Abstract
To investigate the effectiveness of combined aerobic and resistance training (CT), we conducted this meta-analysis to directly compare the effect of CT with that of aerobic training (AT) alone on type 2 diabetic patients. We searched PUBMED, EMBASE, Cochrane Controlled Trials Register, and SPORT DISCUS (from the earliest date available to June 2013) for randomized controlled trials (RCTs) examining effects of CT versus AT in type 2 diabetic patients. Two reviewers selected studies independently. Seven studies met the study criteria (192 male patients, 240 female patients). We found that compared with AT, CT decreased HbA1c, abdominal adipose tissue, total cholesterol, and triglycerides. CT had similar effect on HDL cholesterol, LDL cholesterol, and blood pressure to AT alone. Study withdrawals were similar for AT and CT. No serious adverse events were reported. CT is more effective than AT and does not compromise study completion or safety when compared to AT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes is a group of metabolic disorders characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. The type 2 form of the disease, which is associated with obesity [1] and physical inactivity [2], is growing owing to the increasing prevalence of obesity and sedentary lifestyles.
Chronic hyperglycemia together with central obesity, dyslipidemia, hypertension, and insulin resistance is typical in the setting of the metabolic syndrome (MS) [3]. MS, with a prevalence of >80 % in type 2 diabetic patients, has caused 2–4-fold increase in cardiovascular disease (CVD) risk in diabetic versus nondiabetic subjects [4, 5]. CVD is the leading cause of mortality among individuals with diabetes [6, 7], accounting for 65 % of all deaths among this patient group [8].
Exercise is a cornerstone of diabetes management, along with dietary and pharmacological interventions [9, 10]. The majority of studies have been focused to examine the effect of aerobic training (AT) on type 2 diabetic patients, including indices of obesity, improved cardiovascular risk profile, and decrease of glycosylated hemoglobin (HbA1c) concentration [11, 12]. Thus, the guidelines for prescribing AT are widely known. Owing to the contribution of resistance training (RT) to fat mass loss [13], the addition of RT to AT may be of greater importance for type 2 diabetes, since obesity is the most important factor for the development of type 2 diabetes [14] and is associated with elevated cardiovascular risk [15]. However, very few studies have included a combined training (CT) approach, i.e., AT and RT, even in overweight populations, where the addition of RT may have its greatest impact [16]. Although some health association guidelines recommend that both aerobic and resistance training should be combined in the exercise prescription for type 2 diabetes [17] since some studies had found that combining both forms of exercise to achieve the same dose of exercise might lead to greater glycemic control benefits. However, the research results comparing the effects of CT versus AT on glucose control were not consistent, and the effects of CT versus AT on other risk factors for complications of diabetes were still controversial. Therefore, we performed this meta-analysis to examine randomized controlled trials (RCTs) that compared the effects of CT to AT alone on HbA1c and physiological parameters related to complications of diabetes, to investigate the effectiveness of CT.
Methods
Inclusion and exclusion criteria
Included in this review were studies that included men and women with type 2 diabetes older than 18 years. Only randomized controlled studies were included where at least one group received CT (defined as AT and RT) and one group received AT alone. Only English-language studies were included in the analysis. Exclusion criteria are as follows: (1) studies of patients with type 1 diabetes or gestational diabetes; (2) duplicate publications or substudies of included trials; and (3) studies with less than 12 weeks of follow-up.
Outcome measures
The chronic hyperglycemia that characterizes type 2 diabetes is related to a significant long-term sequelae, including damage to and eventual failure of various organs (macrovascular), and directly related to the likelihood of developing microvascular complications [7]. Therefore, our primary outcome measure was HbA1c, which is considered the gold standard for measuring long-term glycemic control. Our secondary outcomes included abdominal fat mass, blood lipids (HDL cholesterol, LDL cholesterol, total cholesterol, and triglycerides), and blood pressure (systolic and diastolic).
Search strategy
The following electronic databases were searched from the earliest date available to June 2013: PUBMED, EMBASE, Cochrane Controlled Trials Register, and SPORT DISCUS. Also, reference lists of retrieved articles were examined for further studies. Search terms included exercise therapy, exercise movement techniques, exercise, physical exercise, kinesiotherapy, resistance training, muscle stretching exercises, physical exertion, strength training, muscle strengthening, aerobic exercise, type 2 diabetes, ketosis-resistant diabetes, maturity-onset diabetes, noninsulin-dependent diabetes, stable diabetes, maturity-onset diabetes of the young (MODY), noninsulin-dependent diabetes mellitus (NIDDM), and adult-onset diabetes mellitus.
Data extraction
Titles and abstracts of retrieved articles were independently evaluated by two investigators (YH and XW). Reviewers were not blinded to authors, institutions, or manuscript journals. Abstracts that did not provide enough information regarding the inclusion and exclusion criteria were retrieved for full-text evaluation. Reviewers independently evaluated full-text articles and determined study eligibility.
Disagreements were solved by consensus, and if disagreement persisted, by a third reviewer (WL). A standardized data extraction form was used and two reviewers (YH and XW) independently conducted data extraction. Disagreements were solved by consensus or by a third reviewer (WL).
Assessment of risk of bias
Risk of bias was assessed according to the PEDro rating scale and the Jadad scale (maximum score of 10 and 5, respectively, with the higher score reflecting greater methodological quality). The two scales are all used to assess the risk of bias in clinical trials. Among them, the PEDro rating scale is more suitable for physical intervention, but it does not assess withdraws and dropouts, as well as the Jadad scale. For that reason, we used both scales to obtain more information of studies included. The PEDro rating scale is designed to evaluate adequacy of random allocation, concealed allocation, similarity of groups at baseline, blinding of the participants, therapist and/or assessor, measures of at least one key outcome from more than 85 % of the subjects initially allocated to groups, intention-to-treat analysis, between-group analysis, and point estimates and variability [18]. The Jadad scale is designed to determine adequacy of randomization, double-blinding, and description of withdrawals and dropouts [19]. Quality assessment was independently performed by two unblinded reviewers (YH and XW), and disagreements were solved by consensus or by a third reviewer (WL).
Data synthesis and analysis
Data were analyzed by Review Manager Analysis software version 5.1 (The Cochrane Collaboration, Oxford, England). The outcome measure was the weighted mean difference (WMD) or standardized mean difference (SMD). When the standard deviation of the mean difference for each group was not available, it was reconstructed from the actual p value or confidence interval for difference in means between groups or by imputing from the standard deviations observed in other studies of similar methodology [20].
A random effects model was used when the Q statistic for heterogeneity was significant at the level of 0.1; otherwise, the fixed effects model was used. The degree of heterogeneity was quantified using the I 2 statistic, which is the percentage of total variation across studies due to heterogeneity.
Results
Description of studies
Study selection
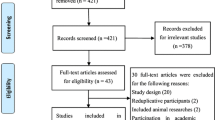
From 3854 potentially relevant citations retrieved from electronic databases and searches of reference lists, seven RCTs met the inclusion criteria [21–27]. A flow diagram of search and selection is shown in Fig. 1.
Study characteristics
The characteristics of the included studies are presented in Table 1. Included studies had a total of 432 patients. Of these, most were female (56 %).The duration of the exercise interventions ranged from 12 to 52 weeks. The AT groups were prescribed 135–225 min of AT per week, at an intensity of 50–85 % of peak heart rate. The CT groups were prescribed 75–135 min of AT per week at 50–85 % of peak heart rate. The RT prescription consisted of two to three sets, of four to nine exercises at an intensity of 50–100 % of the one repetition maximum (1RM: heaviest weight lifted once), three to four times/week. Except one study by Sigal et al. [27], most studies attempted to equalize the total activity exposure/dose between treatment groups by reducing the AT time in the CT group [21, 22, 24, 26] or replacing AT sessions with the same number of RT sessions in the CT group [23, 25].
All of the included articles reported data on dropouts of less than 20 %. Of these, six studies reported data on adherence rates of more than 80 % [21, 23–27].
Six studies reported data on adverse events [21, 22, 24–27]. No major adverse effects occurred (Table 2). Minor adverse events most commonly included cardiovascular disease events that were not deemed to be related to the intervention and musculoskeletal injury or discomfort.
Risk of bias in included studies
Among the seven included studies, only two adequately concealed allocation (Table 3) and no study was double-blind. Therefore, the highest score on the Jadad scale was three of five [21, 22, 25, 27] and eight of ten on the PEDro scale [27].
Effects of exercise
HbA1c
The pooled analysis revealed a trend for CT, to have a more favorable effect on absolute changes in HbA1c (WMD, −0.31 %; 95 % CI, −0.38, −0.25; χ 2 = 6.74, p < 0.00001, I 2 = 11 %) when compared to AT (Fig. 2).
Abdominal fat
Change in abdominal adipose tissue as measured by computed tomography was reported in two studies. In the pooled analysis, subcutaneous adipose tissue showed a WMD of −10.17 cm2 in favor of CT when compared to AT (95 % CI −17.67, −2.67; χ 2 = 0.04, p = 0.008, I 2 = 0 %) (Fig. 3a), and visceral adipose tissue showed a WMD of −12.69 cm2 in favor of CT when compared to AT (95 % CI −24.52, −0.86; χ 2 = 0.49, p = 0.04, I 2 = 0 %) (Fig. 3b).
Blood lipids
Five studies reported the changes of HDL cholesterol, total cholesterol, and triglycerides. Four studies reported the changes of LDL cholesterol. The pooled analysis revealed that there was a decrease in total cholesterol and triglycerides for CT than for AT alone. The WMD is −10.36 mg/dL (95 % CI −15.89, −4.84; χ 2 = 19.83, p = 0.0002, I 2 = 80 %) (Fig. 4c) and −9.25 mg/dL (95 % CI −13.61, −4.90; χ 2 = 0.44, p < 0.0001, I 2 = 0 %) (Fig. 4d), respectively. The difference of effects for CT versus AT on HDL cholesterol and LDL cholesterol were not found. The WMD is 1.18 mg/dL (95 % CI −0.48, 2.84; χ 2 = 15.58, p = 0.16, I 2 = 74 %) (Fig. 4a) and −2.18 mg/dL (95 % CI −7.49, 3.13; χ 2 = 18.11, p = 0.42, I 2 = 83 %) (Fig. 4b), respectively.
Blood pressure
Change of blood pressure was reported in three studies. In the pooled analysis, CT did not show favorable effect when compared to AT. The WMD for systolic blood pressure is 0.62 mmHg (95 % CI −0.74, 1.98; χ 2 = 5.65, p = 0.37, I 2 = 65 %) (Fig. 5a), and the WMD for diastolic blood pressure is 0.82 mmHg (95 % CI −2.05, 3.69; χ 2 = 15.96, p = 0.57, I 2 = 87 %) (Fig. 5b).
Sensitivity analysis
The PEDro rating scale has more items and higher total score than the Jadad scale. Among studies of which score on Jadad scale was 2/5, the score on PEDro rating scale might be 4/10 or 5/10. We removed low quality studies with score <5 on the PEDro rating scale for sensitivity analysis according to a meta-analysis by Marzolini S et al. [28] who also used both of the two scales. There was no difference in the significance of the treatment effects when low-quality studies were removed from all of the planned analyses except LDL cholesterol.
Discussion
To our knowledge, this is the first published meta-analysis directly comparing the effect of AT alone with CT in patients with type 2 diabetes. Collectively, the evidence suggests that CT is more effective than AT alone on glucose control and some related risk factors for complications of diabetes. The proportion of patients who discontinued the studies was similar in both treatment groups. No serious adverse events related to AT or RT components were reported.
There was a significant change in favor of CT when compared to AT in HbA1c. A possible explanation for this can be found in the fact that training can decrease the intramyocytic lipid concentration and increase the fatty acid oxidation capacity [29]. More muscles (upper and lower limbs) were exercised in the combined training than in the aerobic training (only lower limb). Because larger muscle mass was involved in the combined training, it is possible that the total intramyocytic fat content decreases and/or that the fatty acid oxidation capacity increases more through combined than aerobic training, leading to an increased glucose uptake after combined training [29]. An absolute decrease of 1 % in HbA1c levels has been associated with a 25 % decrease in major cardiovascular disease events and a 29 % decrease in microvascular complications [30]. Thus, the observed relative reduction of −0.31 % HbA1c levels caused by CT compared to AT might be expected to produce an 8 % reduction in cardiovascular disease risk and a 9 % reduction in risk of microvascular complications. Such a reduction would be small, but considering the favorable effects of CT on the other diabetic complication risk factors, we can conclude that CT should be a priority.
CT confers a superiority of decreasing abdominal fat compared with AT. Despite the small number of trials, the credibility of this analysis is supported by the confirmed reliability and validity of abdominal fat measures using CT scans. The abdominal fat loss that favored the CT training strategy is of significance because excess abdominal fat is associated with plasma glucose, excess blood lipid levels, high blood pressure, CAD, and stroke [31–33]. While AT is an important factor in the development of sustained negative energy balance, the volume of activity necessary to induce significant fat loss is reported to be greater than 1 h per session on a daily basis over a long period of time [34]. Due to the high level of activity and time required and such physical limitations as musculoskeletal comorbidities, peripheral vascular disease, and diabetic neuropathy, many patients may not be able to adhere to such a high volume of AT necessary for fat mass loss. However, replacing high impact AT sessions with RT sessions may reduce joint and peripheral limb stress while being at a volume that most diabetic patients can reasonably tolerate. In addition, it has been proved that RT could improve pain and disability associated with arthritis of the knee [35].
Pooled analysis resulted in a trend for the CT group when compared to the AT group to decrease total cholesterol and triglycerides by −10.36 and −9.25 mg/dL, respectively. As mentioned above, a possible explanation may be that compared with the aerobic group, a larger muscle mass was included in combination training, possibly bringing about a greater decrease of intramyocytic fat content and/or a greater increase of fatty acid oxidation capacity [29]. These favorable effects may have been responsible for an increased clearance of lipids from the blood. The result of pooled analyses on LDL cholesterol changed when low-quality study was removed. More studies should be included to assess the effect of combined training versus aerobic training alone on LDL.
Although resistance training alone or high-intensity resistance training is reported to potentially increase arterial stiffness of type 2 diabetic patients with a raise in blood pressure [36, 37], this meta-analysis showed that the addition of appropriate resistance training to aerobic training had similar effect on blood pressure to AT alone.
Study limitations
One limitation of this analysis was the small number of randomized controlled studies. Other limitations were the restriction to English language publications, small sample size of some studies, reliance on imputing some of the missing standard deviations of the change in means, and inclusion of studies that did not include adequate allocation concealment or blinded outcome assessors. Due to the small sample size, we were unable to assess reporting bias.
Conclusions
Results suggest that CT is more effective than AT alone in affecting change in HbA1c, abdominal fat, and blood lipids. Compared to AT, CT does not appear to compromise study completion or pose significant hazards in diabetic patients. More studies with strong methodological design and large sample size are required to further evaluate the benefits of CT versus AT.
References
Tentolouris N, Andrianakos A, Karanikolas G, Karamitsos D, Trontzas P, Krachtis P, et al. Type 2 diabetes mellitus is associated with obesity, smoking and low socioeconomic status in large and representative samples of rural, urban, and suburban adult Greek populations. Hormones (Athens). 2012;11:458–67.
Admiraal WM, van Valkengoed IG, L de munter JS, Stronks K, Hoekstra JB, Holleman F. The association of physical inactivity with type 2 diabetes among different ethnic groups. Diabet Med. 2011;28:668–72.
Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome-a new worldwide definition. Lancet. 2005;366:1059–62.
Kronmal RA, Barzilay JI, Smith NL, Psaty BM, Kuller LH, Burke GL, et al. Mortality in pharmacologically treated older adults with diabetes: the cardiovascular health study, 1989–2001. PLoS Med. 2006;3:e400.
Jackson CA, Jones NR, Walker JJ, Fischbacher CM, Colhoun HM, Leese GP, et al. Area-based socioeconomic status, type 2 diabetes and cardiovascular mortality in Scotland. Diabetologia. 2012;55:2938–45.
Bhattacharyya OK, Shah BR, Booth GL. Management of cardiovascular disease in patients with diabetes: the 2008 Canadian Diabetes Association guidelines. CMAJ. 2008;179:920–6.
CDA. Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2008;32:S1–S15.
Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2005. Atlanta: Centers for Disease Control and Prevention; 2005.
ADA. Standards of medical care in diabetes—2011. Diabetes Care. 2011;34:S11–61.
Colberg SR, Sigal RJ, Fernhall B, American College of Sports Medicine; American Diabetes Association, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):2692–6.
Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA. 2001;286:1218–27.
Pi-Sunyer X, Blackburn G, Brancati FL, Bray GA, Bright R, Clark JM, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look ahead trial. Diabetes Care. 2007;30:1374–83.
Pratley R, Nicklas B, Rubin M, Miller J, Smith A, Smith M, et al. Strength training increases resting metabolic rate and norepinephrine levels in healthy 50- to 65-year-old men. J Appl Physiol. 1994;76:133–7.
Rorive M, Letiexhe MR, Scheen AJ, Ziegler O. Obesity and type 2 diabetes. Rev Med Liege. 2005;60:374–82.
Liu A, Abbasi F, Reaven GM. Adiposity indices in the prediction of metabolic abnormalities associated with cardiovascular disease in non-diabetic adults. Nutr Metab Cardiovasc Dis. 2011;21:553–60.
Umpierre D, Ribeiro PA, Kramer CK, Leitão CB, Zucatti AT, Azevedo MJ, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2011;305:1790–9.
Hordern MD, Dunstan DW, Prins JB, Baker MK, Singh MA, Coombes JS. Exercise prescription for patients with type 2 diabetes and pre-diabetes: a position statement from Exercise and Sport Science Australia. J Sci Med Sport. 2012;15:25–31.
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–21.
Jadad A, Moore R, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports or randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12.
Higgins JPT, Deeks JJ. Selecting studies and collecting data. In: Higgins JPT, Green SJ, editors. Cochrane handbook for systematic reviews of interventions. Chichester: The Cochrane Collaboration; 2008. p. 174–5.
Balducci S, Zanuso S, Nicolucci A, Fernando F, Cavallo S, Cardelli P, et al. Anti-inflammatory effect of exercise training in subjects with type 2 diabetes and the metabolic syndrome is dependent on exercise modalities and independent of weight loss. Nutr Metab Cardiovasc Dis. 2010;20:608–17.
Church TS, Blair SN, Cocreham S, Johannsen N, Johnson W, Kramer K, et al. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2010;304:2253–62.
Cuff DJ, Meneilly GS, Martin A, Ignaszewski A, Tildesley HD, Frohlich JJ. Effective exercise modality to reduce insulin resistance in women with type 2 diabetes. Diabetes Care. 2003;26:2977–82.
Kadoglou NP, Fotiadis G, Kapelouzou A, Kostakis A, Liapis CD, Vrabas IS. The differential anti-inflammatory effects of exercise modalities and their association with early carotid atherosclerosis progression in patients with type 2 diabetes. Diabet Med. 2013;30:e41–50.
Lambers S, Van Laethem C, Van Acker K, Calders P. Influence of combined exercise training on indices of obesity, diabetes and cardiovascular risk in type 2 diabetes patients. Clin Rehabil. 2008;22:483–92.
Oliveira VN, Bessa A, Jorge ML, Oliveira RJ, De Mello MT, de Agostini GG, et al. The effect of different training programs on antioxidant status, oxidative stress, and metabolic control in type 2 diabetes. Appl Physiol Nutr Metab. 2012;37:334–44.
Sigal RJ, Kenny GP, Boulé NG, Wells GA, Prud'homme D, Fortier M, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med. 2007;147:357–69.
Marzolini S, Oh PI, Brooks D. Effect of combined aerobic and resistance training versus aerobic training alone in individuals with coronary artery disease: a meta-analysis. Eur J Prev Cardiol. 2011;19:81–94.
Shaw CS, Shepherd SO, Wagenmakers AJ, Hansen D, Dendale P, van Loon LJ. Prolonged exercise training increases intramuscular lipid content and perilipin 2 expression in type I muscle fibers of patients with type 2 diabetes. Am J Physiol Endocrinol Metab. 2012;303:e1158–65.
Zhang Y, Hu G, Yuan Z, Chen L. Glycosylated hemoglobin in relationship to cardiovascular outcomes and death in patients with type 2 diabetes: a systematic review and meta-analysis. PLoS One. 2012;7:e42551.
Liu J, Fox CS, Hickson DA, May WD, Hairston KG, Carr JJ, et al. Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson Heart Study. J Clin Endocrinol Metab. 2010;95:5419–26.
Toss F, Wiklund P, Franks PW, Eriksson M, Gustafson Y, Hallmans G, et al. Abdominal fat and gynoid adiposity and the risk of stroke. Int J Obes (Lond). 2011;35:1427–32.
Hamagawa K, Matsumura Y, Kubo T, Hayato K, Okawa M, Tanioka K, et al. Abdominal visceral fat thickness measured by ultrasonography predicts the presence and severity of coronary artery disease. Ultrasound Med Biol. 2010;36:1769–75.
Bouchard C, Depres JP, Tremblay A. Exercise and obesity. Obes Res. 1993;1:133–47.
Ettinger WHJ, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: the fitness arthritis and seniors trial (fast). JAMA. 1997;277:25–31.
Kawano H, Tanaka H, Miyachi M. Resistance training and arterial compliance: keeping the benefits while minimizing the stiffening. J Hypertens. 2006;24:1753–9.
Ozaki H, Yasuda T, Ogasawara R, Sakamaki-Sunaga M, Naito H, Abe T. Effects of high-intensity and blood flow-restricted low-intensity resistance training on carotid arterial compliance: role of blood pressure during training sessions. Eur J Appl Physiol. 2013;113:167–74.
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Hou, Y., Lin, L., Li, W. et al. Effect of combined training versus aerobic training alone on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Int J Diabetes Dev Ctries 35, 524–532 (2015). https://doi.org/10.1007/s13410-015-0329-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-015-0329-9