Abstract
Even though beta thalassemia major (β-TM) patients’ survival has improved, there are growing concerns about long-term complications and its related therapeutic side effects. We aimed to investigate the prevalence of metabolic syndrome in the β-TM patients in southern Iran. This cross-sectional study was conducted on 100 beta thalassemia major patients, aged 12–40 years and their age- and gender-matched controls. Weight, height, blood pressure, and waist circumference of the patients were evaluated by a single trained physician. Serum triglyceride, total cholesterol, high-density lipoprotein, low-density lipoprotein, and fasting plasma glucose were assessed. World Health Organization (WHO) body mass index (BMI) curves and International Diabetes Federation (IDF) metabolic syndrome criteria were used as a reference. Statistical Package for Social Sciences (SPSS) software version 18.0 was used for analysis. Prevalence of underweight, overweight, and obesity in our patients was 28, 5, and 1%, respectively. In patients with thalassemia (β-TM), prevalence of metabolic syndrome was 22% and was associated with BMI (p = 0.001). It was more prevalent in females (26.3% in females vs. 8.3% in males) (p = 0.045). Serum ferritin was associated with abdominal obesity (p = 0.028) and hypertriglyceridemia (p = 0.017). This study revealed that 22% of β-TM patients had IDF criteria of metabolic syndrome and low HDL was the most frequent positive criterion. Future studies should be conducted to find out the relevant factors to reduce the cardiovascular morbidities associated with metabolic syndrome in β-TM patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Beta thalassemia major (β-TM) is a hereditary anemia resulting from the absence or severe deficiency of β-globin chain production, which leads to chronic hemolytic anemia [1]. These patients are in need of regular blood transfusion to improve oxygen carrying capacity and their overall wellbeing. However, such treatment might lead to iron overload and its related morbidities, such as cardiac, liver, and endocrine system damages [2]. In recent decades, combination of blood transfusion and iron-chelating therapies has improved the life expectancy and quality of life of β-TM patients [3].
While β-TM patients’ survival has improved, there are growing concerns about long-term complications of this disease and its related therapies [2]. One important complication can be metabolic syndrome, which is accompanied by hyperglycemia, dyslipidemia, abdominal obesity, and hypertension. Metabolic syndrome can increase cardiovascular atherosclerotic risks and diabetes mellitus [4]. Hyperinsulinemia and insulin resistance are well documented in β-TM patients [1, 4,5,6,7]; however, its association with metabolic syndrome has not been investigated. Furthermore, there are some sporadic reports about hypertension [8], hypertriglyceridemia [9, 10], and obesity [11]. To the best of our knowledge, there has been no report about the prevalence of metabolic syndrome in β-TM patients. Consequently, we aimed to investigate the prevalence of metabolic syndrome in β-TM patients in southern Iran.
Material and methods
The present cross-sectional study was conducted in thalassemia clinics affiliated to Shiraz University of Medical Sciences, Fars Province, Iran, in 2015. All patients were registered in these clinics after the clinical diagnosis and peripheral blood evaluation and hemoglobin electrophoresis. We enrolled 100 patients with beta thalassemia major, selected through simple randomized sampling. Diabetes mellitus and secondary hypertension were our exclusion criteria. Also, adolescents, who had any type of disability that would prevent us from measuring their weight, height, and waist circumference, and pregnant women were excluded from the study. Healthy age- and gender-matched adolescents were enrolled in the control group. Controls were randomly selected from a cohort study in Kavar, located in south of Fars Province, which include 478 normal population checked for metabolic syndrome.
The patients were transfusion-dependent before the age of 2. All patients were treated with deferoxamine as an iron-chelating therapy. This study was approved by both the local ethics committee and vice-chancellor of research at Shiraz University of Medical Sciences. All patients signed a written informed consent.
Anthropometric data and blood pressure
Weight and height of patients were assessed by a single trained physician. While the patient was standing without shoes; height was measured using an Altura Exata portable stadiometer and the number was rounded to the nearest 0.5 cm. Weight was evaluated using a standard scale (Seca, Germany), while the patient wore light clothes, which was rounded to the nearest 0.1 kg. Body mass index (BMI) was calculated through the standard formula:
We classified the patients according to the World Health Organization (WHO) BMI curves specified by age and gender into four categories [12]: underweight, BMI Z score < − 2; normal, − 2 ≥ Z < +1; overweight, + 1 ≥ Z < +2; and obese adolescents, BMI Z score more than + 2.
Waist circumference (WC) was measured with a Sanny inelastic measuring tape at the midpoint between the last rib and the iliac crest, while the patient was standing relaxed.
Blood pressure (BP) was assessed with a mercury sphygmomanometer (Riester, Germany) using a standard method [13]. The recorded blood pressure was the mean of two BP readings with a 5-min interval in a sitting position.
Biochemical measurements
Serum triglyceride (TG), total cholesterol (Chol), high-density lipoprotein (HDL), low-density lipoprotein (LDL), and fasting plasma glucose (FPG) were assessed on a Dirui-T-240 auto-analyzer with an enzymatic method (New and high Tec, Jilin, China), in Shiraz endocrinology and metabolism research center.
Metabolic syndrome definition
We used the International Diabetes Federation (IDF) consensus worldwide definition to define metabolic syndrome [14]. According to these criteria, presence of at least three of the below components was classified as metabolic syndrome:
-
(1)
Central obesity (< 16 years: WC ≤ 90th percentile and ≤ 16 years: WC ≤ 94 cm in males and ≤ 80 cm in females), which is defined for Eastern Mediterranean and Middle East population.
-
(2)
Raised TG level: ≤ 150 mg/dL
-
(3)
Reduced HDL cholesterol: < 40 mg/dL in males and < 50 mg/dL in females
-
(4)
Raised blood pressure: systolic BP ≤ 130 mmHg or diastolic BP ≤ 85 mmHg
-
(5)
Raised FPG: FPG ≤ 100 mg/dL
Statistics
Statistical analysis was conducted using Statistical Package for Social Sciences (SPSS) software version 18.0. Numerical data was mentioned as mean ± SD. p value less than 0.05 was considered as significant. Normality of data distribution was evaluated using Kolmogorov-Smirnov test. We compare normally distributed data by Student’s t test and not-normal ones by Mann-Whitney test. Qualitative data comparisons were carried out using chi-square test.
Results
One hundred patients with beta thalassemia major aged 23.7 ± 5.9 years and their age- and gender-matched controls were enrolled in this study (Table 1). Patients with thalassemia included 24 males and 76 females, and controls included 36 males and 64 females (p value = 0.07). General characteristics and biochemical studies of our patients were defined by gender shown in Table 2. Male patients had higher diastolic blood pressure (p = 0.018), higher serum ferritin level (p = 0.002), and lower HDL level (p = 0.024). Prevalence of underweight, overweight, and obesity in our patients was 28, 5, and 1%, respectively. BMI categories according to WHO classification in both genders of our patients and controls are shown in Table 3. BMI of thalassemia patients is lower than that of the controls (p < 0.001). We also did not observe any significant difference between prevalence of overweight or obesity among both genders (p = 0.23).
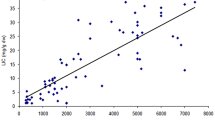
Prevalence of hyperglycemia, abdominal obesity, low HDL, hypertriglyceridemia, and hypertension in patients with thalassemia was 32, 32, 90, 23, and 4%, respectively. Figure 1 and Table 4 reveal that metabolic syndrome was more prevalent in thalassemia patients (p < 0.001). Table 5 shows that there was no significant difference between the prevalence of these criteria in males and females with thalassemia major, except for abdominal obesity, which was more prevalent in females (p < 0.001). Data revealed that 22% of our patients had metabolic syndrome, which was more prevalent in females (26.3% in females vs. 8.3% in males), (p = 0.045). Metabolic syndrome in our patients was associated with BMI (p = 0.001). However, it was not associated with age (p = 0.217), ferritin (p = 0.702), hemoglobin (p = 0.734), and transfusion intervals (p = 0.215). Serum ferritin was associated with abdominal obesity (p = 0.028) and hypertriglyceridemia (p = 0.017), but it was not associated with hyperglycemia (p = 0.381), hypertension (p = 0.33), and low HDL (p = 0.073).
Discussion
The present study revealed that 6% of our thalassemic patients were either overweight or obese. Also, it was shown that 22% of our β-TM patients had metabolic syndrome, and low HDL was the most frequent positive criterion. The present study showed that metabolic syndrome was more prevalent in females. Furthermore, it was shown that metabolic syndrome was associated with BMI; whereas, abdominal obesity and hypertriglyceridemia were associated with serum ferritin.
Prevalence of metabolic syndrome in adults is 26–29% (16–20% in males and 30–37% in females) in Iran [13, 15,16,17,18,19,20], and abdominal obesity is the most prevalent positive criterion. We showed that 2% of healthy adolescents (aged 22.6 ± 5.8 years) in southern Iran have metabolic syndrome, and also low HDL was the most common criterion. However, there is no validated data about the prevalence of metabolic syndrome in β-TM patients. Hence, it was revealed that 8.3% of males and 26.3% of females with β-TM have metabolic syndrome, which is in a similar range of the normal population. However, low HDL was the most prevalent criterion in β-TM patients. Gozashti et al. revealed that prevalence of metabolic syndrome in minor β-TM patients was lower than that in the normal population, and they proposed that minor thalassemia might act as a protective factor for metabolic syndrome [21].
Abnormal glucose tolerance and insulin resistance were previously reported in multi-transfused β-TM patients [5,6,7, 22]. Also, it was shown that insulin resistance was associated with metabolic syndrome [19, 20]. In β-TM patients, hyperglycemia might be due to early impairment of β cell function and insulin resistance. Iron overload and chronic hepatitis C (HCV) could play a significant role in this regard [6]. Some previous studies reported the relationship between serum ferritin levels and insulin resistance in non-diabetic women [23], in over weight and obese population [24], and in Korean men [25]. These results suggest that iron overload is associated with insulin resistance even in non-thalassemic populations [25]. Our result revealed that there is a high prevalence of hyperglycemia (32%) in major thalassemic patients; however, it was not associated with serum ferritin. Also, Kirim et al. revealed that there was no association between β-TM minor and metabolic syndrome criteria, regardless of insulin resistance [26]. Other possible explanation could be liver damage or HCV infection that might play an important role in hyperglycemia of β-TM patient that needs to be investigated in future studies.
Fung et al. reported that 26.5% of non-transfused thalassemia in Canada had BMI of more than 25. This was more than that of non-transfused thalassemia, and females had higher body fat index in comparison to men [11]. It was shown that 6% of our β-TM patients had BMI of more than 25, while, 32% of β-TM patients had abdominal obesity, which was significantly higher in women. The differences between the Fung et al. study and our report could be attributed to the differences in culture and lifestyle [27]. They also revealed that abdominal obesity was associated with serum ferritin. Fung et al. suggested that hypogonadism and growth hormone deficiency secondary to iron overload in β-TM patient played an important role in abdominal obesity [11].
Low level of total cholesterol accompanied with low serum HDL, low serum LDL, and hypertriglyceridemia was well shown in β-TM patients [10, 28,29,30,31,32]. This might be due to increased erythropoiesis that could result in increased cholesterol requirement for cell membrane formation in these patients [29, 33]. Some studies have found a link between serum ferritin and changes in lipid profile of β-TM patients [34, 35]. Khera et al. also reported on a syndrome called hypertriglyceridemia thalassemia in four β-TM patients [9]. Even though pathogenesis of such syndrome is still unclear, it might be associated with high risk of developing atherosclerosis and acute pancreatitis at a young age [9]. Bordbar et al. revealed a genotype-phenotype correlation between lipid profile and different β-globin gene mutations [10]. The most severe gene mutation (β°/β°) in thalassemia patients is accompanied with high reduction in serum lipids [10]. In the present study, we found a high prevalence of low HDL (90%). Also, 23% of our β-TM patients had hypertriglyceridemia, associated with their serum ferritin.
Prevalence of hypertension in β-TM patients was previously reported at 6.7% [36]. In our study, 4% of our β-TM patients had hypertension, which was close to the prevalence in the normal population [13]. However, heart rate variability was reduced in β-TM patients due to early autonomic neuropathy in their hearts [37]. Similar to our results, Tabatabaie et al. revealed that serum ferritin, hemoglobin, and transfusion intervals did not affect the abnormal changes in blood pressure [36].
Although there are several novelties in the present research, such as being the first to evaluate the metabolic syndrome prevalence in β-TM patients, it was also the first to evaluate the prevalence of abdominal obesity and hypertension in β-TM patients of southern Iran. However, there were some limitations. We did not check the fasting insulin level to estimate the Homeostatic Model Assessment (HOMA) index. We suggest considering the evaluation of the HOMA index in β-TM patients in future researches to find out a more accurate estimation of the metabolic syndrome in β-TM patients and its association with insulin resistance.
Conclusion
This study revealed that 22% of β-TM patients had IDF criteria of metabolic syndrome and low HDL was the most frequent positive criterion. Metabolic syndrome was more prevalent in female patients. Abdominal obesity and hypertriglyceridemia were associated with serum ferritin. Further studies should be performed to find the related factors, to reduce the cardiovascular morbidities associated with metabolic syndrome in β-TM patients.
References
Perera NJ, Lau NS, Mathews S, Waite C, Ho PJ, Caterson ID. Overview of endocrinopathies associated with beta-thalassaemia major. Intern Med J. 2010;40(10):689–96.
Borgna-Pignatti C, Cappellini MD, De Stefano P, Del Vecchio GC, Forni GL, Gamberini MR, et al. Survival and complications in thalassemia. Ann N Y Acad Sci. 2005;1054:40–7.
Haghpanah S, Nasirabadi S, Ghaffarpasand F, Karami R, Mahmoodi M, Parand S, et al. Quality of life among Iranian patients with beta-thalassemia major using the SF-36 questionnaire. Sao Paulo Med J. 2013;131(3):166–72.
Annaloro C, Airaghi L, Saporiti G, Onida F, Cortelezzi A, Deliliers GL. Metabolic syndrome in patients with hematological diseases. Expert Rev Hematol. 2012;5(4):439–58.
Najafipour F, Aliasgarzadeh A, Aghamohamadzadeh N, Bahrami A, Mobasri M, Niafar M, et al. A cross-sectional study of metabolic and endocrine complications in beta-thalassemia major. Ann Saudi Med. 2008;28(5):361–6.
Hafez M, Youssry I, El-Hamed FA, Ibrahim A. Abnormal glucose tolerance in beta-thalassemia: assessment of risk factors. Hemoglobin. 2009;33(2):101–8.
Pappas S, Donohue SM, Denver AE, Mohamed-Ali V, Goubet S, Yudkin JS. Glucose intolerance in thalassemia major is related to insulin resistance and hepatic dysfunction. Metab Clin Exp. 1996;45(5):652–7.
Karimi M, Marvasti VE, Motazedian S, Sharifian M. Is beta-thalassemia trait a protective factor against hypertension in young adults? Ann Hematol. 2006;85(1):29–31.
Khera R, Singh M, Goel G, Gupta P, Singh T, Dubey AP. Hypertriglyceridemia thalassemia syndrome: a report of 4 cases. Indian J Hematol Blood Transfus. 2014;30(Suppl 1):288–91.
Bordbar M, Haghpanah S, Afrasiabi A, Dehbozorgian J, Karimi M. Genotype-phenotype correlation related to lipid profile in beta-thalassemia major and intermedia in southern Iran. J Clin Lipidol. 2012;6(2):108–13.
Fung EB, Xu Y, Kwiatkowski JL, Vogiatzi MG, Neufeld E, Olivieri N, et al. Relationship between chronic transfusion therapy and body composition in subjects with thalassemia. J Pediatr. 2010;157(4):641–7. 7 e1–2
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–7.
Tabatabaie AH, Shafiekhani M, Nasihatkon AA, Rastani IH, Tabatabaie M, Borzoo AR, et al. Prevalence of metabolic syndrome in adult population in Shiraz, southern Iran. Diabetes Metab Syndr. 2015;9(3):153–6.
Alberti KG, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469–80.
Hajian-Tilaki K. Metabolic syndrome and its associated risk factors in Iranian adults: a systematic review. Caspian J Intern Med. 2015;6(2):51–61.
Maharlouei N, Bellissimo N, Ahmadi SM, Lankarani KB. Prevalence of metabolic syndrome in pre- and postmenopausal Iranian women. Climacteric. 2013;16(5):561–7.
Shahbazian H, Latifi SM, Jalali MT, Shahbazian H, Amani R, Nikhoo A, et al. Metabolic syndrome and its correlated factors in an urban population in South West of Iran. Journal of diabetes and metabolic disorders. 2013;12(1):11.
Mahjoub S, Haji Ahmadi M, Faramarzi M, Ghorbani H, Moazezi Z. The prevalence of metabolic syndrome according to the Iranian Committee of Obesity and ATP III criteria in Babol, North of Iran. Caspian J Int Med. 2012;3(2):410–6.
Saki F, Ashkani-Esfahani S, Karamizadeh Z. Investigation of the relationship between retinol binding protein 4, metabolic syndrome and insulin resistance in Iranian obese 5–17 year old children. Iran J Pediatr. 2013;23(4):396–402.
Saki F, Karamizadeh Z. Metabolic syndrome, insulin resistance and fatty liver in obese Iranian children. Iran Red Crescent Med J. 2014;16(5):e6656.
Gozashti MH, Hasanzadeh A, Mashrouteh M. Prevalence of metabolic syndrome in patients with minor beta thalassemia and its related factors: a cross-sectional study. J Diabetes Metab Disord. 2014;13(1):108.
Delvecchio M, Cavallo L. Growth and endocrine function in thalassemia major in childhood and adolescence. J Endocrinol Investig. 2010;33(1):61–8.
Sheu WH, Chen YT, Lee WJ, Wang CW, Lin LY. A relationship between serum ferritin and the insulin resistance syndrome is present in non-diabetic women but not in non-diabetic men. Clin Endocrinol. 2003;58(3):380–5.
Gonzalez AS, Guerrero DB, Soto MB, Diaz SP, Martinez-Olmos M, Vidal O. Metabolic syndrome, insulin resistance and the inflammation markers C-reactive protein and ferritin. Eur J Clin Nutr. 2006;60(6):802–9.
Kim CH, Kim HK, Bae SJ, Park JY, Lee KU. Association of elevated serum ferritin concentration with insulin resistance and impaired glucose metabolism in Korean men and women. Metab Clin Exp. 2011;60(3):414–20.
Kirim S, Keskek SO, Turhan A, Saler T. Is beta-thalassaemia minor associated with metabolic disorder? Med Princ Pract. 2014;23(5):421–5.
Azimi-Nezhad M, Herbeth B, Siest G, Dade S, Ndiaye NC, Esmaily H, et al. High prevalence of metabolic syndrome in Iran in comparison with France: what are the components that explain this? Metab Syndr Relat Disord. 2012;10(3):181–8.
Haghpanah S, Davani M, Samadi B, Ashrafi A, Karimi M. Serum lipid profiles in patients with beta-thalassemia major and intermedia in southern Iran. J Res Med Sci. 2010;15(3):150–4.
Madani H, Rahimi Z, Manavi-Shad M, Mozafari H, Akramipour R, Vaisi-Raygani A, et al. Plasma lipids and lipoproteins in children and young adults with major beta-thalassemia from western Iran: influence of genotype. Mol Biol Rep. 2011;38(4):2573–8.
Mansi KM, Aburjai TA. Lipid profile in Jordanian children with beta-thalassemia major. Uluslar hemato-onko. 2008;18(2):93–8.
Al-Quobaili FA, Abou Asali IE. Serum levels of lipids and lipoproteins in Syrian patients with beta-thalassemia major. Saudi Med J. 2004;25(7):871–5.
Dwivedi S, Kumar V. Beta-thalassemia, hyperlipoproteinemia(a), and metabolic syndrome: its low-cost holistic therapy. J Altern Complement Med. 2007;13(2):287–9.
Ricchi P, Ammirabile M, Spasiano A, Costantini S, Di Matola T, Cinque P, et al. Hypocholesterolemia in adult patients with thalassemia: a link with the severity of genotype in thalassemia intermedia patients. Eur J Haematol. 2009;82(3):219–22.
Hartman C, Tamary H, Tamir A, Shabad E, Levine C, Koren A, et al. Hypocholesterolemia in children and adolescents with beta-thalassemia intermedia. J Pediatr. 2002;141(4):543–7.
Papanastasiou DA, Siorokou T, Haliotis FA. Beta-Thalassaemia and factors affecting the metabolism of lipids and lipoproteins. Haematologia. 1996;27(3):143–53.
Tabatabaie M, Hooman N, Arjmandi-Rafsanjani K, Isa-Tafreshi R. Ambulatory blood pressure monitoring for children with beta-thalassemia major: a preliminary report. Iran J Kidney Dis. 2013;7(4):299–303.
Kardelen F, Tezcan G, Akcurin G, Ertug H, Yesilipek A. Heart rate variability in patients with thalassemia major. Pediatr Cardiol. 2008;29(5):935–9.
Acknowledgments
The authors wish to thank Mr. H. Argasi at the Research Consultation Center (RCC) of Shiraz University of Medical Sciences for his invaluable assistance in editing this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The study was approved by Shiraz University of Medical Sciences (SUMS) local Ethics Committee and vice-chancellor of research at SUMS. Written informed consent form was signed by all participants and their parents.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Saki, F., Bahadori, R., Kashkooli, N.M. et al. Prevalence of metabolic syndrome in beta thalassemia major adolescents in southern Iran: a cross-sectional study. Int J Diabetes Dev Ctries 39, 444–450 (2019). https://doi.org/10.1007/s13410-018-0663-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-018-0663-9