Abstract
Purpose: This research aimed to develop non-effervescent floating mini-caplets of Ferrous Ascorbate (FA) using low-density polymers to overcome the problems of poor bioavailability associated with immediate-release iron products. Methods: The excipients and method (melt granulation) were selected based on pre-and post-compression parameters in trial batches. The formulation was optimized by a full factorial 32 experimental design. An optimized formulation was evaluated for drug release kinetic, accelerated stability study, and in vivo study in healthy adult New Zealand female rabbits. Results: The optimized formulation F6 mini-caplets (42.5% FA, 45% Glyceryl palmitostearate as Precirol, 10% polyvinyl pyrrolidone K-30, and 2.5% lactose) were found to have instant floating and 12 h floating duration in 0.1N Hydrochloric acid (HCl) dissolution medium. In vitro drug release (diffusion mechanism) at 1 h and 5 h was 30–35% and 65–70%, respectively. It was found stable for three months under an accelerated stability study. In vivo study showed significantly increased serum iron levels and decreased unsaturated iron binding capacity (UIBC) in the test group (optimized formulation) compared to control and standard (immediate-release iron). Conclusion: Based on the in vitro and in vivo results, we conclude that non-effervescent floating FA mini-caplets have higher bioavailability compared to immediate release FA, which may be attributed to prolonged iron release at its absorption site due to their retention in the gastric region. Hence, non-effervescent floating FA mini-caplets may act as a potential approach for iron deficiency.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Iron, an essential micronutrient, is vital in erythropoiesis [1]. It exists in a ferrous (divalent) and ferric (trivalent) form. As there is no active mechanism for iron excretion, the optimum iron level is maintained by controlled iron absorption through divalent metal transporter 1 (DMT1) carrier protein of duodenal enterocytes and iron recycling from stored iron [2]. Iron deficiency results from chronic blood loss, inadequate iron intake, and increased iron demand during pregnancy and growth. Iron deficiency leads to anaemia, contributing to about 42% of cases in children under the age of five years and 50% of all cases among nonpregnant and pregnant women worldwide [3, 4]. One global study showed that almost 1.2 billion people suffered iron deficiency anaemia; twice the population estimated to have suffered iron deficiency without anaemia (IDWA) [5, 6]. Iron supplementation prevents iron deficiency anaemia [6,7,8].
Oral non-haem iron supplementations are marketed as inorganic or organic salts of ferrous or ferric iron. Ferric iron is less soluble than ferrous at duodenal pH, and only solubilized ferric gets converted into ferrous form. Moreover, duodenal cells absorb iron in ferrous form, not ferric iron. Due to these reasons, ferrous iron is more bioavailable than ferric iron; hence, ferrous preparations are preferred over ferric [9]. Iron absorption increases in the presence of ascorbic acid as it keeps the iron in a ferrous state (absorbable form) [10]. FA, the organic chelate of ferrous iron, is one of the preferred oral iron supplements in clinical practice owing to its high efficacy and tolerability in adults and children [11, 12]. Gastrointestinal side effects are predominant with marketed immediate-release (IR) iron formulations; enteric-coated or sustained-release ferrous iron formulations are available with comparatively low side effects but face poor bioavailability due to short gastric emptying time, as iron is absorbed in the upper gastrointestinal region [13, 14].
The novel Gastroretentive Drug Delivery Systems (GRDDS) use different approaches, i.e. effervescent and non-effervescent floating, expandable, high density, mucoadhesive, super porous hydrogel, and magnetic system, which can delay gastric emptying and may improve the bioavailability of drugs with upper GIT-gastrointestinal, as an absorption window [15, 16]. Floating GRDDS remain buoyant in the stomach because their bulk density is lower than gastric fluid. These systems are retained for a prolonged time in a gastric region without affecting the gastric emptying rate and release the drug slowly at the desired rate [16]. FA GRDDS as a floating effervescent tablet of FA [17] and multi-particulate floating effervescent pellets of FA [18] have been researched. The non-effervescent floating approach for FA has not been investigated.
Mini-caplets as multiple-unit dosage form was selected due to the advantages of small size for ease of administration, less dose dumping risk, and the possibility of dosage adjustment over a single unit [19]. Due to their uniform size and shape, smooth surface, low porosity, and high strength, mini-tablets/caplets can maintain their structure more consistently than other multi-particulate dosage forms, i.e. pellets and granules.
The gas-generating floating systems may face premature evacuation due to the lag time involved before floating, which can be solved by non-effervescent immediately floating dosage forms formulated using low-density fatty materials (Precirol ATO 5®) [16, 20].
This study aimed to develop non-effervescent floating mini-caplets of FA to treat iron deficiency. This formulation would be with improved iron bioavailability compared to immediate release FA formulation. Immediate floating sustained release FA formulation retained in the stomach will release iron continuously for more than 12 h to make it available at the absorption window (duodenum) without saturating the DMT 1 carrier protein. This feature of the formulation would lead to increased utilization of the iron dose administered and would improve the bioavailability of iron which is low in case of immediate release iron formulation. The iron bioavailability is low with immediate release iron formulations due to short gastric emptying time that leads to poor utilization of iron dose administered as iron passes beyond duodenum is poorly absorbed and as the iron absorption is carrier mediated, carrier saturation at absorption site also affects the bioavailability. The higher fraction of unabsorbed iron from immediate release iron products associated with predominant gastrointestinal side effects. The iron bioavailability is also questionable with sustained release and delayed release iron formulations due to short gastric emptying time.
Materials and methods
Materials
FA (Fine Star Industry, India), Ammonio methacrylate copolymer type B as Eudragit RSPO (Evonik Roehm Pharma Polymers, Evonik India Pvt. Ltd.), Polyvinyl pyrrolidone (PVP) K-30 (50 K Daltons molecular weight) (Oxford Lab Fine Chem Limited Liability Partnership, India), 1, 10-Phenanthroline monohydrate (Merck Life Sciences Pvt. Ltd., India), Lactose monohydrate (Pallav Chemicals and Solvents Pvt. Ltd., India), Iron and TIBC kit (Coral Clinical Systems, India) were procured. Glyceryl palmitostearate as Precirol ATO 5® was a sample gift from Gattefosse India Pvt. Ltd. Hydroxyl Propyl Methyl Cellulose-HPMC grade K100M (100 K centipoise viscosity) and K200M (200 K centipoise viscosity) were sample gifts from Colorcon Asia Pvt. Ltd., India.
Methods
Drug characterization and drug-polymer compatibility study by Fourier Transform Infrared Spectroscopy (FTIR)
FTIR spectrum of the drug was checked for characteristic peaks of functional groups. The Drug-polymer compatibility study was checked through a comparison of FTIR spectra of drug and physical mixture of drug with polymers at a 1:1:1 ratio of Drug: Precirol Eudragit RSPO, stored in an airtight container for one month at 25 °C ± 2 °C temperature and 60 ± 5% relative humidity (RH). An IRSpririt FTIR spectrometer, SHIMADZU, Japan, based on the ‘Attenuated total reflection technique’ was used to generate FTIR spectra in a range of wavenumbers of 4000 to 400 cm−1.
Preparation of floating FA mini-caplets
The TR0 batch was prepared by direct compression method in which all the ingredients except Aerosil® were individually screened through the 85# sieve, weighed accurately, and mixed in a poly bag for 5 min. This mixture was blended for 5 min after adding Aerosil® (100# size) to get the final blend. For other batches, the melt granulation process was followed. In this process, all the ingredients (22#) except Precirol were mixed for 5 min in a poly bag. This dry mixture was added to the melted Precirol lipid, contained in a porcelain bowl. The mixture was kneaded for 4 min. (Further, kneading was avoided to keep the mixture in a consistency suitable for granulation through screening, as the hard mass formed due to the solidification of Precirol at room temperature was difficult to granulate). The soft-kneaded mass was screened through 16# to get the undersize granules on a butter paper sheet which were allowed to cool down in open air at room temperature (30 °C), and 60% RH for 10 min. The solidified granules were screened through 16# and 22# sieves to collect the bulk of granules of sizes between 16 and 22#. These granules were selected as the final blend for compression into mini-caplets. The formulation composition of trial batches is shown in Table 1.
The final blends of all the trial batches were checked for the pre-compression parameters, including bulk density, tapped density, and angle of repose, as per the standard procedure [21]. All the formulation blends were compressed using a rotary tablet compression machine (RIMEK Minipress- II MT, India) with 7.5 * 3.5 mm die-punch tooling set [19], set to 100 mg weight per mini-caplet and thickness of 4.6 ± 0.2 mm. All the batches were evaluated for the post-compression parameters.
Evaluation parameters of FA mini-caplets
Weight variation and % friability loss
The compressed mini-caplets were evaluated for weight variation by weighing (Wensar, India) 20 mini-caplets individually and determining the percentage deviation (% D) from the mean weight. The % friability loss was checked by taking mini-caplets equivalent to 6.5 g in a friability apparatus (The Indo Sati Instruments and Chemicals, India), rotated at 25 rotations per minute for 4 min. The % loss was calculated based on the difference in weight before and after the test [21, 22].
Drug content
For each batch, mini-caplets weighing 100 mg FA were crushed and dispersed in 100 ml of 0.1N HCl. The drug dispersion in a closed container was stirred for 1 h in a bath sonicator, kept at 25 °C, filtered, and diluted with 0.1N HCl. The 1 ml diluted drug solution (equivalent to 100 µg/ml) was mixed with 1 ml of 1, 10-Phenanthroline reagent (0.15%w/v in deionized water) for 1 min (makes a red-coloured complex with ferrous metal) and diluted to 10 ml with deionized water. The absorbance of this solution was measured at 515 nm using a UV Spectrophotometer (UV-1800 240 V, Shimadzu, Japan).
In vitro drug release
In vitro drug release was evaluated using USP type 2 Paddle dissolution apparatus (VDA-8D, Veego Instruments Corporation, India). 2 mini-caplets or mini-caplets equivalent to 100 mg FA were introduced into 900 ml 0.1 N HCl dissolution medium, maintained at 37 °C ± 0.5 °C, and stirred at 50 RPM (paddle speed). After 1 h, a 5 ml sample was withdrawn from the dissolution flask (sample amount was replaced with fresh 0.1N HCl), filtered, and analyzed to measure % Cumulative Drug Release (CDR). The samples were collected at every 1 h interval and up to a maximum of 12 h.
Floating lag time and floating duration
These parameters were measured during in vitro drug release evaluation. Floating lag time is the time the mini-caplet takes to reach the dissolution medium surface if it sinks. The floating duration is the total time of floating of mini-caplets on the dissolution medium surface.
Drug release kinetic
To understand the drug release mechanism, model fitting of the % CDR data of the optimized formulation was done using DD Solver 1.0 Program for zero order, first order, Higuchi, Hixon Crowell cube root, and Korsmeyer-Peppas models to find out the best-fit model [23].
Statistical analysis
The statistical analysis was done using Stat-Ease®360 Design Expert software. Response Surface randomized method of 3 Level Factorial with nine runs design type was applied with quadratic model analysis.
Comparison of the in vitro drug release and floating behaviour of optimized floating SR mini-caplets with IR FA tablets
The floating SR FA mini-caplets batch, considered an optimized one, was compared with immediate-release (IR) FA tablets in terms of CDR and floating behaviour. The IR FA single-unit tablet contained 100 mg of elemental iron. The comparison was done to understand the influence of formulation composition on these parameters.
Accelerated stability studies
The check the stability of the formulation under external temperature and humidity, the mini-caplets of the optimized formulation were evaluated. The mini-caplets were evaluated for weight variation, % friability loss, drug content, floating behaviour, and in vitro drug release parameters before its storage, and after three months of storage. The mini-caplets were stored in an airtight High-density polyethylene bottle (HDPE), kept in a stability chamber (PSI, Patel Scientific Instruments Pvt. Ltd.), at 40 °C ± 2 °C temperature and 75 ± 5% RH, as per the accelerated stability studies guideline of International Council for Harmonization [24].
In vivo study
The in vivo animal study was conducted to investigate iron bioavailability (based on the measurement of serum iron and UIBC) [25]. Adult female New Zealand white rabbits weighing 3 to 3.5 kg were employed for the study. Animals were procured from Zydus Research Center, Ahmedabad, and housed at an animal house of L.J. Institute of Pharmacy for two weeks before the study. Rabbits were maintained at 25 ± 3 °C temperature, 55 ± 5% humidity, and a 12-h light/dark cycle. Rabbits were fed with a standard diet and water ad libitum. The study was approved with protocol number LJIP/IAEC/2022–23/04 by the Institutional Animal Ethics Committee, L.J. Institute of Pharmacy, Ahmedabad. Animal care and handling was according to the Committee for Control and Supervision of Experiments on Animals (CCSEA) guidelines.
Study design and biochemical parameters
For the study, rabbits were divided into three groups (n = 3): control (received water), standard (received IR FA), and test (received non-effervescent floating mini-caplets). The standard and test groups were administered the same dose of elemental iron, 2 mg/Kg (equivalent to human dose: 47 mg elemental iron) [26,27,28]. Animals were kept in fasting condition for 12 h before administration of a single dose of the test or standard formulation (using oral intubation tube: 20FG). Blood samples were collected from the marginal ear vein, pre-dose (0 h), and post-dose (3 h, 6 h, and 12 h) to study the effect of formulation on serum iron and UIBC [25], which were estimated using the Ferrozine/Magnesium Carbonate Method (Iron and TIBC colorimetric kit) [29].
The data are presented as mean ± S.E.M (standard error of the mean). The significance of the difference in means between various groups was determined by one-way analysis of variance (ANOVA) and two-way ANOVA. Post hoc comparison was carried out using Tukey’s test. The statistical analysis was performed using GraphPad Prism, Version 8.0.2 (GraphPad Software, Inc., California, USA). In all tests, the criterion for statistical significance was p < 0.05.
Results and discussion
Drug characterization and drug-polymer compatibility study by FTIR
FTIR spectroscopy is a characterization tool used to confirm the molecular structures of the drugs. Figure 1(a) of FTIR spectrum of FA showed a broad peak of the hydroxyl group in the 3500 to 3200 cm−1 range, carbonyl group around 1754 cm−1, and ether linkage c–o–c near 1100 cm−1, which are the characteristic peaks of FA [30,31,32].
FTIR spectrum of a drug mixture with Precirol and Eudragit RSPO polymers (Fig. 1(b)) showed characteristic peaks of a drug with no significant shift, suggesting no chemical interaction between a drug and polymers. The results indicate the compatibility of these polymers with the drug [33, 34]
Preparation of floating FA mini-caplets
Precirol ATO 5 was selected because it is a low-density meltable lipidic material that acts as a binder, facilitates solvent-free melt granulation technique, and may influence mini-caplet floating. It may control the drug release due to the long diffusion path from the dense lipid matrix [21].
Melt granulation facilitates the aggregation of powder particles using binders, which melts or softens at relatively low temperature of 50 to 90 °C. In this granulation process, the low melting binders can be added in the form of molten liquid to the heated powders contained in a formulation. The cooling of aggregated powder and subsequent solidification of the soften or molten binder completes the granulation process. Melt granulation is advantageous over wet granulation as organic or aqueous solvents are not required for this technique, hence it eliminates the solvent recovery process to protect environment. The absence of solvent as such excludes the wetting and drying steps, which makes the entire process less time- and energy-consuming. This method can be used to enhance the stability of moisture sensitive drug and to improve the poor physical properties of the drug [35].
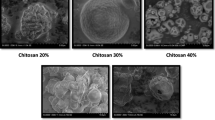
Similar particle size of drug and excipients (except Aerosil) was selected to avoid mixing problems. The initial trial batch TR0 was prepared by the direction compression method to check the suitability of this most economical tablet production method, but because of the failure of this method to produce tablets of desired properties, tablets of all other batches were prepared by the melt granulation technique. Table 2 shows the pre- and post-compression parameters for all the trial batches.
The angle of repose, measured by fixed funnel method, and % Carr’s index, which was calculated based on the difference of bulk density and tapped density, were observed in a range that indicated the acceptable flowability and hence the suitability of the powder blend for the compression. Granules of 16–22# size were selected as the uniform-size granules in the formulation excludes the effect of size-dependent surface area on drug release. The bulk volume of this size range was found appropriate to fill die cavities during compression. The drug release retardation was found more with this size range than that observed with smaller size granules [36, 37]. The capsule shape of a mini-tablet and an average weight of 100 mg per mini-caplet was selected to accommodate a high amount of bulky drug FA [34, 38]. The effect of formulation excipients was checked by keeping the thickness of the mini-caplets of all the batches in a fixed range to avoid the effect of compression force variability on the porosity and, hence, the floatability of the mini-caplets of similar weight. Floating of the trial formulations was achieved at the specified thickness of 4.6 ± 0.2 mm and hence selected for all formulation batches [39]. The TR1 batch was prepared by the melt granulation method to study its effect on the drug release. Precirol may provide a lubricant effect due to its lipidic nature; Aerosil as a lubricant was excluded from the formulation. The TR1 batch exhibited an excellent flow due to the granular structure of the formulation blend. As the formulation of TR2 contained only two excipients, Precirol, and PVP K-30, lactose was added as a diluent to understand the effect of concentration of these excipients and further optimization.
Based on the post-compression data of trial batches, the Batch TR11 formulation, which yielded prolonged drug release for 12 h, was considered for further optimization. The concentration of two formulation factors was varied at three different levels for the optimization as per the 32 full factorial Design of experiment. PVP K-30 was varied at 7.5, 10, and 12.5% and Precirol at 40, 42.5, and 45% concentration. FA was kept constant at 42.5% in each standard experimental run formulation, and lactose was sufficient to make 100% of the formulation blend of F1 to F9 as per Table 3, which also shows values of post-compression parameters of these batches. All experiments were performed in triplicate and presented as mean ± SD.
Evaluation parameters of FA mini-caplets
Weight variation and % friability loss
The post-compression parameters were evaluated per the Indian Pharmacopoeia 2022 specified limits of ± 7.5% deviation to mean for weight variation and less than 1% loss for % friability loss [36, 37]. All the batches passed these criteria.
Drug content
The % drug content was calculated using the regression equation of absorbance (y) vs concentration (x) as y = 0.0193x + 0.0019. This equation was generated from the standard calibration of FA in 0.1N HCl. Drug content was found within ± 5%SD for all the batches and considered acceptable.
In vitro drug release
TR0 batch, based on the mean % CDR ± SD found as 65.4 ± 2.1 at 1 h and 71.2 ± 3.5 at 2 h, respectively, failed to sustain the in vitro drug release. The TR1 batch showed in vitro drug release of 35.2 ± 1.7 at 1 h and 46.3 ± 2.1 at 2 h, indicating sustained drug release compared to the TR0 batch, which may be attributed to slow diffusion of drug molecules from the solidified drug-Precirol lipid matrix [20, 21, 40]. Based on these observations, melt granulation was selected for the rest of the batches. Figure 2 compares % CDR data of trial batches TR1 to TR12.
The comparative evaluation of in vitro % CDR of batch TR1 to TR12 indicated Precirol and PVP K-30 as important formulation factors that affected the drug release. As per Fig. 2(a) and (b), decreased Precirol and increased hydrophilic drug, increased drug release (comparison of TR3 with TR1 and TR2), and it may be due to the lowering of matrix effect of low lipid on high drug content. Adding different grades or concentrations of hydrophilic and swellable polymer HPMC (comparison of TR2 with TR4 to TR7) could not sustain the drug release, possibly due to the higher permeability of dissolution medium in the dosage form. The addition of low permeable Eudragit RSPO (batch TR8) could not sustain drug release, which may be due to its effect on lowering the matrix effect of Precirol on the drug in its presence.
As per Fig. 2(b), the binder, PVP K-30, in optimum amount retarded the drug release, but low (due to less binding effect) and high concentrations (higher permeability due to its hydrophilicity) increased drug release (comparison of TR1 with TR2, and TR10 with TR11 and TR12). The comparison of TR9 containing higher Precirol and TR10 with lower drug amounts indicated a similar and more reduced drug release profile over TR2, which led to the selection of the drug concentration at 42.5% in the formulation.
The % CDR profiles of F1 to F9 runs, displayed in Fig. 3(a), were compared, and observations confirmed the findings of trial batches.
It was found that at a fixed concentration of PVP K-30 an increased concentration of Precirol retarded the drug release, and at a fixed concentration of Precirol, drug release was more in batches with lower and higher concentrations of PVP K-30, compared to batches with 10% which is median concentration. The combined effect of these formulation factors was also reflected in a similar way for the standard experimental run F6 (with + 1 Precirol and 0 PVP K-30 levels), which sustained the drug release for the highest 12 h, whereas F7 (with -1 Precirol and + 1 PVP K-30 levels) with lowest for 7 h, and F1 (with -1 Precirol and -1 PVP K-30 levels) for 9 h. The % CDR at 1 h and 5 h were found and considered as two significantly affected response variables as the desired drug release at these time points could be effectively correlated with other time points. The standard experimental run F6 floating mini-caplets were found with the desired range of 30 to 35% CDR at 1 h, 65 to 70% CDR at 5 h, and prolonged release up to 12 h.
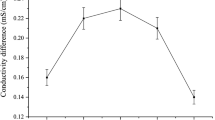
Floating lag time and floating duration
The floating lag time observed in the TR3 batch, which contained 30% Precirol, was higher than the other batches, which indicated that the low concentration of low-density Precirol did not result in an instant floatation of the mini-caplets. All the batches except TR3 were floated instantly (Zero lag time) and indicated that the concentration range of the formulation ingredients in these batches did not affect floating behaviour. Figure 3(b) depicts the floating behaviour of Std run F6. All the trial and F1 to F9 standard run batches floated throughout the in vitro drug release study.
Based on the post-compression data of F1 to F9 standard runs, the F6 run was found with all the parameters in the desired range. It was considered the optimized formulation batch for further drug release kinetic, accelerated stability study, and in vivo bioavailability study in female rabbits.
Drug release kinetic
The mechanism and kinetics of drug release from the dosage form can be understood by fitting the drug release profile data into various models. Figure 3(c) indicated the Korsmeyer Peppas as the best-fit model for the % CDR of Std run F6, based on R2 = 0.999. The observed value of exponent n (0.444) < 0.5 confirmed the diffusion mechanism of drug release from the lipid matrix [41].
Statistical analysis
The ANOVA and fit statistics data suggested the quadratic model used was significant for the response variable R1-CDR at 1 h without transformation and R2 -CDR at 5 h data after response transformation to ‘Base 10 log’. The data also confirmed the model’s ability to navigate the design space for both response variables. The regression analysis of the data generated polynomial equations for the % CDR at 1 h as R1 = 36.27–3.68A-1.65AB + 7.65 B2 and for the Log10 (% CDR at 5 h) as R2 = 1.85–0.0305A-0.0219AB + 0.0361 B2, where A and B represent Precirol and PVP K-30 concentration respectively. The higher and negative coefficient value of Precirol alone and in combination with PVP K-30 proved their release retarding effect, whereas a higher and positive value of quadratic term for PVP K-30 concentration indicated its effect on increased drug release. These equations would help decide the concentration of the formulation factors to get any desired response variable value [42].
Statistical analysis of input experimental data of formulation composition of F1 to F9 and R1 (% CDR at 1 h) and R2 (The % CDR at 5 h) generated 3D curves and overlay graph. 3D response surface curves indicated the effect of Precirol and PVP K-30 on response variable R1 as per Fig. 4(a) and on R2 as per Fig. 4(b). Figure 4(c) Shows the overlay plot with design space (yellow region), generated for the range of Precirol and PVP K-30 concentration used in the formulations to get values of R1 as 30 to 35%, and R2 as 65 to 70%. The design space region [43] suggested a optimization batch with same formulation as of Std run F6 which was prepared, and its evaluation data on R1 = 33.9 ± 1.8 and R2 = 67.8 ± 2.6 were similar to the predicted values of R1 = 31.7 and R2 = 66.6 predicted by the software and that validated the model used for the formulation optimization.
Statistical analysis of standard run F1 to F9 (a) 3D response surface curve of the effect of formulation factors on response variable R1-% CDR at 1 h (b) 3D response surface curve of the effect of formulation factors on response variable R2- % CDR at 5 h (c) Overlay plot of formulation factors for the desired response variables (d) Comparison of in vitro drug release profiles of standard experimental run F6, found before and after three months storage of accelerated stability study
Comparison of in vitro drug release of Std run F6 mini-caplets with IR FA tablets
The cumulative in vitro drug release from floating SR FA mini-caplets in Std run 6 (optimized batch) and from immediate-release FA tablets was found as per Table 4. The drug content of the immediate-release FA tablet was analyzed and found to be 100 ± 3.1%.
The IR FA tablet immediately sank to the bottom of the dissolution medium flasks and released 100% drug within 2 h, whereas the Std run F6 mini-caplets floated immediately in the dissolution media and sustained the drug release for up to 12 h. The floating and drug release behaviour of the floating SR FA formulation was the result of the formulation composition, which contained Precirol and PVP K-30 in a certain amount. The floating and sustained drug-release iron formulation would enhance its bioavailability compared to the IR iron formulation.
Accelerated stability study
Evaluation data of Std run F6 mini-caplets were compared before and after three months of storage under the experimental conditions as per ICH guidelines. The mean ± SD of weight variation, % friability, % drug content, and floating lag time were 96 ± 3, 0.2, 98 ± 3, and zero, respectively, before storage and 96 ± 3, 0.2, 96 ± 2, and zero after storage. Before and after storage, mini-caplets floated throughout the in vitro drug release study. Figure 4(d) compared graphically the in vitro drug release profiles obtained before and after storage and indicated no significant changes. Based on the no or non-significant changes in the values of these parameters, standard experimental run F6 was found stable for three months, stored in an airtight HDPE bottle, at 40 °C ± 2 °C temperature and 75 ± 5% RH.
In vivo study
Rabbits were used to study the effect of the developed formulation in vivo as the rabbit intestine behaviour matched that of human duodenal mucosa for iron absorption [44,45,46]. Rabbit size was suitable for the mini-caplet study. Iron absorption was studied by serum iron and UIBC levels. Increased serum iron levels may be observed after iron administration. UIBC measures unoccupied binding sites on transferrin as the difference between TIBC-total iron-binding capacity (the maximum concentration of iron that can bind to transferrin) and serum iron [29].
As shown in Fig. 5(a), the mean serum iron level in the control, standard, and test groups was found to be 96.33 µg/dL, 105.33 µg/dL, and 114 µg/dL, respectively, with no statistical significance at 0 h. At 3, 6, and 12 h post-dosing, serum iron in the test group (149 µg/dL, 167 µg/dL, 181.33 respectively) was higher compared to control (104 µg/dL, 97.66 µg/dL, 90.33 µg/dL respectively) with significant difference (p < 0.01). At 12 h, serum iron was higher in the test group (181.33 µg/dL) compared to the standard group (115.33 µg/dL) with a significant difference (p < 0.01). The Area Under Curve (AUC) of the test was significantly higher compared to the control and standard (Fig. 5(b)).
Effect of different formulations on (a) Serum iron at different time intervals (b) AUC of serum iron (0–12 h) (c) Unsaturated Iron Binding Capacity (UIBC) at different time intervals (d) AUC of UIBC (0–12 h) (For serum iron and UIBC, analysis was done by Two way ANOVA, and for AUC of serum iron and UIBC, analysis was done by One way ANOVA, followed by post-hoc comparison by Tukey’s test. *p < 0.05; **p < 0.01; ***p < 0.001 vs Control; $p < 0.05; $$p < 0.01 vs standard)
As shown in Fig. 5(c), UIBC of the standard was lower compared to control at 6 and 12 h post formulation with a significant difference (p < 0.05). UIBC of the test was significantly low compared to the control and standard at all time points post-treatment (p < 0.01). As shown in Fig. 5(d), the AUC of the test was significantly low compared to the control and standard. For the in-vivo study, we used a female New Zealand white rabbit [47]. Three animals were kept per group based on the power of the study [48].
The increased serum iron level and decreased UIBC of the test compared to the standard indicate that the overall iron absorption from the test (non-effervescent floating FA mini-caplets) was significantly higher than the standard (immediate release formulation).
To predict the clinical benefit of the test formulations over standard reference formulation, the relative bioavailability (the rate and extent of drug absorption) is considered [49].
Mean AUC Serum iron for test (floating FA SR mini-caplet formulation, Std run F6 batch) and standard (IR FA tablet) was observed as 1914 ± 66.3 and 1496 ± 49.9 respectively. Based on these values, % relative bioavailability of test was 28% higher than standard formulation.
The higher absorption of iron may be attributed to the retention of the test formulation in the stomach due to floating behaviour, which released fractional iron, available for absorption at the duodenum without carrier saturation. The sustained release of iron from the test may also reduce side effects associated with IR iron preparations [17, 50].
Conclusion
From the results of the present study, we conclude that the formulation (Std run F6) of non-effervescent floating FA mini-caplets is an optimized formulation based on desired in vitro post-compression parameters, stability study and in-vivo data. Compared to the IR formulation, the improved iron bioavailability of the optimized formulation may be attributed to the release of iron from the dosage form at its absorption site for a prolonged period due to retention in the gastric region. It may also reduce gastrointestinal side effects due to fractional drug release and improved utilization of the iron dose. Nevertheless, effect of the formulation on other iron biomarkers in diet-induced iron-deficient animal models may support clinical application of the developed formulation.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Muñoz M, García-Erce JA, Remacha ÁF. Disorders of iron metabolism. Part 1: Molecular basis of iron homoeostasis. J Clin Pathol. 2011;64:281–6.
Meynard D, Babitt JL, Lin HY. The liver : conductor of systemic iron balance. Blood J Am Soc Hematol. 2014;123(2):168–76.
Organization WH. Nutritional Anaemias : Tools for Effective Prevention. Organization WH, editor. WHO Document Production Services, Geneva, Switzerland; 2017.
Fuqua BK, Vulpe CD, Anderson GJ. Intestinal iron absorption. J Trace Elem Med Biol. 2012;26:115–9. https://doi.org/10.1016/j.jtemb.2012.03.015.
Al-naseem AA, Sallam AA, Choudhury S, Thachil J. Iron deficiency without anaemia : a diagnosis that matters. Clin Med. 2021;21:107–13.
Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123:615–24.
Serati M, Torella M. Preventing complications by persistence with iron replacement therapy: a comprehensive literature review. Curr Med Res Opin. 2019;35:1065–72. https://doi.org/10.1080/03007995.2018.1552850.
Stoffel NU, Cercamondi CI, Brittenham G, Zeder C, Geurts-moespot AJ, Swinkels DW, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women : two open-label, randomised controlled trials. Lancet Haematol. 2017;4:e524-33. https://doi.org/10.1016/S2352-3026(17)30182-5.
Santiago P. Ferrous versus ferric oral iron formulations for the treatment of iron deficiency: A clinical overview. Sci World J. 2012;2012:846824.
Pasricha SR, Tye-Din J, Muckenthaler MU, Swinkels DW. Iron deficiency. Lancet. 2021;397:233–48. https://doi.org/10.1016/S0140-6736(20)32594-0.
Malhotra N, Kriplani A, Pal B, Bhat V, Swami O. Ferrous ascorbate: Current clinical place of therapy in the management of iron deficiency anemia. J SAFOG. 2021;13:99–105.
Gupta DN, Gupta DR, Jahan DU, Bais DA. Comparative study of different oral iron preparations in Gynecological and postnatal patients. Int J Clin Obstet Gynaecol. 2020;4:330–2.
Pavord S, Daru J, Prasannan N, Robinson S, Stanworth S, Girling J. UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol. 2020;188:819–30.
Kumar A, Brookes MJ. Iron therapy in inflammatory bowel disease. Nutrients. 2020;12:1–14.
Kumar M, Kaushik D. An Overview on Various Approaches and Recent Patents on Gastroretentive Drug Delivery Systems. Recent Pat Drug Deliv Formul. 2018;12:84–92.
Singh BN, Kim KH. Floating drug delivery systems : an approach to oral controlled drug delivery via gastric retention. 2000;63:235–59.
Singh K, Jain SK, Razdan K, Singh H, Sahajpal NS, Singh H, et al. Formulation and Evaluation of Ferrous Ascorbate Floating Tablets for the Treatment of Anaemia. Drug Deliv Lett. 2019;9:299–307.
Pendse B, Sawarkar S, Damani M. 2021 Design and Development of a Novel Gastroretentive Multiunit Particulate System and Colon Targeted Tablet in Capsule System for Effective Management of Anaemia. Int J Pharm Sci Res 12 2628–40. https://doi.org/10.13040/IJPSR.0975-8232.12
Tawfeek HM, Saleem IY, Roberts M. Dissolution Enhancement and Formulation of Rapid-Release Lornoxicam Mini-Tablets. 2014;103:2470–83.
Goole J, Van GB, Pilcer G, Deleuze P, Blocklet D. Pharmacoscintigraphic and pharmacokinetic evaluation on healthy human volunteers of sustained-release floating minitablets containing levodopa and carbidopa. Int J Pharm. 2008;364:54–63.
Panda M, Rao MEB, Patra CN, Panda J, Panigrahi KC, Patro G. Formulation and development of floating multiple-unit minitablets of Nimodipine without using a gas-generating agent : in vitro and in vivo characterization. Futur J Pharm Sci. 2020;6:1–9.
Pharmaceutical Methods. Indian Pharmacopoeia. Ghaziabad: The Indian Pharmacopoeia Commission; 2007 177–82
Rao KV, Venkatchalam VV. Mucoadhesive biphasic minitablets of cefuroxime axetil: Formulation development, characterization and in vivo bioavailability study. J Drug Deliv Sci Technol. 2016;35:260–71. https://doi.org/10.1016/j.jddst.2016.07.003.
International Conference on Harmonization (ICH). Guidance for industry: Q1A(R2) Stability testing of new drug substances and products. ICH Q1A(R2). 2003 p. 24.
Kheiri R, Koohi MK, Sadeghi-Hashjin G, Nouri H, Khezli N, Hassan MA, et al. Comparison of the effects of iron oxide, as a new form of iron supplement, and ferrous sulfate on the blood levels of iron and total iron-binding globulin in the rabbit. Iran J Med Sci. 2017;42:79–84.
Ali Seif El-Nasr I, Abdmoneim Mahmoud S, Mahmoud Elnaddar E, Ali Ammar H. Ferrous sulphate alone versus combination of ferrous sulphate and lactoferrin for the treatment of iron deficiency anemia during pregnancy and their effect on neonatal iron stores: a randomized clinical trial. Egypt J Hosp Med. 2021;84:1955–60.
Gringras M. A Comparison of Two Combined Iron-Folic Acid Preparations in the Prevention of Anaemia in Pregnancy. J Int Med Res. 1982;10:268–70.
Nair A, Jacob S. A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm. 2016;7:27.
Kundrapu S, Noguez J. Laboratory Assessment of Anemia . 1st ed. Adv. Clin. Chem. Elsevier Inc.; 2018. https://doi.org/10.1016/bs.acc.2017.10.006
Tian XL, Tian DF, Wang ZY, Mo FK. Synthesis and evaluation of chitosan-Vitamin C complex. Indian J Pharm Sci. 2009;71:371–6.
Dave VS, Haware RV, Sangave NA, Sayles M, Popielarczyk M. Drug-Excipient Compatibility Studies in Formulation Development : Current Trends and Techniques. Am Assoc Pharm Sci. 2015;2015:9–15.
Rodig OR. Spectrometric Identification of Organic Compounds. J Chem Educ. 1963;39(11):546.
Patil S, Talele GS. Gastroretentive mucoadhesive tablet of lafutidine for controlled release and enhanced bioavailability. Drug Deliv. 2015;22:312–9.
Jaiswar DR, Amin PD. Solid-state characterization of ferrous ascorbate. Int J Pharm Pharm Sci. 2012;4:282–7.
Mashinchian O, Johari-Ahar M, Ghaemi B, Rashidi M, Barar J, Omidi Y. Impacts of quantum dots in molecular detection and bioimaging of cancer. BioImpacts. 2014;4:149–66.
Sg H, Suresh S, Asadulla S. Formulation and Evaluation of Colon Specific Drug Delivery Systems of Selected Anti-Inflammatory Agent. Int J Res Pharm Chem. 2012;2:513–22.
El-Zahaby SA, Kassem AA, El-Kamel AH. Design and evaluation of gastroretentive levofloxacin floating mini-tablets-in-capsule system for eradication of Helicobacter pylori. Saudi Pharm J. 2014;22:570–9. https://doi.org/10.1016/j.jsps.2014.02.009.
Yohannes B, Abebe A. Determination of tensile strength of shaped tablets. Powder Technol. 2021;383:11–8. https://doi.org/10.1016/j.powtec.2021.01.014.
Manley L, Hilden J, Valero P, Kramer T. Tablet Compression Force as a Process Analytical Technology (PAT): 100% Inspection and Control of Tablet Weight Uniformity. J Pharm Sci. 2019;108:485–93. https://doi.org/10.1016/j.xphs.2018.07.004.
Patel DM, Patel NM, Patel VF, Bhatt DA. Floating granules of ranitidine hydrochloride-gelucire 43/01: Formulation optimization using factorial design. AAPS PharmSciTech. 2007;8:E24–31.
Hayashi T, Kanbe H, Okada M, Suzuki M, Ikeda Y, Onuki Y, et al. Formulation study and drug release mechanism of a new theophylline sustained-release preparation. Int J Pharm. 2005;304:91–101.
Thomas L, Viswanad V. Formulation and optimization of clotrimazole-loaded proniosomal gel using 3 2 factorial design. Sci Pharm. 2012;80:731–48.
Kan S, Lu J, Liu J, Wang J, Zhao Y. A quality by design (QbD) case study on enteric-coated pellets: Screening of critical variables and establishment of design space at laboratory scale. Asian J Pharm Sci. 2014;9:268–78. https://doi.org/10.1016/j.ajps.2014.07.005.
Cox TM, O’Donnell MW. Studies on the control of iron uptake by rabbit small intestine. Br J Nutr. 1982;47:251–8.
Hosny KM. Solid lipid nanoparticles loaded with iron to overcome barriers for treatment of iron deficiency anemia. Drug Des Dev Ther. 2015;9:313–20.
Dabbagh AJ, Shwaery GT, Keaney JF, Frei B. Effect of Iron Overload and Iron Deficiency on Atherosclerosis in the Hypercholesterolemic Rabbit. Arterioscler Thromb Vasc Biol. 1997;17(11):2638–45.
Bergström E, Hernell O, Lönnerdal B, Persson LA. Sex differences in iron stores of adolescents: what is normal? J Pediatr Gastroenterol Nutr. 1995;20:215–24.
Percie du Sert N, Bamsey I, Bate ST, Berdoy M, Clark RA, Cuthill I, et al. The Experimental Design Assistant. PLoS Biol. 2017;15:e2003779.
D.M. Brahmankar and S.B. Jaiswal. 2015 Biopharmaceutics and Pharmacokinetics-A TREATISE. Third. Delhi: Vallabh Prakashan; 2015.
Cook JD, Carriaga M, Skikne BS, Kahn SG, Schalch W. Gastric delivery system for iron supplementation. Lancet. 1990;335:1136–9.
Acknowledgements
The authors would like to acknowledge Colorcon Asia Pvt. Ltd., India, and Gattefosse India Pvt. Ltd. for gift samples.
Funding
The authors declare that grant for procurement of chemicals and characterization of formulations was received from L J University.
Author information
Authors and Affiliations
Contributions
The author Shital Trivedi reviewed literature, performed experimental work, study design and optimization, data analysis, data interpretation, writing and editing of manuscript; author Vijay Kevlani contributed in animal handling, data interpretation, and final editing, and corresponding author Shreeraj Shah provided supervision and critical review of the initial draft.
Corresponding author
Ethics declarations
Consent for publication
The authors declare that any individual person’s data in any form (including any individual details, images or videos) was not utilized during the manuscript preparation.
Research involving animals
The animal study was approved on Oct 10, 2022, by the Institutional Animal Ethics Committee, L.J. Institute of Pharmacy (Protocol number: LJIP/IAEC/2022–23/04). Animal care and handling were per the Committee for Control and Supervision of Experiments on Animals (CCSEA) guidelines.
Conflict of interest
All the authors (Shital Trivedi, Shreeraj Shah, Vijay Kevlani) declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Trivedi, S., Kevlani, V. & Shah, S. Ferrous ascorbate non-effervescent floating mini-caplets as an oral iron supplement. Drug Deliv. and Transl. Res. (2024). https://doi.org/10.1007/s13346-024-01691-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s13346-024-01691-x