Abstract
Hydrogels are promising ultrasound-responsive drug delivery systems. In this study, we investigated how different ultrasound parameters affected drug release and structural integrity of self-healing hydrogels composed of alginate or poloxamers. The effects of amplitude and duty cycle at low frequency (24 kHz) ultrasound stimulation were first investigated using alginate hydrogels at 2% w/v and 2.5% w/v. Increasing ultrasound amplitude increased drug release from these gels, although high amplitudes caused large variations in release and damaged the gel structure. Increasing duty cycle also increased drug release, although a threshold was observed with the lower pulsed 50% duty cycle achieving similar levels of drug release to a continuous 100% duty cycle. Poloxamer-based hydrogels were also responsive to the optimised parameters at low frequency (24 kHz, 20% amplitude, 50% duty cycle for 30 s) and showed similar drug release results to a 2.5% w/v alginate hydrogel. Weight loss studies demonstrated that the 2% w/v alginate hydrogel underwent significant erosion following ultrasound application, whereas the 2.5% w/v alginate and the poloxamer gels were unaffected by application of the same parameters (24 kHz, 20% amplitude, 50% duty cycle for 30 s). The rheological properties of the hydrogels were also unaffected and the FTIR spectra remained unchanged after low frequency ultrasound stimulation (24 kHz, 20% amplitude, 50% duty cycle for 30 s). Finally, high-frequency ultrasound stimulation (1 MHz, 3 W.cm−2, 50% duty cycle) was also trialled; the alginate gels were less responsive to this frequency, while no statistically significant impact on drug release was observed from the poloxamer gels. This study demonstrates the importance of ultrasound parameters and polymer selection in designing ultrasound-responsive hydrogels.
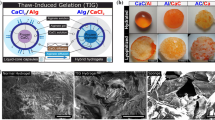
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Development of stimuli-responsive drug delivery systems to provide on-demand release remains at the forefront of pharmaceutical research. An ideal formulation of this nature will demonstrate controlled drug release rates at baseline which can be increased when required upon exposure to a stimulus. Such tunable release has been of particular interest in conditions that require frequent dosing over a long treatment period such as chronic pain, diabetes and tissue repair [1].
While on-demand drug release is possible using various stimuli and delivery platforms [2], a particularly encouraging approach has been the combination of ultrasound with hydrogels. Ultrasound, which uses sound waves above the audible range for humans (> 20 kHz), has seen widespread use on the human body for both diagnostic and therapeutic applications and has been demonstrated as safe for clinical use [3]. Hydrogels, which comprise a chemically or physically crosslinked polymer network with high water content (between 70 and 99%), are physicochemically and mechanically similar to biological tissue and have thus shown high biocompatibility [4, 5] and have seen interest as platforms for on-demand release.
Drug release from hydrogels typically occurs at a slow and sustained rate due to the tortuous network structure and high viscosity of the formulation [6]. When ultrasound is applied to hydrogels, the stimulus is thought to disrupt the network structure by cavitation, the formation and destruction of gas filled bubbles within the hydrogel, and thereby increase the size of pores in hydrogels leading to drug release [7, 8]. Another theory suggests that the thermal effects of ultrasound stimulation lead to a temperature-induced disturbance of the gel by changing its rheological properties. This change can lead to pore size increases resulting in increased drug release. A variety of hydrogels have been investigated for ultrasound-triggered drug release [2, 7]. Certain preparations have been more extensively investigated owing to their ability to rapidly self-heal following removal of ultrasound.
Alginate and poloxamer hydrogels have the potential for self-healing [9, 10]. Negatively charged alginate polymer backbones build ionic interactions with divalent cations, in our case calcium cations, to form and reform a hydrogel, and have demonstrated ultrasound responsiveness at polymer concentrations ranging from 1 to 4% w/v. Thus far, alginate hydrogels have been used for ultrasound-stimulated delivery of small molecules [9], macromolecules [11], and nanoparticles [12]. However, it remains unclear whether ultrasound application has any long-term effects on the rheological properties of these gels, potentially leading to faster biodegradation of the gel, which would be a crucial determinant in the clinical utility of this platform.
Poloxamer, similar to alginate, has the ability to reversibly assemble into hydrogels without forming covalent bonds [10]. In contrast to alginate, poloxamer gels due to the formation of spherical micelles and the dehydration of the core of the micelles above a certain temperature [10]. Poloxamer gels are, therefore, temperature-responsive and have shown the ability to achieve sustained drug release in vitro [13]. The non-ionic polymers consist of a hydrophobic core block (poly(propylene oxide), PPO) and two hydrophilic terminal blocks (poly (ethylene oxide), PEO) and different types of poloxamer can have different ratios of these blocks, which alters their hydrophilicity [10]. Among commonly used varieties, poloxamer 188 is a more hydrophilic poloxamer and can, therefore, incorporate larger quantities of small hydrophilic drugs like ibuprofen, while poloxamer 407 is more hydrophobic but is associated with more sustained release and less erosion of the hydrogel. The combination of these two poloxamers has shown to achieve high drug loading, reduced burst release and sustained release of small hydrophilic drugs in vivo [13]. These gels are not commonly investigated for ultrasound-stimulated release but might be an attractive option due to their excellent biocompatibility and ease of injectability [14].
Ultrasound is a highly tunable stimulus and ultrasound-triggered drug release has been observed at a variety of frequencies (number of waves per second) ranging from kHz to MHz [9, 15]. Low-frequency ultrasound stimulation (LFUS) in the kHz range (< 100 kHz) has been extensively used for transdermal drug delivery [3, 16] and is generally associated with significant drug release after ultrasound stimulation [3, 9]. However, at high intensities, it can lead to cell membrane disruption and cell death [3, 8]. High-frequency ultrasound stimulation (HFUS, ≥ 1 MHz) has been used since the 1950s and has Food and Drug Administration (FDA) approval to be used for hyperthermia, cancer therapy and bone fracture healing [17]. It has also been used to achieve drug delivery to the brain [3] but has its own risks when used at high intensities as it can lead to tissue heating and burns [17]. A hydrogel that is responsive to either low or high frequencies would be advantageous for widespread use across applications. The optimal frequency range to achieve ultrasound-triggered release in a clinical setting has not yet been determined. Other parameters such as amplitude (pressure range exerted by the stimulus), duty cycle (proportion of time the stimulus is on), and duration of administration are also routinely varied to optimise drug delivery while maintaining safety of the technique [3, 11, 18,19,20]. Thus, it is important to establish which frequency can achieve drug release and how the modulation of other ultrasonic parameters may affect drug release and gel structure.
In this study, we evaluated how alginate and poloxamer hydrogels behaved when exposed to different ultrasonic frequencies, amplitudes/intensities and duty cycles. The effect of varying these ultrasound parameters on release of the model drug ibuprofen hydrochloride was studied, and any lasting structural changes were determined.
Materials and methods
Materials
Sodium alginate powder, ibuprofen sodium salt, poloxamer 407 (Pluronic® F-127) and poloxamer 188 (Kolliphor® P 188) were purchased from Sigma Aldrich (St Louis, MO, USA). Phosphate-buffered saline (PBS) tablets were purchased from VWR International (Radnor, PA, USA). Ethanol 99.5% was obtained from ECP Labchem (Auckland, NZ). Calcium chloride was purchased from Merck (Darmstadt, Germany), NaCl from Scharlau (Sentmenat, Spain) and Milli-Q water was obtained from a CFOF01205 Milli-Q water purification system made by Millipore (Burlington, MA, USA).
Preparation of gels
Alginate
To make 2 mL of a calcium-crosslinked hydrogel, sodium alginate was first dissolved in PBS (pH 7.4). Next, 0.8 mL of this solution was mixed with 0.8 mL of 0.25% w/v ibuprofen hydrochloride solution. Eight aliquots (0.05 mL) of a 1.05% w/v calcium chloride solution were added to each 1.6 mL solution of alginate and ibuprofen over 1 min, while the mixture was being vortexed using a Talboys Advanced Vortex Mixer (Troemner, Thorofare, NJ, USA) at 2500 rpm. The addition of each aliquot was followed by 8 s of vortex mixing. The gel mixture was then left to form for 30 min. Hydrogels with final alginate concentrations of 2 and 2.5% w/v were produced using this method. Preparations attempted using higher alginate concentrations faced issues with their homogeneity while those using lower concentrations collapsed under ultrasound stimulation. All tested gels had a final ibuprofen concentration of 0.1% w/v.
Poloxamer
To make poloxamer 188 and 407 hydrogel, a previously described cold stirring method was used [13]. Poloxamer 188 (11% w/w) was first dissolved in Milli-Q water with NaCl (0.4% w/w) by continuous stirring at 4 °C for 2 h. Poloxamer 407 (25% w/w) was then added and left to dissolve under continuous stirring at 4 °C overnight. The hydrogels were loaded with ibuprofen (0.1% w/w), aliquoted by weight into sample tubes, and left to form for 30 min at room temperature.
Porosity of hydrogels
The porosity of the hydrogels was assessed according to a previously described method with modification to gain a better insight into the crosslinking of the gels [21]. In brief, blank hydrogel samples (2 mL of either alginate formulation, 2 g of poloxamer) were prepared, left to gel and then lyophilised (VirTis BenchTop Pro freeze dryer, SP Industries, Warminster, PA, USA). After lyophilisation, the hydrogels were weighed and then placed into 10 mL of ethanol for 24 h. Subsequently, the samples were removed from the ethanol and weighed. The porosity (%) was calculated using the following equation:
W1 represents the weight of the gel after lyophilisation and before immersion in ethanol, W2 is the weight of the gel after immersing in ethanol, ρ is the density of ethanol and V is the volume of ethanol added to the hydrogel.
Interaction between drug and hydrogel
The interactions between drug and hydrogel were studied by Fourier transform infrared (FTIR) spectroscopy using a Bruker Tensor 37 FTIR spectrometer (Billerica, MA, USA), equipped with a MIRacle diamond. Hydrogels were prepared with a 1:1 ratio of polymer to ibuprofen, left to gel and then lyophilised. Samples were scanned 32 times at a resolution of 4 cm−1 from wavenumbers 1800 to 600 cm−1.
Ultrasound administration
Ultrasound stimulation at 24 kHz
The influence of different amplitudes and duty cycles on hydrogels was assessed at low-frequency ultrasound (24 kHz). Hydrogels were stimulated using a Hielscher UP200S ultrasonic processor with a Sonotrode S2 probe (Teltow, Germany) at a frequency of 24 kHz for 30 s with adjusted amplitude (0–100%) and duty cycle (0–100%). A 30-s stimulation period was chosen, as longer periods caused significant structural disruption of the hydrogels. This machine has a maximum power output of 200 W which can be modulated by adjusting the amplitude and duty cycle. The probe was placed in the PBS, 2 cm above the hydrogel surface in 10 mL PBS during stimulation. With this set up, a 100% amplitude was theoretically calculated to have a power output of 18.8 W1. This correlates to an average power output of 5.64 W and 9.4 W at a duty cycle of 30% and 50%, respectively (Table 1). The performance of the hydrogels was tested up to their amplitude and duty cycle thresholds.
Ultrasound stimulation at 1 MHz
After establishing the effect of different amplitudes and duty cycles at LFUS, the effect of a higher frequency (1 MHz) was assessed. A Johari JUS-2 therapeutic ultrasound device (Jodhpur, India) was used to stimulate hydrogels with high frequency ultrasound. The 1 MHz ultrasound was applied at a 50% duty cycle for up to 10 min with an intensity of 3 W.cm−2. A 10-min time period was chosen, as no significant release was detected for shorter stimulations and as pulsed 1 MHz ultrasound stimulation for up to 10 min is commonly used in clinical studies [22]. The longer duration was also promoted to account for the stimulation through less acoustically responsive test tubes [23]. The probe was placed at the bottom of a hydrogel-containing flat bottom tube (Techno Plas, St Marys, SA, Australia). The theoretical power output applied to the bottom of the tube was calculated to be 5.52 W at a 100% duty cycle. At a duty cycle of 50%, the average power applied is, in theory, 2.76 W.
Drug release studies
Ibuprofen-loaded hydrogel samples (2 mL of alginate, 2 g of poloxamer) were prepared directly into sample tubes. Following gel formation, 10 mL PBS was added to the tubes and the tubes were transferred to a Lab Companion BS-31 oscillating water bath (Billerica, MA, USA) set to 100 rpm and 37 °C. Drug release studies were performed over 120 min. At each sample time point, the release media was removed and replaced with fresh PBS (Fig. 1). Samples were taken every 30 min. In samples where ultrasound stimulation was tested, ultrasound protocols as described in the “Ultrasound administration” section were applied immediately after the 30 and 90 min buffer replacement timepoints. A buffer replacement step was performed at 31 and 91 min or 40 and 100 min for the 24 kHz and 1 MHz protocol, respectively. For 1 MHz stimulation, an additional buffer replacement step was performed at 50 min. The 30-min time point for ultrasound stimulation was chosen to avoid the initial burst release phase and the 90-min time point to allow the hydrogel to re-heal before repeated stimulation. The buffer removed at each timepoint had its ibuprofen concentration assayed via UV–visible spectrophotometry at 222 nm. A wavescan of buffer removed from unloaded hydrogel controls of each formulation after 120 min of passive release and LFUS stimulation at 30 and 90 min from 200 to 400 nm was performed and compared to a wavescan of 0.1% w/v ibuprofen in PBS to confirm that no interference from either hydrogel was detected at this wavelength (Suppl. Fig. 1). The complete incorporation of the added ibuprofen (0.1% w/v) was assumed to calculate the drug release percentage.
Mass change assessment
Erosion of hydrogels after LFUS was assessed by measuring the mass of gels undergoing drug release studies at 0 and 120 min (t0 and t120). In the case of the t0 mass, this was measured before addition of any PBS to the vial. In the case of the t120 mass, all excess PBS was removed from the vial and care was taken to ensure only the intact gel mass was measured. The percentage change in mass was calculated using the following equation:
Mass changes of both ultrasound-stimulated and unstimulated gels were recorded.
Impact of LFUS on hydrogel polymers
The impact of LFUS on the hydrogel polymers was assessed using FTIR spectroscopy. Hydrogels without ibuprofen were prepared, left to gel and then lyophilised. Additionally, unloaded gels that had undergone the drug release study protocol, both ultrasound stimulated and unstimulated, were lyophilised and tested. Samples were scanned 32 times at a resolution of 4 cm−1 from wavenumbers 1800 to 600 cm−1 using a Bruker Tensor 37 FTIR spectrometer, equipped with a MIRacle diamond.
Viscosity assessment
To investigate the effect of LFUS on hydrogel structure, rheological measurements were performed using a TA Discovery HR-2 oscillatory rheometer (New Castle, DE, USA) with a 20-mm parallel plate. Gels that had undergone drug release studies, both ultrasound stimulated and unstimulated, were tested. The viscosities at a 2 s−1 shear rate of each gel sample were recorded.
Self-healing hydrogel properties
The self-healing properties of unloaded hydrogels before and after 120 min of release with or without LFUS were assessed by performing frequency sweeps using a TA Discovery HR-2 oscillatory rheometer with a 20-mm parallel plate. Gel samples were tested before and after drug release studies, ultrasound stimulated and unstimulated. The frequency sweep was performed with 2% strain and angular frequencies from 0.1 to 100 rad/s at 37 °C.
Statistical analysis
All experiments were performed as n ≥ 3 with data presented as mean ± SEM. Data was analysed in the GraphPad prism using two-tailed unpaired t-tests with significance determined if a p-value < 0.05 was returned.
Results
Porosity of hydrogels
The porosity of the different hydrogels was assessed to gain insight into the crosslinking of the hydrogels. The 2% and 2.5% w/v alginate hydrogels showed an average porosity of 12.1 ± 0.6% and 12.2 ± 0.4%, respectively. Poloxamer hydrogel showed an average porosity of 17.6 ± 3.7%. However, the difference between the porosities of any of the hydrogels was not statistically significant (p > 0.05).
Ibuprofen and hydrogel polymer interactions
To study the interactions of ibuprofen with the hydrogel polymers, FTIR spectra were collected from hydrogels without ibuprofen, from 1:1 ibuprofen-loaded hydrogels and from pure ibuprofen (Fig. 2). Calcium-crosslinked alginate hydrogel showed peaks at 1601 cm−1 (C-O stretching, asymmetric stretching), 1412 cm−1 (C-O stretching, symmetric stretching) and 1028 cm−1 (C-O stretching), which could also be observed in the ibuprofen-loaded hydrogels (Fig. 2a). Ibuprofen showed peaks at 1407 cm−1 (C-C aromatic) and 1545 cm−1 (COO− carboxylate anion) of which the 1407 cm−1 peak was merged with the 1412 cm−1 peak of alginate in the combined sample. In the drug-loaded hydrogel, the ibuprofen peak at 1545 cm−1 had shifted with a peak present at 1585 cm−1 with a shoulder at 1607 cm−1, suggesting a chemical interaction between alginate and ibuprofen.
Stacked and scaled FTIR transmittance spectra for a alginate, 1:1 loaded ibuprofen alginate hydrogel and ibuprofen and b the different types of poloxamer, 1:1 ibuprofen poloxamer hydrogel and ibuprofen. Spectra were detected from 600 to 1800 cm−1. Hydrogel and ibuprofen peaks are indicated with dashed lines. Ibuprofen peak shifts were observed in both hydrogels
For poloxamer hydrogel, peaks at 1343 cm−1 (O–H bend) and 1100 cm−1 (C-O stretch) could be observed in the different types of polymers as well as the ibuprofen-loaded hydrogel (Fig. 2b). Ibuprofen peaks at 1407 cm−1 (C-C aromatic) could be observed in the ibuprofen-loaded sample, while the 1545 cm−1 (COO− carboxylate anion) ibuprofen peak shifted to a higher wavenumber, indicating the interaction between the poloxamers and ibuprofen.
Effect of amplitude and duty cycle on low frequency ultrasound-stimulated release from alginate hydrogels (24 kHz)
Ibuprofen-loaded hydrogels were first exposed to ultrasound at a fixed duty cycle of 50% with amplitudes varied to 20%, 60% and 100% to establish the effect of different amplitudes on ultrasound-stimulated release. All the ultrasound amplitudes tested resulted in increasing rates of ibuprofen release when compared to no stimulation (Fig. 3).
Ibuprofen release after ultrasound stimulation at different amplitudes from a 2% w/v and b 2.5% w/v alginate hydrogels. Samples were subjected to a 30-s ultrasound pulse at the 30 and 90 min timepoints (indicated by an upwards arrow under the x-axis) at a frequency of 24 kHz, fixed duty cycle of 50%, and varied amplitudes of 20, 60 and 100%. Significance is shown where release at the 120 min timepoint is greater than that of no stimulation (*p < 0.05, **p < 0.01) and greater than that of the 20% amplitude (†p < 0.05). Error bars refer to ± SEM of three measurements
Stimulated drug release from both the 2% and 2.5% w/v alginate gels increased as the ultrasound amplitude was increased further. After 120 min, all tested ultrasound protocols had experienced greater drug release than the unstimulated control for either hydrogel (Fig. 3). Increasing amplitude increased the variability in drug release. Therefore, no significant difference could be observed in total drug release when different amplitudes were applied for the 2.5% w/v gel (Fig. 3b). In contrast, for the 2% w/v gel, the 100% amplitude was observed to release significantly more drug than the 20% amplitude (Fig. 3a, p < 0.05). At both alginate concentrations, the 100% amplitude visibly caused some degree of gel erosion. Due to the large variability in release with the higher amplitudes, only the 20% amplitude was investigated further.
After establishing the effect of different ultrasonic amplitudes, the effect of altering duty cycles at LFUS was assessed. Ultrasound was fixed at a 20% amplitude and duty cycles of 30% and 100% were evaluated for the gels and compared to the already tested 50% duty cycle. The 30% duty cycle experienced the lowest drug release for both gels with no significant difference compared to unstimulated control in both cases. There was no notable difference in release behaviour observed when comparing the 50% and 100% duty cycles for either gel; over 120 min, the protocols yielded ~ 41–43% drug release from the 2% w/v gel and ~ 22–23% drug release from the 2.5% w/v gel (Fig. 4). A 30% duty cycle saw lower release than a 50% duty cycle from both the 2% w/v (Fig. 4a, p < 0.05) and 2.5% w/v (Fig. 4b, p < 0.01) gels. The 50% duty cycle protocol was taken forward ahead of the 100% duty cycle protocol as it had a lower total ultrasound exposure on the gel.
Ibuprofen release after ultrasound stimulation at different duty cycles from a 2% w/v and b 2.5% w/v alginate hydrogels. Samples were subjected to a 30-s ultrasound pulse at the 30 and 90 min timepoints (indicated by an upwards arrow under the x-axis) at a frequency of 24 kHz, fixed amplitude of 20% and varied duty cycles of 30, 50 and 100%. Significance is shown where release at the 120 min timepoint is greater than that of no stimulation (*p < 0.05, **p < 0.01) and less than that of the 50% duty cycle (†p < 0.05, ††p < 0.01). Error bars refer to ± SEM of three measurements
Responsiveness of a poloxamer hydrogel to optimised ultrasound parameters at low frequency ultrasound (24 kHz)
After establishing the best protocol to achieve temporally controlled release from alginate hydrogels at 24 kHz (50% duty cycle, 20% amplitude for 30 s applied at 30 and 90 min), the same parameters were applied to poloxamer hydrogel. Drug release from poloxamer hydrogel was significantly higher after 120 min when the gels were stimulated with ultrasound compared to the unstimulated control (Suppl. Fig. 2, p < 0.05). The release over 120 min after ultrasound stimulation from poloxamer hydrogel was similar to the release from 2.5% w/v alginate hydrogel when stimulated using the same ultrasonic parameters with 19.6 ± 1.4% and 22.5 ± 1.0% release, respectively. The cumulative release at 120 min was significantly lower compared to the 2% w/v alginate hydrogel (43.0 ± 3.9%, p < 0.05).
To understand the immediate impact of ultrasound on drug release, we examined the release rate of ibuprofen from ultrasound stimulated and unstimulated hydrogels at the 30 to 31 min (Fig. 5a) and 90 to 91 min (Fig. 5b) intervals. The ultrasound-stimulated release rate was significantly higher (p < 0.01) during the 30 to 31 min period for 2.5% w/v alginate and poloxamer hydrogels. However, during the 90 to 91 min period only the ultrasound-stimulated release rate from poloxamer was significantly higher than baseline (p < 0.05). The impact of ultrasound on 2% w/v alginate hydrogel at the 30 to 31 or 90 to 91 min periods was highly variable, and no significant difference was observed in the ibuprofen release rate from this hydrogel (ns = p ≥ 0.05). Additionally, no significant difference was observed in the rate of ultrasound-stimulated release from the 2.5% w/v alginate hydrogel during the 90 to 91 min period due high variability in results.
Drug release percentage per minute from alginate (2% w/v and 2.5% w/v) and poloxamer hydrogel after 30 s of passive release (-US) or ultrasound pulses (+ US) at 24 kHz, 50% duty cycles and 20% amplitude at a 30 and b 90 min. The drug release rates during the 30 to 31 min and 90 to 91 min periods were measured. Significant differences in drug release percentages per minute between unstimulated (−US) or ultrasound-stimulated (+ US) release have been indicated (*p < 0.05**, p < 0.01 and ns = p ≥ 0.05). Error bars refer to ± SEM of three measurements
Gel mass change following low-frequency ultrasound administration
To establish the effect of LFUS on hydrogel mass and to establish if ultrasound-stimulated release is correlated with erosion, mass changes of hydrogels undergoing drug release studies were assessed. In the absence of ultrasound administration, no notable changes to formulation weights were observed for alginate hydrogels (Fig. 6). Over the same experimental period, the application of ultrasound led to a 10.4 ± 2.7% loss in weight from the 2% w/v gel and a 1.2 ± 0.7% loss in weight from the 2.5% w/v gel. Of the 120 min readings, only the weight of the 2% w/v gel exposed to ultrasound was significantly different from its baseline weight (p < 0.05). Poloxamer hydrogel experienced notable changes in weight over 120 min with or without ultrasound stimulation (p < 0.001). Weight loss for ultrasound-stimulated poloxamer hydrogel was not significantly different to unstimulated poloxamer hydrogel (p > 0.05).
Weight change percentage from baseline for alginate (2% w/v and 2.5% w/v) and poloxamer hydrogel following 120 min release study. Samples were assessed after unstimulated (−US) or ultrasound-stimulated (+US) release studies. In the case of ultrasound stimulation, these samples were subjected to 30 s of 24 kHz ultrasound at a 20% amplitude and 50% duty cycle. The instance where a significant difference between the 0 min and 120 min weights of the samples was observed has been indicated (*p < 0.05 and ***p < 0.001). Error bars refer to ± SEM of three measurements
Hydrogel polymers following low-frequency ultrasound administration
The impact of LFUS on the intramolecular covalent bonds of the hydrogel polymers was assessed by collecting FTIR spectra of alginate and poloxamer hydrogels before and after passive release or stimulation with LFUS to establish if ultrasound stimulation causes the breakdown of the polymer chains (Fig. 7). All samples of calcium-crosslinked alginate hydrogel showed peaks at 1601 cm−1 (C-O stretching, asymmetric stretching), 1412 cm−1 (C-O stretching, symmetric stretching) and 1028 cm−1 (C-O stretching) and no difference between the spectra can be seen (Fig. 7a).
Stacked and scaled FTIR transmittance spectra for a alginate, alginate after 120 min of passive release (−US, 2% w/v and 2.5% w/,) and LFUS (+US, 2% and 2.5% w/v) and b the different types of poloxamer, poloxamer after 120 min of passive release (−US) and after LFUS (+US). Spectra were detected from 600 to 1800 cm−1. In the case of ultrasound stimulation, these samples were subjected to 30 s of 24-kHz ultrasound at a 20% amplitude and 50% duty cycle at 30 and 90 min. Alginate and poloxamer hydrogel peaks are indicated with black dashed lines
For poloxamer hydrogel, peaks at 1343 cm−1 (O–H bend) and 1100 cm−1 (C-O stretch) could be observed in all samples, and no difference between the spectra can be seen (Fig. 7b).
Viscosity changes following low-frequency ultrasound administration
To assess the effect of LFUS on hydrogel structure, the viscosity of hydrogels after completing drug release studies at a 2 s−1 shear rate was assessed. Following the 120-min release study, in the absence of ultrasound stimulus, the viscosity of the 2% w/v alginate gel was 47.4 ± 5.9 Pa.s, the viscosity of the 2.5% w/v gel was 50.3 ± 9.5 Pa.s, and for poloxamer hydrogel, it was 642.8 ± 33.0 Pa.s (Fig. 8). The 2% w/v gel exposed to ultrasound had a viscosity of 35.4 ± 4.4 Pa.s, whereas its 2.5% w/v counterpart had a viscosity of 46.8 ± 2.3 Pa.s. Poloxamer had a viscosity of 656.1 ± 20.3 Pa.s when exposed to ultrasound. Overall, the viscosity of the poloxamer hydrogel was significantly higher compared to the alginate hydrogels. No significant differences in viscosity were observed between any samples (ultrasound-stimulated or unstimulated) irrespective of which gel was used (p ≥ 0.05).
Viscosity of alginate (2% w/v and 2.5% w/v) and poloxamer hydrogels at 2 s−1 following 120 min release study. Samples were assessed after unstimulated (−US) or ultrasound-stimulated (+ US) release studies. In the case of ultrasound stimulation, these samples were subjected to 30 s of 24 kHz ultrasound at a 20% amplitude and 50% duty cycle at 30 and 90 min (ns = p ≥ 0.05). Error bars refer to ± SEM of three measurements
Self-healing properties of hydrogels after low-frequency ultrasound administration
The impact of LFUS on the self-healing properties of the hydrogels was assessed by performing frequency sweeps of the hydrogels before and after 120-min release study (Fig. 9). Samples were assessed either before or after unstimulated or ultrasound-stimulated release studies. The storage modulus remained above the loss modulus for all samples at all times. The 2% w/v alginate hydrogel showed the lowest storage and loss modulus ranging from 199.2 to 477.6 Pa and 20.4 to 61.7 Pa respectively (Fig. 9a), compared to poloxamer with a storage modulus ranging from 13,393.8 to 33,949.5 Pa and loss modulus from 3797.6 to 11,834.0 Pa (Fig. 9c). The 2.5% w/v alginate had a storage modulus in the range of 315.3 to 822.8 Pa and loss modulus of 32.8 to 104.1 Pa (Fig. 9b). To analyse differences in the frequency sweeps, the moduli at the middle of the frequency range at 10 rad/s were compared. For each gel, no significant difference in storage modulus was observed between any sample (before, unstimulated or ultrasound-stimulated) (p ≥ 0.05). The loss moduli of each gel were also not significantly different when comparing the hydrogels before or after ultrasound-stimulated release studies (p ≥ 0.05) and no significant difference in loss moduli of the 2.5% w/v alginate hydrogel and the poloxamer hydrogel between any sample group was observed (p ≥ 0.05). However, the 2% w/v alginate hydrogel’s loss modulus was significantly higher for the samples undergoing unstimulated drug release compared to the hydrogels before drug release (p < 0.05) and ultrasound-stimulated gels (p < 0.01).
Frequency sweeps of a 2% w/v alginate, b 2.5% w/v alginate and c poloxamer hydrogels at 2% strain from 0.1 to 100 rad/s before (grey) or following 120-min release study. Samples were assessed before (grey) and after unstimulated (−US) or ultrasound-stimulated (+US) release studies. In the case of ultrasound stimulation, these samples were subjected to 30 s of 24 kHz ultrasound at a 20% amplitude and 50% duty cycle at 30 and 90 min. Error bars refer to ± SEM of three measurements
Ultrasound stimulation at high frequency (1 MHz)
Finally, we assessed the ability of HFUS (1 MHz) to stimulate drug release. First, different intensities and administration times were trialled. At intensities and administration times below 3 W.cm−2 and 10 min, no significant drug release was achieved. Therefore, the ibuprofen-loaded hydrogels were exposed to ultrasound for 10 min at a frequency of 1 MHz, a 50% duty cycle and an intensity of 3 W.cm−2. Based on the results regarding duty cycle impact at 24 kHz, a 50% duty cycle was conserved to achieve comparability. Ultrasound stimulation was applied at 30 and 90 min. Ultrasound stimulation at 30 min resulted in significantly increased rates of ibuprofen release in 2% w/v and 2.5% w/v alginate hydrogels when compared to no stimulation (Fig. 10a, p < 0.05). This effect was not observed at the second stimulation at 90 min for the alginate hydrogels (Fig. 10b). For poloxamer, 1 MHz stimulation had no impact on ibuprofen release rate.
Drug release percentage per minute from 2% w/v, 2.5% w/v alginate and poloxamer hydrogel after 10 min of passive release or ultrasound pulses at 1 MHz and 50% duty cycle at a 30 and b 90 min. The drug release rates during the 30–40 min and 90–100 min periods were measured. Significant differences in drug release percentages per minute between unstimulated (−US) or ultrasound-stimulated (+US) release have been indicated (* p < 0.05 and ns = p ≥ 0.05). Error bars refer to ± SEM of three measurements
Drug release rates per minute were also notably lower compared to stimulation at 24 kHz, 50% duty cycle and 20% amplitude. Ibuprofen release rates at 1 MHz were below 0.19 ± 0.01% (2.5% w/v alginate hydrogel) from all hydrogels compared to a maximum of 12.36 ± 4.59% release from 2% w/v alginate hydrogel at 24 kHz.
Mass changes of hydrogels after HFUS and the effect of HFUS on viscosity were not assessed as the drug release was not notable enough to warrant further investigations.
Discussion
To develop a suitable ultrasound-responsive hydrogel for drug delivery, it is important to identify ideal hydrogel compositions and ultrasonic parameters. The current study demonstrates that amplitude, duty cycle and frequency all impact on ultrasound as a stimulus to achieve on-demand drug delivery and that hydrogel composition alters responsiveness. Alginate and poloxamer were chosen as both gels have the potential for self-healing behaviour [9, 10] which would be beneficial after ultrasound stimulation. Ultrasound can lead to disruption of hydrogel structure [24], but in the case of self-healing hydrogels, the drug release rates can return to baseline after ultrasound stimulation, giving the opportunity to achieve on-demand release from these systems.
A simple formulation comprising alginate crosslinked with calcium was explored first as this had routinely demonstrated desirable drug release and self-healing behaviour following low frequency ultrasound stimulation at 20 kHz [9, 11, 12]. We identified two candidate alginate concentrations of 2% and 2.5% w/v, which showed increased drug release when exposed to LFUS and returned to baseline release behaviour once the stimulus was removed. Alginate hydrogels at lower concentrations than these either showed extensive release in the absence of ultrasound or could not withstand a standard ultrasound administration protocol of 50% duty cycle at 20% amplitude for 30 s and were therefore omitted. In the case of poloxamers, no optimal formulation has yet been reported regarding ultrasound stimulation. Consequently, we chose an in-house formulation that has shown sustained release in vitro for 5 days and in vivo over at least 3 days [13]. Furthermore, the concentrations of poloxamer we tested were chosen as lower concentrations already showed some mechanical weakness when exposed to ultrasound.
To assess the interaction of the hydrogels with the loaded drug ibuprofen, we collected FTIR data which showed the peaks that correlated to the chemical structures of poloxamer [25], alginate [26], and ibuprofen [27]. These peaks have been reported in previously published literature. However, all ibuprofen-hydrogel mixtures showed peak shifts of ibuprofen, suggesting hydrogen bonding occurring between the hydrogel and ibuprofen occurred during the gelation process. The functional groups of ibuprofen are likely to build hydrogen bonds with the polymer backbone of alginate and poloxamer, leading to the peak shift from 1545 cm−1 to a higher wavenumber of 1585 cm−1 [28]. Ultrasound-triggered physical disruption of hydrogels could disturb the hydrogen bonds and contribute to increased drug release rates as one of the mechanisms of ultrasound-triggered drug release [7].
As the next step, we investigated how ultrasonic parameters affected drug release by first looking at different amplitudes and duty cycles at low frequency ultrasound stimulation. We looked for ultrasound parameters that would ensure the stimulus would trigger drug release without causing irreversible damage to the alginate hydrogel. The viscoelastic structure of hydrogels naturally allows them to recover from some level of deformation, so it was important to get an indication of the hydrogels’ ultrasonic deformation thresholds. As amplitude corresponds to the pressure exerted by ultrasound, it was unsurprising that increasing this parameter would trigger greater drug release and, if used in excess, cause structural damage. Previous studies using alginate formulations, both gel-based and nano-carrier-based, have noted that increased amplitudes lead to increased drug release [11, 29]. Our work agrees with these findings, although we emphasise the importance of identifying the range of amplitudes within which drug release is increased without irreversibly compromising gel structure.
Conversely, the relationship between duty cycle and ultrasound responsiveness is more complicated. Pulsed (< 100% duty cycle) ultrasound is used in place of continuous wave (100% duty cycle) ultrasound in the biological setting due to its reduced propensity to heat tissues [30]. Ultrasound applied at a 50% duty cycle has previously achieved equivalent therapeutic outcomes to a 100% duty cycle in enhancing skin permeability of sinomenine hydrochloride [31]. In other studies, duty cycles even lower than 50% were seen to improve small molecule cell uptake to a similar extent as a 100% duty cycle [32]. Finally, triggering ultrasound pulses specifically in response to biological cues such as heartbeats has achieved superior gene delivery to the left ventricle of rats when compared to using a 100% duty cycle [33]. Although these examples did not feature hydrogel systems, they help reinforce our observations of comparable drug release using the 50% and 100% duty cycles.
Following these observations, the effect of the optimised ultrasonic parameters at low frequency was assessed using a different hydrogel. Poloxamer hydrogel is not commonly investigated for ultrasound-stimulated release but has the benefit of being potentially self-healing like alginate [10]. Promisingly, poloxamer hydrogel showed similar ultrasound responsiveness at the optimised amplitude and duty cycle at low frequency compared to 2.5% w/v alginate hydrogel. This adds another prospective preparation to our known library of hydrogels that demonstrate ultrasound-stimulated drug release.
The hydrogel-LFUS combination has previously been used both in applications that are destructive to formulation structure [24] and applications where formulation structure is unchanged [9]. Alginate has demonstrated ideal properties for the latter of these applications, although our weight loss and viscosity evaluations confirmed the importance of a high in-formulation polymer concentration to ensure the system is protected from ultrasound-mediated erosion. For example, the 2.5% w/w alginate hydrogel formulation has shown significant ultrasound-triggered ibuprofen release even though there is no significant erosion after ultrasound stimulation suggesting that in these instances, ultrasound-mediated erosion is unlikely to have caused ibuprofen release. Poloxamer seemed to erode to a great extent in release media, with or without LFUS. Interestingly, the erosion did not correlate to the amount of drug release as unstimulated poloxamer hydrogel eroded to a similar extent as stimulated hydrogel but achieved significantly less drug release. These results suggest that other processes apart from the disruption of the gel caused drug release from the poloxamer gel after LFUS. One possible mechanism causing ultrasound-triggered release from poloxamer hydrogel is the mechanism of streaming or ultrasound-triggered movement of particles as seen in other studies [8, 34, 35]. Ultrasound-triggered oscillation causes the movement of particles within and out of the hydrogel by causing circulating fluid flow within the structures. This fluid flow is proportional to the amplitude and is not disruptive to the gel if it is below a certain threshold. This possible ultrasound-triggered release mechanism explains the increased release of ibuprofen from the poloxamer hydrogel after LFUS which does not seem to relate to the gel’s erosion.
The break of intramolecular bonds of the polymer chains can also be excluded as the cause of increased drug release after LFUS, as the FTIR spectra of the hydrogels remained unchanged throughout the experiment with or without LFUS. Furthermore, ultrasound stimulation at low frequency does not affect the chemical structure of the polymers, and therefore, the self-healing properties are not compromised. Frequency sweeps before and after release studies with LFUS also showed no significant difference in storage and loss modulus, suggesting that the gels remained self-healing throughout the experiment. The loss modulus of the 2% w/v alginate hydrogel showed significantly higher values after 120 min of unstimulated release compared to gels before release or LFUS release studies. This higher loss modulus could be related to the lack of weight loss seen in the unstimulated 2% w/v alginate hydrogel. As this trend is not seen in the storage modulus, its impact on gel structure is also likely to be negligible.
We were also interested in seeing how much of the drug was being released specifically while LFUS was being administered. In the case of poloxamer, the increase in drug release was observed as an immediate consequence of LFUS administration. Conversely, while the alginate hydrogels tended to see increased release rates compared to baseline during administration, this difference was not seen as significantly greater in most circumstances. As all formulations observed an overall increase in drug release, this study demonstrates that the effects of ultrasound on drug release may persist beyond the removal of the stimulus.
As a next step, the influence of ultrasound frequency on ultrasound-stimulated release was assessed. HFUS (> 1 MHz) is also commonly investigated for ultrasound-stimulated release [7, 15]. It has also been used in physiotherapy or in vitro cell experiments due to its promising results on stimulating cell growth [23].
Ultrasound stimulation in the high-frequency range was applied for 10 min and at a high intensity (3 W.cm−2) to achieve notable release. This HFUS significantly enhanced the release rate of ibuprofen from 2 to 2.5% w/v alginate hydrogels. A previous study has observed ultrasound-triggered protein release from poly(N-isopropylacrylamide) (pNIPAAm) at a similar frequency and intensity [15], where the authors reported the increased release to correlate with the ultrasound increasing hydrogel temperature. It does not appear that current methods using 1 MHz ultrasound are exploiting the soundwave to trigger release, but rather that they are taking advantage of the side effect of the ultrasound heating the hydrogel to increase diffusive processes. This may explain why drug release from poloxamer hydrogel could not be increased using HFUS, as poloxamer viscosity and structure are minimally affected at temperatures beyond the gelation point which potentially reduces the ease of ibuprofen diffusion out of the hydrogel. More detailed analyses would be indicated to understand why alginate, but not poloxamer, was responsive to HFUS. However, our study demonstrates the versatility of alginate in showing responsiveness to both LFUS and HFUS while showing low levels of gel erosion. This makes alginate a versatile hydrogel with the ability to have potentially synergistic effects at low and high ultrasound frequencies.
From a structural standpoint, alginate and poloxamer appear to both be suitable polymers for developing implantable ultrasound-responsive delivery systems. Alginate seems to be a potentially more suitable candidate as it is ultrasound-responsive to low and high frequencies and more capable of reassembling after ultrasound stimulation than poloxamer. Although we could not assess this, it would be useful to take a closer look at structural changes to the polymer in real-time while applying the ultrasonic stimulus. A technique that allows this to be evaluated would help better understand the mechanism by which ultrasound triggers drug release, whether this is due to transient alterations in the structural conformation of the hydrogel or whether it is due to streaming effects by which the ultrasound is simply pushing the drug through the tortuous polymer meshwork.
Finally, it is well known that alginate is a biodegradable polymer with hydrogels formed using such polymers, typically only lasting a few months in vivo [36,37,38]. Future studies will focus on the biodegradability of the formulation and assess its long-term release profiles and ultrasound-responsive behaviour before identifying a suitable clinical application for the technology.
In the future, these hydrogels will be used in vivo by implanting or injecting them into tissue. Ultrasound will be applied to the hydrogel through the tissue to cause temporal and spatial controlled drug release, similar to the study by Huebsch et al. [9]. However, before translation, the optimised frequency, duty cycle and amplitude must be determined, which has been attempted in this study.
Conclusion
Ultrasound-responsive behaviour of self-healing hydrogels was dependent on the polymer and ultrasonic parameters used. Increasing ultrasonic amplitude at LFUS led to increased drug release from the hydrogels but high amplitudes damaged the hydrogel structure. Separately, the 50% and 100% duty cycles demonstrated similar increases in drug release from the hydrogels at LFUS indicating that it was not necessary to use this parameter at its maximum level to maximise drug release. HFUS caused ultrasound-triggered release in 2% w/v and 2.5% w/v alginate hydrogel but overall showed less increases in release rates. The poloxamer-based hydrogel, while responsive to LFUS like alginate hydrogel, did not seem to achieve ultrasound-triggered release at HFUS. Future work will evaluate the drug delivery potential of these formulations across longer timeframes, thereby extending their potential clinical value. The current study demonstrates that ultrasound is a complex stimulus with various factors needing attention in order to realise its potential to be used to tune drug delivery rates from hydrogels.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Davoodi P, Lee LY, Xu Q, Sunil V, Sun Y, Soh S, et al. Drug delivery systems for programmed and on-demand release. Adv Drug Deliv Rev. 2018;104–38. Available from: https://doi.org/10.1016/j.addr.2018.07.002.
Cheah E, Wu Z, Thakur SS, O’Carroll SJ, Svirskis D. Externally triggered release of growth factors - a tissue regeneration approach. J Control Release. 2021;74–95. Available from: https://pubmed.ncbi.nlm.nih.gov/33600882/.
Mitragotri S. Healing sound: the use of ultrasound in drug delivery and other therapeutic applications. Nat Rev Drug Discov. 2005;4:255–60. Available from: https://pubmed.ncbi.nlm.nih.gov/15738980/.
Zhang YS, Khademhosseini A. Advances in engineering hydrogels. Science. Science. 2017. Available from: https://pubmed.ncbi.nlm.nih.gov/28473537/.
Drury JL, Mooney DJ. Hydrogels for tissue engineering: Scaffold design variables and applications. Biomaterials. 2003;4337–51. Available from: https://pubmed.ncbi.nlm.nih.gov/12922147/.
Sun Z, Song C, Wang C, Hu Y, Wu J. Hydrogel-based controlled drug delivery for cancer treatment: a review. Mol Pharm. Am Chem Soc. 2020;17:373–91. Available from: https://doi.org/10.1021/acs.molpharmaceut.9b01020.
Wei P, Cornel EJ, Du J. Ultrasound-responsive polymer-based drug delivery systems. Drug Deliv Transl Res. Springer. 2021;11:1323–39. Available from: https://doi.org/10.1007/s13346-021-00963-0.
Pitt WG, Husseini G, Staples BJ. Ultrasonic drug delivery - a general review [Internet]. NIH Public Access. Expert Opin Drug Deliv. 2004;37–56. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1361256/.
Huebsch N, Kearney CJ, Zhao X, Kim J, Cezar CA, Suo Z, et al. Ultrasound-triggered disruption and self-healing of reversibly cross-linked hydrogels for drug delivery and enhanced chemotherapy. National Academy of Sciences. Proc Natl Acad Sci USA. 2014;111:9762–7. Available from: https://www.pnas.org/content/111/27/9762.
Abdeltawab H, Svirskis D, Sharma M. Formulation strategies to modulate drug release from poloxamer based in situ gelling systems [Internet]. Taylor & Francis. Expert Opin Drug Deliv. 2020;495–509. Available from: https://www.tandfonline.com/doi/abs/10.1080/17425247.2020.1731469.
Emi T, Michaud K, Orton E, Santilli G, Linh C, O’Connell M, et al. Ultrasonic generation of pulsatile and sequential therapeutic delivery profiles from calcium-crosslinked alginate hydrogels. Molecules [Internet]. Multidisciplinary Digital Publishing Institute (MDPI). 2019;24. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6470886/.
Kearney CJ, Skaat H, Kennedy SM, Hu J, Darnell M, Raimondo TM, et al. Switchable release of entrapped nanoparticles from alginate hydrogels. Adv Healthc Mater. 2015;4:1634–9. Available from: https://pubmed.ncbi.nlm.nih.gov/26044285/.
Abdeltawab H, Bolam SM, Jaiswal JK, McGlashan SR, Young SW, Hill A, et al. In situ gelling system for sustained intraarticular delivery of bupivacaine and ketorolac in sheep. Elsevier. Eur J Pharm Biopharm. 2022;174:35–46.
Abdeltawab H, Svirskis D, Boyd BJ, Hill A, Sharma M. Injectable thermoresponsive gels offer sustained dual release of bupivacaine hydrochloride and ketorolac tromethamine for up to two weeks. Elsevier. Int J Pharm. 2021;604:120748.
Wu CH, Sun MK, Shieh J, Chen CS, Huang CW, Dai CA, et al. Ultrasound-responsive NIPAM-based hydrogels with tunable profile of controlled release of large molecules. Ultrasonics Elsevier. 2018;83:157–63.
Mitragotri S, Blankschtein D, Langer R. Ultrasound-mediated transdermal protein delivery. Science (1979). Sci. 1995;269:850–3. Available from: https://pubmed.ncbi.nlm.nih.gov/7638603/.
Miller DL, Smith NB, Bailey MR, Czarnota GJ, Hynynen K, Makin IRS. Overview of therapeutic ultrasound applications and safety considerations. NIH Public Access. J Ultrasound Med. 2012;31:623–34. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3810427/.
Pan H, Zhou Y, Izadnegahdar O, Cui J, Deng CX. Study of sonoporation dynamics affected by ultrasound duty cycle. Ultrasound Med Biol. 2005;31:849–56. Available from: https://pubmed.ncbi.nlm.nih.gov/15936500/.
Thakur SS, Ward MS, Popat A, Flemming NB, Parat MO, Barnett NL, et al. Stably engineered nanobubblesand ultrasound - an effective platform for enhanced macromolecular delivery to representative cells of the retina. PLoS One. Pub Lib Sci. 2017;12:e0178305. Available from: https://doi.org/10.1371/journal.pone.0178305.
Kang H, Yin N, Lyon H, Rupenthal ID, Thakur SS, Mugisho OO. The influence of hyperglycemia on the safety of ultrasound in retinal pigment epithelial cells. Cell Biol Int. 2021;45:558–68. Available from: https://pubmed.ncbi.nlm.nih.gov/33049086/.
Buyana B, Aderibigbe BA, Ray SS, Ndinteh DT, Fonkui YT. Development, characterization, and in vitro evaluation of water soluble poloxamer/pluronic-mastic gum-gum acacia-based wound dressing. John Wiley & Sons, Ltd. J Appl Polym Sci. 2020;137:48728. Available from: https://doi.org/10.1002/app.48728.
Zeng C, Li H, Yang T, Deng Z h., Yang Y, Zhang Y, et al. Effectiveness of continuous and pulsed ultrasound for the management of knee osteoarthritis: a systematic review and network meta-analysis. Osteoarthritis Cartilage. W.B. Saunders. 2014;22:1090–9.
Fontana F, Iberite F, Cafarelli A, Aliperta A, Baldi G, Gabusi E, et al. Development and validation of low-intensity pulsed ultrasound systems for highly controlled in vitro cell stimulation. Ultrasonics. Elsevier; 2021;116:106495.
Pereira TA, Ramos DN, Lopez RFV. Hydrogel increases localized transport regions and skin permeability during low frequency ultrasound treatment. Sci Rep. 2017;7. Available from: https://pubmed.ncbi.nlm.nih.gov/28287146/.
Manikandan M, Kannan K, Manavalan R. Compatibility studies of camptothecin with various pharmaceutical excipients used in the development of nanoparticle formulation. Int J Pharm Pharm Sci. 2013;5:315–21. Available from: https://www.researchgate.net/publication/278021847_Compatibility_studies_of_camptothecin_with_various_pharmaceutical_excipients_used_in_the_development_of_nanoparticle_formulation#pf5.
Fajardo AR, Silva MB, Lopes LC, Piai JF, Rubira AF, Muniz EC. Hydrogel based on an alginate-Ca2+/chondroitin sulfate matrix as a potential colon-specific drug delivery system. RSC Adv. 2012;2:11095–103.
Ibuprofen - FTIR - Spectrum - SpectraBase. [cited 2022 Jun 10]. Available from: https://spectrabase.com/spectrum/7EIk8i47TDx.
Ryabenkova Y, Jadav N, Conte M, Hippler MFA, Reeves-Mclaren N, Coates PD, et al. Mechanism of hydrogen-bonded complex formation between ibuprofen and nanocrystalline hydroxyapatite. Langmuir. Am Chem Soc. 2017;33:2965–76. Available from: https://doi.org/10.1021/acs.langmuir.6b04510.
Li X, Wang Z, Xia H. Ultrasound reversible response nanocarrier based on sodium alginate modified mesoporous silica nanoparticles. Frontiers Media S.A. Front Chem. 2019;7:59. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6378627/.
Sandler V, Feingold P. The thermal effects of pulsed ultrasound. South African Journal of Physiotherapy. 1981;37:10–2.
Yin L, Qin FH, Zhou Y, Qi X. Enhancing percutaneous permeability of sinomenine hydrochloride using dual-frequency sonophoresis. Editions de Sante. J Drug Deliv Sci Technol. 2016;36:62–7.
Marin A, Muniruzzaman M, Rapoport N. Acoustic activation of drug delivery from polymeric micelles: effect of pulsed ultrasound. Journal of Controlled Release. J Control Release. 2001;71:239–49. Available from: https://pubmed.ncbi.nlm.nih.gov/11295217/.
Chen S, Shohet RV, Bekeredjian R, Frenkel P, Grayburn PA. Optimization of ultrasound parameters for cardiac gene delivery of adenoviral or plasmid deoxyribonucleic acid by ultrasound-targeted microbubble destruction. J Am Coll Cardiol. 2003;42:301–8. Available from: https://pubmed.ncbi.nlm.nih.gov/12875768/.
Rychak JJ, Klibanov AL, Hossack JA. Acoustic radiation force enhances targeted delivery of ultrasound contrast microbubbles: in vitro verification. IEEE Trans Ultrason Ferroelectr Freq Control. 2005;52:421–32. Available from: https://pubmed.ncbi.nlm.nih.gov/15857050/.
Thakur SS, Chen YS, Houston ZH, Fletcher N, Barnett NL, Thurecht KJ, et al. Ultrasound-responsive nanobubbles for enhanced intravitreal drug migration: an ex vivo evaluation. Eur J Pharm Biopharm. 2019;136:102–7. Available from: https://pubmed.ncbi.nlm.nih.gov/30660691/.
Fragonas E, Valente M, Pozzi-Mucelli M, Toffanin R, Rizzo R, Silvestri F, et al. Articular cartilage repair in rabbits by using suspensions of allogenic chondrocytes in alginate. Biomaterials. 2000;21:795–801. Available from: https://pubmed.ncbi.nlm.nih.gov/10721748/.
Nunamaker EA, Purcell EK, Kipke DR. In vivo stability and biocompatibility of implanted calcium alginate disks. J Biomed Mater Res A. 2007;83:1128–37. Available from: https://pubmed.ncbi.nlm.nih.gov/17595019/.
Tamosaityte S, Galli R, Uckermann O, Sitoci-Ficici KH, Later R, Beiermeister R, et al. Biochemical monitoring of spinal cord injury by FT-IR spectroscopy-effects of therapeutic alginate implant in rat models. Public Library of Science. PLoS One. 2015;10. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4641584/.
Acknowledgements
The authors would like to thank the technical staff at the University of Auckland School of Pharmacy for providing training and maintaining the facilities used to perform the experiments.
Funding
This research was supported through the University of Auckland Faculty Research Development Fund and the New Zealand Health Research Council (22/539). Svenja Meissner is supported by the University of Auckland Doctoral Scholarship. Darren Svirskis is supported by the HRC Hercus Fellowship (19/007). Brad Raos is supported by the Neurological Foundation First Fellowship (1952 FF).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by Svenja Meissner, Sachin S. Thakur, Jhansi H. Akepogu, Samantha M. Arnet, Mohammed Z. Dean, Jessie Ji and Grace Wright. The first draft of the manuscript was written by Svenja Meissner, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Meissner, S., Akepogu, J.H., Arnet, S.M. et al. Investigating the influence of ultrasound parameters on ibuprofen drug release from hydrogels. Drug Deliv. and Transl. Res. 13, 1390–1404 (2023). https://doi.org/10.1007/s13346-022-01277-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-022-01277-5