Abstract
The purpose of this study was to develop and evaluate nanoemulsions (NEs) containing besifloxacin for ocular drug delivery. Pseudo ternary phase diagrams were constructed using Triacetin (oil), Cremophor® RH 40 (surfactant), and Transcutol®P (co-surfactant) to identify NE regions. Six formulations were developed by low-energy emulsification method and then evaluated for size, refractive index, pH, osmolality, viscosity, and drug release. After accelerated physical stability and bovine conrneal permeation studies, NE2 was chosen as optimized formulation forantimicrobial efficacy, and hen’s egg test-chorioallantoic membrane (HET-CAM) tests. The particle size of optimum NE was 14 nm with a narrow size distribution. Moreover, other physicochemical characterizations were in the acceptable range for ocular administration. Besifloxacin-loaded NEs demonstrated sustained release pattern and 1.7-fold higher permeation compared with the control suspension in the ex vivo transcorneal permeation study. HET-CAM test indicated no irritation, and HL% revealed no damage to the tissue, so the optimum NE is well tolerated by the eye. In vitro antimicrobial evaluation, showed comparative efficacy of lower drug-loaded NE (0.2%) versus 0.6% besifloxacin suspension (equal concentration to commercial besifloxacin eye drop). In conclusion, besifloxacin-loaded NEs could be considered as a suitable alternative to the marketed suspension for treating bacterial eyeinfections.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacteria are the most important cause of various eye infections, including keratitis, conjunctivitis, blepharitis, endophthalmitis, and dacryocystitis. These conditions are accompanying with different risk factors such as contact lenses, trauma, and surgery [1, 2]. The most common Gram-positive and Gram-negative pathogens causing ocular infections are Staphylococcus aureus and Pseudomonas aeruginosa, afflicting 11/100,000 persons in the USA and nearly 799/100,000 persons a year in developing countries to keratitis which is the second leading cause of blindness and also 135/10,000 persons in the USA to bacterial conjunctivitis which is a third of ocular pathologies worldwide [3,4,5].
Lack of proper treatment for the infectious eyes can cause vision damage. Fluoroquinolones with broad-spectrum antibacterial activity against both Gram-positive and Gram-negative pathogens are effectively used in recent years. But unfortunately, resistance to older agents in this group has been reported recently [6, 7]. Besifloxacin (BSF) is a novel fluoroquinolone family member with broad and potent antibacterial activity against various pathogens, including drug-resistant strains. The dual inhibitory mechanism which allows it to inhibit both bacterial DNA gyrase and topoisomerase IV equally and also lack of systemic formulation minimizes microbial resistance to BSF in comparison to other fluoroquinolones [8, 9].
BSF hydrochloride is a water-insoluble drug, so it is formulated as an ophthalmic suspension (0.6%) under the trade name of Besivance®. FDA has approved this medication for treating bacterial conjunctivitis in 2009. Recommended dose for BSF in bacterial conjunctivitis is three times a day for 5 to 7 days [5].
Although eye drop formulations have various advantages such as ease of administration, higher drug concentration at the site of action, and minimum systemic adverse effects, but short precorneal residence, due to the tear drainage and blinking in one hand, and presence of bimodal corneal structure in other hand, leads to low penetration of the drug into the eyes [10]. Furthermore, solid particles of BSF in the suspension form need to solubilize before elimination from eye surface which takes time, and by then, it may cause blurred vision and inconvenience for the patient. These limitations make ocular bioavailability of BSF less than 5% and increase daily frequency administration, which reduces patient compliance. So it seems developing a novel, sustained release formulation containing lower dose of BSF will enhance the therapeutic characteristics of this drug.
Nanoemulsions are defined as colloidal dispersion consisting of two immiscible liquids, generally small spherical oil droplets (less than 100 nm), dispersed in aqueous medium, stabilized with a mixture of surfactant and co-surfactant [11, 12]. Many advantages have been presented by NEs such as high kinetic stability, high capacity to dissolve large quantities of hydrophobic drugs, sustained drug release, low viscosity, improved corneal permeation to deeper layer of ocular tissue, and ease of sterilization [12,13,14]. The aim of this study is to formulate novel BSF-loaded nanocarrier in lower amount (0.2%) in comparison with the 0.6% BSF suspension (equal concentration to the commercial eye drop) to promote its therapeutic efficacy.
Material and methods
Materials
Besifloxacin powder was purchased from Senova Technology Co., Ltd, China; Transcutol®P (diethylene glycerol monoethyl ether) was provided from Gattefosse, France; Triacetin (glycerol triacetate) was supplied from Samchun Chemical Co., Ltd, South Korea; and Cremophor® RH 40 and Dialysis tubing cellulose membrane was obtained from Sigma Aldrich Chemical Company, USA.
Component selection
Oil, surfactant, and co-surfactant for NE formulation were chosen according to the BSF solubility in the various components. The solubility of BSF was identified by adding the excess amount of BSF in 1 mL of the oils (Triacetin, Miglyol 812 and Capryol 90), co-surfactants (PEG 400, Transcutol®P and PG), and 15% w/w surfactant solutions (Tween 80, Cremophor®RH 40 and Brij 35). Samples were first mixed by vortex and then placed in a shaker at 25 °C to attain equilibrium. After 24 h, samples were centrifuged at 10,000 rpm for 10 min. The supernatant was separated and diluted with methanol. Finally, the solubilized amount of BSF in each vehicle was obtained by UV spectrophotometer at 290 nm.
Construction of partial pseudo-ternary phase diagrams
Pseudo-ternary phase diagrams of quaternary systems consisting of oil (Triacetin), surfactant (Cremophor®RH 40), co-surfactant (Transcutol®P), and water at various surfactant/co-surfactant weight ratios (RSM) were constructed using water titration method to procure the oil-in-water (o/w) nanoemulsion regions. Appropriate amounts of oil, surfactant, and co-surfactant were weighed into glass vials and mixed at room temperature until a homogenous mixture was reached. Then distilled water was added dropwise to the mixture and stirred. After each titration step, the sample was monitored visually for clarity. Mixtures with optically transparent or translucent appearance, served as NE. Finally, Sigma-plot Ver.12 software was used for construction of Pseudo-ternary phase diagrams.
Preparation of BSF-loaded nanoemulsions
Following the identification of o/w NE regions on the phase diagrams, BSF-loaded NEs were prepared by low-energy emulsification method according to the following described procedure. The oil phase was separately prepared by mixing the intended amounts of oil (3 wt% or 4.5 wt%) and surfactant mixture (15 wt%, 22.5 wt%, or 30 wt%). To the following mixture, constant amount of BSF (0.2 wt%) was added and persistently stirred using a mechanical stirrer. Then, the required amount of water was added dropwise and stirred for another 1 h at 1000 rpm in order to obtain a transparent/translucent NE (total weight of 1 g).
Physicochemical characterization
All developed BSF NEs were characterized as described below:
Droplet size and polydispersity index
Photon correlation spectroscopy using a Zetasizer Nano ZS (Malvern Instruments Ltd., UK) was applied for measuring droplet size and polydispersity index (PDI) of BSF NEs. All measurements were performed in triplicate, at room temperature at 90° angle.
pH measurement
The pH of samples was determined using a calibrated pH-meter (Sartorius, Germany) at room temperature. All measurements were done three times, and the data are stated as mean ± standard deviation (SD).
Refractive index
The refractive index of formulations was measured at 25 °C by placing sufficient amount of samples on the slide of the refractometer (Atago refractometer, Model 3T, Japan).
Osmolality
The vapor pressure osmometer (K-7000, Knauer, Germany) was employed to measure the osmolality of NEs.
Viscosity
The rheological characteristic of formulations was evaluated at 25 °C using a Brookfield DVII viscometer (Brookfield Engineering Laboratories Inc., USA) fitted with spindle No. 34. About 10 mL of formulations were poured into the container, and the rotation speed was increased up from 25 to 200 rpm, and the viscosity was determined from the linear portion of the rheogram, where the shear stress (dynes/cm2) was plotted against the shear rate (s−1).
In vitro drug release studies
The in vitro release studies of BSF-loaded NEs were conducted in the triplicate using USP dissolution tester apparatus II. The temperature was set at 34 ± 0.5 °C to simulate the ocular surface temperature. One mL of each formulation was instilled in a cellulose dialysis bag (MW cut-off 12,400 Da) that was drenched in distilled water at 4 °C for 24 h. The dialysis bag was then attached to the paddle of the dissolution tester with speed revolution of 50 rpm in 250 mL release medium consisting of phosphate buffer (pH = 7.4). The test was carried out for 6 h, and at definite time intervals (15, 30, 45, 60, 90, 120, 180, 240, 300, and 360 min), 2 mL of medium was withdrawn and substituted by fresh buffer. Samples were analyzed by UV spectrophotometer at 290 nm, and the percentage of release efficiency (RE) was calculated using the following formula [15].
where y is the percentage of drug released at time t.
Accelerated physical stability
The stability of formulations was checked through three different tests including heating–cooling cycles, freeze–thaw cycles, and centrifugation [16,17,18,19]. After each test, formulations were observed to control if any physical instability such as phase separation, opacity, drug precipitation, or droplet size change had occurred.
Heating–cooling cycles
Formulations were kept six cycles between refrigerator temperature (2–8 °C) and 40 °C, each for 48 h.
Freeze–thaw cycles
Three freeze–thaw cycles were carried out between − 21 and + 25 °C for at least 48 h at each temperature.
Centrifugation
Centrifugation at 13,000 rpm for 30 min was performed for those formulations which passed the previous tests.
Ex vivo transcorneal permeation studies
Ex vivo transcorneal permeation studies of BSF NEs were carried out using Franz-type diffusion cells with 2.27 cm2 diffusion area.
Whole bovine eyeballs were obtained from a local slaughter house and conveyed to the laboratory in phosphate-buffered saline maintained at 4 °C. The corneas were carefully removed along with surrounding scleral tissue and rinsed with cold phosphate-buffered saline. Corneas were mounted between the donor and receptor compartments of the Franz cells in such a way that the surface of excised cornea was covered entirely with diffusion medium. The receptor compartment was filled with 12 mL of phosphate-buffered saline (pH = 7.4) and agitated persistently using magnetic stirrer, while the donor compartment was filled with 0.2 mL of selected BSF-loaded NEs or control (BSF suspension). The upper space of donor part was covered with parafilm to avoid formulation evaporation, and the temperature of the system was set at 34 ± 1 °C. Sink conditions were maintained during the examination. About 0.5 mL from receptor medium was withdrawn at 30, 60, 90, 120, 180, 240, 300, and 360 min and after dilution analyzed by UV spectroscopy at 290 nm.
Determination of corneal hydration levels
At the end of the permeation study, the scleral ring around the cornea was cautiously excised and removed; then, the cornea was rinsed with water and excess water was removed using a paper filter. The wet weight, Wa, of each corneal sample was then measured. Corneas were dried in an incubator at 60 °C for 16 h to obtain the dry corneal weight, Wb. The percentage of corneal hydration level (HL%) was measured for corneas treated with formulation using the following formula [20]:
Transmission electron microscopy
Morphological observation of optimized NE was conducted using TEM (TEM; Philips EM208s). The selected sample was prepared as described before and then was placed on a 300 mesh carbon-coated copper grid and after drying, the process was operated at 100 kV.
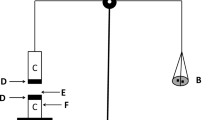
Ocular irritancy test
In vitro ocular tolerance was evaluated using the hen’s egg test-chorioallantoic membrane (HET-CAM) test to make sure that BSF-loaded NEs are safe for ocular administration. Freshly collected fertilized hen’s eggs were incubated at 37 ± 0.5 °C and 60.0 ± 5.0% relative humidity, rotating manually every 12 h for 10 days. At the end of the tenth day, intact eggs with the ideal embryo growth were detected. After eggshell and inner membranes were removed, 0.2 mL of each formulation, NaOH (as control positive) and phosphate-buffered saline (as control negative) were instilled on the CAM surface. Hemorrhage, hyperemia, and coagulation of blood vessels were investigated at various times post administration (0.5, 2, and 5 min) to analyze irritancy of the formulations [21].
Antimicrobial efficacy study
Antimicrobial activity of optimized formulation was evaluated using the agar diffusion test by the cup plate technique. Selected formulation was compared with 0.6 mg/ml BSF suspension. The surface of sterile nutrient agar was inoculated with Pseudomonas aeruginosa and Staphylococcus aureus with an optical density equal to 0.5 McFarland. About 100 µL of selected formulation and the control suspension was poured into cups and then incubated at 37 °C for 24 h. The inhibition zone around each cup was then measured and compared with control [22].
Statistical analysis
All experiments were performed three times, and findings exhibited as mean ± SD. One-way ANOVA with Tuckey post hoc test with p < 0.05 as a significant level was applied by using Graf pad primes software version 7 to determine statistical differences between samples.
Results and discussion
Component selection
An important criterion to formulate O/W NEs is solubility of poorly water soluble drug in oil, surfactant, and co-surfactant. Solubility of drug in the oily phase is very important since it leads to more drug loading and maintains drug in the solubilized form. As shown in Table 1, the solubility of BSF was found to be higher in Triacetin in comparison to the other oils. It would be noted that by reducing lipid chain length in Triacetin (as small chain triglyceride) and existence of amphiphilic nature in Capryol 90 structure (as medium chain triglyceride), solvent capacity of these vehicles has been increased in comparison to Miglyol 812 (as medium chain triglyceride) and isopropyl myristate (as long chain triglyceride) with negligible or no solubilizing effect. Although BSF is a water-insoluble drug, it has log P value equal to 0.7, which means moderate lipophilicity, so it is reasonable that high solubility of BSF in these oils would not be reached. As for surfactants, since high amounts of these excipients generally causes ocular toxicity, it is important to choose non-ionic surfactant to lower the toxicity. On the other hand, for developing O/W NEs, HLB value of surfactant should be between 8 and 18 [23]. Cremophor® RH 40 has both features mentioned above, and BSF showed higher solubility within this surfactant solution. Among screened co-surfactants, Transcutol®P showed the highest BSF solubility. Therefore it was selected for preparation of BSF NEs.
Construction of partial pseudo-ternary phase diagrams
For preparing ocular NEs, various types of components based on solubility test including Triacetin as an oil, Cremophor® RH 40 as a nonionic surfactant, and Transcutol®P as a co-surfactant were chosen. All selected ingredients are safe for ophthalmic use, and their effectiveness on corneal penetration has been proven in several studies [24,25,26,27]. Since concentration of each constituent plays an important role in the formation of stable NE, three pseudo-ternary phase diagrams were constructed by water titration method at different Cremophor® RH 40: Transcutol®P (surfactant mixture) weight ratios (RSM) of 1:1, 1:2, and 2:1. As illustrated in Fig. 1, all three systems demonstrated O/W NE region. These phenomena showed that all nominated excipients are compatible sufficiently together to form NE structure. Among various RSM, the most extensive NE region was observed with 1:2 RSM which is in accordance with similar studies [22, 28]. This finding indicates that the incorporation of oil in the system will increase with enhancement of co-surfactant concentration at a fixed level of surfactant mixture. It seems the expansion of the NE domain at 1:2 RSM is due to hydrophobic chain length compatibility. As Triacetin and Transcutol®P both have short to medium hydrocarbon chain length; therefore, nearby hydrophobic chains have matched tighter together and this guarantees more stability of the system [29]. Based on the results, 1:2 RSM was selected for development of NE formulations.
Preparation of BSF-loaded NEs
According to the pseudo-ternary phase diagrams, six formulations consisting of different concentrations of oil, surfactant, and co-surfactant were chosen (Table 2). Fixed amount of BSF powder was incorporated in each sample as described in the preparation method. All formulations were stable after 72 h at room temperature, so were used for further evaluations.
Physicochemical characterization of BSF-loaded NEs
Droplet size and polydispersity index
The average droplet size of all formulations was found to be less than 15 nm. Also, polydispersity index (PDI) values of all formulations ranging from 0.145 to 0.217 demonstrated uniformity and narrow size distribution of droplets. This small and uniform droplet size could be explained by proper arrangement of co-surfactant molecules into the surfactant film covering oil droplets, which results in reduced fluidity and viscosity of interfacial film and thus lesser diameter of droplets [30]. Nanometric size of droplets could deliver higher amounts of drug into the eye due to increased surface area and improved ability of drug to penetrate into the ocular tissues. On the other hand, small droplets can limit the availability of drug only to targeted tissue and thus decrease side effects and dose frequency [31].
pH measurement
Although normal tear fluid pH is about 7.4, buffering capacity of tear fluid can modify pH of the applied products immediately. Hence, the acceptable range of pH for ophthalmic use is between 3.0 and 8.6 [32], BSF NE formulations exhibited an acceptable range of pH from 3.91 to 4.57 (Table 3).
Refractive index
Inappropriate refractive index (RI) value shows the possibility of visual impairment and discomfort caused by eye drops [33]. All RI data were in the range from 1.35 to 1.38, which is in the acceptable range of RI (less than 1.476) for ophthalmic administration [34].
Osmolality
As shown in Table 3, the osmolality value of all formulations is from 619 to 1648 mOsmol/kg. Since the tolerable range of osmolality for ocular administration is about 171 to 1711 mOsm/kg [32], therefore, no possibility of irritation is expected for prepared formulations.
Viscosity
Another critical parameter of eye formulations is viscosity. Although higher viscosity results in prolonged residence time in the eye, it may also cause difficulties in product instillation, eye irritation, and reflex tearing [35]. So the recommended viscosity value is less than 20 cP [36]. For all NE formulations, Newtonian behavior with viscosities between 2.87 cP and 5.33 cP was observed (Table 3).
In vitro drug release studies
Controlled and sustained drug delivery is one of the valuable features of ophthalmic products, since it may reduce dose frequency and thus improve patient compliance. NEs are systems that can provide this advantage for ocular use [37, 38]. Based on the in vitro drug release profile, illustrated in Fig. 2, prolonged release pattern was observed during 6 h in all NE formulations. Due to the dilution effect of tear fluid and short residence time of liquid preparations on the surface of the eye, area under the curve of percentage of drug released versus time within 1 h is considered as calculated release data in this study. As shown in Table 3, NE6 exhibited the lowest RE% (20.59%). On the other hand, NE1 showed the highest RE% (30.02%) after 1 h. It seems that the distribution of BSF between the oily core and the surrounding surfactant film of nanodroplets can retard the diffusion of the drug.
Effect of surfactant concentration on RE%
By evaluating the impact of surfactant amount on RE%, it was concluded that in both fixed oil concentration groups (3 and 4.5%), the release rate was decreased significantly (p < 0.05) by increasing the percentage of the surfactant mixture from 15 to 22.5 or 30%. It is assumed that higher concentration of Smix could surround the oil droplets and restrict the drug diffusion to the release medium. In other words, a compacted interfacial layer acts as a barrier turning NEs into the nanoreservoirs resulting in sustained release behavior [39].
Effect of oil concentration on RE%
In all three groups with constant amount of Smix, a slight drop of RE% could be observed by elevation of oil percentage from 3 to 4.5%, which is attributed to more dissolving of hydrophobic BSF in the oily phase of NE structures. It is predictable that by further enhancement of oil amount, a significant reduction in release rate could occur as mentioned in previous work [40, 41]. Although all developed NEs exhibited appropriate formulation characteristics such as droplet size, RI, osmolality, pH, and viscosity with extended-releas properties, regarding saftey concern, NE1 and NE2 that consist of the lowest amount of surfactant mixture (15%) were selected for further evaluations.
Accelerated physical stability studies
Formulations went through three different stress conditions to evaluate physical stability. During heating–cooling cycles and after centrifugation, no physical instability, including phase separation, creaming, cracking, growth of droplet size (Table 4), or any turbidity was observed. Only during freeze–thaw cycles when NEs were stored at − 21 °C, turbidity was observed, which was then recovered at room temperature. This temporary turbidity could be explained by coagulation and crystallization of oil globules [25].
Ex vivo transcorneal permeation
Permeation profile of optimized formulations as compared with control suspension has been illustrated in Fig. 3. According to the calculated apparent permeability coefficients (Papp) listed in Table 5, NE1 and NE2 exhibited 1.2 and 1.7-fold higher penetration than the control suspension respectively. Higher diffusion of BSF NEs through excised bovine cornea could be due to permeation enhancing properties of Smix and oil existed in the NE formulations. Various studies have revealed that these excipients facilitate the transport of drugs into the internal ocular tissues by transient influence on the integrity of cornea epithelium [23, 27, 42]. Furthermore, nanosized droplets could bypass corneal barriers by the endocytosis process [43].
On the other hand, it seems that Papp difference between NE1 and NE2 is probably attributed to the higher oil content of NE2, resulting in improved formulation adhesion to lipophilic cornea epithelium [44].
The corneal HL% is a factor that can provide information about any damage to the cornea upon instillation of formulation. Values higher than 83% would cause damage to the tissue. As displayed in Table 4, HL values of both NE formulations are in the normal range of 76–79%, indicating that none of them cause any damage to the tissue [45].
Since NE2 showed a significant effect on corneal penetration of BSF in comparison with BSF suspension (p < 0.05), so this sample was selected for in vitro irritancy and antimicrobial efficacy studies.
Transmission electron microscopy
TEM images exhibited spherical oil droplets with diameter under 20 nm as shown in Fig. 4. The result was in agreement with size analysis performed by nanosizer. Nanodroplets were dispersed randomly and no agglomeration was observed in the field.
Ocular irritancy test
The mucosal structure of the eye is very sensitive to instillation of drug. So investigation on irritation possibility of any topical formulation proposed for administration at the anterior segment of the eye is necessary. In vivo toxicity studies such as Draize test are recommended to switch with efficient in-vitro test because of ethical concern. Similarity of the vascular tissue between CAM and human conjunctiva makes HET-CAM test a proper alternative to examine any ocular irritancy such as hyperemia, hemorrhages, and coagulation [46, 47]. So in the present study, the HET-CAM test was carried out to evaluate the irritation potential of NE2. It should be considered that no irritation was noticed after PBS and NE instillation during 5 min, while using NaOH, clotting and hemorrhages were observed as illustrated in Fig. 5. So it seems that the optimized NE formulation is non-irritant for ophthalmic administration.
Antimicrobial efficacy study
Antimicrobial efficacy of NE2 containing 0.2% BSF and 0.6% BSF suspension (equivalent to the marketed product, Besivance®) as control was executed against susceptible microorganisms, pseudomonas aeruginosa and staphylococcus aureus by using cup plate method. After 24-h incubation, a noticeable inhibitory zone diameter was observed for both NE and control samples (Fig. 6). Based on the results (Table 6), slightly larger inhibition zone diameter was found for 0.2% NE against 0.6% suspension (approximately 3 mm and 1.5 mm for Staphylococcus aureus and Pseudomonas aeruginosa, respectively). Although almost identical anti-microbial effectiveness is obtained for both tested samples, it should be noted that desirable antimicrobial potential was achieved by lowering the amount of drug to one-third of the control suspension. It would be noted that similar findings have been achieved in previous studies by employing nanosized emulsions for antimicrobial efficacy evaluation [22, 48].
Conclusion
In this study, BSF loaded NEs were developed by low energy emulsification method as a novel formulation used for bacterial eye infections. Optimized formulation was lower than 20 nm in size and exhibited suitable physicochemical properties and sustained release profile, which could result in longer duration of action. Moreover, ex vivo transcorneal permeation was significantly higher than the control suspension, and in spite of reducing dose to one-third of commercial product, in vitro antimicrobial efficiency also showed a comparable antimicrobial activity with control suspension. Based on irritation studies, the developed formulation was found to be safe for ophthalmic use. It seems that NE could be considered as a promising strategy to improve BSF therapeutic efficiency. However, further in-vivo investigations are needed to optimize the NE for the ocular administration of BSF.
References
Teweldemedhin M, Gebreyesus H, Atsbaha AH, Asgedom SW, Saravanan M. Bacterial profile of ocular infections: a systematic review. BMC Ophthalmol. 2017. https://doi.org/10.1186/s12886-017-0612-2.
O’Callaghan RJ. The Pathogenesis of Staphylococcus auerus Eye Infections. Pathogens. 2018. https://doi.org/10.3390/pathogens7010009.
Mahvan TD, Hornecker JR, Buckley WA, Clark S. The role of besifloxacin in the treatment of bacterial conjunctivitis. Ann Pharmacother. 2014. https://doi.org/10.1177/1060028014524175
Rahimi F, Hashemian MN, Khosravi A, Moradi G, Bamdad S. Bacterial keratitis in a tertiary eye centre in Iran: a retrospective study. Middle East Afr J Ophthalmol. 2015. https://doi.org/10.4103/0974-9233.151870.
Tótoli EG, Salgado HRN. Besifloxacin: a critical review of its characteristics, properties, and analytical methods. Crit Rev Anal Chem. 2018. https://doi.org/10.1080/10408347.2018.1429885.
Proksch JW, Granvil CP, Siou-Mermet R, Comstock TL, Paterno MR, Ward KW. Ocular pharmacokinetics of besifloxacin following topical administration to rabbits, monkeys, and humans. J Ocul Pharmacol Ther. 2009. https://doi.org/10.1089/jop.2008.0116.
Miller D, Chang JS, Flynn HW, Alfonso EC. Comparative in vitro susceptibility of besifloxacin and seven comparators against ciprofloxacin- andmethicillin-susceptible/nonsusceptible staphylococci. J Ocul Pharmacol Ther. 2013. https://doi.org/10.1089/jop.2012.0081
Haas W, Pillar CM, Zurenko GE, Lee JC, Brunner LS, Morris TW. Besifloxacin, a novel fluoroquinolone, has broad-spectrum in vitro activity against aerobic and anaerobic bacteria. Antimicrob Agents Chemother. 2009. https://doi.org/10.1128/AAC.00418-09.
DeLeon J, Silverstein BE, Allaire C, Gearinger LS, Bateman KM, Morris TW, Comstock TL. Besifloxacin ophthalmic suspension 0.6% administered twice daily fo 3 days in the treatment of bacterial conjunctivitis in adults and children. Clin Drug Investig. 2012. https://doi.org/10.2165/11632470-000000000-00000
Morrison PW, Khutoryanskiy VV. Advances in ophthalmic drug delivery. Ther Deliv. 2014. https://doi.org/10.4155/tde.14.75.
McClements DJ. Nanoemulsions versus microemulsions: terminology, differences, and similarities. Soft Matter. 2012. https://doi.org/10.1039/C2SM06903B.
Gupta A, Eral HB, Hatton TA, Doyle PS. Nanoemulsions: formation, properties and applications. Soft Matter. 2016. https://doi.org/10.1039/c5sm02958a.
Vandamme TF. Microemulsions as ocular drug delivery systems: recent developments and future challenges. Prog Retin Eye Res. 2002. https://doi.org/10.1016/s1350-9462(01)00017-9.
Ammar HO, Salama HA, Ghorab M, Mahmoud AA. Nanoemulsion as a potentialophthalmic delivery system for dorzolamide hydrochloride. AAPS Pharm Sci Tech. 2009a. https://doi.org/10.1208/s12249-009-9268-4.
Khan KA, Rhodes CT. Effect of compaction pressure onthe dissolution efficiency of some direct compression systems. Pharm Acta Helv. 1972;47:594–607.
Djordjevic L, Primorac M, Stupar M. In vitro release of diclofenac diethylamine from caprylocaproyl macrogolglycerides based microemulsions. Int J Pharm. 2005. https://doi.org/10.1016/j.ijpharm.2005.02.014.
Chen H, Mou D, Du D, Chang X, Zhu D, Liu J, Xu H, Yang X. Hydrogel-thickened microemulsion for topical administration of drug molecule at an extremely low concentration. Int J Pharm. 2007. https://doi.org/10.1016/j.ijpharm.2007.03.052.
Shafiq S, Shakeel F, Talegaonkar S, Ahmad FJ, Khar RK, Ali M. Development and bioavailability assessment of ramipril nanoemulsion formulation. Eur J Pharm Biopharm. 2007. https://doi.org/10.1016/j.ejpb.2006.10.014.
Butani D, Yewale C, Misra A. Amphotericin B topical microemulsion:formulation, characterization and evaluation. Colloids Surf B Biointerfaces. 2014. https://doi.org/10.1016/j.colsurfb.2014.01.014.
Liu Z, Zhang X, Wu H, Li J, Shu L, Liu R, Li L, Li N. Preparation and evaluation of solid lipid nanoparticles of baicalin for ocular drug delivery system in vitro and in vivo. Drug Dev Ind Pharm. 2011. https://doi.org/10.3109/03639045.2010.522193
Alany RG, Rades T, Nicoll J, Tucker IG, Davies NM. W/O microemulsions for ocular delivery: evaluation of ocular irritation and precorneal retention. J Control Release. 2006. https://doi.org/10.1016/j.jconrel.2005.11.020.
Shah J, Nair AB, Jacob S, Patel RK, Shah H, Shehata TM, Morsy MA. Nanoemulsion based vehicle for effective ocular delivery of moxifloxacin using experimental design and pharmacokinetic study in rabbits. Pharmaceutics. 2019. https://doi.org/10.3390/pharmaceutics11050230.
Pathak MK, Chhabra G, Pathak K. Design and development of a novel pH triggered nanoemulsified in-situ ophthalmic gel of fluconazole: ex-vivo transcorneal permeation, corneal toxicity and irritation testing. Drug Dev Ind Pharm. 2013. https://doi.org/10.3109/03639045.2012.707203.
Tamilvanan S, Benita S. The potential of lipid emulsion for ocular delivery of lipophilic drugs. Eur J Pharm Biopharm. 2004. https://doi.org/10.1016/j.ejpb.2004.03.033.
Ammar HO, Salama HA, Ghorab M, Mahmoud AA. Nanoemulsion as a potential ophthalmic delivery system for dorzolamide hydrochloride. AAPS Pharm Sci Tech. 2009b. https://doi.org/10.1208/s12249-009-9268-4.
Patel N, Nakrani H, Raval M, Sheth N. Development of loteprednol etabonate-loaded cationic nanoemulsified in-situ ophthalmic gel for sustained delivery and enhanced ocular bioavailability. Drug Deliv. 2016. https://doi.org/10.1080/10717544.2016.1223225.
Mahboobian MM, Seyfoddin A, Aboofazeli R, Foroutan SM, Rupenthal ID. Brinzolamide-loaded nanoemulsions: ex vivo transcorneal permeation, cell viability and ocular irritation tests. Pharm Dev Technol. 2019. https://doi.org/10.1080/10837450.2018.1547748.
Fouad SA, Basalious EB, El-Nabarawi MA, Tayel SA. Microemulsion and poloxamer microemulsion-based gel for sustained transdermal delivery of diclofenac epolamine using in-skin drug depot: in vitro/in vivo evaluation. Int J Pharm. 2013. https://doi.org/10.1016/j.ijpharm.2013.06.009.
Ammar HO, Salama HA, Ghorab M, Mahmoud AA. Development of dorzolamide hydrochloride in situ gel nanoemulsion for ocular delivery. Drug Dev Ind Pharm. 2010. https://doi.org/10.3109/03639041003801885.
Tayel SA, El-Nabarawi MA, Tadros MI, Abd-Elsalam WH. Promising ion-sensitive in situ ocular nanoemulsion gels of terbinafine hydrochloride: design, in vitro characterization and in vivo estimation of the ocular irritation and drug pharmacokinetics in the aqueous humor of rabbits. Int J Pharm. 2013. https://doi.org/10.1016/j.ijpharm.2012.12.049.
Raval N, Khunt D, Misra M. Microemulsion-based delivery of triamcinolone acetonide to posterior segment of eye using chitosan and butter oil as permeation enhancer: an in vitro and in vivo investigation. J Microencapsul. 2018. https://doi.org/10.1080/02652048.2018.1425750.
United State Pharmacopeia, Ophthalmic Products-Quality Tests, in USP39-NF34, 2016. pp. 589–595.
Fialho SL, da Silva-Cunha A. New vehicle based on a microemulsion for topical ocular administration of dexamethasone. Clin Exp Ophthalmol. 2004;32:626–32.
Kesavan K, Pandit JK, Kant S, Muthu MS. Positively charged microemulsions of dexamethasone: comparative effects of two cosurfactants on ocular drug delivery and bioavailability. Ther Deliv. 2013. https://doi.org/10.4155/tde.13.106.
Zignani M, Tabatabay C, Gurny R. Topical semi-solid drug delivery: kinetics and tolerance of ophthalmic hydrogels. Adv Drug Deliv Rev. 1995. https://doi.org/10.1016/0169-409X(95)00015-Y.
Radomska-Soukharev A, Wojciechowska J. Microemulsions as potential ocular drug delivery systems: phase diagrams and physical properties depending on ingredients. Acta Pol Pharm. 2005;62:465–71.
Pathak K, Pattnaik S, Swain K. Application of nanoemulsions in drug delivery. in: Jafari SM, McClements DJ editors. Nanoemulsions, Elsevier Inc; 2018;415–433
Peters MCC, Santos Neto ED, Monteiro LM, Yukuyama MN, Machado MGM, de Oliveira IF, Zanin MHA, Löbenberg R, Bou-Chacra N. Advances in ophthalmic preparation: the role of drug nanocrystals and lipid-based nanosystems. J Drug Target. 2019. https://doi.org/10.1080/1061186X.2019.1663858.
Singh Y, Meher JG, Raval K, Khan FA, Chaurasia M, Jain NK, Chourasia MK. Nanoemulsion: concepts, development and applications in drug delivery. J Control Release. 2017. https://doi.org/10.1016/j.jconrel.2017.03.008.
Mahboobian MM, Seyfoddin A, Rupenthal ID, Aboofazeli R, Foroutan SM. Formulation development and evaluation of the therapeutic efficacy of brinzolamide containing nanoemulsions. Iran J Pharm Res. 2017;16:847–57.
Soliman OAE, Mohamed EA, Khatera NAA. Enhanced ocular bioavailability of fluconazole from niosomal gels and microemulsions: formulation, optimization, and in vitro-in vivo evaluation. Pharm Dev Technol. 2019. https://doi.org/10.1080/10837450.2017.1413658.
Kumar R, Sinha VR. Preparation and optimization of voriconazole microemulsion for ocular delivery. Colloids Surf B Biointerfaces. 2014. https://doi.org/10.1016/j.colsurfb.2014.02.007.
Calvo P, Vila-Jato JL, Alonso MJ. Comparative in vitro evaluation of several colloidal systems, nanoparticles, nanocapsules, and nanoemulsions, as ocular drug carriers. J Pharm Sci. 1996. https://doi.org/10.1021/js950474+.
Muchtar S, Abdulrazik M, Frucht-Pery J, Benita S. Ex-vivo permeation study of indomethacin from a submicron emulsion through albino rabbit cornea. J Control Release. 1997. https://doi.org/10.1016/S0168-3659(96)01503-9.
Schoenwald RD, Huang HS. Corneal penetration behavior of beta-blocking agents I: physiochemical factors. J Pharm Sci. 1983. https://doi.org/10.1002/jps.2600721108.
Dholakiya SL, Barile FA. Alternative methods for ocular toxicology testing: validation, applications and troubleshooting. Expert Opin Drug Metab Toxicol. 2013. https://doi.org/10.1517/17425255.2013.783013.
Wilson SL, Ahearne M, Hopkinson A. An overview of current techniques for ocular toxicity testing. Toxicology. 2015. https://doi.org/10.1016/j.tox.2014.11.003.
Üstündag-Okur N, Gökçe EH, Eğrilmez S, Özer Ö, Ertan G. Novel ofloxacin-loaded microemulsion formulations for ocular delivery. J Ocul Pharmacol Ther. 2014. https://doi.org/10.1089/jop.2013.0114.
Funding
This research was financially supported (Grant No. 9704192161) by the Hamadan University of Medical Sciences, Hamadan, I.R. Iran.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kassaee, S.N., Mahboobian, M.M. Besifloxacin-loaded ocular nanoemulsions: design, formulation and efficacy evaluation. Drug Deliv. and Transl. Res. 12, 229–239 (2022). https://doi.org/10.1007/s13346-021-00902-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-021-00902-z