Abstract
The involvement of recent technologies, such as nanotechnology and three-dimensional printing (3DP), in drug delivery has become the utmost importance for effective and safe delivery of potent therapeutics, and thus, recent advancement for oral drug delivery through 3DP technology has been expanded. The use of computer-aided design (CAD) in 3DP technology allows the manufacturing of drug formulation with the desired release rate and pattern. Currently, the most applicable 3DP technologies in the oral drug delivery system are inkjet printing method, fused deposition method, nozzle-based extrusion system, and stereolithographic 3DP. In 2015, the first 3D-printed tablet was approved by the US Food and Drug Administration (FDA), and since then, it has opened up more opportunities in the discovery of formulation for the development of an oral drug delivery system. 3DP allows the production of an oral drug delivery device that enables tailor-made formulation with customizable size, shape, and release rate. Despite the advantages offered by 3DP technology in the drug delivery system, there are challenges in terms of drug stability, safety as well as applicability in the clinical sector. Nonetheless, 3DP has immense potential in the development of drug delivery devices for future personalized medicine. This article will give the recent advancement along with the challenges of 3DP techniques for the development of oral drug delivery.

Graphical abstract
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Drug delivery refers to approaches, systems, technologies, and formulations that act as a medium of transport for the administration of therapeutics to be delivered to the body to exert its therapeutic effect. The area for drug delivery has expanded and advanced greatly over the years with a current focus on targeted delivery to improve the efficacy and safety profile of drugs [1, 2]. This development of drug delivery has garnered increasing attention as it can offer a highly personalized pharmaceutical treatment through tailored engineering release profiles [3].
Additive manufacturing or specifically 3DP is a revolutionary technology in pharmaceutical manufacturing as it opens up the possibility of creating limitless dosage forms that are equivalent to conventional drug fabrication methods in terms of product quality and efficacy [1, 4]. 3DP is a computer-aided technique, which constructs 3D solid objects from a digital file by the sequential deposition of several layers. It is capable of developing a range of drug delivery systems that covers from oral controlled-release systems, microchips, and drug implants to multiphase-release dosage forms, hence, underscoring 3DP technology as an essential tool to design both simple and complex customized drug delivery systems [4, 5].
The various 3DP technologies used in pharmaceutical manufacturing include fused deposition modeling (FDM), stereolithography (SLA), direct energy deposition, thermal inkjet printing (TIJ), and selective laser sintering (SLS) [3, 5]. For oral drug delivery, for instance, the utilization of these technologies exceeds the conventional manufacturing methods as they can bypass multiple steps, such as granulation, compacting, or coating, thereby enhancing the quality and efficacy of the formulation [6]. In addition to meeting the economics and standard quality demands, the utilization of 3DP in fabricating personalized pharmaceutical drug delivery systems offers the benefits of stability of multiple drugs within a single dosage dorm, precise dose of each drug and ideal release kinetic modulations [7, 8].
3DP in pharmaceutical technology aims to develop patient-centered dosage forms based on structure design, with research steering towards the creation of targeted-release drug delivery systems in free-form geometries [7, 9]. There are some researches investigating the dosage forms for topical administration such as salicylic acid anti-acne patch and 5-fluorouracil biodegradable patch [10, 11]. However, most extensive research mainly focuses on oral dosage forms, as it is one of the least invasive routes of administration among all types of dosage forms and generally meets patients’ compliance [12, 13]. The growing interest in utilizing various 3DP techniques is evident by the huge variety of 3D-printed products over the years, ranging from fast disintegrating tablets, extended-release tablets, and nanosuspension to polypill [14]. For instance, orodispersible paracetamol tablets can be manufactured using the SLS [15], whereas immediate-release theophylline tablets adopt the FDM technique [16].
The first FDA-approved 3D-printed tablet in the year 2015, Spritam (levetiracetam) manufactured by Aprecia Pharmaceuticals, incorporated large doses up to 1000 mg in a single dosage form which helps to improve the compliance of epileptic patients as it simplifies the administration of the drug [17]. This advancement perpetually imprints the milestone in 3D pharming and changes the outlook of the drug manufacturing field. Thus, this review will look into the challenges and perspectives of 3DP, current 3DP pharmaceutical technologies, upscale from patient home to production scale, and future prospects of 3DP in the context of oral drug delivery system.
Challenges and perspectives
The technological advancement of 3DP, intertwined with novel scientific concepts and interdisciplinary work, can offer boundless possibilities for meeting the needs of personalized drug therapy as well as addressing the issues related to poor drug delivery systems [7, 10]. However, there are a few limitations in the commercialization of 3DP in the market such as the high cost in developing new formulations or re-design of existing formulations through 3DP, selection of appropriate excipients, and maintenance of pharmaco-technical properties of final products. Although 3DP is a versatile technique that can incorporate many different kinds of pharmaceutical active ingredients, the compatibility of the drug and excipients must be established on a case-by-case basis to achieve stable physicochemical properties of a formulation [6, 18, 19].
Each of the many types of 3DP available has its own set of advantages and challenges. For example, the major challenges in exploiting stereolithography to manufacture customized drug products involve extensive regulatory issues and implementation of production models to efficiently produce individual therapeutic needs into small batches of drug products of standard quality [20]. Some 3DP technologies such as semi-solid extrusion (EXT), FDM, and powder-based (PB), which use nozzle mechanism to build layers, sequentially face the greatest challenge in maintaining reproducible and consistent flow due to the alternate stop-and-restart print head during the printing of a single or multiple products. PB 3DP, in particular, needs special laboratories for printing, as removal of excess powder that arise from problems such as clogging of nozzles in the printer head, binder migration, and improper powder feeding can be hazardous to health [21,22,23].
Different 3DP technologies produce 3D-printed tablets of different mechanical resistance. Although FDM can produce highly resistant tablets [24], PB and EXT yield products that have weaker structures as seen from their higher friability values (3.55%) in comparison to that of conventional tablets [1]. The flaw in the appearance of the finished products of 3DP is also more visible due to the stacking of plastic beads or large-sized powder and especially significant to products manufactured using EXT or PB techniques because of its long drying duration before they can be handled. As for FDM, its products are more prone to have seam lines between layers [1, 5, 25]. Nevertheless, according to a study by Pietrzak et al., the tablet morphology can be improved if methacrylic polymers are integrated and high resolution (100 μm layer thickness) is employed during 3DP of drugs [26].
Safety point of view is another aspect that needs careful consideration due to the built-in flexibility of 3DP equipment and wider opportunities for illegal printing of drug products, tampering, or adulteration of the dose and mix-up treatment regimens among patients. 3DP technologies can also significantly speed up the manufacturing process but there is a barrier to ensure safety, efficacy, and stability of the printed medicines as compared to conventional. Thus, it is expected that a broad-based application of 3DP in the pharmaceutical sector will be significantly affected by tight regulatory requirements to ensure the quality, safety, and efficacy of all the medicines produced. It will also be a great obstacle for the regulatory authorities to establish the guidelines, laws, tamper-proof strategies, and quality systems for use and consumption of 3D-printed medicines, given the stringent requirements of the pharmaceutical sector and the rapid evolving 3DP technologies [27].
Current 3D printing technologies in pharmaceutical drug delivery
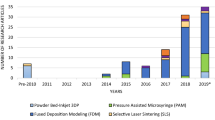
Several 3DP technologies have been developed over the years. Some commonly used methods (Fig. 1) are being briefly introduced below.
The various three-dimensional printing techniques. Reprinted with permission from Konta et al. [27]
Inkjet printing method
Inkjet printing method uses a powder base for the sprayed ink droplets; further, it hardens to form a solid. The active pharmaceutical ingredients and excipients of various combinations are sprayed precisely in the form of droplets onto a non-powder substrate [5]. There are two techniques in which this method can be performed, namely, the drop on demand and continuous jet method. In the continuous jet method, the droplets are constantly released from the sprayer to the substrate and only shifted towards the waste line when it is not needed which can account for unavoidable wastage. On the other hand, in the drop on demand, only a specific amount of droplets will be sprayed on the substrate [4]. Inkjet printing method has been applied for the manufacturing of felodipine solid dispersion and levofloxacin implant [28].
One of the major advantages of inkjet printing is its scalability to formulate, for instance, personalized medicine, drugs with complex release profiles, and a combination of multiple drugs into a single device with minimum waste and cost at high processing rate [29, 30]. Nevertheless, more studies to research on suitable printing techniques in the industrial scale should be established to enable scale up production of pharmaceuticals by inkjet printing [30].
Thermal inkjet printing method
Thermal inkjet printing (TIJ) uses the heat, produced from the microresistor when current is induced to vaporize the aqueous ink forming bubble that will coalesce, expand, and later be released from the nozzle as droplets [4]. One of the drawbacks of TIJ is the high temperature applied may potentially lead to degrade heat-labile active ingredients and excipients which limits its pharmaceutical use [31, 32]. However, the development of TIJ has enabled extemporaneous dispensing of some drugs onto 3D drug carriers [33]. Solid dosage forms of rasagiline mesylate and nanosuspension of folic acid are some formulations that are manufactured using this technique [34, 35]. These additive manufacturing processes are classified into seven distinct categories by the American Society for Testing and Materials group, which are as described hereafter [36].
Direct inkjet writing method
The direct inkjet writing method is useful to design complex solid dosage forms with finer sized structures and shapes without the requirement of exclusive equipment [4, 37]. This method uses a computer-controlled translational stage to move the ink deposition nozzle which then leads to the generation of layer by layer 3D microstructure [4, 33]. Several ink designs that can be utilized in this technique include dilute fluids, polymer melts, colloidal suspensions, and gels, which can be hardened to form solids by various methods like liquid evaporation and gelation [38].
Fused deposition method
FDM comprises polymer melting, extrusion, and layer by layer deposition before the solid dosage form is produced in which its shape is defined using the computer-aided design model [4, 33]. This method was invented and later patented by Scott Crump in 1989 with the intention to overcome the shortcomings of the inkjet printing method [4]. One of the advantages of FDM is the shape and pore size of the intended solid dosage form can be customized by modifying the various properties of raster [5]. FDM can be utilized to manufacture various solid dosage forms, such as implants, zero-order release tablets, multi-layered tablets, and fast dissolving tablets [4]. Some examples of FDM’s application are the formulation of extended-release patient-tailored prednisolone tablet and controlled-release budesonide tablet [39, 40].
Despite the downside of FDM which is the thermal degradation of heat-labile drugs, it can be overcome by the selection and usage of some other excipients, making FDM suitable for drugs of lower melting temperatures [41].
Pressure-assisted microsyringe (PAM)
The PAM method is similar to FDM, with the only difference in which the PAM method does not require the melting of materials. The principle of PAM is related to the release of viscous semi-liquid material using a syringe to produce the desired 3D model [42]. PAM 3D printer system is used to design and substantialize the diverse construction of 3D models. PAM technology utilizes a computer-controlled microsyringe, which provides the desired structure with the release of the dissolved polymer under consistent and low pressure [42, 43]. The subsequent processes include drying and solidification, which allow the dosage form to obtain sufficient physical strength.
Zip dose method
The zip dose method was first established by the Massachusetts Institute of Technology in the late 1980s. This method involves the application of aqueous fluid as a binding fluid to incorporate the layer of powder, which serves as a substrate [4]. A high porosity and drug-loading capacity solid dosage form of desired size and shape will be produced by repeating the process several times [4, 44]. Hence, this technique is useful to manufacture solid dosage form with a higher dose and requires a high disintegration rate [44]. For example, the zip dose method was applied to fabricate a personalized dose of levetiracetam, an antiepileptic drug [44].
Binder deposition method
In this method, liquid formulation serves as a binder. The ink is sprayed in the form of small droplets onto the powder bed, which consists of the active pharmaceutical ingredient and excipients at the optimum speed to produce the desired dosage form [45].
Material jetting method
In this process, a liquid formulation such as solution, suspension, or UV-curable resins is jetted from the printer rapidly which then hardens to form particles of desired size and shape. This technique is commonly used to produce microparticles as it has a droplet size of 100 mm, which accounts for its high resolution [46].
Powder bed fusion method
This is a fast and complex method which requires the fusion of high and low melting point binders using heat produced by a laser beam [45].
Stereolithography method
It uses UV light or other high energy light sources to cause polymerization of liquid photo-polymerizable resins [45]. This method was used for the manufacturing of salicylic acid anti-acne patch and modified-release tablet containing a combination of 4-aminosalicylic acid and paracetamol [10, 47].
3D printing for oral drug delivery
3DP technology is recently used to develop oral drug delivery devices as well as a dosage form for personalized therapy. 3D-printed drug-eluting devices offer the possibility for personalization in terms of shape, size, and architecture, but their clinical application has remained relatively unexplored [3]. In the pharmaceutical field, 3DP allows novel drug delivery systems to be manufactured. Single or multiple drugs can be incorporated in one tablet and the release pattern is controlled through the manipulation of the composition of the polymer. Drug release is controlled by the use of different polymer [48, 49], geometry [21], compartmentation [50, 51], or infill pattern [52, 53]. The personalization of the dose could allow the optimization of the dose considering the gender, age, weight, disease state, and genetic profile.
3D-printed oral drug delivery devices
3D printing mouth guard
The first-in-human study of a 3D-printed wearable oral delivery device was in the form of a mouth guard. It is the most astounding development of 3D-printed medicine as it allows coupling with 3D scanning technology that captures information about the patients’ anatomical features, which is useful in the production of a tailored device that precisely fits the size and geometrical requirements [10, 54]. The first human study was carried out in six volunteers to examine the feasibility of tailor-fitting vanillic acid (VA)-eluting mouth guards. In this study, the weight of the mouth guards within each group slightly decreased (< 10%) over time. The quantity of VA that remained in the mouth guards of horizontally sliced PVA (low) (HSPL) was 78%, vertically sliced PVA (high) (VSPH) was 54%, and horizontally sliced PVA (high) (HSPH) was 39%. The high remaining of PVA within the HSPL indicates that it has the longest release duration. The VA-loaded region showed concomitant whitening area after three cycles of wearing, following the release of VA in the saliva [3, 6].
A dissolution study was performed to understand the release kinetic of VA in the mouth (in vivo) compared to in vitro dissolution release. The results showed release of VA in mouth from mouth guard was rapid compared to in vitro dissolution release in apparatus. Similarly, the maximum time to release VA from HSPH, VSPH, and HSPL groups in in vitro condition was approximately 19 h, 21 h, and 57 h respectively. However, the VA release within 6 h in the mouth from the same device. The accelerated release of VA from the mouth guards in the mouth may be due to the perturbations generated by the constant tongue movements and the intense salivation [3].
Conventionally mouth guards were prepared by adopting the casting and molding method which is a time-consuming process [55, 56]. However, the making of mouth guards using 3DP techniques takes less than 2 h, starting from the intraoral scan to the final wearing of the customized mouth guard. Some volunteers complained about discomfort in wearing mouth guards, which may be due to the low resolution of FDM manufacturing [57]. Microfabrication nozzle alone or in combination with an electric field-guided ink dispenser can be used to improve the resolution of FDM manufacturing [58]. Compared with conventional formulations of topical gels that applied at high doses periodically, a drug-eluting mouth guard releases a small amount of drug over a long period of time. A drug-eluting mouth guard also enables specific targeting on the desired region for the release of the drug. Moreover, polymers such as poly(ε-caprolactone) and poly(N-vinylpyrrolidone) with lower melting temperatures ranging from 100 to 120 °C can be considered as they allow the incorporation of drugs with lower thermal stability [6].
Tablet-in-device
Tablet-in-device (TiD) is a combination of 3DP technologies with a novel gastric floating system to increase the gastric retention time, achieve sustained release, and improve bioavailability. A compressed tablet was inserted into a TiD system, which is a 3D-printed device made from polylactic acid (PLA) filaments. Placing the compressed tablet into a TiD system hinders the rapid drug release and also resists acidic condition [21, 39, 59,60,61,62]. These devices consist of two parts: a body and a cap.
Two types of TiD systems are created and applied in vivo: single-net TiD and double-net TiD (Fig. 2). Drugs loaded in both TiD systems show better floating ability in the stomach with long-term gastric retention as compared to drugs without TiD system. To build an acid-resistant TiD system, PLA filament is selected as the building material as it maintains its rigidity in 0.1 mol/L HCl solution even after 3 h [63].
Illustrations of two types of TiD systems: single-net TiD (a) and eccentric double-net TiD (d) and the assembly of them (b, c, e, f). Reprinted with permission from Fu et al. [63]
A study of riboflavin loaded into the two types of TiD system was carried out to compare the release pattern of riboflavin with and without TiD system. The low viscous hydrophilic polymer, HPMC E5, was used in producing the riboflavin tablet. The release of 75% of riboflavin tablets was at 10 h without the incorporation of TiD system (naked riboflavin tablet). Riboflavin tablet loaded in a single-net TiD system was shown a longer duration of release as compared to the naked riboflavin tablet in which the cumulative release of riboflavin in single-net TiD system is less than 19% after 72 h. The differences in the drug release duration between naked tablets and drug-loaded in a single-net TiD system is that the single-net TiD system provided a barrier effect to the riboflavin tablet which inhibited the swelling of the HPMC E5 polymer and the diffusion of formed slurries even after 72 h [63]. Riboflavin tablet that was loaded in a double-net TiD system showed a shorter release duration of riboflavin in which approximately 27% cumulative release was achieved within 28 h. However, riboflavin tablets loaded in the double-net TiD system had slower release duration as compared to the naked riboflavin tablet as the 75% cumulative release was achieved at around 50 h. Thus, it can be concluded that the drugs loaded in both TiD systems showed better floating ability in the stomach as compared to drugs without TiD system. Optimization of tablet formulations associated with floating devices enables the achievement of long-term controlled-release loaded drugs by oral routes which failed to be achieved in the conventional oral sustained-release systems [63]. Another advantage of the TiD system is that the design is independent, leading to a broader way of modification such as bioadhesive and osmotic pump can be added to the TiD system in the future.
Printfill
Printfill is formed using FDM and injection volume filling (IVF) printing systems. This combination of techniques enables the easier incorporation of drug or excipient liquid systems to the extended scaffold at room temperature (Fig. 3). FDM is able to form an architecture designed by computer software (example CAD) by squeezing appropriate filament through the hot nozzle of a 3D printer.
Digital design of printfills with drug represented by red points and the enteric polymer represented as green ones. Reprinted with permission from Linares et al. [64]
The combination of FDM technology with HME during the intermediate process can overcome its major drawbacks of low drug-loading property and the inability of thermosensitive drug printing. FDM technology offers accurate manufacturing of 3D-printed scaffolds system that can hold the content from IVF and helping to control the drug release. This provides many possibilities in different dosage forms. The experimental results for dimensions of the formulation are similar to the theoretical results which indicate that this method helps in the addition of pH-sensitive polymer without an additional process as a fluid bed [64].
Besides, the availability of dual or multiple extruder 3D printers allows the production of tablets with different drug profiles [8, 21]. Two types of the tablet were printed by Linares et al.: theophylline with enteric polymer and without enteric polymer. The enteric polymer acts as a pH-sensitive polymer, which allows theophylline to specifically release at the colon with alkaline pH. After 2 h under pH 1.2, the tablet printed with enteric polymer released only 2.3% theophylline. When the solution pH increased to 7.5, drug release increased to 50% after 2 h and 80% after 8 h. However, tablet printed without enteric polymer shows rapid drug release as compared to tablets printed with enteric polymer [64]. In in vitro studies, the perfect sealing of the scaffold and the homogenous layer obtained with the delaying release polymer contribute to the ability for colon-specific drug delivery of the performed printfills [8, 21].
3D-printed oral drug delivery (non-device)
3DP allows the approach of personalized medication, instead of treating every individual using a single type of drug [65, 66]. This revolution is achieved by tailoring the drug according to patients’ needs and preferences, such as modifying the shape, size, strength, dosage, and release characteristics, and also producing multi-drug combinations [53, 65, 66]. For example, once-a-day fixed dose combinations help in addressing the poor compliance issues related to the high daily number of prescribed therapeutics and dosing regimen complexity. Before the fabrication, important information such as active ingredient, release kinetics and administration mode needed to be identified promptly.
3DP is carried out as follows: design and create a dosage form using computer-aided design software, blend the selective drug(s) and polymer(s) and load the mixture into a 3D printer. The 3D dosage form is then constructed in the layer by layer manner according to the design requirement [2].
Tuberculosis (TB) is a lethal and infectious disease that usually required at least 6 months of combination drug therapy [67], recommended by the World Health Organization to ensure effective treatment. Rifampicin (RIF) and isoniazid (ISO) are both first-line medications for TB, which is well absorbed in the stomach and intestine, respectively [68, 69]. However, RIF is shown to be unstable when ISO is dissolved in the gastric environment [70], thus impairing its bioavailability in combination therapy. This dual-compartmental dosage unit (dcDU) was designed in silico by CAD and prepared in two steps firstly outer PVA shell manufacturing by 3DP and subsequent fabrication of drug-containing filament by HME. This dcDU was designed in a cylindrical shape with a separate wall, composed of water-insoluble PLA [51].
The two compartments enable the isolation of RIF and ISO to modulate their release. Both active ingredients are blended with PEO at a 70:30 (w/w) ratio separately with a batch size of 4 g, then hot-melt extruded into high-dose filaments to produce 0.7–0.9 mm diameters filaments that could fit into the apertures of the cylinder. HME allows an accurate and dust-free drug loading to be obtained. Furthermore, PVA water-soluble cap is selectively printed at the end of one compartment. As the cap is expected to dissolve after 1–2 h, thus delaying the release of its content after the oral administration. On the other hand, the drug-loaded in the unsealed compartment was expected to release immediately after ingestion. A dcDU shows delay dissolution and absorption for a drug in different compartments, allowing RIF and ISO delivery in a single dosage form without drug interaction in both in vitro and in vivo studies (Fig. 4). It also provides environmental protection to both drugs, providing a more prominent effect on the drug release kinetics, shown in in vitro studies [51].
The model of a dual-compartmental dosage unit (dcDU). Reprinted with permission from Genina et al. [51]
In another experiment, domperidone (DOM) was selected for making 3DP-based dosage form. DOM is dopamine (D2) receptor antagonist used to treat nausea and vomiting caused by gastroenteritis, chemotherapy, and radiotherapy [71, 72]. It is an insoluble weak base (pKa1 = 7.8, pKa2 = 11.5) that has low solubility in a neutral and alkaline environment, making its oral bioavailability reported in the range of 13–17% due to incomplete absorption and first-pass metabolism [72, 73]. Besides, the drug needs to be taken three times a day due to its short elimination half-life of 7.5 h [72]. To increase its bioavailability and minimize the frequency of intake, FDM-based 3DP technology is used to fabricate an intragastric floating sustained delivery for DOM.
DOM was the first hot-melt extruded into hydroxypropyl cellulose (HPC) filament. A hollow-structured tablet (Fig. 5) was designed that showed a rigid outer shell of HPC led to slow solvent penetration and release inner loaded drugs after a lag phase of 2 h [74]. The filaments were then printed into hollow-structured tablets by changing the shell numbers (1, 2, 3, and 4) and the infill percentages (0%, 10%, 20%, and 30%). Additional shell adds on weight and strength, while infill percentage generates the tablets from complete hollow to fully solid filled, which affects the floating ability of the tablet without significantly influencing the release rates of tablets [75].
In vitro studies showed that the floating capacity is highly correlated to the floating density. The higher the density, the shorter the floating time (Table 1). The BaSO4-labeled tablets were observed in Fig. 6 to stay in the stomach for 8 h, became fuzzy and indistinct at 10 h (Fig. 6e), and finally disappeared at 12 h (Fig. 6f). In vivo pharmacokinetic studies on the rabbits showed the relative bioavailability of the floating sustain release (FSR) tablets compared with reference commercial tablets (Motilium) was 222.49 ± 62.85% [75]. Except for Cmax, all the parameters had increased in the FSR tablets.
a–f X-rays indicating the positions of the BaSO4-labeled DOM-floating sustain release tablets in the gastrointestinal tract of New Zealand rabbits at different time points. X-rays are taken at a 2 h, b 4 h, c 6 h, d 8 h, e 10 h, and f 12 h. Reprinted with permission from Chai et al. 2017 [75]
In conclusion, the fabrication of the DOM-FSR tablet with a hollow structure confirmed that the buoyancy of tablets was closely related to their densities. Prolonged floating and release were observed both in vitro and in vivo. The feasibility of fabricating intragastric drug delivery device by FDM holds high potential to develop a rapid and low-cost platform utilized for drug screening and personalized medical care.
Additionally, researchers chose metformin and glimepiride with different dosage regimens and daily dosing [76, 77] as well as different absorption sites in the gastrointestinal tract (GIT) [78, 79]. In order to allow co-administration, 3DP is used to manufacture a bilayer dosage form containing two drugs to patients’ daily dosage regimens. Incorporation of two drugs with different release patterns will improve patient compliance and reduce the frequency of medication intake as well as medication cost [80].
Metformin was embedded in Eudragit® RL sustained-release layer with a different percentage of composition, while glimepiride was mixed with the PVA layer. Both API were mixed until homogenization was achieved. A flat cylindrical with smoothed edges (pill-shaped) which consists of two layers were designed and produced via FDM 3D printers. The upper layer contained water-soluble glimepiride-loaded PVA while the lower part consisted of the metformin-loaded sustained-release layer, composed of the below-described filaments (Fig. 7) [81].
Graphical illustration of bilayer oral solid dosage production containing metformin and glimepiride. Reprinted with permission from Gioumouxouzis et al. [81]
Dissolution studies revealed that 100% of the metformin was dissolved after 480 min with dosage forms deriving from filament produced with the single-screw extruder. For dosage forms produced from the twin-screw extruder, metformin released slightly slower with 91.76% and 86.98% release after 540 and 480 min, respectively. 87.04% of glimepiride was dissolved after 75 min, and the dissolution reached a plateau of 91.31% after 120 min [81]. The formulation was concluded to be successful, as the release of the APIs was complete within the desirable absorption margins, which was 2–3 h for glimepiride and 8 h for metformin [79, 82, 83]. Thus, FDM may be used to develop two-compartment antidiabetic formulation that combines immediate-release glimepiride and sustained-release metformin, making co-administration and once-daily dosing of the two regimens feasible.
Since personalized medicines are to be produced on demand, non-destructive characterization techniques can be considered. To investigate the final product quality, destructive tests such as high-performance liquid chromatography (HPLC) and UV spectroscopy assays that are expensive require a highly skilled operator and samples from a large batch are usually performed. However, quality control and safety in 3DP drugs are yet to be well established.
Based on a research carried on paracetamol-loaded 3D-printed cylindrical tablets composed of an acrylic polymer (Eudragit L100-55), the use of process analytical technologies (PAT) with “point-and-shoot” approach and the evaluation of drug content and drug distribution shows excellent linearity (R2 = 0.996) and accuracy (RMSEP = 0.63%), providing a transformative approach to support the integration of 3DP into clinical pharmacy practice [84].
The most common method used for tablet production is usually direct compression [85]. However, there are certain limitations for direct compression, including low drug loading in tablets, a high portion of excipients [85,86,87], segregation, and dust contamination [85]. For example, compression of 500 mg paracetamol requires 800 mg of excipients to produce a formulation of 1300 mg. This might lead to patient incompliance as tablets in larger sizes are difficult to swallow and may even cause choking [85,86,87]. Therefore, an extrusion-based 3DP was used to fabricate a formulation of immediate-release high drug-loading paracetamol oral tablets with an API of 80% (w/w). In this case, paste-based extrusion 3DP process was used as it applies to a wider range of drugs, allows higher drug loading, and also avoids possible drug degradation caused by the high temperatures and UV irradiation used in FDM and UV curing-based inkjet methods, respectively [87, 88].
Paracetamol powder was ground to achieve particles less than 100 μm diameter, then mixed with various composition with different percentage composition, forming a paste. The paste was filled in a syringe cartridge in the 3D printer and extruded layer by layer with a 100% infill percentage until the desired tablet dimension was reached.
In vitro release data of paracetamol 3D tablet reveals the immediate release of the drug (> 90%) within 10 min. Moreover, no change in physical form was observed in XRD and DSC after the fabrication of tablets from extrusion-based 3DP. Paracetamol 3D tablet also passed all the pharmacopeia quality tests such as hardness, weight variation, friability, and disintegration. This concludes that the 3D extrusion-based printing method for tablet production can produce quality tablets with current USP standards [89].
Budesonide is a corticosteroid drug used as slow-release capsules, often used in treating inflammatory bowel disease (IBD) [71, 90]. Budesonide possesses a strong affinity for corticosteroid receptors and features both potent topical anti-inflammatory effects and low systemic bioavailability [91]. The aim to fabricate a new budesonide dosage form is to achieve appropriate dissolution kinetics. PVA filament was ground into a fine powder that can be sifted through a sieve with a mesh size of 1000 μm. Two grams of budesonide 5% w/w was manually mixed with 38 g of PVA powder and then extruded into filaments. FDM printer was used to fabricate the rounded hard capsule-shaped tablets with budesonide containing filament. The tablets were then coated with a solution containing Eudragit1 L100 powder and a mixture of 97% isopropanol. The coat of Eudragit1 L100 was intended to produce a gastro-resistant product [40].
Two commercial budesonide products named Entocort1 and Cortiment1 (Uceris1) were evaluated for dissolution in a dynamic dissolution bicarbonate buffer system. The Cortiment1 showed slow and delayed release in the upper small intestine; however, Entocort1 has rapidly released budesonide in the same region. On the other hand, 3D-printed caplet formulation showed sustain release profile starting from the mid-small intestine to colon [40]. This reveals the potential of fabricating modified-release oral dosage form using FDM 3DP technologies.
3DP associated with the use of PAM is beneficial in manufacturing tablets with prolonged drug release profiles with both sufficient mechanical strength and stable floating capability [43]. To achieve extended and stable controlled-release drug with the gastric retentive property, a combination of 3DP and gastro-retentive drug delivery systems was established. With this study, a PAM-linked computer with a commercial pressure-assisted syringe 3D printer was used to fabricate the ginkgolide tablets. The fabricated 3D-printed tablets with the specific parameters were established under a different range of parameters [43]. The FTIR spectra of pure drug present a characteristic peak at 1780.7 cm−1 (–C=O, conjugative effect, ring tension effect) [92]. For the 3D-printed ginkgolide tablet, a characteristic peak at 1782.8 cm−1 can also be found and no new peak was observed. The conclusion can be drawn as there was no major change in the significant functional group that indicated there was no chemical interaction between excipient and drug during the printing process. The floating lag time of the ginkgolide tablet is shorter and stable even in different pH environments when compared to a conventional tablet. The floating ability of the ginkgolide tablet relies on air trapped in a matrix structure, which helps the tablet to float from the very beginning even without an acidic pH environment. The 3D-printed tablets possessed satisfactory 10–12 h in vitro and 8–10 h in vivo gastro-retention property and exhibited constant 10–12 h of controlled-release ability. The diversity of release profiles may be attributed to the difference in the inner structure [43].
The PAM method is beneficial in manufacturing tablets like ginkgolide tablet with prolonged drug release profile, sufficient mechanical strength, and stable floating capability. Besides, during the preparation and printing process, no chemical interaction was observed between the drug and excipients. 3DP is a reliable technique in the manufacturing of controlled-release oral dosage form by alteration of 3D inner structure [43].
Production of smaller batches by using 3DP is considered as cost-effective and it plays an important role in individualized drug therapy [19, 93, 94]. The intention of the formulation is to create a 3D-printed oral drug with a variable release profile including immediate and controlled-release patterns with sufficient drug-loading property. Production of drug-loaded material was 3D-printed into 6, 8, and 10 × 2.5 mm tablets. These with 15% and 90% infill levels by utilizing HME 30% (w/w) ISO was formulated with single or multiple modified polymers with oral drug delivery property [95]. The prepared formulations which are composed of HPC were found to show excellent printability. HPC is a good printable material for 3DP which was evident by the majority of printable filaments contained 40–65% (w/w) HPC (EF or HF). However, HPMC in the range of 40–60% (w/w) was found to be an unsuitable polymer for the formulation. In this study, all prepared filament showed low moisture uptake at low humidity while high moisture uptake at a higher relative humidity (RH), which is typical for all starch-based and cellulose polymers. The increase in mass (%) at low RH (30% RH and 60% RH) was small, between 0.33 and 0.71%. However, in high RH (90%), the moisture uptake of all filaments was rapidly intensified. The maximum weight increased of filament in this study is 45.78%. Filament with greater total moisture uptake ability under high humidity conditions shows bad printability. In this study, filaments that have breaking distance (toughness) of less than 1.5 mm showed high brittleness when loaded into the 3D printer while filaments with higher breaking distance showed good printability [95].
The drug release profile can be further affected by altering the size of particles, geometrical structure, surface area to volume ratio, or infill level of the printed tablets. An 80% drug release of ISO was observed between 40 and 852 min from the 8 mm printed tablet that has 90% infill. The formulation contains PEO showed the most rapid drug release as PEO is hydrophilic polymer able to hydrate rapidly to form a gel-like layer that may facilitate the release of drugs. Besides, the formulation containing HPC HF polymer showed the most sustained drug release profile, which did not complete 100% release in 24 h sampling time. This is due to HPC HF polymer has a high molecular weight (MW = 1,150,000) which typically used in the manufacturing of controlled-release drugs with the range of 15–35% (w/w). Moreover, the effect of tablet size on drug release was not prominent. However, it is observed that 10 mm tablet released the drug the slowest, while 6 mm tablet the fastest, which may be attributed to the tablets’ surface area. Thus, the higher the surface area to volume ratio showed a more rapid drug release profile [96].
The versatile properties of 3D-printed tablets in vitro drug release highlight the possibility to adjust dosage form and drug release depending on the patient’s need. This 3DP technology is able to present the personalization in the manufacturing of oral dosage form by adjustable drug properties [95].
3DP is beneficial to simplify the early development works of various dosage forms, for instance, in preparation of modified-release dosage forms for rapid prototyping which is beneficial to the preclinical studies. 3DP is used to fabricate PVA capsule shells, which is an erosion-based polymer. The 3D-printed capsule of lamivudine was designed for delay burst release by controlling the thickness of the capsule shell. These delayed-release capsules of lamivudine showed regional absorption in preclinical studies [97].
The induction time of drug release from the cavity can be controlled within 12 to 198 min by adjusting printed capsule shell thicknesses. The dissolution test was carried out to observe the impact of PVA capsule thicknesses on the drug release profile. For APIs filled 1-, 3-, and 5-wall capsules, the increasing burst times were 17.5 ± 1.7 to 62.1 ± 4.6 to 162.1 ± 4.2 min respectively. In addition, the 85% release times were 7.4 ± 2.7 to 15.3 ± 3.7 and 32.9 ± 13.3 min correspondingly. Hence, it indicated that the effect of increased capsule shell thicknesses delayed release of the drug. Besides, in vivo drug release was observed in a regional study of the dog GIT, where 3-wall and 7-wall API filled capsules were used. The in vivo Tlag of the immediate-release formulation was as expected which is less than 15 min while 45 and 105 min for 3- and 7-wall capsuled respectively. The in vivo Tlag of 3D-printed capsules were approximately half of the burst delay times in vitro, 62.1 and 197.5 min respectively.
Factors such as API variation, dosage forms, dissolution media, viscosity, and print conditions determine the dissolution of the printed capsule. These results provide a platform for prediction and interrogation of the regional permeability in GIT through the different thicknesses of capsule wall and separate release profile. Thus, 3D-printed drug product provides quick pharmacokinetics reads as part of the on-site formulation tool kit, decreasing the overall timeline of pharmaceutical development [97].
Fast dissolving oral films (FDFs) is an alternative approach to allow the fast dissolution of the drug without water requirement. This advantage served the purpose of increasing consumer acceptance. However, to include taste-masking excipient in the formulation using FDFs is a challenging task. To overcome this, single-layered FDF (SLFDF) or multi-layered FDF (MLFDF) films fabricated by the FDM method allowed the drug layer to be covered with the taste-masking layer [61]. The filaments were prepared containing polyethylene oxide (PEO) or PVA with paracetamol or ibuprofen as model drugs and strawberry powder as a taste-masking layer [98].
Mass spectroscopy analysis and HPLC indicated the stability of active ingredients during the film preparation process. 3D-printed FDFs in DSC thermograms also suggested miscibility of the excipient and active ingredients, where the weight uniformity of 3D-printed FDFs was greater than 97% with content uniformity of between 106 and 112.4%, which fulfills the requirement stated in the British Pharmacopeia (85–115%) [99]. Besides, the thickness variation within a single film was less than 4% [98].
The thicknesses of SLFDFs can be as thin as 197 ± 21 mm, and thicknesses of MLFDFs are starting from 298 ± 15 mm. Only mesh films have short disintegration time among 3D FDFs. Mesh SLFDFs presented disintegration time as short as 42 ± 7 s and 48 ± 5 s for mesh MLFDFs, based on the formulation and design [98]. In this study, glipizide as the treatment of diabetes was selected as a model drug. By utilizing the HME method, the glipizide was loaded into commercial PVA filaments [100]. Then, dual-nozzle 3DP was used to print the drug-loaded filaments to form a double-chamber glipizide dosage form known as DuoTablet. DuoTablet demonstrates a smaller tablet (internal chamber) within a larger tablet (external chamber). Each chamber of this device contains different glipizide concentrations which allow a controlled or delayed release of glipizide [100,101,102].
The final drug-loading rates of two filaments of the glipizide PVA were 2.2% and 4.8%, respectively, which were successfully produced via HME. However, there was reduction of filament property of formability for 3DP when attempting to incorporate higher drug loading which is more than 5%. Furthermore, the result of a thermal analysis indicated that in the temperature range during both printing and extruding process, glipizide was thermally stable. In the temperature range, the mass loss of drug-loaded filament was 6% w/w and 0.1% w/w mass loss for the raw material [59].
The in vitro dissolution tests of DuoTablet performed a 5-h controlled-release profile that highlights its potential to modulate the drug release by different ratios of the drug in different layers. In this device, drug incorporated in the internal compartment will not be released until the external layer is dissolved practically and releases the drug in the external layer first (Fig. 8). During the first 2 h of the dissolution, almost 90% of the drug in the external layer was released. In addition, through a dissolution test, a lag time of approximately 85 min was required for the release of drugs in the internal compartment. This lag time was mainly depending on the polymer used in the formulation and the uniformity and thickness of the external layer. This study suggested a promising approach of FDM 3DP technology in the development of a controlled-release drug delivery system with multiple concentration distribution of drugs [59].
From production scale to patient home
In this scientific community, introducing 3DP of medications into pharmaceutical compounding should not be a difficult task. Due to the fact of producing a superb quality of API-loaded filament and database with objects to print, fused deposition modeling seems to have the easiest approach to the pharmaceutical compounding in the pharmacies. Allied health professionals such as pharmacists are able to take advantage of this versatile 3DP method to print the complex shaped dosage form with defined architectures in a cost-effective way [6].
3DP of medications in patients’ facilities is no longer a strange term and somehow it is being extensively discussed among the diverse network of interacting scientists. Self-printing medications can be clinically beneficial for patients on medical care as higher involvement will be given throughout the treatment process. FDM-based 3D printer is ideal for personal use due to the fact that they are affordable and are available in open source that can be easily built by anyone. Thermoplastic materials in the form of filament are usually used in FDM 3D printers as starting materials to be fed into the printer. Various forms of printable filaments are available in the market, and it is obtained from several pharmaceutical-grade polymers such as PEO, cellulose derivatives, ethylene-vinyl acetate, and others [103,104,105]. There are several advantages of the FDM method, which include the production of defined crystalline shape as well as stable amorphous drug. The stability issues of amorphous drugs can be overcome due to the mechanism involved such as evaporation of the solvent from the drug solution in a short amount of time and melting process of active pharmaceutical ingredients together with the polymer [106].
Despite the advantages that can be brought by the FDM printer for the patient to self-print their medications at home, it still seems impossible for the patient to print their own medications at home as this additive manufacturing technique is rather advanced for the community. The quality of drug manufactured and the safety issues of drug printed at home will be considered as the two main challenges for the implementation of this method. Besides that, time-consuming training on the operation of the printer needs to be provided by the professionals to the patients accordingly to minimize the risk of quality defects during the printing process. On the other hand, 3DP of drugs will lead to some drawbacks, such as the risk of combining multiple active pharmaceutical ingredients within one formulation by patients without accessing the adverse effects of the polypills formulated [1].
The vision of introducing the 3DP technique into the pharmaceutical industry as a common manufacturing method seems far away from reality due to the fact that there is an insufficiency of ready-made production machinery available in the market. However, Aprecia® Pharmaceuticals, the world’s first and only pharmaceutical manufacturer that is validated by FDA, has set the trend by developing the first marketed drug production using 3DP. In this advanced pharmaceutical printing technology, by feeding liquid on a conveyor, repeated cycles of building layers are carried out to form tablets [5]. It is certain that without the development of machinery specifically for pharmaceutical applications, 3DP will remain in the research phase instead of proceeding to the pharmacotherapeutic applications [8]. Tranfield et al. emphasized that in order to develop an ideal 3D printer with excellent quality, it is essential to have the collaboration between 3D printer manufacturers, professional excipient suppliers, scientists, and pharmaceutical regulators [9].
One of the good points of 3DP in the industry is the low labor cost. 3DP removes the tedious process which requires numerous people to operate multiple machines and forming a production line to create a product. 3D printer only requires an operator to start the machine and a series of automated processes will be carried out by the printer in producing the ideal product. Hence, it requires low labor costs as no skilled machinists or operators are required to be part of the production team [107].
The conventional manufacturing methods required plenty of researches to produce a perfect product before testing the acceptability of the product in the market. One of the potential advantages of 3DP is the ability to produce a prototype in a short period of time and test it before launching to the market. Creating a prototype in a short period of time through 3DP allows a business to obtain frequent feedback from potential investors that cannot be achieved through traditional manufacturing methods. This is because 3DP enables the prototypes to be altered and customized more rapidly and frequently to improvise the product and make it satisfiable to the potential buyer. Therefore, 3DP could be able to provide an enhanced competitive advantage by delivering better products in a shorter space of time and enable the testing of the product before launching to the market [108].
On the other side, 3DP technology is not always the right choice for product development as it brings certain disadvantages. One of the disadvantages is that 3DP equipment and materials which require higher cost than conventional drug production. The initial expenses of using the technology are very high as the industrial-grade 3D printers itself costs hundreds of thousands of dollars. In addition, plastic filaments used in 3D printers can cost up to $25 to $45 per kilogram. Still, with the current increasing trend of technology development, it is to believe that the price of 3D printer and its materials might be lowered in the future. In June 2013, the Chinese Government committed approximately $245 million to drive advancements in 3DP. If the commitment continues, the 3DP might be affordable to the community in the future [107, 109].
Another dark side about 3DP is that there is a lack of legislation and regulations to control manufacturing and production in the industry. For example, the product can be counterfeit or do not meet the minimum requirement of quality. All of these low-quality products could be achieved with ease, at reduced costs and at a faster rate via 3DP technology. Thus, 3DP can become a potential advantage to the counterfeiters but may bring harm to the consumer. Despite the effort by lawmakers in regulating the 3D-printed products, there is still a lack of regulation in the 3D manufacturing devices. One suggestion that can be made to control the 3D manufacturing devices is to consider the declaration and registration of 3DP devices to become compulsory, restrict the blueprints’ dissemination, and also introduce software limitations on items that can be printed [108].
Conclusion and future prospects
In conclusion, 3DP technology opens the opportunity for the customization of an advanced drug delivery system for an individual. Ever since the FDA approved the manufacturing of 3DP technology, the studies on the development of oral dosage form have expanded rapidly. 3DP allows the manufacturing of oral drug delivery devices that enhances the solubility and release of a poorly soluble drugs. With the current trend of 3DP applications in the drug delivery system, it is possible that the combination of conventional pharmaceutical technologies with 3DP will be implemented in the future to expand the areas of application of 3DP. Such hybrid systems will combine the proven effectiveness of conventional pharmaceutical technologies with the benefits of 3DP in order to create a patient-centric yet low material wastage of oral drug delivery systems. The additional advantages of the 3DP drug delivery device should be applied to the development of pediatric and geriatric oral dosage forms to ensure the desired release rate and to achieve the maximum therapeutic effect. Even though the stability, quality, and applicability of 3DP drug delivery devices are the major challenges now, it is to be believed that with patience and perseverance, 3DP will continue to develop and improve to be a safe and effective pharmaceutical formulation in the future considering regulatory requirement.
References
Moulton SE, Wallace GG. 3-dimensional (3D) fabricated polymer based drug delivery systems. J Control Release. 2014;193:27–34.
Trenfield SJ, Awad A, Goyanes A, Gaisford S, Basit AW. 3D printing pharmaceuticals: drug development to frontline care. Trends Pharmacol Sci. 2018;39:440–51.
Liang K, Carmone S, Brambilla D, Leroux J-C. 3D printing of a wearable personalized oral delivery device: a first-in-human study. Sci Adv. American Association for the Advancement of Science [cited 2019 Jul 12]. 2018;4:eaat2544. https://doi.org/10.1126/sciadv.aat2544.
Bansal M, Sharma V, Singh G, Harikumar SL. 3D printing for the future of pharmaceuticals dosages forms. Int J Appl Pharm. 2018; 1–7.
Katakam P, Dey B, Assaleh FH, Hwisa NT, Adiki SK, Chandu BR, et al. Top-down and bottom-up approaches in 3D printing technologies for drug delivery challenges. Crit Rev Ther Drug Carrier Syst. 2015;32:61–87 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25746205.[cited 2018 Jul 13].
Jamróz W, Szafraniec J, Kurek M. Jachowicz R. 3D printing in pharmaceutical and medical applications—recent achievements and challenges. Pharm Res . Springer. 2018;35:176.
Afsana JV, Haider N, Jain K. 3D printing in personalized drug delivery. Curr Pharm Des. 2019;24:5062–71 Available from: http://www.ncbi.nlm.nih.gov/pubmed/30767736. [cited 2019 Jul 15].
Norman J, Madurawe RD, Moore CMV, Khan MA, Khairuzzaman A. A new chapter in pharmaceutical manufacturing: 3D-printed drug products. Adv Drug Deliv Rev. 2017;108:39–50.
Osouli-Bostanabad K, Adibkia K. Made-on-demand, complex and personalized 3D-printed drug products. Bioimpacts. 2018;8:77–9 Tabriz University of Medical Sciences; Available from: http://www.ncbi.nlm.nih.gov/pubmed/29977828. [cited 2019 Jul 15].
Goyanes A, Det-Amornrat U, Wang J, Basit AW, Gaisford S. 3D scanning and 3D printing as innovative technologies for fabricating personalized topical drug delivery systems. J Control Release. 2016;234:41–8.
Yi H-G, Choi Y-J, Kang KS, Hong JM, Pati RG, Park MN, et al. A 3D-printed local drug delivery patch for pancreatic cancer growth suppression. J Control Release. 2016;238:231–41 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27288878. [cited 2019 Jul 15].
Pandey M, Choudhury H, Yeun OC, Yin HM, Lynn TW, Tine CLY, et al. Perspectives of nanoemulsion strategies in the improvement of oral, parenteral and transdermal chemotherapy. Curr Pharm Biotechnol. 2018;19:276–92.
Choudhury H, Gorain B, Chatterjee B, Mandal UK, Sengupta P, Tekade RK. Pharmacokinetic and pharmacodynamic features of nanoemulsion following oral, intravenous, topical and nasal route. Curr Pharm Des. 2017;23.
Zeeshan F, Madheswaran T, Pandey M, Gorain B. Three-dimensional (3-D) printing technology exploited for the fabrication of drug delivery systems. Curr Pharm Des. 2018;24:5019–28.
Fina F, Goyanes A, Gaisford S, Basit AW. Selective laser sintering (SLS) 3D printing of medicines. Int J Pharm. 2017;529:285–93. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28668582.Accessed 15 July 2019.
Solanki NG, Tahsin M, Shah AV, Serajuddin AT. Formulation of 3D printed tablet for rapid drug release by fused deposition modeling: screening polymers for drug release, drug-polymer miscibility and printability. J Pharm Sci. 2018;107:390–401. [cited 2019 Jul 15]. https://doi.org/10.1016/j.xphs.2017.10.021.
First 3D-printed pill. Nat Biotechnol. 2015;33:1014 Available from: http://www.nature.com/articles/nbt1015-1014a. [cited 2019 15].
Ishengoma FR, Mtaho AB. 3D printing: developing countries perspectives. Int J Comput Appl. 2014. Available from: https://pdfs.semanticscholar.org/c251/6eba4c2c1d3254ac33c413d52f7ea79f8be4.pdf
Palo M, Holländer J, Suominen J, Yliruusi J, Sandler N. 3D printed drug delivery devices: perspectives and technical challenges. Expert Rev Med Devices. 2017;14:685–96.
FDA approves the first 3D printed drug product. Aprecia Pharm [Internet]. The Economic Times. 2015. http://www.multivu.com/players/English/7577251-aprecia-pharmaceuticals-spritam/. Accessed 15 July 2019.
Goyanes A, Robles Martinez P, Buanz A, Basit AW, Gaisford S. Effect of geometry on drug release from 3D printed tablets. Int J Pharm. 2015;494:657–63.
Prasad LK, Smyth H. 3D printing technologies for drug delivery: a review. Drug Dev Ind Pharm. Taylor & Francis. 2016 [cited 2019 Jan 7];42:1019–31. https://doi.org/10.3109/03639045.2015.1120743.
Ani Jose P, Christoper PG. 3D printing of pharmaceuticals—a potential technology in developing personalized medicine. Asian J Pharm Res Dev. 2018;6:46–54 Available from: http://ajprd.com. [cited 2019 Jul 15].
Okwuosa TC, Pereira BC, Arafat B, Cieszynska M, Isreb A, Alhnan MA. Fabricating a shell-core delayed release tablet using dual FDM 3D printing for patient-centred therapy. Pharm Res. 2017;34:427–37 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27943014. [cited 2019 Jul 15].
Muley S, Nandgude T, Poddar S. Extrusion–spheronization a promising pelletization technique: in-depth review. Asian J Pharm Sci. 2016;11:684–99 Available from: https://www.sciencedirect.com/science/article/pii/S1818087616300721. Elsevier;[cited 2019 Jul 15].
Pietrzak K, Isreb A, Alhnan MA. A flexible-dose dispenser for immediate and extended release 3D printed tablets. Eur J Pharm Biopharm. 2015;96:380–7 Elsevier; [cited 2019 Jul 15]. Available from: https://www.sciencedirect.com/science/article/pii/S0939641115003306.
Konta A, García-Piña M, Serrano D. Personalised 3D printed medicines: which techniques and polymers are more successful? Bioengineering. 2017;4:79 [cited 2019 Jul 15]Available from: http://www.ncbi.nlm.nih.gov/pubmed/28952558.
Scoutaris N, Alexander MR, Gellert PR, Roberts CJ. Inkjet printing as a novel medicine formulation technique. J Control Release. 2011;156:179–85.
Boehm RD, Miller PR, Daniels J, Stafslien S, Narayan RJ. Inkjet printing for pharmaceutical applications. Mater Today. Elsevier Ltd. 2014;17:247–52.
Daly R, Harrington TS, Martin GD, Hutchings IM. Inkjet printing for pharmaceutics—a review of research and manufacturing. Int J Pharm. Elsevier B.V. 2015;494:554–67.
Buanz ABM, Saunders MH, Basit AW, Gaisford S. Preparation of personalized-dose salbutamol sulphate oral films with thermal ink-jet printing. Pharm Res. 2011 [cited 2018 Jul 13];28:2386–92. https://doi.org/10.1007/s11095-011-0450-5.
Meléndez PA, Kane KM, Ashvar CS, Albrecht M, Smith PA. Thermal inkjet application in the preparation of oral dosage forms: dispensing of prednisolone solutions and polymorphic characterization by solid-state spectroscopic techniques. J Pharm Sci. 2008;97:2619–36.
Merits and uses of 3DP in pharmaceutical drug delivery.
Genina N, Janßen EM, Breitenbach A, Breitkreutz J, Sandler N. Evaluation of different substrates for inkjet printing of rasagiline mesylate. Eur J Pharm Biopharm. 2013;85:1075–83.
Pardeike J, Strohmeier DM, Schrödl N, Voura C, Gruber M, Khinast JG, et al. Nanosuspensions as advanced printing ink for accurate dosing of poorly soluble drugs in personalized medicines. Int J Pharm. 2011;420:93–100.
KM S, Kulsum JU. 3D printing: a new avenue in pharmaceuticals. World J Pharm Res. 2016;5:1686–701.
He Y, Wu Y, Fu JZ, Gao Q, Qiu JJ. Developments of 3D printing microfluidics and applications in chemistry and biology: a review. Electroanalysis. 2016;1658–78.
Lewis JA. Direct ink writing of 3D functional materials. Adv Funct Mater. John Wiley & Sons, Ltd. 2006;16:2193–204.
Skowyra J, Pietrzak K, Alhnan MA. Fabrication of extended-release patient-tailored prednisolone tablets via fused deposition modelling (FDM) 3D printing. Eur J Pharm Sci. 2015;68:11–7.
Goyanes A, Chang H, Sedough D, Hatton GB, Wang J, Buanz A, et al. Fabrication of controlled-release budesonide tablets via desktop (FDM) 3D printing. Int J Pharm. 2015;496:414–20.
Kollamaram G, Croker DM, Walker GM, Goyanes A, Basit AW, Gaisford S. Low temperature fused deposition modeling (FDM) 3D printing of thermolabile drugs. Int J Pharm.Elsevier. 2018;545:144–52.
Goole J, Amighi K. 3D printing in pharmaceutics: a new tool for designing customized drug delivery systems. Int J Pharm. 2016;499:376–94.
Wen H, He B, Wang H, Chen F, Li P, Cui M, et al. Structure-based gastro-retentive and controlled-release drug delivery with novel 3D printing. AAPS PharmSciTech. Springer International Publishing. 2019;20:68.
Aprecia Pharmaceuticals. FDA approves the first 3D printed drug product. 2015
Gibson I, Rosen D, Stucker B (Brent). Additive manufacturing technologies: 3D printing, rapid prototyping, and direct digital manufacturing.
BO G, GV S, SB K, DR C, GS A, GP S. 3D Printing in pharmaceutical manufacturing: opportunities and challenges. Int J Bioassays. 2016;5:4723.
Wang J, Goyanes A, Gaisford S, Basit AW. Stereolithographic (SLA) 3D printing of oral modified-release dosage forms. Int J Pharm. 2016;503:207–12.
Alhijjaj M, Belton P, Qi S. An investigation into the use of polymer blends to improve the printability of and regulate drug release from pharmaceutical solid dispersions prepared via fused deposition modeling (FDM) 3D printing. Eur J Pharm Biopharm Elsevier. 2016;108:111–25.
Khaled SA, Burley JC, Alexander MR, Roberts CJ. Desktop 3D printing of controlled release pharmaceutical bilayer tablets. Int J Pharm. 2014;461:105–11 Available from: http://linkinghub.elsevier.com/retrieve/pii/S0378517313010144. [cited 2018 Jul 13].
Maroni A, Melocchi A, Parietti F, Foppoli A, Zema L, Gazzaniga A. 3D printed multi-compartment capsular devices for two-pulse oral drug delivery. J Control Release. 2017;268:10–8.
Genina N, Boetker JP, Colombo S, Harmankaya N, Rantanen J, Bohr A. Anti-tuberculosis drug combination for controlled oral delivery using 3D printed compartmental dosage forms: from drug product design to in vivo testing. J Control Release. 2017;268:40–8.
Kyobula M, Adedeji A, Alexander MR, Saleh E, Wildman R, Ashcroft I, et al. 3D inkjet printing of tablets exploiting bespoke complex geometries for controlled and tuneable drug release. J Control Release. 2017;261:207–15.
Sadia M, Arafat B, Ahmed W, Forbes RT, Alhnan MA. Channelled tablets: an innovative approach to accelerating drug release from 3D printed tablets. J Control Release. 2018;269:355–63.
Muwaffak Z, Goyanes A, Clark V, Basit AW, Hilton ST, Gaisford S. Patient-specific 3D scanned and 3D printed antimicrobial polycaprolactone wound dressings. Int J Pharm. 2017;527:161–70.
Pae A, Yoo R-K, Noh K, Paek J, Kwon K-R. The effects of mouthguards on the athletic ability of professional golfers. Dent Traumatol. 2013;29:47–51.
Nakajima K, Takeda T, Kawamura S, Shibusawa M, Nara K, Kaoru N, et al. A vacuum technique to increase anterior thickness of athletic mouthguards to achieve a full-balanced occlusion. Dent Traumatol. John Wiley & Sons, Ltd (10.1111). 2008;24:50–2.
Yamada A, Niikura F, Ikuta K. A three-dimensional microfabrication system for biodegradable polymers with high resolution and biocompatibility. J Micromechanics Microengineering. IOP Publishing. 2008;18:25035.
Zhang B, Seong B, Nguyen V, Byun D. 3D printing of high-resolution PLA-based structures by hybrid electrohydrodynamic and fused deposition modeling techniques. J Micromechanics Microengineering. IOP Publishing. 2016;26:25015.
Li Q, Wen H, Jia D, Guan X, Pan H, Yang Y, et al. Preparation and investigation of controlled-release glipizide novel oral device with three-dimensional printing. Int J Pharm. 2017;525:5–11.
Goyanes A, Kobayashi M, Martínez-Pacheco R, Gaisford S, Basit AW. Fused-filament 3D printing of drug products: microstructure analysis and drug release characteristics of PVA-based caplets. Int J Pharm. 2016;514:290–5.
Goyanes A, Buanz ABM, Hatton GB, Gaisford S, Basit AW. 3D printing of modified-release aminosalicylate (4-ASA and 5-ASA) tablets. Eur J Pharm Biopharm. 2015;89:157–62 Available from: http://linkinghub.elsevier.com/retrieve/pii/S0939641114003580. [cited 2018 Jul 13].
Tagami T, Fukushige K, Ogawa E, Hayashi N, Ozeki T. 3D printing factors important for the fabrication of polyvinylalcohol filament-based tablets. Biol Pharm Bull. 2017;40:357–64.
Fu J, Yin H, Yu X, Xie C, Jiang H, Jin Y, et al. Combination of 3D printing technologies and compressed tablets for preparation of riboflavin floating tablet-in-device (TiD) systems. Int J Pharm. Elsevier. 2018;549:370–9.
Linares V, Casas M, Caraballo I. Printfills: 3D printed systems combining fused deposition modeling and injection volume filling. Application to colon-specific drug delivery. Eur J Pharm Biopharm. Elsevier. 2019;134:138–43.
Alhnan MA, Okwuosa TC, Sadia M, Wan K-W, Ahmed W, Arafat B. Emergence of 3D printed dosage forms: opportunities and challenges. Pharm Res Springer US. 2016;33:1817–32.
Awad A, Trenfield SJ, Gaisford S, Basit AW. 3D printed medicines: a new branch of digital healthcare. Int J Pharm. 2018;548:586–96.
WHO | Global tuberculosis report 2018. WHO World Health Organization; 2019.
Gallo GG, Radaelli P. Rifampin. Anal Profiles Drug Subst. Academic Press. 1976;5:467–513.
Mariappan TT, Singh S. Regional gastrointestinal permeability of rifampicin and isoniazid (alone and their combination) in the rat. Int J Tuberc Lung Dis. 2003;7:797–803.
Shishoo CJ, Shah SA, Rathod IS, Savale SS, Vora MJ. Impaired bioavailability of rifampicin in presence of isoniazid from fixed dose combination (FDC) formulation. Int J Pharm. 2001;228:53–67.
O’Shaughnessy K. BMA new guide to medicine & drugs. 9th ed. London: Dorling Kindersley; 2015.
Reddymasu SC, Soykan I, McCallum RW. Domperidone: review of pharmacology and clinical applications in gastroenterology. Am J Gastroenterol. 2007;102:2036–45.
Nagarsenker MS, Garad SD, Ramprakash G. Design, optimization and evaluation of domperidone coevaporates. J Control Release. 2000;63:31–9.
Melocchi A, Parietti F, Loreti G, Maroni A, Gazzaniga A, Zema L. 3D printing by fused deposition modeling (FDM) of a swellable/erodible capsular device for oral pulsatile release of drugs. J Drug Deliv Sci Technol. 2015;30:360–7.
Chai X, Chai H, Wang X, Yang J, Li J, Zhao Y, et al. Fused deposition modeling (FDM) 3D printed tablets for intragastric floating delivery of domperidone. Sci Rep. Nature Publishing Group. 2017;7:2829.
Hwang Y-C, Kang M, Ahn CW, Park JS, Baik SH, Chung DJ, et al. Efficacy and safety of glimepiride/metformin sustained release once daily vs. glimepiride/metformin twice daily in patients with type 2 diabetes. Int J Clin Pract. John Wiley & Sons, Ltd (10.1111). 2013;67:236–43.
BNF. 74th ed. BMJ Group and the Royal Pharmaceutical Society of Great Britain; 2014.
McCreight LJ, Bailey CJ, Pearson ER. Metformin and the gastrointestinal tract. Diabetologia. Springer Berlin Heidelberg 2016;59:426–35.
Ning X, Sun J, Han X, Wu Y, Yan Z, Han J, et al. Strategies to improve dissolution and oral absorption of glimepiride tablets: solid dispersion versus micronization techniques. Drug Dev Ind Pharm. 2011;37:727–36.
Paes AH, Bakker A, Soe-Agnie CJ. Impact of dosage frequency on patient compliance. Diabetes Care American Diabetes Association. 1997;20:1512–7.
Gioumouxouzis CI, Baklavaridis A, Katsamenis OL, Markopoulou CK, Bouropoulos N, Tzetzis D, et al. A 3D printed bilayer oral solid dosage form combining metformin for prolonged and glimepiride for immediate drug delivery. Eur J Pharm Sci. 2018;120:40–52.
Song R. Mechanism of metformin: a tale of two sites. Diabetes Care. American Diabetes Association; 2016;39:187–189.
Metformin hydrochloride extended-release tablets type of posting notice of intent to revise posting date. 2018.
Trenfield SJ, Goyanes A, Telford R, Wilsdon D, Rowland M, Gaisford S, et al. 3D printed drug products: non-destructive dose verification using a rapid point-and-shoot approach. Int J Pharm. Elsevier. 2018;549:283–92.
Gohel MC, Jogani PD. A review of co-processed directly compressible excipients. J Pharm Pharm Sci. 2005;8:76–93.
African Journal of Pharmacy and Pharmacology. Academic Journals; 2007.
Khaled SA, Burley JC, Alexander MR, Yang J, Roberts CJ. 3D printing of tablets containing multiple drugs with defined release profiles. Int J Pharm. 2015;494:643–50 Available from: http://linkinghub.elsevier.com/retrieve/pii/S0378517315300855. [cited 2018 Jul 13].
Okwuosa TC, Stefaniak D, Arafat B, Isreb A, Wan K-W, Alhnan MA. A lower temperature FDM 3D printing for the manufacture of patient-specific immediate release tablets. Pharm Res. 2016;33:2704–12.
Khaled SA, Alexander MR, Wildman RD, Wallace MJ, Sharpe S, Yoo J, et al. 3D extrusion printing of high drug loading immediate release paracetamol tablets. Int J Pharm. 2018;538:223–30.
McConnell EL, Liu F, Basit AW. Colonic treatments and targets: issues and opportunities. J Drug Target. 2009;17:335–63.
Gionchetti P, Praticò C, Rizzello F, Calafiore A, Capozzi N, Campieri M, et al. The role of budesonide-MMX in active ulcerative colitis. Expert Rev Gastroenterol Hepatol Taylor & Francis. 2014;8:215–22.
Wang W, Kang Q, Liu N, Zhang Q, Zhang Y, Li H, et al. Enhanced dissolution rate and oral bioavailability of Ginkgo biloba extract by preparing solid dispersion via hot-melt extrusion. Fitoterapia. 2015;102:189–97.
Jamroz W, Kurek M, Lyszczarz E, Brniak W, Jachowicz R. Printing techniques: recent developments in pharmaceutical technology. Acta Pol Pharm. 2017;74:753–63.
Lim SH, Kathuria H, Tan JJY, Kang L. 3D printed drug delivery and testing systems—a passing fad or the future? Adv Drug Deliv Rev. 2018;132:139–68.
Öblom H, Zhang J, Pimparade M, Speer I, Preis M, Repka M, et al. 3D-Printed isoniazid tablets for the treatment and prevention of tuberculosis—personalized dosing and drug release. AAPS PharmSciTech. Springer International Publishing. 2019;20:52.
Solutions F. POLYOXΚ™ water soluble resins combining flexibility with consistency.
Smith D, Kapoor Y, Hermans A, Nofsinger R, Kesisoglou F, Gustafson TP, et al. 3D printed capsules for quantitative regional absorption studies in the GI tract. Int J Pharm. 2018;550:418–28.
Ehtezazi T, Algellay M, Islam Y, Roberts M, Dempster NM, Sarker SD. The application of 3D printing in the formulation of multilayered fast dissolving oral films. J Pharm Sci Elsevier Ltd. 2018;107:1076–85.
Home—British Pharmacopoeia. 2017.
Goyanes A, Wang J, Buanz A, Martínez-Pacheco R, Telford R, Gaisford S, et al. 3D printing of medicines: engineering novel oral devices with unique design and drug release characteristics. Mol Pharm American Chemical Society. 2015;12:4077–84.
Patil H, Tiwari RV, Repka MA. Hot-melt extrusion: from theory to application in pharmaceutical formulation. AAPS PharmSciTech. 2016;17:20–42.
Shah S, Repka MA. Melt extrusion in drug delivery: three decades of progress. New York: Springer; 2013. p. 3–46.
Jamróz W, Kurek M, Łyszczarz E, Szafraniec J, Knapik-Kowalczuk J, Syrek K, et al. 3D printed orodispersible films with aripiprazole. Int J Pharm. Elsevier. 2017;533:413–20.
Genina N, Holländer J, Jukarainen H, Mäkilä E, Salonen J, Sandler N. Ethylene vinyl acetate (EVA) as a new drug carrier for 3D printed medical drug delivery devices. Eur J Pharm Sci. Elsevier. 2016;90:53–63.
Melocchi A, Parietti F, Maroni A, Foppoli A, Gazzaniga A, Zema L. Hot-melt extruded filaments based on pharmaceutical grade polymers for 3D printing by fused deposition modeling. Int J Pharm. Elsevier. 2016;509:255–63.
Qi S, Craig D. Recent developments in micro- and nanofabrication techniques for the preparation of amorphous pharmaceutical dosage forms. Adv Drug Deliv Rev. Elsevier. 2016;100:67–84.
Attaran M. The rise of 3-D printing: the advantages of additive manufacturing over traditional manufacturing. Bus Horiz. Elsevier. 2017;60:677–88.
Gebhardt A, Hötter J-S, Gebhardt A, Hötter J-S. Rapid prototyping. Addit Manuf Hanser. 2016:291–352.
Pîrjan A, Petroşanu D-M. The impact of 3d printing technology on the society and economy. J Inf Syst Oper Manag. Romanian-American University. 2013;7:360–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pandey, M., Choudhury, H., Fern, J.L.C. et al. 3D printing for oral drug delivery: a new tool to customize drug delivery. Drug Deliv. and Transl. Res. 10, 986–1001 (2020). https://doi.org/10.1007/s13346-020-00737-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-020-00737-0