Abstract
Background
MTBH, a novel hesperetin derivative, possesses in vivo hepatoprotective effects against carbon tetrachloride (CCl4)-induced acute liver injury in Institute of Cancer Research (ICR) mice.
Objectives
This study investigated the pharmacokinetics and tissue distribution of MTBH and its conjugated metabolites in rats after a single dose of MTBH.
Methods
Male Sprague–Dawley (SD) rats were orally administered (25, 50, 100 mg/kg) or intravenously administered (25 mg/kg) MTBH and blood samples were withdrawn at specific times. Moreover, after a single oral dose of MTBH (200 mg/kg), tissues (heart, liver, spleen, lung, kidney, stomach, intestine, brain and muscle) were collected at scheduled time points.
Results
The concentration of MTBH in plasma and tissues was assayed by HPLC before and after hydrolysis with β-glucuronidase or sulfatase. The glucuronides/sulfates were extensively present in the plasma, moreover, the free form was detectable in the plasma, but in a small amount equivalent to nearly 0.85–1.46 % of the amount of glucuronides/sulfates, the absolute bioavailability of MTBH was approximately 31.27 %. In tissues, the free form appeared in all tissues examined, with trace amount in brain and muscle, and considerable concentration in stomach and lung. Glucuronides/sulfates were the major forms in intestine, kidney and liver, whereas not detectable in heart, brain and muscle. The liver and intestine were found likely to accumulate MTBH at a high concentration among all tissues.
Conclusions
The free form of MTBH was present in the circulation and all assayed organs, whereas its glucuronides/sulfates were the major forms in plasma and intestine, kidney and liver after a single dose.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Free-form MTBH was present in plasma and all assayed organs. |
MTBH glucuronides and sulfates were the major forms in plasma, intestine, kidney and liver. |
MTBH-O-glucuronide and MTBH-O-sulfate but not MTBH-O-sulphoglucuronides were the main conjugated metabolites of MTBH in vivo. |
The absolute bioavailability of MTBH was increased compared with hesperetin. |
1 Introduction
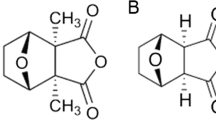
Hesperetin, which is derived from the hydrolysis of hesperidin (hesperetin 7-O-β-rutinoside) is a flavonoid abundant in citrus fruits and derived products such as juices [1]. Hesperetin can be absorbed by the colonocytes [2] via proton-coupled active transport and transcellular passive diffusion (colon) and then extensively metabolized by UDP-glucuronosyltransferases and sulfotransferases producing glucuronidated and/or sulfated compounds [3]. On the other hand, hesperetin and hesperetin 7-glucoside are directly absorbed by enterocytes (intestine) [4, 5]. Hesperetin exhibits various pharmacological properties related to antioxidant and free radical scavenging [6–8], anti-inflammatory [9, 10], antiviral [11], blood lipid lowering [12, 13] and anticarcinogenic activities [14]. It has been shown to inhibit chemically induced urinary bladder [15], mammary [16] and colon carcinogenesis [17, 18] in laboratory cells and animals. In addition, it is also used for the treatment of hemorrhoids [19] and in the prevention of postoperative thromboembolism [20]. In spite of this wide range of therapeutic efficacy, its poor water solubility, poor oral bioavailability, shorter half-life and rapid clearance of hesperetin from the body restrict its wide use as a potent phytomolecule. Study reported that the elimination half-life (t 1/2) of hesperetin is 1.78 h in rats [21] and 3.12 h in healthy human subjects [22]. Thus, to maintain the therapeutic levels for longer duration, frequent administration would be necessary. In our previous studies, to overcome these disadvantages above, a series of hesperetin derivatives were synthesized and the anti-inflammatory activity was evaluated. It was found that MTBH (8-methylene-tert-butylamine-3′,5,7-trihydroxy-4′-methoxyflavanone, Fig. 1) can significantly inhibit the expression of interleukin-6 (IL-6) and tumor necrosis factor-a (TNF-α) induced by lipopolysaccharide (LPS) in RAW264.7 cell than its parent compound hesperetin. In addition, we further found that MTBH has apparent hepatoprotective effects on CCl4-induced acute hepatic injury by markedly decreasing the activities of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) in ICR mouse (our unpublished data).
Despite our in vitro and in vivo bioactivities of MTBH conducted thus far, its pharmacokinetic behavior and tissue distribution remained unknown, which has hindered its further development. To improve our understanding of the mechanism of action of MTBH, it is necessary to know which metabolites are present in the body and in which tissues and organs they are found. The purposes of this study were to investigate the dose-dependent pharmacokinetics of MTBH and its conjugated metabolites after oral administration of MTBH (25, 50, and 100 mg/kg) and to evaluate its absolute bioavailability by comparing with intravenous (I.V.) injection of 25 mg/kg MTBH, the tissue distribution of MTBH and its conjugated metabolites after oral administration of 200 mg/kg MTBH was also studied in rats.
2 Materials and Methods
2.1 Chemicals and Reagents
Hesperetin (Xi’an grass plant technology Co., Ltd, purity >98 %, Lot No. XC1009018), hesperidin (National Institutes for Food and Drug Control, purity >99 %, Lot No. 110721-200613) was used as internal standard (IS), 8-methylene-tert-butylamine-3′,5,7-trihydroxy-4′-methoxyflavanone (MTBH, purity >97 %, Fig. 1) was synthesized and purified by Professor jing-bo Shi (School of Pharmacy, Anhui Medical University, Hefei, China). Acetonitrile, methanol and formic acid were chromatographic grade and purchased from Merck (Darmstadt, Germany). β-Glucuronidase from Escherichia coli (type IX-A, Lot: SLBD7403V) and Sulfatase from Helix pomatia (type H-1, Lot: SLBK3653V) were purchased from Sigma (St Louis, MO, USA). Deionized water was made by a Milli-Q® academic ultrapure water purification system supplied by Millipore (Shanghai, China) filtered through a 0.22-μm filter. All other chemicals and solvents used were of analytical grade.
2.2 Animals
Male SD rats, weighing 280–320 g, were obtained from the Animal Breeding Center of Anhui Medical University. The animal protocol was approved by the Animal Ethics Committee of Anhui Medical University (animal ethics approval number: 20140342). The rats were housed in a room with controlled temperature (22 ± 2 °C) and humidity (50 ± 5 %) and a 12-h light–dark cycle prior to the study. All rats were fasted 12 h and freely accessed to water before dosing and fasting continued for another 3 h.
2.3 HPLC Analysis of MTBH
The Shimadzu HPLC system consisted of a LC-20AD pump, a SIL-20AC auto sampler, a CTO-20A column oven and a SPD-10AVP UV detector. All the modules were controlled by a CBM-20A communications bus module (Tokyo, Japan). A Phenomenex Luna C18 column (250 mm × 4.6 mm, 5 μm) and a C18 precolumn (4 × 2 mm) kept at 35 °C were used to separate the MTBH and the IS. Separation was performed with a gradient elution program at the flow rate of 1.0 mL/min with the ultraviolet detection wavelength at 288 nm. The mobile phase was acetonitrile (solvent A) and formic acid water (0.5 %, solvent B). The gradient elution program was: 76 % A (0–5 min), 76–30 % A (5–15 min), 30–76 % A (15–16 min), 76 % A (16–24 min). The retention times of hesperidin and MTBH were 7.7 and 9.0 min, respectively. The method was fully validated according to FDA guidelines for specificity, linearity, precision, accuracy, lower limit of quantitation (LLOQ), recovery and stability.
2.4 Preparation of Standard Solutions and Quality Control Samples
An appropriate amount of MTBH was dissolved in acetonitrile to make a stock solution of 1.0 mg/mL. The stock solution was serially diluted with acetonitrile to get the working standard solutions at the desired concentrations: 0.5, 1, 2, 5, 10, 20, 50, 100, 200 and 400 μg/mL. Hesperidin was dissolved in acetonitrile to provide a stock solution of 1.0 mg/mL, and diluted with ethyl acetate to a final concentration of 0.05 and 0.1 µg/mL, respectively. All samples were stored at 4 °C until use. 5 μL of working standard solutions was added to 50 μL blank plasma (or 40 μL of working standard solutions was added to 400 μL blank tissue homogenates) to give calibration standards at concentrations of 0.05, 0.1, 0.2, 0.5, 1, 2, 5, 10, 20 and 40 µg/mL for plasma and tissues. For the validation of the method, quality control (QC) samples at three concentrations of 0.09, 1.6, and 32 µg/mL for plasma and tissues were prepared separately in the same fashion and stored at −20 °C until analysis.
2.5 Drug Administration, Blood and Tissue Collection
In the pharmacokinetic study, a total of 40 SD rats were randomly divided into four groups with 10 rats each. MTBH was prepared using 0.5 % (w/v) sodium carboxymethyl cellulose (CMC-Na) or a polyethylene glycol 400 (PEG400):propanediol:ethanol:water = 35:35:10:25 mixtures for preparation of oral and I.V. solutions. After an overnight fasting, Groups 1, 2 and 3 were administrated at a single dose of 25, 50 and 100 mg/kg via oral administration, respectively. Group 4 was administrated at a single dose of 25 mg/kg via I.V. injection. Blood sample (approximately 0.5 mL) was collected from the supraorbital vein into heparinized tubes at different time points (0, 7, 15, 30 min, 1, 1.5, 2, 3, 5, 7, 9, 12, 15, and 24 h following oral administration, or 0, 5, 10, 15, 20, 30 min, 1, 1.5, 2, 3, 5, 7, 9, 12, 15 and 24 h following I.V. injection). The plasma was separated by centrifugation at 3000g for 15 min and then stored at −20 °C until analysis.
In the tissue distribution study, a total of 66 SD rats were randomly divided into eleven groups with 6 rats each; the rats were killed prior to (0 h) and at 0.5, 1, 1.5, 2, 4, 6, 8, 12, 16 and 24 h after a single oral dose of 200 mg/kg MTBH using carbon dioxide. At each time point (6 rats each), blood samples were withdrawn, then systemically perfused with cool normal saline. Then, the heart, liver, spleen, lung, kidney, stomach, intestine, brain and skeletal muscle were collected, washed with normal saline, blotted dry with filter paper and weighed. The tissues were chopped and homogenized in normal saline under constant cooling, and the homogenates were stored at −20 °C until analysis.
2.6 Sample Treatment
Calibrators, QCs, real plasma samples and tissue homogenates were thawed and vortex-mixed thoroughly for 30 s. The plasma samples were spiked with 10 µL of sodium acetate buffer (0.1 mol/L, pH 5.0) and 10 µL of ascorbic acid (200 mg/mL), then acidified with 5 µL formic acid, and extracted with 500 µL of ethyl acetate (containing 0.1 µg/mL of hesperidin as the IS). The tissue homogenates were added 80 µL of sodium acetate buffer (0.1 mol/L, pH 5.0) and 80 µL of ascorbic acid (200 mg/mL), then acidified with 40 µL formic acid, and extracted with 2000 µL of ethyl acetate (containing 0.05 µg/mL of hesperidin as the IS). After vortex-mixing for 3 min and centrifugation at 14,000g for 15 min, aliquots of the organic phase were carefully transferred to another tube and evaporated under nitrogen gas to dryness at 37 °C. The residues were dissolved in 100 μL of the mobile phase followed by vortex-mixing and centrifugal filtration (0.22 µm filter unit); the filtrate (50 µL) was analyzed using HPLC.
2.7 Quantitation of MTBH and its Conjugated Metabolites in Plasma and Tissues
The concentrations of MTBH glucuronides or total conjugates (glucuronides plus sulfates) in plasma were quantified from the amount of corresponding aglycone (MTBH) liberated from the conjugated metabolites by hydrolysis with β-glucuronidase or sulfatase (containing β-glucuronidase), individually. Plasma was divided into three aliquots (50 µL of each fraction). The conditions of hydrolysis are described in the following: for hydrolysis by β-glucuronidase, 50 µL aliquot of plasma was incubated with 10 µL of β-glucuronidase (1000 unit/mL, in 0.1 mol/L sodium acetate buffer, pH 5.0) and 10 µL of ascorbic acid (200 mg/mL) for 4 h at 37 °C; for hydrolysis by sulfatase/β-glucuronidase, 50 µL aliquot of plasma was incubated with 10 µL of sulfatase (1000 unit/mL, containing 39,861 unit/mL of β-glucuronidase, in 0.1 mol/L sodium acetate buffer, pH 5.0) and 10 µL of ascorbic acid (200 mg/mL) for 4 h at 37 °C. The concentrations of MTBH glucuronides or total conjugates in tissue homogenates were analyzed according to the method described above except the volume of tissue homogenates and enzyme buffer was 400 and 80 µL, respectively. For free-form MTBH determination, plasma or tissue homogenates was subjected to the method described above except for the addition of enzyme-free buffer and without incubation with β-glucuronidase or sulfatase. The samples were further processed as described in 2.6 and analyzed by HPLC.
2.8 Identification of MTBH Conjugated Metabolites using TOF LC–MS
Identification of MTBH conjugated metabolites was performed on an Agilent 1260 Series Rapid Resolution LC system comprising a HPLC pump, a PDA detector scanning from 250 to 700 nm, and an autosampler cooled to 4 °C, together with an Agilent 6224 ESI/TOF mass spectrometer (Agilent Technologies, CA, USA). The mobile phase consisted of A, acetonitrile and B, 0.1 % formic acid water at a flow rate of 0.4 mL/min using a Phenomenex Luna C18 column (150 mm × 4.6 mm, 3 μm) maintained at 35 °C. The gradient elution program was: 5 % A (0–5 min), 5–50 % A (5–20 min), 50–50 % A (20–28 min), 5 % A (28–31 min). An aliquot (10 μL) of sample was injected for each analysis. A scan from m/z 50–1000 for 31 min was carried out using electrospray positive mode. Extracted ion chromatograms were generated for each of the conjugated metabolites. Spectra were obtained by background subtraction from the summed spectra under the chromatographic peak of interest. The spectra contain cation adducts, the abundant molecular ion and, owing to in-source collision-induced dissociation, a fragment that is either MTBH or demethylated MTBH, thus providing mass spectral identification.
2.9 Data Analysis
The pharmacokinetic parameters of MTBH were calculated by a noncompartment model using WinNonLin version 5.0.1 (Pharsight). The peak plasma concentration (C max) and the time to peak concentration (T max) were taken directly from experimental data. The elimination rate constant (k) was obtained by means of linear regression analysis of the semi-logarithmic plasma concentration–time curve and the t 1/2 was calculated as 0.693/k e. The area under the plasma concentration–time curve from 0 to the last measurable concentration at time t (AUC0–t) was calculated by the trapezoidal rule. All the results were expressed as the mean ± SD. Statistical comparisons of the pharmacokinetic parameters were analyzed using paired Studentʼs t test or one-way ANOVA with the Scheffe test, respectively. P values <0.05 was considered statistically significant. All statistical analyses were performed using SPSS 17.0.
3 Results
3.1 Qualitative Analysis of Plasma and liver
The greatest amounts of conjugated metabolites of MTBH were seen in the liver, therefore, extracts of samples of this tissue were subjected to confirmatory analysis by Agilent TOF LC–MS. Plasma and liver of rats that received MTBH were analyzed by directly deproteinization with methanol in a ratio of 1:3 (plasma or liver homogenates: methanol) without hydrolysis, three main species were detected in plasma or liver homogenates (Fig. 2). One was characterized by m/z 564 (retention time, RT 11.1 min), consistent with MTBH-O-glucuronide. One species with m/z 388 eluting at the RT of 11.9 min was consistent with MTBH molecular ion [MTBH+H]+. One species with m/z 468 eluting at the RT of 13.9 min was consistent with MTBH-O-sulfate.
HPLC-PDA-MS analysis of MTBH conjugated metabolites in rat plasma and liver. Chromatograms represent gradient reversed-phase HPLC analysis of plasma and liver collected 1 h after oral administration of 200 mg/kg MTBH. Representative chromatograms of (a, e) plasma or liver sample with a PDA detector at 288 nm, and plasma or liver sample with extracted ion chromatograms (b, f) Peak 1, m/z 564, consistent with MTBH-O-glucuronides, c, g peak 2, m/z 388, consistent with MTBH molecular ion [MTBH+H]+, d, h peak 3, m/z 468, consistent with MTBH-O-sulfate. Insets show positive-ion ESI spectra for each metabolite
3.2 Pharmacokinetics Study
The calibration curve of MTBH in plasma showed good linearities (r > 0.99) in the range of 0.05–40.0 µg/mL. Validation of this assay method indicated that all coefficients of variation for intra-day and inter-day analysis were below 9.7 %, and the relative standard deviations (RSD) were less than 13.0 %, indicating good precision and accuracy. The recovery of MTBH from plasma was 85.55–90.73 % at 0.09, 1.6 and 32 µg/mL. The LLOQ and limit of detection (LOD) of MTBH were 0.05 and 0.02 µg/mL, respectively. The results of autosampler (4 °C, 24 h), room temperature (25 °C, 12 h), temperature at 37 °C (4 h), three freeze–thaw cycle (−20 to 25 °C) and long-term (−20 °C, 30 days) stability indicated that the MTBH was stable under various storage conditions since the bias in three levels (0.09, 1.6, and 32 µg/mL) was within ± 13.4 % of their nominal values (data not shown). The typical HPLC chromatograms are shown in Fig. 3. The retention times of hesperidin and MTBH were 6.7, and 11.2 min, respectively. No endogenous interference was found at these retention times for processed blank rat plasma samples or liver homogenates, indicating the high selectivity of this HPLC method.
Representative chromatograms of a standard mixture, b blank rat plasma, and plasma collected at 1 h post-dose c before hydrolysis, and d after hydrolysis with β-glucuronidase or e sulfatase/β-glucuronidase; f blank rat liver, and liver collected at 1 h post-dose g before hydrolysis, and h after hydrolysis with β-glucuronidase or i sulfatase/β-glucuronidase. 1 hesperidin, 2 MTBH
Previous studies indicated that hesperetin is found in human plasma and urine almost exclusively as its conjugated form, glucuronides and sulphoglucuronides [4]. In our study, the concentrations of free form, glucuronides and glucuronides/sulfates of MTBH in plasma and tissue homogenates were determined before and after hydrolysis with β-glucuronidase or sulfatase/β-glucuronidase, respectively. The mean plasma concentration–time profiles of free form, glucuronides and glucuronides/sulfates of MTBH are shown in Fig. 4, and the relevant pharmacokinetic parameters of free form, glucuronides and glucuronides/sulfates of MTBH in rats after oral (25, 50 and 100 mg/kg) or I.V. (25 mg/kg) administration are presented in Table 1, respectively. Before enzymolysis, the free form was detectable in plasma for up to 2–4 h at three dose levels. The pharmacokinetic parameters were dose independent for free form after oral administration in rats. The mean T max and t 1/2 values of the free form were approximately 0.25–0.5 h and 0.31–0.46 h, respectively. These results indicated that free form was rapidly absorbed into the blood, and then rapidly eliminated from the circulation. After hydrolysis with β-glucuronidase or sulfatase/β-glucuronidase, both the plasma concentration–time profiles of glucuronides and glucuronides/sulfates exhibited a second peak, indicating possible enterohepatic circulation. The C max and AUC0–t of glucuronides/sulfates were significantly higher than those of glucuronides, combined with the results of qualitative analysis of MTBH conjugated metabolites in plasma, indicating the presence of sulfates in plasma. The C max and AUC0–t of free form to those of glucuronides/sulfates were approximately 5.77–8.92 % and 0.85–1.46 %, respectively, which indicated that level of free form was much lower than that of glucuronides/sulfates in systemic circulation. In this study, MTBH exhibited linear pharmacokinetics within the dose range tested, as indicated by a linear increase in the C max and AUC0–t with oral dose at 25, 50 and 100 mg/kg (Fig. 5a, b) without a significant difference in the elimination parameters such as clearance (CL) and t 1/2 across the doses (Table 1). The dose-normalized AUC0–t values (based on 25 mg/kg) were 24.05, 25.06 and 29.70 µg·h/mL for glucuronides, and 28.69, 32.87 and 36.71 µg·h/mL for glucuronides/sulfates at 25, 50 and 100 mg/kg, respectively (Table 1). After I.V. administration of MTBH at 25 mg/kg in rats, the plasma concentrations of free form declined in a poly-exponential fashion, and free form was converted to glucuronides and glucuronides/sulfates rapidly and reached their peak concentrations in about 0.5–1 h after dosing (Fig. 4). The t 1/2 for free form, glucuronides and glucuronides/sulfates of MTBH was approximately 0.46, 4.57, and 4.63 h, respectively, which was not significantly different from that of free form, glucuronides and glucuronides/sulfates of MTBH after oral administration. The AUC0–t of free form to that of glucuronides/sulfates was approximately 6.59 %, which was markedly higher than that of free form after oral administration of MTBH at 25 mg/kg in rats. MTBH absolute bioavailability was approximately 31.27 %.
3.3 Tissue Distribution Study
The concentration of MTBH in tissues was determined as described above. The calibration curves of MTBH in various tissue homogenates showed good linearities (r > 0.99) in the range of 0.05–40 µg/mL. The precision evaluation showed that all coefficients of variation were below 12.1 % and the accuracy analysis showed that the RSD were below 13.7 %. The recoveries of MTBH from various tissues ranged from 67.31 to 85.16 %. The LLOQ and LOD of MTBH were 0.05 and 0.02 µg/mL, respectively.
Tissue distribution was assessed at ten different time points (0.5, 1, 1.5, 2, 4, 6, 8, 12, 16, and 24 h) after oral administration of 200 mg/kg MTBH to rats. Figure 6 shows the concentration–time profile of free form, glucuronides and glucuronides/sulfates of MTBH in various tissues. The pharmacokinetic parameters of free form, glucuronides and glucuronides/sulfates of MTBH in various tissues are presented in Table 2. The results demonstrated that MTBH underwent a rapid and wide distribution to all examined tissues. The free form was found in all tissues assayed, whereas, glucuronides and glucuronides/sulfates were not detectable in heart, brain and muscle (Figs. 6 and 7). Only trace amounts of free form was presented in brain and muscle, and considerable concentration of free form was detected in stomach and lung. The relative AUC0–t of free form was ranked as stomach > lung > intestine > liver > heart > spleen > kidney > brain > muscle. The AUC0–t of free form to that of glucuronides/sulfates was in the range from 3 to 90 % (Table 2), which indicated that the level of glucuronides and sulfates and/or tissue uptake of glucuronides/sulfates metabolites differed between tissues. Glucuronides/sulfates were the major form in intestine, kidney and liver, and the relative AUC0–t of glucuronides/sulfates was ranked as liver > intestine > kidney. The difference of AUC0–t between glucuronides/sulfates and glucuronides afforded the estimated AUC0–t of sulfates; AUC0–t of sulfates was ranked as liver > intestine > kidney > spleen > lung > stomach. The C max or AUC0–t of MTBH sulfates was always lower than that of glucuronides in plasma and the tissues (including stomach, intestine, kidney, spleen, liver and lung).
Mean (± SD) plasma and tissues concentration–time profiles of free form (F), glucuronides (G) and glucuronides/sulfates (S/G) of MTBH in various tissues (including heart, liver, spleen, lung, kidney, stomach, intestine, brain and muscle) after a single oral dose of 200 mg/kg MTBH to rats (n = 6 per time point)
Mean (± SD) concentration of free form (MTBH), glucuronides (MTBH-G) and glucuronides/sulfates (MTBH-S/G) of MTBH in plasma and various tissues (including heart, liver, spleen, lung, kidney, stomach, intestine, brain and muscle) collected at 0.5 and 1 h after a single oral dose of 200 mg/kg MTBH to rats
4 Discussion
MTBH is a novel derivative of hesperetin with potent anti-inflammatory activity which is being evaluated in vitro and in vivo in our previous study, so it is reasonable and necessary to perform the pharmacokinetics and tissue distribution study of MTBH. In the rat organism, MTBH was largely metabolized to different conjugates (glucuronides, sulfates), which was found in plasma and tissues, including stomach, intestine, kidney, spleen, liver and lung. Two main conjugated metabolites were identified with Agilent TOF LC/MS after oral administration of the agent to rats: MTBH-O-glucuronide and MTBH-O-sulfate. Owing to the unavailability of the authentic standards of conjugated metabolites, the concentrations of the conjugated metabolites of MTBH were determined indirectly after hydrolysis with β-glucuronidase and sulfatase. A HPLC method was successfully developed and validated for the determination of MTBH in rat plasma and various tissues for their satisfactory sensitivity, specificity and selectivity. There was no any endogenous matrix interference with MTBH and hesperidin. Because the sulfatase used in this study contained sulfatase and a considerable amount of β-glucuronidase, hydrolysis with sulfatase resulted in simultaneous hydrolysis of both sulfates and glucuronides. The plasma and tissue homogenates required only single-step extractions by ethyl acetate before and after hydrolysis with β-glucuronidase or sulfatase/β-glucuronidase, respectively, which is suitable for the analysis of large batches of samples. The method has been successfully applied to study pharmacokinetics and tissue distribution of MTBH in rats.
After a single oral dose of MTBH, the free-form MTBH was detectable in plasma, suggesting that it did enter the systematic circulation per se. This was quite different from that of hesperetin reported in a previous study that there was no free aglycone in human plasma [4]. After the plasma samples were treated with β-glucuronidase or sulfatase/β-glucuronidase, both peak area and peak height of MTBH increased significantly in the HPLC chromatogram, indicating that MTBH glucuronides and glucuronides/sulfates were present in the bloodstream and the corresponding MTBH were liberated from conjugated metabolites following enzymatic hydrolysis. This was in accordance with that of hesperetin which was absorbed into the systematic circulation as glucuronides and sulphoglucuronides [5, 23–26]. After absorbed from the small intestine, free-form MTBH was rapidly eliminated from plasma with t 1/2 less than 0.5 h, whereas the t 1/2 of MTBH glucuronides and glucuronides/sulfates was about 4–6 h. The values of the t 1/2 of MTBH glucuronides/sulfates were found to be much longer than that of hesperetin estimated previously, in experiments where the flavanone glycosides were administered in the form of citrus juices [27]. The absolute bioavailability of MTBH was approximately 31.27 % which was also significantly higher than that of hesperetin (with a mean absolute bioavailability at about 12.87 %) [28]. The two molecules, hesperetin and MTBH, differ in their physicochemical properties and molecular weight (MW). Hesperetin has the lower MW (C16H14O6, 302.27 g/mol) in comparison with MTBH (C21H25O6N, 387.18 g/mol). MTBH is significantly more hydrophilic than hesperetin, with LogP of 1.9, whereas hesperetin have LogP value of 2.9. The water solubility of MTBH (28.57 µg/mL) was increased approximately 5.07-fold compared to that of hesperetin (5.63 µg/mL) in our previous study. This increased water solubility and better hydrophilicity may be one of the explanation for this significantly higher bioavailability of MTBH than hesperetin. The highest concentration of free form, glucuronides and glucuronides/sulfates of MTBH was detected at about 0.25, 1 and 1 h, respectively, suggesting that free-form MTBH was absorbed more rapidly. However, the plasma drug exposure of free-form MTBH after oral administration was less than 2 % of that of MTBH glucuronides/sulfates, suggesting that free-form MTBH was extensively converted into MTBH glucuronides and sulfates in the intestinal cells or during further first-pass metabolism. On the contrary, the plasma drug exposure of free-form MTBH after I.V. injection was more than 6 % of that of MTBH glucuronides/sulfates, which was approximately 4.51 to 7.75-fold to that of free-form MTBH after oral administration. One possible reason was that a part of MTBH glucuronides and sulfates were formed in the intestinal wall except in liver prior to absorption. Based on these data, the main forms in circulation were MTBH conjugated metabolites, which was in good agreement with that of hesperetin in the literature [4, 29–31]. Comparison of the C max and AUC0–t between MTBH glucuronides/sulfates and glucuronides showed marked differences, which clearly indicated that the conjugated metabolites included not only MTBH glucuronides but also sulfates. By subtracting the AUC0–t of the glucuronides from that of correspondent glucuronides/sulfates, it could be found that the AUC0–t of the sulfates was about 14.52–24.41 % of its correspondent glucuronides. This fact furnishes the evidence that MTBH was majorly metabolized to glucuronides and less to sulfates, combined with our qualitative results of MTBH conjugated metabolites in plasma, the sulfoglucuronyl diconjugates of MTBH were not found in the plasma. This was somewhat different from that of hesperetin in the literature which showed that the main metabolites of hesperetin were glucuronidated, and that 13 % of them were sulpho-glucuronidated [4]. After oral and I.V. administration of MTBH, the plasma kinetics profiles of MTBH glucuronides and glucuronides/sulfates had a particular shape, with one peak 1 h after the drug ingestion and a smaller one at about 2 h. One explanation may be the existence of an enterohepatic recycling of MTBH conjugated metabolites, with the second peak corresponding to the re-absorption of the metabolites secreted in bile. The possibility of a significant excretion of MTBH metabolites in bile (6–12 %) had been elucidated in rats in our previous study (our unpublished data). The absorption of MTBH was rapid and much faster than that of hesperetin after oral administration of its flavanone glycosides, hesperidin, either as pure compounds or in the form of citrus juices [4, 27, 32]. The mean T max values of free-form and conjugated-form MTBH after oral administration at three dose levels were from 0.25 to 1 h, which was significant shorter than that of hesperetin with mean T max value from 5.4 to 5.8 h [4] after the ingestion of two doses of orange juice in humans. One possible reason was that the absorption site of the MTBH is the small intestine where it was absorbed much faster and hesperidin, which was not deglycosylated nor absorbed in the small intestine, but was hydrolyzed in the distal part of the intestine and the colon by the enteric microflora, and then absorbed in the caecum [26, 33, 34] where it was absorbed much slower.
For tissue distribution analysis, before organ collection, a systemic perfusion with cool saline was performed to avoid the interference of residual blood. Our results showed that free-form MTBH was present in various organs including brain after a single oral dose of 200 mg/kg MTBH to rats. The emergence of a considerable level of the free-form MTBH in the liver and lung may have been biotransformed from its glucuronides/sulfates in the blood circulation. This fact can be explained by the presence of deconjugation enzymes such as glucuronidase and sulfatase on the cell membranes of these organs [35–37]. We did not find MTBH glucuronides and glucuronides/sulfates in brain, muscle and heart, however, the presence of trace amounts of such conjugated metabolites, not detectable in our conditions, cannot be excluded. Contrary to the finding in plasma, sulfates rather than glucuronides were found as the major conjugates of MTBH in the liver, kidney and lung, indicating that the MTBH glucuronides in blood circulation might have transformed through deconjugation by glucuronidase and subsequent reconjugation by sulfotransferase in these organs.
Results indicated that distribution process was very quick (with a mean T max value from 0.5 to 1 h) reaching all the examined tissues with the highest levels detected in liver suggesting a potential role of this organ in the metabolism of MTBH. MTBH had been elucidated to possess in vivo hepatoprotective effects against CCl4-induced acute liver injury in ICR mice in our previous study, which could be attributed to the activity of total potencies of unchanged MTBH and its conjugated metabolites in the liver. Moreover, the observed high hepatic levels are in accordance with previous tissue distribution studies of hesperetin in rats after a dietary intake [38].
Generally speaking, the conjugated metabolites were recognized as the inactive product of drugs. Nevertheless, there were increasing evidences showing that the conjugated metabolites of polyphenols such as myricetin [39], quercetin [40–44] and baicalin [45] exhibited beneficial bioactivities. This study shows that MTBH mainly existed as conjugated metabolites in the systematic circulation and most organs, the own biological activity of the conjugated metabolites of MTBH should be considered and future investigated to understand the clinical implications of MTBH, despite though the possibility of hydrolysis into free-form MTBH inside the cells.
5 Conclusion
This work investigated the pharmacokinetic properties of a novel hesperetin derivative MTBH in plasma and tissues after a single dose in rats. Free-form MTBH was unequally distributed in plasma and a wide variety of tissues examined, and MTBH glucuronides/sulfates were the major forms in systematic circulation and in intestine, kidney and liver tissues. The liver was found likely to accumulate MTBH at a high concentration among all the tissues. The results of this pharmacokinetics and tissue distribution are undoubtedly useful to understand the targets of MTBH in exerting its biological effect and health impact.
References
Gil-Izquierdo A, Gil MI, Ferreres F. Effect of processing techniques at industrial scale on orange juice antioxidant and beneficial health compounds. J Agric Food Chem. 2002;50(18):5107–14.
Brand W, van der Wel PA, Rein MJ, Barron D, Williamson G, van Bladeren PJ, Rietjens IM. Metabolism and transport of the citrus flavonoid hesperetin in Caco-2 cell monolayers. Drug Metab Dispos. 2008;36(9):1794–802.
Bredsdorff L, Nielsen IL, Rasmussen SE, Cornett C, Barron D, Bouisset F, Offord E, Williamson G. Absorption, conjugation and excretion of the flavanones, naringenin and hesperetin from alpha-rhamnosidase-treated orange juice in human subjects. Br J Nutr. 2010;103(11):1602–9.
Manach C, Morand C, Gil-Izquierdo A, Bouteloup-Demange C, Remesy C. Bioavailability in humans of the flavanones hesperidin and narirutin after the ingestion of two doses of orange juice. Eur J Clin Nutr. 2003;57(2):235–42.
Nielsen IL, Chee WS, Poulsen L, Offord-Cavin E, Rasmussen SE, Frederiksen H, Enslen M, Barron D, Horcajada MN, Williamson G. Bioavailability is improved by enzymatic modification of the citrus flavonoid hesperidin in humans: a randomized, double-blind, crossover trial. J Nutr. 2006;136(2):404–8.
Bouskela E, Cyrino FZ, Lerond L. Effects of oral administration of different doses of purified micronized flavonoid fraction on microvascular reactivity after ischaemia/reperfusion in the hamster cheek pouch. Br J Pharmacol. 1997;122(8):1611–6.
Miyake Y, Yamamoto K, Tsujihara N, Osawa T. Protective effects of lemon flavonoids on oxidative stress in diabetic rats. Lipids. 1998;33(7):689–95.
Kim JY, Jung KJ, Choi JS, Chung HY. Hesperetin: a potent antioxidant against peroxynitrite. Free Radic Res. 2004;38(7):761–9.
Hirata A, Murakami Y, Shoji M, Kadoma Y, Fujisawa S. Kinetics of radical-scavenging activity of hesperetin and hesperidin and their inhibitory activity on COX-2 expression. Anticancer Res. 2005;25(5):3367–74.
Galati EM, Monforte MT, Kirjavainen S, Forestieri AM, Trovato A, Tripodo MM. Biological effects of hesperidin, a citrus flavonoid. (Note I): antiinflammatory and analgesic activity. Farmaco. 1994;40(11):709–12.
Paredes A, Alzuru M, Mendez J, Rodriguez-Ortega M. Anti-Sindbis activity of flavanones hesperetin and naringenin. Biol Pharm Bull. 2003;26(1):108–9.
Borradaile NM, Carroll KK, Kurowska EM. Regulation of HepG2 cell apolipoprotein B metabolism by the citrus flavanones hesperetin and naringenin. Lipids. 1999;34(6):591–8.
Kim HK, Jeong TS, Lee MK, Park YB, Choi MS. Lipid-lowering efficacy of hesperetin metabolites in high-cholesterol fed rats. Clin Chim Acta. 2003;327(1–2):129–37.
Garg A, Garg S, Zaneveld LJ, Singla AK. Chemistry and pharmacology of the Citrus bioflavonoid hesperidin. Phytother Res. 2001;15(8):655–69.
Yang M, Tanaka T, Hirose Y, Deguchi T, Mori H, Kawada Y. Chemopreventive effects of diosmin and hesperidin on N-butyl-N-(4-hydroxybutyl)nitrosamine-induced urinary-bladder carcinogenesis in male ICR mice. Int J Cancer. 1997;73(5):719–24.
So FV, Guthrie N, Chambers AF, Moussa M, Carroll KK. Inhibition of human breast cancer cell proliferation and delay of mammary tumorigenesis by flavonoids and citrus juices. Nutr Cancer. 1996;26(2):167–81.
Tanaka T, Makita H, Kawabata K, Mori H, Kakumoto M, Satoh K, Hara A, Sumida T, Tanaka T, Ogawa H. Chemoprevention of azoxymethane-induced rat colon carcinogenesis by the naturally occurring flavonoids, diosmin and hesperidin. Carcinogenesis. 1997;18(5):957–65.
Miyagi Y, Om AS, Chee KM, Bennink MR. Inhibition of azoxymethane-induced colon cancer by orange juice. Nutr Cancer. 2000;36(2):224–9.
Buckshee K, Takkar D, Aggarwal N. Micronized flavonoid therapy in internal hemorrhoids of pregnancy. Int J Gynaecol Obstet. 1997;57(2):145–51.
Tsimoyiannis EC, Floras G, Antoniou N, Papanikolaou N, Siakas P, Tassis A. Low-molecular-weight heparins and Daflon for prevention of postoperative thromboembolism. World J Surg. 1996;20(8):968–71 (discussion 72).
Maiti K, Mukherjee K, Murugan V, Saha BP, Mukherjee PK. Exploring the effect of Hesperetin–HSPC complex–a novel drug delivery system on the in vitro release, therapeutic efficacy and pharmacokinetics. AAPS PharmSciTech. 2009;10(3):943–50.
Kanaze FI, Bounartzi MI, Georgarakis M, Niopas I. Pharmacokinetics of the citrus flavanone aglycones hesperetin and naringenin after single oral administration in human subjects. Eur J Clin Nutr. 2007;61(4):472–7.
Hackett AM, Marsh I, Barrow A, Griffiths LA. The biliary excretion of flavanones in the rat. Xenobiotica. 1979;9(8):491–501.
Bokkenheuser VD, Shackleton CH, Winter J. Hydrolysis of dietary flavonoid glycosides by strains of intestinal Bacteroides from humans. Biochem J. 1987;248(3):953–6.
Hollman PC, Bijsman MN, van Gameren Y, Cnossen EP, de Vries JH, Katan MB. The sugar moiety is a major determinant of the absorption of dietary flavonoid glycosides in man. Free Radic Res. 1999;31(6):569–73.
Felgines C, Texier O, Morand C, Manach C, Scalbert A, Regerat F, Remesy C. Bioavailability of the flavanone naringenin and its glycosides in rats. Am J Physiol Gastrointest Liver Physiol. 2000;279(6):G1148–54.
Erlund I, Meririnne E, Alfthan G, Aro A. Plasma kinetics and urinary excretion of the flavanones naringenin and hesperetin in humans after ingestion of orange juice and grapefruit juice. J Nutr. 2001;131(2):235–41.
Li YM, Li XM, Li GM, Du WC, Zhang J, Li WX, Xu J, Hu M, Zhu Z. In vivo pharmacokinetics of hesperidin are affected by treatment with glucosidase-like BglA protein isolated from yeasts. J Agric Food Chem. 2008;56(14):5550–7.
Matsumoto H, Ikoma Y, Sugiura M, Yano M, Hasegawa Y. Identification and quantification of the conjugated metabolites derived from orally administered hesperidin in rat plasma. J Agric Food Chem. 2004;52(21):6653–9.
Mullen W, Archeveque MA, Edwards CA, Matsumoto H, Crozier A. Bioavailability and metabolism of orange juice flavanones in humans: impact of a full-fat yogurt. J Agric Food Chem. 2008;56(23):11157–64.
Brett GM, Hollands W, Needs PW, Teucher B, Dainty JR, Davis BD, Brodbelt JS, Kroon PA. Absorption, metabolism and excretion of flavanones from single portions of orange fruit and juice and effects of anthropometric variables and contraceptive pill use on flavanone excretion. Br J Nutr. 2009;101(5):664–75.
Ameer B, Weintraub RA, Johnson JV, Yost RA, Rouseff RL. Flavanone absorption after naringin, hesperidin, and citrus administration. Clin Pharmacol Ther. 1996;60(1):34–40.
Griffiths LA, Barrow A. Metabolism of flavonoid compounds in germ-free rats. Biochem J. 1972;130(4):1161–2.
Manach C, Morand C, Demigne C, Texier O, Regerat F, Remesy C. Bioavailability of rutin and quercetin in rats. FEBS Lett. 1997;409(1):12–6.
O’Leary KA, Day AJ, Needs PW, Sly WS, O’Brien NM, Williamson G. Flavonoid glucuronides are substrates for human liver beta-glucuronidase. FEBS Lett. 2001;503(1):103–6.
Pasqualini JR, Chetrite GS. Recent insight on the control of enzymes involved in estrogen formation and transformation in human breast cancer. J Steroid Biochem Mol Biol. 2005;93(2–5):221–36.
Reed MJ, Purohit A, Woo LW, Newman SP, Potter BV. Steroid sulfatase: molecular biology, regulation, and inhibition. Endocr Rev. 2005;26(2):171–202.
Takumi H, Mukai R, Ishiduka S, Kometani T, Terao J. Tissue distribution of hesperetin in rats after a dietary intake. Biosci Biotechnol Biochem. 2011;75(8):1608–10.
Hiermann A, Schramm HW, Laufer S. Anti-inflammatory activity of myricetin-3-O-beta-d-glucuronide and related compounds. Inflamm Res. 1998;47(11):421–7.
Moon JH, Tsushida T, Nakahara K, Terao J. Identification of quercetin 3-O-beta-d-glucuronide as an antioxidative metabolite in rat plasma after oral administration of quercetin. Free Radic Biol Med. 2001;30(11):1274–85.
Manach C, Morand C, Crespy V, Demigne C, Texier O, Regerat F, Remesy C. Quercetin is recovered in human plasma as conjugated derivatives which retain antioxidant properties. FEBS Lett. 1998;426(3):331–6.
Shirai M, Kawai Y, Yamanishi R, Kinoshita T, Chuman H, Terao J. Effect of a conjugated quercetin metabolite, quercetin 3-glucuronide, on lipid hydroperoxide-dependent formation of reactive oxygen species in differentiated PC-12 cells. Free Radic Res. 2006;40(10):1047–53.
Yang JH, Hsia TC, Kuo HM, Chao PD, Chou CC, Wei YH, Chung JG. Inhibition of lung cancer cell growth by quercetin glucuronides via G2/M arrest and induction of apoptosis. Drug Metab Dispos. 2006;34(2):296–304.
Yoshino S, Hara A, Sakakibara H, Kawabata K, Tokumura A, Ishisaka A, Kawai Y, Terao J. Effect of quercetin and glucuronide metabolites on the monoamine oxidase-A reaction in mouse brain mitochondria. Nutrition. 2011;27(7–8):847–52.
Trinh HT, Joh EH, Kwak HY, Baek NI, Kim DH. Anti-pruritic effect of baicalin and its metabolites, baicalein and oroxylin A, in mice. Acta Pharmacol Sin. 2010;31(6):718–24.
Acknowledgments
This project was supported by the National Science Foundation of China (Nos: 81273526, and 81473268), Anhui provincial key Scientific and technological project (1301042212), Anhui Provincial Natural Science Foundation (1308085MH145), Specialized Research Fund for the Doctoral Program of Higher Education (20123420120001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Shen, C., Qian, Z., Chen, R. et al. Single Dose Oral and Intravenous Pharmacokinetics and Tissue Distribution of a Novel Hesperetin Derivative MTBH in Rats. Eur J Drug Metab Pharmacokinet 41, 675–688 (2016). https://doi.org/10.1007/s13318-015-0293-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-015-0293-2