case of MIDD.
A 40-year-old female with 22 years of DM on glimepiride presented with significant weight loss, fatigue, and pain under the left heel. She had a positive family history of DM in her mother, sister, maternal grandmother, maternal aunts, and cousins. She had no history of hearing loss. Her height was 152 cm, weight was 48.7 kg, BMI was 21.08 kg/m2, waist circumference was 79 cm, and visceral fat was 3%. Clinical examination showed mild diabetic peripheral neuropathy and plantar fasciitis. The findings of lab investigations were as follows: FBG 234 mg/dL, PPBG 301 mg/dL, HbA1C 9.3%, random C-peptide 1.4 ng/mL, negative islet auto-antibodies and serum creatinine 0.9 mg/dL. The results of the lipid profile, liver function tests, ECG, echocardiogram, and treadmill test were all normal.
Blood samples were sent for genetic analysis and the test results confirmed MIDD by the detection of a heteroplasmic missense mutation in the MT-TL1 gene namely, A to G transition at 3243 position (m.3243A > G) encoding for the leucine transfer RNA. The patient was informed about the diagnosis, and she was treated with insulin and mitochondriotropic agents like coenzyme Q10, L-carnitine, and vitamin E, and her blood glucose control and symptoms improved.
Discussion
The reporting of monogenic diabetes mellitus (MDM) cases in India is lower compared to Western populations. While MDM, particularly MODY, has been extensively studied and documented in Western populations, its recognition and reporting in India have been comparatively limited [7,8,9,10,11,12,13,14,15,16]. This difference could be attributed to various factors, including differences in healthcare infrastructure, awareness among healthcare professionals, access to genetic testing facilities, and genetic predispositions within populations.
However, there has been an increasing awareness of MDM in India in recent years, with more studies focusing on its prevalence, clinical characteristics, and genetic underpinnings within the Indian population [17, 18]. Efforts are being made to improve the diagnosis and management of MDM in India, including the establishment of specialized centers and collaborations with international research groups.
This case series provides a comprehensive overview of various types of MDM picked up from a single diabetes center at Kozhikode in Kerala. To our knowledge, this represents the largest and most diverse collection of MDM cases reported from a standalone secondary care outpatient diabetes center without in-house genetic testing facilities in India. The discussion of these cases offers valuable insights into the prevalence pattern, clinical characteristics, diagnostic challenges, and management considerations associated with different subtypes of MDM from a diabetes clinic perspective. It underscores the significance of considering MDM as a differential diagnosis, particularly in cases where there is an atypical presentation or a lack of response to conventional treatments.
Misdiagnosing MDM as either T1DM or T2DM is common due to their overlapping clinical features. Thus, accurately identifying MDM is essential for tailoring management to the specific genetic subtype, thereby enhancing treatment outcomes and reducing complications, and a recent study illustrates how this can be done in an Indian setting [19]. For example, if HNF1A MODY, HNF4A MODY, and NDM are diagnosed as T1D, they will be treated with insulin lifelong and the response is likely to be poor. In our case series, before diagnosing MODY and NDM, many patients were diagnosed as either T1DM or T2DM and were put on insulin or other oral hypoglycemic agents with inadequate control of their diabetes. However, after initiating targeted treatments such as SU for these specific subtypes, patients exhibited significant and consistent improvement over the years. Unlike in T2DM, where SU treatment may fail or require intensification with multiple drugs over time, our cases demonstrated sustained improvement on the same dose of SU, even after years of treatment. Aside from one or two instances of blood glucose spikes due to missed medication, patients generally maintained smooth blood glucose control over the years. This underscores the importance of accurate diagnosis and the implementation of specific treatments for optimal management of these cases. Different genetic variations of MDM may necessitate distinct treatment approaches. Recognizing MDM cases allows for personalized treatment strategies, including medication selection and lifestyle interventions, to optimize glycemic control and minimize long-term complications [20, 21].
Family screening plays a crucial role in MDM due to its genetic basis and varied clinical presentations. It helps identify asymptomatic cases, especially among relatives of affected individuals, enabling early diagnosis and preventive measures like lifestyle modifications. Furthermore, understanding genetic predispositions aids in personalized treatment decisions, facilitates genetic counseling for comprehending inheritance patterns, and has family planning implications.
Exploring the prevalence and genetic diversity of MDM contributes to a better understanding of the disease’s epidemiology and underlying genetic mechanisms. This information can help healthcare planning, resource allocation, and research efforts aimed at improving diagnostic accuracy, treatment options, and preventive strategies.
Furthermore, the successful identification of MDM cases in our clinic demonstrates the feasibility of employing clinical screening methods, even in settings with limited resources for genetic testing. Collaboration with genetic testing centers has proven instrumental in confirming the diagnosis and elucidating the underlying genetic mutations thereby facilitating improved patient outcomes and a reduction in long-term complications. We would like to appeal to all pediatric endocrinology centers, diabetes centers, and neonatal clinics to try to diagnose MDM so that the quality of life of those diagnosed can be improved and unnecessary lifelong insulin can be avoided.
Conclusion
A comprehensive clinical evaluation, along with targeted genetic testing, can significantly improve the detection of MDM, even in primary or secondary diabetes care settings. Early identification is crucial for optimizing treatment outcomes and enhancing the patient's quality of life.
References
Shields BM, Hicks S, Shepherd MH, Colclough K, Hattersley AT, Ellard S. Maturity-onset diabetes of the young (MODY): how many cases are we missing? Diabetologia. 2010;53:2504–8.
Riddle MC, Philipson LH, Rich SS, Carlsson A, Franks PW, Greeley SAW, Nolan JJ, Pearson ER, Zeitler PS, Hattersley AT. Monogenic diabetes: from genetic insights to population-based precision in care. Reflections from a diabetes care editors’ expert forum. Diabetes Care. 2020;43:3117–28.
Fajans SS, Bell GI. MODY: history, genetics, pathophysiology, and clinical decision making. Diabetes Care. 2011;34:1878–84.
Doria A, Patti ME, Kahn CR. The emerging genetic architecture of type 2 diabetes. Cell Metab. 2008;8:186–200.
Ledermann HM. Maturity-onset diabetes of the young (MODY) at least ten times more common in Europe than previously assumed? Diabetologia. 1995;38:1482.
Sureshkumar P, Radha V, Mohan V, et al. Maternally inherited diabetes and deafness (MIDD)—a series of case reports. Int J Diabetes Dev Ctries. 2023;43:583–6.
Anuradha S, Radha V, Deepa R, Hansen T, Carstensen B, Pederson O, Mohan V. A prevalent amino acid polymorphism at codon 98 (Ala98Val) of the hepatocyte nuclear factor-1A is associated with maturity onset diabetes of the young and younger age at onset of type 2 diabetes in Asian Indians. Diabetes Care. 2005;28:2430–5.
Radha V, Ek J, Anuradha S, Hansen T, Pedersen O, Mohan V. Identification of novel variants in the hepatocyte nuclear factor 1 alpha gene in South Indian patients with maturity onset diabetes of young. J Clin Endocrine Metab. 2009;94:1959–65.
Chapla A, Mruthyunjaya MD, Asha HS, et al. Maturity onset diabetes of the young in India – a distinctive mutation pattern identified through targeted next-generation sequencing. Clin Endocrinol. 2015;82(4):533–42.
Nair VV, Chapla A, Arulappan N, Thomas N. Molecular diagnosis of maturity onset diabetes of the young in India. Indian J Endocrinol Metab. 2013;17(3):430–41.
Sarkar A, Rajamani JI. Maturity onset diabetes of the young: the Indian scenario. IJOPP [Internet]. 2022;15(1):01–7.
Radha V, Mohan V, Rakesh K. Genetics for the pediatric endocrinologists-1 diagnosis of monogenic diabetes among children and adolescents. J Pediatr Endocrinol Diab. 2022;22:23–30.
Kashyap A, Sharma KN. An overview of monogenic diabetes in the Indian subcontinent. 2023;7(1):32–41.
Jahnavi S, Poovazhagi V, Mohan V, Sureshkumar P, et al. Clinical and molecular characterization of neonatal diabetes and monogenic syndromic diabetes in Asian Indian children. Clin Genet. 2013;83:439–45.
Nayak S, Sarangi AN, Sahoo SK, et al. Neonatal diabetes mellitus: novel mutations. Indian J Pediatr. 2021;88:785–92.
Sampathkumar G, Valiyaparambil PP, Kumar H, et al. Low genetic confirmation rate in South Indian subjects with a clinical diagnosis of maturity-onset diabetes of the young (MODY) who underwent targeted next-generation sequencing for 13 genes. J Endocrinol Invest. 2022;45:607–15.
Lakshmanan NK, Pavithran PV, Bhavani N, Abraham N, et al. Monogenic diabetes: a single center experience from South India. Pediatr Diabetes. 2021;22(1):75–81.
Radha V, Mohan V, Rakesh K. Genetics for the pediatric endocrinologists-1 diagnosis of monogenic diabetes among children and adolescents. J Pediatr Endocrinol Diab. 2022;2:23–30.
Aarthy R, Aston-Mourney K, Amutha A, Mikocka-Walus A, Anjana RM, Unnikrishnan R, Jebarani S, Venkatesan U, Gopi S, Radha V, Mohan V. Identification of appropriate biochemical parameters and cut points to detect maturity onset diabetes of young (MODY) in Asian Indians in a clinic setting. Sci Rep. 2023;13:11408.
Mohan V, Radha V. Precision diabetes is slowly becoming a reality. Med Princ Pract. 2019;28:1–9.
Unnikrishnan R, Radha V, Mohan V. Challenges involved in incorporating personalised treatment plan as routine care of patients with diabetes. Pharmgenomics Pers Med. 2021;14:327–33.
Acknowledgment
We would like to thank the Indian Council of Medical Research (ICMR) for funding the genetic analysis through Dr V Radha’s project “Investigations of the Association of Mutations in MODY and NDM by Translational Genomic Research.” We would like to thank M/S Servier and Serdia Pharmaceuticals, India for supporting the genetic testing of some of the MODY participants in this project. Dr. P. Sureshkumar would like to thank the Madras Diabetes Research Foundation (MDRF) in Chennai for their help with the genetic studies. We also acknowledge Dr. Anusree E, PharmD for her assistance with the manuscript preparation and typing.
Funding
This genetic study was funded by ICMR through Dr. V Radha’s project “Investigations of the Association of Mutations in MODY and NDM by Translational Genomic Research.”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study protocol was approved by the Institutional Ethics Committee of Dr. Suresh’s DiabcareIndia. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
We confirm that we have obtained written consent from our patients to publish their case histories in the International Journal of Diabetes in Developing Countries.
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sureshkumar, P., Radha, V., Unnikrishnan, R. et al. Clinical profile of monogenic diabetes: A case series from a single South Indian diabetes clinic. Int J Diabetes Dev Ctries (2024). https://doi.org/10.1007/s13410-024-01403-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13410-024-01403-8