Abstract
Background
Epigenetic processes and miRNAs have been recognized as new targets for anticancer drug design. However, old multi-target drugs such as aspirin may also target epigenetic processes.
Aim
This review aims to provide an overview of our current knowledge on the modulation of epigenetic processes by aspirin and other non steroidal anti-inflammatory agents (NSAIDs) and their implications for cancer treatment and chemoprevention.
Synthesis
In vitro and in vivo studies, as well as primary patient data, suggest that aspirin and other NSAIDs reverse tumour suppressor gene hypermethylation in cancer tissues. It must be emphasized that, at this point in time, patient data are limited and DNA hypermethylation reversal has been investigated, but not tumour suppressor gene activation. In addition, evidence from experimental and patient data suggests that aspirin and NSAIDs may also reverse global DNA hypomethylation. At the histone level, both induction and inhibition of deacetylases by aspirin have been reported. Also, direct acetylation of histones by aspirin has been reported, while the natural salicylate anacardic acid has been found to inhibit histone acetyltransferase p300 both in vitro and in vivo, and to regulate gene expression through modulation of histone acetylation. Salicylates and other NSAIDs may also down-regulate miRNAs with oncogene-like functions or up-regulate miRNAs with tumour suppressor-like functions. Up till now, clinical trials have been aimed at investigating the effect of salicylates and NSAIDs on a limited number of miRNAs.
Conclusion
So, although the existing evidence is still limited, evidence is accumulating that epigenetic targets may represent nodal targets for the anti-proliferative actions of salicylates and NSAIDs. This, in turn, may have implications for cancer chemoprevention and treatment. Undoubtedly, this notion requires further investigation, but if proved correct, it could lead to the design of less toxic agents that target epigenetic processes as part of existing or novel multi-targeted treatment modalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
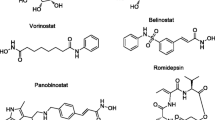
The term epigenetics refers to heritable traits in cells and organisms that do not involve changes in the underlying DNA sequence, i.e., that result in changes in gene expression commonly caused by environmental factors [1] These changes may persist through cell division and for the remainder of the organism’s life. Epigenetic processes include gene promoter hypermethylation, global DNA hypomethylation, histone acetylation, phosphorylation, ubiquitylation and sumolyation, and nucleosome remodelling [2]. The net effect of these processes is activation or silencing of genes. Modulation of expression of key genes by epigenetic processes can lead to the initiation, progression or maintenance of carcinogenesis, and even to drug resistance. On the other hand, microRNAs may regulate protein expression of specific genes, either by inhibiting mRNA translation through binding to their 3΄ untranslated regions, or by destabilizing target mRNAs [3–5]. Thus, up-regulation of a miRNA is expected to enhance the silencing of its target mRNAs, while miRNA down-regulation is expected to result in up-regulation of its target mRNAs. However, this is not a one-to-one relationship. Several miRNAs may bind to one mRNA and co-operate to silence gene expression. Conversely, a single miRNA may affect several mRNAs [6–8]. Epigenetic and miRNA functions are highly interconnected, since miRNA genes themselves can be epigenetically regulated and miRNAs can repress key enzymes that drive epigenetic remodelling [9]. Based on the evolving knowledge, epigenetic processes and miRNAs have been recognized as new targets for anticancer drug design [2, 10]. Currently, several epigenetic drugs are under evaluation in pre-clinical and clinical trials, or have already been FDA approved. They can be classified into two groups, those inhibiting DNA methyltransferases (DNMT) and those inhibiting histone deacetyltransferases (HDAC). It has been recognized, however, that both DNMT and HDAC inhibitors may activate oncogenes due to lack of specificity, resulting in accelerated tumour progression [11]. In addition, epigenetic states, once corrected, may revert to the original state due to the reversible nature of specifically DNA methylation patterns. In addition, currently approved epigenetic agents are known to be associated with significant toxicities. Therefore, there is a need for more specific and safer drugs. Despite hundreds of clinical trials for anti-cancer drugs that are currently in progress, most of these trials fail to pass Phase I. Previously developed drugs with novel anti-tumour properties, however, offer a viable and cost-effective alternative, since these drugs have known pharmacokinetic and safety profiles [12]. Furthermore, silencing of tumour suppressor genes has been recognized as an important (early) step in carcinogenesis. Reversal of this process by epigenetic drugs could serve as an effective chemotherapeutic strategy for patients with multiple tumour suppressor gene hypermethylations [13]. Aspirin and other non steroidal anti-inflammatory agents (NSAIDs), i.e., old drugs currently being investigated for identifying novel targets for their action, would be good candidates for such an approach. Epidemiological studies have shown that regular use of NSAIDs reduces the risk of the development of at least some cancers [14, 15]. So far, however, the mechanisms underlying the anti-tumour activities of NSAIDs remain to be elucidated. Known targets for aspirin and other NSAIDs include COX-I and COX-II, pathways regulating cell cycle, apoptosis, cell differentiation, cell response, proteasome and redox-mediated signaling, transcription factors such as NF-κΒ and the estrogen receptor, tumor suppressor genes such as p53, growth factors such as VEGF-A, VEGF-C and VEGF-D, and intracellular regulatory enzymes [16, 17]. Epigenetic processes may also define novel targets for aspirin and other NSAIDs. So, investigation of the effect of aspirin and other NSAIDs on epigenetic targets is expected to reveal novel insights into the mechanisms underlying the anticancer activities of these agents, and into appropriate dosage regimen and duration of treatment when used as epigenetic modulators in cancer treatment and chemoprevention. In the field of cancer therapeutics, nucleoside inhibitors of DNA methylation, i.e., azacitidine and decitabine, now part of standard care for the treatment of patients with myelodysplastic syndrome (MDS), provide good examples of old, and even abandoned, drugs that have taken a novel role in cancer therapy. This review aims to investigate epigenetic processes as novel putative targets for aspirin and NSAIDs, and to gain insights into the clinical implications of these novel targets for cancer treatment and chemoprevention.
2 Targeting DNA methylation
Silencing of the expression of gatekeeper or mismatch repair genes promotes growth in the affected cells. Classical knowledge stipulates that mutation or deletion of coding regions is responsible for gene inactivation. However, more recently alternatives have been defined, of which DNA promoter methylation represents an important mechanism for the induction of gene silencing. Methylation of tumour suppressor genes is thought to be an early event in carcinogenesis [18]. The CpG island methylator phenotype is characterized by hypermethylation of the promoters of several tumour suppressor genes and is associated with the inactivation of various pathways involved in tumourigenesis [19]. This methylator phenotype has amply been documented in e.g. gastric cancer tissues, precancerous lesions, Helicobacter pylori infected non neoplastic mucosa and in colon adenomatous polyps. DNA methylation is brought about by DNA methyltransferases (DNMT). The human genome harbours four genes that encode DNMTs (DNMT1, DNMT2, DNMT3A and DNMT3B) with DNMT1 and DNMT3B being the more potent ones [20].
Evidence is now emerging suggesting that salicylates, i.e., aspirin and other NSAIDs, can modulate DNA methylation (Table 1 and 2). Recent data obtained from molecular modelling studies have shown that the salicylates 5,5-methylenedisalicylic acid and trimethylaurintricarboxylic acid (NSC97317) can inhibit DNMT1 [21, 22]. Specifically, Kuck et al. [21] conducted a virtual screening of more than 65,000 lead-like compounds selected from the National Cancer Institute collection using a multistep docking approach with a previously validated homology model of the catalytic domain of human DNMT1. Experimental evaluation of top-ranked molecules led to the discovery of novel small molecule DNMT1 inhibitors. The virtual screening hits were further evaluated for DNMT3B inhibition, revealing several compounds with selectivity towards DNMT1. Among those, 5,5-methylenedisalicylic acid was found to have detectable, although weak, inhibitory effect on DNMT1 in biochemical assays. Yoo et al. [22] investigated trimethylaurintricarboxylic acid (NSC97317), a compound structurally related to 5,5-methylenedisalicylic acid, and found a low micromolar inhibitory effect on DNMT1 (IC(50) = 4.79 μM). Docking studies of the new inhibitor with the catalytic domain of DNMT1 suggested that NSC97317 can bind to the catalytic site. However, the impact of the above studies is as yet limited, since the biological relevance of the findings has not been evaluated.
Experimental data indicate that NSAIDs may induce promoter demethylation and reactivate the expression of some metastasis-related suppressor genes in lung cancer cells, implying that NSAIDs may serve as a resource for the development of a new class of demethylating agents [23]. Pan et al. first demonstrated that NS398, a NSAID, can inhibit lung cancer cell invasion through the up-regulation of a number of genes, including the secreted protein acidic and rich in cysteine (SPARC) gene. In addition, these investigators demonstrated that up-regulation of SPARC expression by NS398 in human lung cancer cells was mediated by promoter demethylation. In the same study, sulindac sulphide and indomethacin were also found to reduce promoter methylation. This demethylation was associated with a decrease in DNA methyltransferase expression. Based on their results, the authors suggested that NSAIDs induce promoter demethylation by repressing DNMT expression. [23]. However, equating inhibition of DNA methyltransferase activity and actual hypomethylation induction may not be that straightforward. DNA methyltransferase activity is proliferation dependent and cell cycle regulated. Thus, any insult that leads to proliferation arrest may also lead to a measurable decrease in DNA methyltransferase activity, but in this setting decreased activity has not been conclusively shown to affect methylation [11].
In agreement with experimental data, an epidemiological study has shown that chronic aspirin use may be associated with a lower prevalence of E-cadherin (CDH1) promoter methylation in non-neoplastic gastric mucosa [24]. E-cadherin is a cell adhesion molecule that is involved in tumour invasion/metastasis. In addition, it is thought to act as a tumour suppressor. E-cadherin can indeed be silenced epigenetically, i.e., silencing of the CDH1 gene by promoter CpG island methylation has been observed in precancerous lesions, Helicobacter pylori-infected chronic gastritis and gastric cancer. Tahara et al. [24] assessed the CDH1 methylation status in noncancerous gastric mucosa in chronic aspirin users. To this end, gastric mucosa samples were obtained from 217 cancer–free subjects, including 37 chronic aspirin users and 180 subjects with no history of chronic or occasional intake of aspirin. Methylation–specific polymerase chain reaction (MSP) was performed and CDH1 gene promoter methylation was detected in 69 subjects (31.7 %). Chronic aspirin use was found to be associated with a significantly lower rate of CDH1 methylation [nonuser versus user 36.1 % versus 10.8 %; odds ratio (OR) = 0.21, 95 % confidence interval (CI) = 0.07–0.63, P = 0.005]. From their results, the authors concluded that aspirin may have a suppressive effect on methylation-related gastric carcinogenesis [24]. The same group of investigators has shown that chronic NSAID use suppresses the CpG island methylation phenotype of the p14(ARF), p16(INK4a), death-associated protein kinase (DAPK) and CDH1 tumour suppressor genes in human gastric mucosa [25].
In contrast with the two previous studies, two other epidemiological studies on rectal and colon cancer [26, 27] have failed to show any association between aspirin and/or NSAID use and the CpG island methylator phenotype. However, it must be emphasized that these studies were aimed at investigating the effect of a number of factors on the CpG island methylator phenotype, with aspirin or NSAID use being one of them. In addition, in the study on rectal cancer [26] a low number of patients with CpG island methylator phenotype was included, resulting in a low power for the detection of an association between chronic aspirin/NSAID use and the CpG island methylator phenotype. In the latter study, Slattery et al. investigated associations between inflammation and specific tumour markers, including the association between regular aspirin or NSAID use and the CpG island methylator phenotype. A total of 1,505 rectal cancer patients was identified, of which 982 were reviewed. Specimens obtained through preoperative biopsies or paraffin embedded tissues from the resections were retrieved. Information on regular aspirin or NSAID use was obtained through appropriate questionnaires. Regular use was defined as use of at least 3 times a week for one month. No association was found between aspirin or NSAID use and the CpG island methylator phenotype, but the investigators pointed out that the measures of association were imprecise because of the limited number of CpG island methylation positive tumours [26]. In another study, Slattery et al. [27] used data from a population-based case control study to evaluate whether diet and lifestyle factors are associated with the CpG island methylator phenotype. Regular use of aspirin or NSAIDs was one of the factors included. Eligibility criteria for the cases included diagnosis with first-primary incident colon cancer between October 1, 1991 and September 30, 1994, between 30 and 79 years of age at the time of diagnosis and mentally competent to complete the interview. In addition to the eligibility criteria for the cases, at the time of recruitment the controls had no previous history of colorectal cancer. The CpG island methylator phenotype was assessed for the following markers: MINT1, MINT2, MINT31, p16 and hMLH1. The criterion for CpG island methylator phenotype (CIMP)-high was methylation of the CpG islands of two or more of these markers. CIMP-low was defined as zero or one of the five markers methylated. By doing so, the NSAIDs evaluated were found to be inversely associated with both CIMP-low and CIMP-high tumours [27]. Thus, also this study failed to reveal a specific association of aspirin/NSAID use with a high CpG methylator phenotype. Some of the parameters included in the study design, however, such as markers selected for DNA methylation assessment and the classification of CpG island methylator phenotypes, may have affected the outcome.
To the best of our knowledge, only one trial has included the possible modulation of DNA methylation by aspirin and NSAIDs as a tertiary outcome. The Chemoprevention for Barrett’s Esophagus Trial (CBET) was a phase IIb multi-centre randomized placebo-controlled trial of celecoxib in patients with Barrett’s esophagus and low- or high-grade dysplasia [28]. Patients were randomly assigned to treatment with 200 mg of celecoxib or placebo, both administered orally twice daily. The primary outcome was the change from baseline to 48 weeks of treatment in the proportion of biopsy samples with dysplasia between the celecoxib and placebo arms. It was found that celecoxib did not prevent the progression of Barrett’s dysplasia to cancer. Reversal in promoter methylation of the tumour suppressor genes p16, APC and CDH1 was one of the tertiary outcomes [28]. Paired baseline and post-treatment samples were available from 22 patients for comparison with methylation of all three genes. Among the 10 celecoxib-treated patients, six showed no change in methylation of any of the three genes examined, two had a gain in methylation in one gene, and two had a loss of methylation in one gene. Among the 12 placebo-treated patients, six showed no change in the methylation in any gene, three had a gain in methylation in one gene, and another three had a loss of methylation in one gene. Thus, no net change in methylation was observed in either the celecoxib or the placebo arms [28].
In another study, DNA methylation data were collected as part of a randomized double blind, placebo-controlled trial testing the efficacy of aspirin, folic acid, or both in the prevention of colorectal adenomas [29]. Eligible individuals met at least one of the following criteria: one or more histologically-confirmed adenoma removed within 3 months prior to recruitment, one or more histologically-confirmed adenoma removed within 16 months prior to recruitment and a lifetime history of two or more histologically-confirmed adenomas, or a histologically-confirmed adenoma at least 1 cm in diameter removed within 16 months prior to recruitment. The study had a three-by-two factorial design, comparing 81 mg and 325 mg of aspirin per day with placebo and comparing 1 mg of folic acid per day with placebo. The investigators examined the association between aspirin, folate and other dietary and lifestyle factors with CpG island methylation of the ERα and SFRP1 genes in both the right colon and the rectum. Three hundred eighty-eight subjects were included in the methylation analyses out of the 1,121 subjects participating in the parent study. It was found that aspirin was not statistically significantly associated with ER-α or SFRP1 methylation. However, subjects assigned to the aspirin treatment exhibited a slightly lower ERα methylation status in the right colon compared to the placebo, implying a possible protective role of aspirin against promoter DNA methylation [29]. However, this study may not be really informative since (i) it was based on a convenience sample of specimens and (ii) there was a low intra-class correlation between biopsies in a given individual.
3 Targeting global hypomethylation
Global DNA hypomethylation is an early event in the neoplastic progression of most human and animal cancers, including colon cancer [30]. Animal data have indicated that a 7 day treatment with NSAIDs, i.e., piroxicam, sulindac and celecoxib, reverses global DNA hypomethylation in azoxymethane-induced colon tumors in male F344 rats [31, 32]. Tao et al. [31] investigated DNA hypomethylation in colon cancer as a surrogate end-point biomarker for the evaluation of the efficacy of chemopreventive agents. Agents that were either effective or ineffective in preventing colon cancer were evaluated for their ability to modulate DNA hypomethylation in azoxymethane-induced colon tumours in male F344 rats. DNA methylation was determined using a mouse monoclonal anti-5-methylcytosine antibody. Colon tumours were found to exhibit a 70 % reduction in DNA methylation relative to normal colonic mucosa. DNA methylation in the tumours was found to be increased after 7 days of treatment with agents that have previously been shown to prevent colon cancer (i.e., calcium chloride, alpha-diflouromethylornithine [DFMO], piroxicam and sulindac), whereas agents previously shown not to prevent colon cancer in rats (low dose aspirin, 2-carboxyphenyl retinamide [2-CPR], quercetin, 9-cis retinoic acid and rutin) did not increase DNA methylation [31]. In the same experimental model, Pereira et al. [32], investigated the ability of celecoxib and alpha-difluoromethylornithine (DFMO) to modulate DNA hypomethylation. Celecoxib (500 mg/kg), DFMO (100, 1,000 and 3,000 mg/kg) or celecoxib + 1,000 mg/kg DFMO were administered for 7 or 28 days prior to sacrifice at week 37. Treatment with celecoxib or DFMO for 7 days was found to reverse the DNA hypomethylation level. Both celecoxib and 1,000 mg/kg DFMO were more effective in reversing DNA hypomethylation after 28 days of treatment than after 7 days, and after 28 days of treatment the level of DNA methylation in the tumours was no longer different from that in normal mucosa. Although the mechanism by which NSAIDs reverse global DNA hypomethylation has not been elucidated yet, increase in the activity of DNMT and/or increase in the level of the methyl donor, S-adenosyl methionine (SAM), have been proposed. In the same experimental model, it was found that celecoxib reversed the hypermethylation of the ER-α gene, probably through reduction of histone acetylation [32].
Shen et al. [33] investigated whether celecoxib could reverse aberrant methylation in human colorectal cancers. To this end, biopsies were obtained from four colorectal lesions (one hyperplastic polyp, two adenomatous polyps and one adenocarcinoma) of patients before and after treatment with 200 mg celecoxib per day for 30 days, and were analysed for global DNA methylation and promoter methylation of the ER-α gene. Global DNA methylation was found to be decreased in the adenomatous polyps and adenocarcinomas before treatment, whereas methylation of the ER-α gene promoter was increased. After a 30-day treatment with celecoxib, global DNA methylation was increased and hypermethylation of the ER-α gene promoter was decreased in the adenomatous polyps, but not in the adenocarcinomas, indicating that the drug was able to reverse global DNA hypomethylation and hypermethylation of the ER-α gene in adenomatous polyps, but not in adenocarcinomas [33].
Thus, experimental and primary human data suggest that aspirin and other NSAIDs may reverse tumour suppressor gene hypermethylation in tumour tissues. However, it must be emphasized that, as of yet, the human data are limited. Furthermore, the human studies were aimed at investigating hypermethylation reversal, but not tumour suppressor gene activation. Hypermethylation reversal may not always lead to tumour suppressor gene activation due to the involvement of other downstream processes. In addition, evidence from experimental and human data suggests that aspirin and NSAIDs also reverse global DNA hypomethylation. However, the mechanism underlying the dual action of aspirin and of the other NSAIDs on DNA methylation, i.e., reversal of tumour suppressor gene hypermethylation and reversal of global DNA methylation, seems difficult to define. Although direct modulation of both DNMTs and demethylases may be at work, modulation of targets upstream of epigenetic processes such as the cellular redox state may also be relevant.
4 Histone modifications
Post-translational histone modifications influence the access of transcription factors to DNA target sites to affect gene activity. Specifically, histone acetylation destabilizes chromatin through charge neutralization of the basic lysine residues leading to changes in the chromatin structure and, ultimately, the transcription of genes. Histone modifications are brought about by several enzymes, including histone acetyl transferases (HATs), histone deacetylases (HDACs), histone methyltransferases (HMTs) and histone demethylases (HDMTs). HATs activate and HDACs suppress gene activity, while HMTs and HDMTs either activate or inhibit gene expression, depending on the site and the extent of the methylation induced [34]. HDAC inhibitors represent a new class of promising anti-neoplastic agents, while there is an ongoing interest in inhibitors of HATs, HMTs and HDMTs [35].
5 Targeting histone deacetylases
Current experimental evidence on the modulation of HDACs by salicylates is limited. However, it is interesting to note that both induction and inhibition of HDACs by aspirin have been reported. In a very recent study, Kamble et al. [36] reported that treatment of liver cells with acetylsalicylic acid and salicylic acid induced the HDAC Sirtuin 1 via the production of hydrogen peroxide [36]. There is, however, also one report of HDAC inhibition by sodium salicylate, which is based on data of a study on the teratogenic effect of sodium salicylate on axial abnormalities induced in embryo models [37]. Di Renzo et al. [37] aimed to verify whether the inhibition of embryonic HDAC enzymes, and the consequent tissue hyperacetylation, could underlie axial skeletal defects observed after the exposure of pregnant rodents to sodium salicylate. To this end, pregnant mice were intra-peritoneally treated with sodium salicylate (0-150–300–450 mg/kg) and sacrificed at 1, 3, 5 h after treatment or at term of gestation. A significant sodium salicylate dose-related HDAC inhibitory effect, compatible with a mixed-type partial inhibition mechanism, was detected. A clear dose-related hyperacetylation of histones was observed in embryos exposed in utero to sodium salicylate. A similar HDAC inhibitory activity of salicylates has, however, the not yet been established in adult tissues and/or cancer cells.
An additional in vitro study, aimed at investigating the interaction of the histone deacetylase inhibitors suberoylanilide hydroxamic acid and sodium butyrate with aspirin revealed their synergy in the induction of cell death in the ovarian cancer cell line A2780, but failed to demonstrate inhibition of HDACs by aspirin. Treatment with aspirin had no effect on the acetylation status of histones, neither in the presence nor in the absence of HDAC inhibitors [38]. In fact, it has been found that salicylates and aspirin can modulate HDAC activity by mechanisms not involving enzymatic inhibition. Thus, these agents may epigenetically regulate gene expression through modulation of the interactions of HDACs with transcription factors. In agreement with this notion, Deckmann et al. [39] recently reported that treatment of HeLa cells with dimethylcelecoxib, a non COX2 inhibiting derivative of celecoxib, leads to an enhanced formation of a complex consisting of NF-κB and HDAC1 that binds to the EGR1 gene promoter, resulting in down-regulation of EGR1 expression [39]. The implications of this finding for anticancer drug targeting require further investigation, since (i) NSAIDs have also been reported to up-regulate EGR1 and (ii) EGR1 is a transcription factor, that regulates the expression of about 30 genes and seems to have dual roles in promoting cell survival and apoptosis, depending on the downstream targets involved. In addition, its role in tumourigenesis seems to be cell type-specific. EGR1 has often been reported to be a tumour suppressor gene that induces the up-regulation of a member of the transforming growth factor-β superfamily, i.e., NSAID-activated gene 1 (NAG-1), a protein with an anti-tumourigenic and pro-apoptotic activity [40]. However, other reports have indicated that EGR1 down-regulation may promote tumour cell death.
An interesting question that remains to be addressed is whether salicylates can both induce and inhibit HDACs. In fact, it could be hypothesized that salicylates modulate the fine-tuning of the action of HDACs through redox signalling. This hypothesis remains to be tested and its putative implications for anticancer research remain to be established.
6 Targeting histone acetyltransferases
Since aspirin acetylates proteins, it could be hypothesized that aspirin may also acetylate histones. Indeed, experimental data based on mass spectrometry have shown that aspirin, among other cellular proteins, acetylates histones in HCT-116 colon cancer cells [41]. Using anti-acetyl lysine antibodies, Marimuthu et al. [41] demonstrated that aspirin causes the acetylation of multiple proteins whose molecular weight ranges from 20 to 200 kDa. The identity of these proteins was subsequently determined using immuno-affinity purification, mass spectrometry and immunoblotting. A total of 33 cellular proteins were identified as potential targets of aspirin-mediated acetylation, including enzymes of the glycolytic pathway, cytoskeleton proteins, histones, ribosomal and mitochondrial proteins. In another study, it was found that low concentrations of aspirin induce lysine acetylation of eNOS, and that histone deacetylase 3 antagonizes this action of aspirin. Although this study aimed to investigate cardiovascular actions of aspirin, the authors postulated that the interaction of aspirin and HDAC might act in an antagonistic fashion to regulate gene expression with implications for the anticancer effects of aspirin [42]. It remains to be established, however, whether direct histone acetylation by aspirin can modulate the epigenetic regulation of gene expression. On the other hand, a natural salicylate, anacardic acid (6-pentadecyl salicylic acid), has been shown to inhibit histone acetyl-transferase p300 both in vitro and in vivo, and to regulate gene expression through modulation of histone acetylation [43–45]. More importantly, anacardic acid has been shown to have anti-tumour activities through its histone acetyltransferase inhibition and other mechanisms, including the regulation of histone acetyltransferase p300 transcript and protein levels and NF-κΒ inhibition [43]. Sung et al. [44] investigated the effect of anacardic acid on the NF-κB pathway and found that anacardic acid suppresses NF-κB activation mediated by a variety of stimuli. In addition, anacardic acid was found to inhibit constitutive NF-κB activity. Furthermore, the experimental data suggested that anacardic acid might suppress TNF-induced NF-κB activation via suppression of TNF-induced p65 acetylation through inhibition of histone acetyltransferase activity [44]. Sun et al. [45] also found that anacardic acid can inhibit the Tip60 histone acetyltransferase in vitro, and can block Tip60-dependent activation of the ATM and DNA-PKCS protein kinases by DNA damage in vivo. Furthermore, anacardic acid was found to sensitize human tumour cells to the cytotoxic effects of ionizing radiation [45]. In addition, a very recently published in vitro study has shown that aspirin can regulate DNMT1 via down-regulation of the expression of the acetyltransferase Tip60 in antigen-stimulated RBL2H3 cells [46]. The mechanism of down-regulation of Tip60 by aspirin was not investigated. However, the authors suggested proteasome-dependent degradation of Tip60 by aspirin or transcriptional regulation of the expression of Tip60 by aspirin [46].
Thus, evidence, although limited, supports the notion that salicylates and other NSAIDs can modulate histone modifications. Data from plant studies, however, indicate that histone modification does not play a role in salycilate-mediated regulation of gene expression [47]. In fact, existing experimental data provoke more questions than answers: (i) Are all histone modifications mediated by aspirin and other NSAIDs? Up till now, evidence suggests that salicylates modulate histone acetylation. However, Tanaka et al. [48] have reported that NO-releasing aspirin induces histone H2AX phosphorylation and apoptosis in S-phase cells through the generation of reactive oxygen species (ROS). Although this study aimed to report a potentially cytotoxic effect of NO-aspirin, it remains to be established whether NO-aspirin and/or other salicylates and NSAIDs modulate gene transcription through histone phosphorylation. (ii) Is histone modification a drug effect or a class effect for salicylates and other NSAIDs? Up till now, only salicylates, aspirin and dimethylcelecoxib have been reported to modulate histone modification. (iii) What is the mechanism of histone modification by salicylates and other NSAIDs? (iv) How does histone modification combine with the other mechanisms of anticancer activity of salicylates and other NSAIDs? Salicylates and other NSAIDs have been shown to inhibit NF-κB activity. In fact, Deckman et al. [35] have shown that dimethylcelecoxib modulates the NFkB-HDAC1 interaction.
7 Targeting microRNAs
Current evidence suggests that microRNAs (miRNAs) act in a manner equivalent to oncogenes or tumour suppressor genes during cancer development and progression. miRNAs generally decrease mRNA expression or translation levels and, therefore, miRNAs targeting an oncogene exhibit a tumour suppressor activity via the reduction of gene expression and a subsequent control of cellular growth. On the other hand, certain miRNAs may have oncogene-like functions, with high miRNA expression levels inducing oncogenic transformation. Since miRNA expression levels are known to change in cancer cells, inhibition of over-expression of an oncogene-type miRNA or enhancement of under-expression of a tumor suppressor-type miRNA may have therapeutic effects [49]. Thus, studies aimed at therapeutically targeting of miRNAs have in the recent past been initiated. Generally, up-regulation of miRNAs can be achieved through the administration of synthetic miRNAs or the administration of miRNA expressing vectors. Down-regulation of miRNAs can be achieved through the administration of anti-sense nucleotides, often chemically modified to ensure stability and specificity. There are multiple potential limitations associated with the development and testing of miRNA-based therapies. These include, but are not limited to, off-target effects, avoidance from internal nucleases and toxicity. Experimental evidence suggests that salicylates and other NSAIDs can also down-regulate oncogene-type miRNAs and up-regulate tumour suppressor-type miRNAs. Up till now, the effect of salicylates and NSAIDs has been investigated for a limited number of miRNAs. Since the research field of miRNAs is rapidly evolving and novel technologies for high throughput measurement of miRNA expression levels become available, the effect of salicylates on miRNA expression regulation and its putative anticancer implications are expected to be defined soon.
A very recent in vitro study showed that sulindac can inhibit the invasion of human MDA-MB-231 breast and HCT116 colon tumour cells in vitro at concentrations less than those required to inhibit tumour cell growth [15]. In an attempt to elucidate the underlying mechanism, the investigators evaluated the effect of sulindac on miRNAs and, by doing so, found that 132 miRNAs were affected by sulindac treatment, including miR-9, miR-10b, miR-17 and miR-21, four miRNAs that had been previously implicated in tumour invasion and metastasis. Suppression of NF-κB-mediated transcription of miRNAs was thought to be the underlying cause. Indeed, it was found that NF-κB suppresses the expression of the four miRNAs at the transcriptional level by binding to the respective promoters. In addition, sulindac was found to inhibit the translocation of NF-κB to the nucleus by decreasing the phosphorylation of IKKβ and IκB. Analysis of the promoter sequences of the four miRNAs revealed that 81 out of 115 sequences tested contained NF-κB-binding sites [15]. In addition, aspirin has been reported to be able to down-regulate miR-21 [50]. Lan et al. [50] investigated potential transcription factor 7 like 2 (TCF7L2/TCF4) target miRNAs through a bioinformatics approach. They discovered 26 miRNA transcription start sites within close proximity to TCF4 chromatin occupancy sites, and validated these sites as TCF4 targets in LS174T colon carcinoma cells, MCF-7 breast cancer cells and U87 glioma cells by ChIP-PCR. Triggered by the poorly understood preventive effect of aspirin on colorectal cancer incidence and mortality, they demonstrated down-regulation of miR-21 upon administration of aspirin in LS174T colon carcinoma cells [50]. Interestingly, miR-21 is up-regulated in nearly all epithelial cell-derived solid tumours, including breast, pancreas, lung, stomach, prostate, colon, head and neck and oesophageal cancers. In addition, it has been shown that miR-21 is involved in both the initiation and progression of human cancers. miR-21 is also up-regulated in several haematological malignancies, including leukemias, lymphomas and multiple myelomas. miR-21 has also been found to be over-expressed in glioblastomas, osteosarcomas and spermatocytic seminomas. miR-21 is a negative regulator of p53 signalling, whereas NF-κB signalling is promoted by miR-21. Most of the evidence suggests that miR-21 suppresses the expression of a number of genes that participate directly or indirectly in extrinsic or intrinsic apoptosis pathways to promote tumourigenesis. miR-21 has also been shown to affect the expression of the WNT1 gene as well as that of the tumour suppressor genes PTEN, RECK and PDCD4, and to induce tumourigenesis [51–53], suggesting a central role for miR-21 in cancer. A very recent publication has reported, for the first time, that targeting miR-21 may inhibit pancreatic cancer tumour growth both in vitro and in vivo [54]. Thus, therapeutic targeting of miR-21 may be beneficial for a large number of targets. However, global over-expression of miR-21 does not induce tumours, whereas tissue-specific over-expression does, leading to confusion on whether miR-21 acts as a driver or as a passenger of tumourigenesis.
Ιn a very recently published study, Saito et al. [55] determined miRNA expression profiles in 53 gastric tumours, including gastric adenomas (atypical epithelia), early gastric cancers and advanced gastric cancers, and in gastric cancer cells treated with celecoxib. miR-29c was found to be significantly down-regulated in gastric cancer tissues relative to non-tumour gastric mucosa, and this down-regulation was most prominent in advanced gastric carcinomas. Accordingly, miR-29c has been reported to exhibit tumour suppression functions in gastric carcinoma cells [55]. Celecoxib treatment resulted in miR-29c up-regulation in human gastric cancer cells. In addition up-regulation of miR-29c by celecoxib induced suppression of the oncogene MCL-1, one of the putative miR-29c targets, and a concomitant apoptosis in gastric cancer cells [55].
Chen et al. [56] investigated alterations in miRNA expression patterns in colorectal cancer cells following celecoxib treatment. By doing so, celecoxib was found to inhibit HT-29 cell growth in vitro, and this growth inhibition was partly attributable to the altered expression of miRNAs. Of the 28 aberrantly expressed miRNAs found, 20 were up-regulated and 8 were down-regulated in the HT-29 cells treated with celecoxib compared to the matched control cells. Additionally, the aberrantly expressed miRNAs in HT-29 cells treated with celecoxib were found to modulate multiple target genes involved in several essential cell survival pathways [56].
Since miRNAs can target multiple genes, the anticancer effect of miRNA modulation is not always straightforward. For example, it was recently reported that delivery of the pro-apoptotic miR34a in p53-deficient Saos2 cells did not increase the cell’s sensitivity to apoptosis due to a down-regulation of SIRT1 by miR34a and a subsequent increase in NF-κB activity. Co-treatment with miR34a and aspirin, however, promoted Saos2 cell death [57]. This finding suggests that, although the effect of isolated modulation of a miRNA cannot always be predicted, a synergistic interaction between miRNA modulation by aspirin and a concurrent action of aspirin on e.g. NF-κΒ inhibition can impose anticancer effects.
8 Conclusions and perspectives
Evidence suggests that salicylates and NSAIDs can modulate gene expression, either by silencing or by up-regulating gene expression. As yet, however, the mechanisms by which salicylates and NSAIDs modulate gene expression are not fully known. Current literature data suggest mechanisms for gene silencing by aspirin and NSAIDs through NF-κB and MAPK modification. The mechanisms underlying gene up-regulation are, however, more difficult to delineate. One possibility could be through epigenetic modulation. Current data indeed suggest that epigenetic modulation of gene expression by these agents may play such a role. Moreover, it appears that salicylates and NSAIDs target multiple epigenetic processes. Targeting of multiple epigenetic processes by the same drug is anticipated to be less toxic and more efficient via the establishment of balances between reversal of DNA hypermethylation of tumour suppressor genes and reversal of global DNA hypomethylation. Existing data are, however, limited and most of them are based on statistical associations, without firm in vivo validated cause-effect relationships. So, alternative mechanisms might also explain the observed associations. In any case, the targeting of epigenetic processes may underlie the action of multi-target salicylates and NSAIDs, with putative clinical implications for cancer treatment and chemoprevention. As yet, however, the existing data on the modulation of epigenetic processes by aspirin and NSAIDs are scarce and conflicting, and further research is needed before firm conclusions can be drawn. This research could lead, not only to novel applications of salicylates and NSAIDs in cancer treatment and chemoprophylaxis, but also to the treatment and/or prevention of other diseases and physiological conditions, such as ageing, in which epigenetic processes are known to be involved. In addition, this research could lead to the design of less toxic agents that target epigenetic processes. In this respect, the natural salicylate anacardic acid has already been used as a lead compound for the design of novel acetyl-transferase inhibitors [58].
Another interesting question to be addressed is how important epigenetic targets are in relation to the other, already known, conventional targets of aspirin and NSAIDs. It could be hypothesized that epigenetic targets are the nodal targets of aspirin and NSAIDs. Epigenetic modifications represent ways by which cells may effectively translate multiple signaling inputs into phenotypic outputs. In other words, epigenetic changes may elicit an adaptive response to various events, rather than to one a priori event that controls gene expression [59]. Research on plant physiology has provided valuable information on the mechanism of action of salicylates. Salicylates are phyto-hormones that modulate plant stress responses to various environmental stressors, i.e., salicylic acid enhances plant adaptation to environmental stress through modulation of the expression of a vast number of genes, at least partly through DNA methylation [60]. Aspirin and other NSAIDs are multi-target agents that are known to modulate multiple signaling pathways [61]. In addition, salicylates and NSAIDs modulate cellular redox states and induce cellular stress responses. Reactive oxygen species (ROS) are known inducers of epigenetic changes [61]. Thus, it could be suggested that salicylates produce reactive oxygen species, modulate ROS signaling and affect gene expression through epigenetic alterations. Although further research is required to integrate the multiple mechanisms of action of salicylates into a central mechanism, existing evidence supports the interplay among redox regulation, epigenetic alterations and pathway signalling [59, 62]. The net effect of these mechanisms is the modulation of gene expression. Down-regulation of tumour suppressor genes seems to be one of the primary steps in carcinogenesis, whereas advanced tumour stages are rather associated with alterations in the expression of genes that promote invasion and metastasis. Salicylates and NSAIDs have been shown to up-regulate the expression of tumour suppressor genes [60], although the molecular mechanisms underlying this up-regulation have not yet been clearly defined. One theory could be that salicylates and NSAIDs modulate gene expression through direct interactions with diverse intracellular signal transduction pathways. Growing evidence, however, supports the epigenetic regulation of tumour suppressor genes such as e.g. PTEN [63]. Also, at pharmacological concentrations, salicylates inhibit COX2 expression through transcription based mechanisms, i.e., by blocking C/EBPβ phosphorylation, activation and binding to the COX2 promoter via p90 ribosomal S6 kinase 1/2 (RSK1/2) [64]. On the other hand, it is known that COX2 expression is regulated through epigenetic mechanisms [65]. Thus, it may be suggested that, apart from enzymatic inhibition, salicylates and NSAIDs regulate COX2 via both mechanisms targeting signalling pathways and epigenetic mechanisms. To the best of our knowledge, there are no mechanistic studies available that directly support this hypothesis for salicylates. However, this dual mechanism of gene regulation, involving both direct interaction with intracellular signalling pathways and modulation of epigenetic mechanisms, is supported by curcumin and the regulation of NAG-1 by the HDAC inhibitor trichostatin A [66, 67]. Since a single epigenetic factor is able to orchestrate the expression of a large number of genes, modulation of epigenetic processes by aspirin and NSAIDs is expected to have implications for cancer chemoprevention and treatment. In this respect, it would be interesting to gain further insight into the contribution of the modulation of epigenetic mechanisms in the overall mechanisms of action of aspirin and NSAIDs as chemopreventive agents. A further step could be to e.g. investigate to what extent the epigenetic mechanisms are involved in the up-regulation of tumour suppressor genes. In addition, further research might be aimed at unraveling the possible synergistic anti-proliferative effects of aspirin and other NSAIDs with other compounds that modulate epigenetic processes, with already approved epigenetic drugs and/or with conventional chemotherapeutics and small molecules designed for targeted cancer treatment.
In conclusion, although the existing evidence is still limited, a picture is emerging that epigenetic targets potentially represent essential nodes for the anti-proliferative action of salicylates and NSAIDs. This may have implications for cancer chemoprevention and treatment.
References
D. Nebert, G. Zhang, E. Vesell, From human genetics and genomics to pharmacogenetics and pharmacogenomics: past lessons, future directions. Drug Metab Rev 40, 187–224 (2008)
P.K. Lo, S. Sukumar, Epigenomics and breast cancer. Pharmacogenomics 9, 1879–1902 (2008)
J.G. Martínez, J. Pérez-Escuredo, P. Castro-Santos, C.A. Marcos, J.L. Pendás, M.F. Fraga, Hermsen. M.A. Hypomethylation of LINE-1, and not centromeric SAT-α, is associated with centromeric instability in head and neck squamous cell carcinoma. Cell Oncol 35, 259–67 (2012)
S. Babashah, M. Sadeghizadeh, M.R. Tavirani, S. Farivar, Soleimani. M. Aberrant microRNA expression and its implications in the pathogenesis of leukemias. Cell Oncol 35, 317–34 (2012)
R. Nagadia, P. Pandit, W.B. Coman, J. Cooper-White, C. Punyadeera, miRNAs in head and neck cancer revisited. Cell Oncol 36, 1–7 (2013)
C. Lema, M. Cunningham, MicroRNAs and their implications in toxicological research. Toxicol Lett 198, 100–105 (2010)
P.J. Mishra, P.J. Mishra, D. Barenjee, J.R. Bertino, MiRNSPs or MiR polymorphisms, new players in microRNA mediated regulation of the cell. Cell Cycle 7, 853–858 (2008)
P.J. Mishra, J.R. Bertino, MicroRNA polymorphisms: the future of pharmacogenomics, molecular epidemiology and personalized medicine. Pharmacogenomics 10, 399–416 (2009)
E.D. Wiklund, J. Kjems, S.J. Clark, Epigenetic architecture and miRNA: reciprocal regulators. Epigenomics 6, 823–840 (2010)
F.A. Duijkers, R.X. de Menezes, I.J. Goossens-Beumer, D.J. Stumpel, P. Admiraal, R. Pieters, J.P. Meijerink, M.M. van Noesel, Epigenetic drug combination induces genome-wide demethylation and altered gene expression in neuro-ectodermal tumor-derived cell lines. Cell Oncol 36, 351–62 (2013)
J.P. Issa, H.M. Kantarjian, Targeting DNA methylation Clin Cancer Res 15, 3938–46 (2009)
J. García-Quiroz, J. Camacho, Astemizole: an old anti-histamine as a new promising anti-cancer drug. Anticancer Agents Med Chem 11, 307–14 (2011)
C. Zhao, X. Bu, Promoter methylation of tumor-related genes in gastric carcinogenesis. Histol Histopathol 27, 1271–82 (2012)
T.M. Brasky, M.R. Bonner, K.B. Moysich, C.B. Ambrosone, J. Nie, M.H. Tao, S.B. Edge, B.V. Kallakury, H.M. Ochs-Balcom, C. Marian, M. Trevisan, P.G. Shields, J.L. Freudenheim, Non steroidal anti-inflammatory drug use (NSAID) and breast cancer risk in the western New York exposures and breast cancer (WEB) study. Cancer Causes Control 9, 1503–1512 (2010)
Li, X.; Gao, L.; Cui, Q.; Gary, B.D.; Dyess, D.L.; Taylor, W.; Shevde, L.A.; Samant, R.S.; Dean-Colomb, W.; Piazza, G.A.; Xi, Y. Sulindac inhibits tumor cell invasion by suppressing NF-κB-mediated transcription of microRNAs. Oncogene 31, 4979–4986 (2012)
E. Yiannakopoulou, Modulation of lymphangiogenesis: a New target for aspirin and other Nonsteroidal anti-inflammatory agents? a systematic review. J Clin Pharmacol 52, 1749–54 (2011)
M. Dovizio, A. Bruno, S. Tacconelli, P. Patrignani, Mode of action of aspirin as a chemopreventive agent. Recent Results Cancer Res 191, 39–65 (2013)
J. Worm, P. Guldberg, DNA methylation: an epigenetic pathway to cancer and a promising target for anticancer therapy. J Oral Pathol Med 31, 443–9 (2002)
J. Paluszczak, V. Krajka-Kuźniak, W. Baer-Dubowska, The effect of dietary polyphenols on the epigenetic regulation of gene expression in MCF7 breast cancer cells. Toxicol Lett 192, 119–125 (2010)
J.L. Medina-Franco, T. Caulfield, Advances in the computational development of DNA methyltransferase inhibitors. Drug Discov Today 16, 418–425 (2011)
D. Kuck, N. Singh, F. Lyko, J.L. Medina-Franco, Novel and selective DNA methyltransferase inhibitors: Docking-based virtual screening and experimental evaluation. Bioorg Med Chem 18, 822–829 (2010)
J. Yoo, J.L. Medina Franco, Trimethylaurintricarboxylic acid inhibits human DNA methyltransferase 1: insights from enzymatic and molecular modeling studies. J Mol Model 18, 1583–1589 (2012)
M.R. Pan, H.C. Chang, L.Y. Chuang, W.C. Hung, The nonsteroidal anti-inflammatory drug NS398 reactivates SPARC expression via promoter demethylation to attenuate invasiveness of lung cancer cells. Exp Biol Med (Maywood) 233, 456–462 (2008)
T. Tahara, T. Shibata, M. Nakamura, H. Yamashita, D. Yoshioka, M. Okubo, N. Maruyama, T. Kamano, Y. Kamiya, H. Fujita, M. Nagasaka, M. Iwata, K. Takahama, M. Watanabe, I. Hirata, T. Arisawa, Chronic aspirin use suppresses CDH1 methylation in human gastric mucosa. Dig Dis Sci 55, 54–9 (2010)
T. Tahara, T. Shibata, H. Yamashita, M. Nakamura, D. Yoshioka, M. Okubo, I. Hirata, T. Arisawa, Chronic nonsteroidal anti-inflammatory drug (NSAID) use suppresses multiple CpG islands hyper methylation (CIHM) of tumor suppressor genes in the human gastric mucosa. Cancer Sci 100, 1192–1197 (2009)
M.L. Slattery, R.K. Wolff, J. Herrick, B.J. Caan, W. Samowitz, Tumor markers and rectal cancer: support for an inflammation-related pathway. Int J Cancer 125, 1698–1704 (2009)
M.L. Slattery, K. Curtin, C. Sweeney, T.R. Levin, J. Potter, R.K. Wolff, H. Albertsen, W.S. Samowitz, Diet and lifestyle factor associations with CpG island methylator phenotype and BRAF mutations in colon cancer. Int J Cancer 120, 656–663 (2007)
E.I. Heath, M.I. Canto, S. Piantadosi, E. Montgomery, W.M. Weinstein, J.G. Herman, A.J. Dannenberg, V.W. Yang, A.O. Shar, E. Hawk, A.A. Forastiere, Chemoprevention for Barrett’s esophagus trial research group. Secondary chemoprevention of Barrett’s esophagus with celecoxib: results of a randomized trial. J. Natl. Cancer Risk 99, 545–557 (2007)
K. Wallace, M.V. Grau, A.J. Levine, L. Shen, R. Hamdan, X. Chen, J. Gui, R.W. Haile, E.L. Barry, D. Ahnen, G. McKeown-Eyssen, J.A. Baron, J.P. Issa, Association between folate levels and CpG Island hypermethylation in normal colorectal mucosa. Cancer Prev Res (Phila) 3, 1552–1564 (2010)
J.C. Figueiredo, M.V. Grau, K. Wallace, A.J. Levine, L. Shen, R. Hamdan, X. Chen, R.S. Bresalier, G. McKeown-Eyssen, R.W. Haile, J.A. Baron, J.P. Issa, Global DNA hypomethylation (LINE-1) in the normal colon and lifestyle characteristics and dietary and genetic factors. Cancer Epidemiol Biomarkers Prev 18, 1041–1049 (2009)
L. Tao, W. Wang, P.M. Kramer, R.A. Lubet, V.E. Steele, M.A. Pereira, Modulation of DNA hypomethylation as a surrogate endpoint biomarker for chemoprevention, of colon cancer. Mol Carcinogen 39, 79–842 (2004)
M.A. Pereira, L. Tao, W. Wang, Y. Li, A. Umar, V.E. Steele, Modulation by celecoxib and difluoromethylornithine of the methylation of DNA and the estrogen receptor-alpha gene in rat colon tumors. Carcinogenesis 25, 1917–1923 (2004)
R. Shen, L. Tao, Y. Xu, S. Chang, J. Van Brocklyn, J.X. Gao, Reversibility of aberrant global DNA and estrogen receptor-alpha gene methylation distinguishes colorectal precancer from cancer. Int J Clin Exp Pathol 2, 21–23 (2009)
R.M. Eglen, T. Reisine, Screening for compounds that modulate epigenetic regulation of the transcriptome: an overview. J Biomol Screen 16, 1137–1152 (2011)
A. Mai, L. Altucci, Epi-drugs to fight cancer: from chemistry to cancer treatment, the road ahead. Int J Biochem Cell Biol 41, 199–213 (2009)
P. Kamble, K. Selvarajan, C. Aluganti Narasimhulu, M. Nandave, S. Parthasarathy, Aspirin may promote mitochondrial biogenesis via the production of hydrogen peroxide and the induction of Sirtuin1/PGC-1α genes. Eur J Pharmacol 699, 55–61 (2013)
F. Di Renzo, G. Cappelletti, M.L. Broccia, E. Giavini, E. Menegola, The inhibition of embryonic histone deacetylases as the possible mechanism accounting for axial skeletal malformations induced by sodium salicylate. Toxicol Sci 104, 397–404 (2008)
J. Sonnemann, I. Hüls, M. Sigler, C.D. Palani, T.T. le Hong, U. Völker, H.K. Kroemer, J.F. Beck, Histone deacetylase inhibitors and aspirin interact synergistically to induce cell death in ovarian cancer cells. Oncol Rep 20, 219–224 (2008)
K. Deckmann, F. Rörsch, G. Geisslinger, S. Grösch, Dimethylcelecoxib induces an inhibitory complex consisting of HDAC1/NF-κB(p65)RelA leading to transcriptional downregulation of mPGES-1 and EGR1. Cell Signal 24, 460–467 (2012)
H. Yoshioka, T. Watanabe, T.E. Eling, Nonsteroidal anti-inflammatory drug-activated gene (NAG-1/GDF15) expression is increased by the histone deacetylase inhibitor trichostatin A. J Biol Chem 283, 33129–33137 (2008)
S. Marimuthu, R.S. Chivukula, L.F. Alfonso, M. Moridani, F.K. Hagen, G.J. Bhat, Aspirin acetylates multiple cellular proteins in HCT-116 colon cancer cells: Identification of novel targets. Int J Oncol 39, 1273–1283 (2011)
S.B. Jung, C.S. Kim, A. Naqvi, T. Yamamori, I. Mattagajasingh, T.A. Hoffman, M.P. Cole, A. Kumar, J.S. Dericco, B.H. Jeon, K. Irani, Histone deacetylase 3 antagonizes aspirin-stimulated endothelial nitric oxide production by reversing aspirin-induced lysine acetylation of endothelial nitric oxide synthase. Circ Res 107, 877–87 (2010)
J. Tan, B. Chen, L. He, Y. Tang, Z. Jiang, G. Yin, J. Wang, X. Jiang, Anacardic acid (6-pentadecylsalicylic acid) induces apoptosis of prostate cancer cells through inhibition of androgen receptor and activation of p53 signaling. Chin J Cancer Res 24, 275–83 (2012)
B. Sung, M.K. Pandey, K.S. Ahn, T. Yi, M.M. Chaturvedi, M. Liu, B.B. Aggarwal, Anacardic acid (6-nonadecyl salicylic acid), an inhibitor of histone acetyltransferase, suppresses expression of nuclear factor-kappaB-regulated gene products involved in cell survival, proliferation, invasion, and inflammation through inhibition of the inhibitory subunit of nuclear factor-kappaBalpha kinase, leading to potentiation of apoptosis. Blood 111, 4880–4891 (2008)
Y. Sun, X. Jiang, S. Chen, B.D. Price, Inhibition of histone acetyltransferase activity by anacardic acid sensitizes tumor cells to ionizing radiation. FEBS Lett 580, 4353–4356 (2006)
Y. Kim, K. Kim, D. Park, E. Lee, H. Lee, Y.S. Lee, J. Choe, Y.M. Kim, D. Jeoung, DNA methyl transferase I acts as a negative regulator of allergic skin inflammation. Mol Immunol 53, 1–14 (2013)
A. Koornneef, K. Rindermann, C. Gatz, C.M. Pieterse, Histone modifications do not play a major role in salicylate-mediated suppression of jasmonate-induced PDF1.2 gene expression. Commun Integr Biol 1, 143–5 (2008)
T. Tanaka, A. Kurose, H.D. Halicka, X. Huang, F. Traganos, Z. Darzynkiewicz, Nitrogen oxide-releasing aspirin induces histone H2AX phosphorylation, ATM activation and apoptosis preferentially in S-phase cells: involvement of reactive oxygen species. Cell Cycle 5, 1669–74 (2006)
M. Yanokura, K. Banno, Y. Kobayashi, I. Kisu, A. Ueki, A. Ono, K. Masuda, H. Nomura, A. Hirasawa, N. Susumu, D. Aoki, MicroRNA and endometrial cancer: Roles of small RNAs in human tumors and clinical applications (Review). Oncol Lett 1, 935–940 (2010)
F. Lan, X. Yue, L. Han, Z. Shi, Y. Yang, P. Pu, Z. Yao, C. Kang, Genome-wide identification of TCF7L2/TCF4 target miRNAs reveals a role for miR-21 in Wnt-driven epithelial cancer. Int J Oncol 40, 519–526 (2012)
Y. Chen, W. Liu, T. Chao, Y. Zhang, X. Yan, Y. Gong, B. Qiang, J. Yuan, M. Sun, X. Peng, MicroRNA-21 down-regulates the expression of tumor suppressor PDCD4 in human glioblastoma cell T98G. Cancer Lett 272, 197–205 (2008)
F. Meng, R. Henson, H. Wehbe-Janek, K. Ghoshal, S.T. Jacob, T. Patel, MicroRNA-21 regulates expression of the PTEN tumor suppressor gene in human hepatocellular cancer. Gastroenterology 133, 647–658 (2007)
Q. Yao, H. Xu, Q.Q. Zhang, H. Zhou, L.H. Qu, MicroRNA-21 promotes cell proliferation and down-regulates the expression of programmed cell death 4 (PDCD4) in HeLa cervical carcinoma cells. Biochem Biophys Res Commun 388, 539–542 (2009)
Sicard, F.; Gayral, M.; Lulka, H.; Buscail, L.; Cordelier, P. Targeting miR-21 for the Therapy of Pancreatic Cancer. Mol Ther, 2013, doi: 10.1038/mt.2013.35
Y. Saito, H. Suzuki, H. Imaeda, J. Matsuzaki, K. Hirata, H. Tsugawa, S. Hibino, Y. Kanai, H. Saito, T. Hibi, The tumor suppressor microRNA-29c is downregulated and restored by celecoxib in human gastric cancer cells. Int J Cancer 132, 1751–1760 (2013)
W.C. Chen, M.S. Lin, Y.L. Ye, H.J. Gao, Z.Y. Song, X.Y. Shen, microRNA expression pattern and its alteration following celecoxib intervention in human colorectal cancer. Exp Ther Med 3, 1039–1048 (2012)
J. Tan, L. Fan, J.J. Mao, B. Chen, L. Zheng, T. Zhang, T. Li, J. Duan, Y. Duan, Z. Jin, W. Kuang, Restoration of miR-34a in p53 deficient cells unexpectedly promotes the cell survival by increasing NFκB activity. J Cell Biochem 113, 2903–8 (2012)
E.D. Eliseeva, V. Valkov, M. Jung, M.O. Jung, Characterization of novel inhibitors of histone acetyltransferases. Mol Cancer Ther 6, 2391–2398 (2007)
A.R. Cyr, F.E. Domann, The redox basis of epigenetic modifications: from mechanisms to functional consequences. Antioxid Redox Signal 15, 551–589 (2011)
R.H. Dowen, M. Pelizzola, R.J. Schmitz, R. Lister, J.M. Dowen, J.R. Nery, J.E. Dixon, J.R. Ecker, Widespread dynamic DNA methylation in response to biotic stress. Proc Natl Acad Sci U S A 109, E2183–E2191 (2012)
K. Schrör, Pharmacology and cellular/molecular mechanisms of action of aspirin and non-aspirin NSAIDs in colorectal cancer. Best Pract Res Clin Gastroenterol 25, 473–484 (2011)
E.C. Yiannakopoulou, E. Tiligada, Protective effect of salicylates against hydrogen peroxide stress in yeast. J Appl Microbiol 106, 903–908 (2009)
M.C. de Andrés, K. Imagawa, K. Hashimoto, A. Gonzalez, H.I. Roach, M.B. Goldring, R.O. Oreffo, Loss of methylation in CpG sites in the NF-κB enhancer elements of inducible nitric oxide synthase is responsible for gene induction in human articular chondrocytes. Arthritis Rheum 65, 732–742 (2013)
Fata, J.E.; Debnath, S.; Jenkins, E.C. Jr; Fournier, M.V. Nongenomic Mechanisms of PTEN Regulation. Int. J. Cell Biol., 2012, 379685
K.K. Wu, Transcription-based COX-2 inhibition: a therapeutic strategy. Thromb Haemost 96, 417–422 (2006)
D.A. Dixon, F.F. Blanco, A. Bruno, P. Patrignani, Mechanistic aspects of COX-2 expression in colorectal neoplasia. Recent Results Cancer Res 191, 7–37 (2013)
S. Fu, R. Kurzrock, Development of curcumin as an epigenetic agent. Cancer 116, 4670–4676 (2010)
Conflict of interest statement
The author has nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yiannakopoulou, E. Targeting epigenetic mechanisms and microRNAs by aspirin and other non steroidal anti-inflammatory agents - implications for cancer treatment and chemoprevention. Cell Oncol. 37, 167–178 (2014). https://doi.org/10.1007/s13402-014-0175-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-014-0175-7