Abstract
Parkinson disease (PD) is highly prevalent among neurodegenerative diseases, affecting a diverse patient population. Despite a general willingness of patients to participate in clinical trials, only a subset of patients enroll in them. Understanding the barriers to trial participation will help to alleviate this discrepancy and improve trial participation. Underrepresented minorities, older patients, and patients with more medical comorbidities in particular are underrepresented in research. In clinical trials, this has the effect of delaying trial completion, exacerbating disparities, and limiting our ability to generalize study results. Efforts to improve trial design and recruitment are necessary to ensure study enrollment reflects the diversity of patients with PD. At the trial design level, broadening inclusion criteria, attending to participant burden, and focusing on trial efficiency may help. At the recruitment stage, increasing awareness, with traditional outreach or digital approaches; improving engagement, particularly with community physicians; and developing targeted recruitment efforts can also help improve enrollment of underrepresented patient groups. The use of technology, for virtual visits, technology-based objective measures, and community engagement, can also reduce participant burden and increase recruitment. By designing trials to consider these barriers to trial participation, we can improve not only the access to research for all our patients but also the quality and generalizability of clinical research in PD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Parkinson disease (PD) is the second most common neurodegenerative disease, affecting patients in a range of ages, geographic locations, and racial and ethnic backgrounds, and affecting men and women [1,2,3]. There is a pressing need for both basic science and clinical research to develop improved therapeutics. However, poor recruitment is a chronic problem in clinical studies of patients with PD. An informal survey by The Michael J. Fox Foundation (MJFF) found that although 80% of patients were at least “somewhat likely” to be willing to participate in a trial, fewer than 10% had participated [4]. Patients who do participate in a trial overwhelmingly report a willingness to enroll in another and would recommend participation to others [5]. Despite this readiness of patients, 90% of clinical trials fail to enroll patients within the target amount of time requiring an extended enrollment period [6]. Furthermore, only 1/3 of multicenter trials achieve their planned recruitment goals forcing trials to close early because of inadequate recruitment [7,8,9]. For these reasons, the MJFF and others have prioritized education and outreach about clinical trials [10].
Despite significant efforts, there remain many formal and informal barriers to trial participation in Parkinson disease, which have several important consequences. Delays in trial completion result in delays in the review and potential approval of new drugs. Incomplete trials reduce patient confidence in clinical research in general. Moreover, barriers to trial participation disproportionately affect some populations more than others. The impact of these barriers can affect the sex, age, racial, ethnic, socioeconomic, and geographic diversity of the patients included, which, in turn, limits the generalizability of trial results and our understanding of the therapeutic effectiveness of agents. In this review, we examine some of the major barriers to trial participation in Parkinson disease, consider the implications of these barriers on diversity and trial generalizability, and discuss novel designs for recruitment and participation.
Barriers to Trial Participation
Barriers to trial participation can occur at several stages in trial design and recruitment. Some patients are excluded from trials explicitly as part of the trial design. The indirect burdens of trial participation—physical, financial, and logistical costs—on patients and their caregivers can also pose an obstacle.
Restrictive Inclusion and Exclusion Criteria
Formal barriers imposed by trial design can have a major effect on recruitment and participation. Eligibility criteria are intended to ensure the safety of participants, limit confounding variables, and define the population. However, restrictive eligibility criteria can also serve as a barrier to recruitment and limit our understanding of the generalizability of an intervention. Restrictive eligibility criteria have raised concerns about the generalizability of clinical trials in many fields, including stroke [11], cardiology [12,13,14], oncology [15,16,17], endocrinology [18], psychiatry [19, 20], nephrology [21], rheumatology [22], critical care [23], and substance abuse [24]. For example, in oncology, among patients newly diagnosed with non–small cell lung cancer, a recent analysis has shown that 79% of patients would be ineligible for trials based on standard eligibility criteria [16]; a similar analysis in cardiology showed that 81% of patients with heart failure would be ineligible for a trial [12].
In PD, analysis of the postmarketing use of agents demonstrates that clinical trials often exclude the very patient groups in whom those agents will be used. There are frequently differences in the trial population compared to the real-world use. For example, a postmarketing study of rasagiline demonstrates its use as monotherapy in older patients than were studied in the phase 3 TEMPO trial (65.4 vs 60.5 years) [25, 26]. A postmarketing study of entacapone also demonstrates its use in older patients as compared to the phase 3 clinical trials (69 vs 62.7 years) [27, 28]. Istradefylline was found to be used in older patients (70.7 vs 65.5 years) with a longer duration of disease (8.8 vs 7.7 years) and greater motor symptoms than in the phase 3 trial (UPDRS Part 3 score 33.7 vs 21) [29, 30]. Patients with surgical treatments, including DBS, were excluded from the study of istradefylline, but 31% of patients in postmarketing analysis had undergone surgical intervention.
Age
Exclusion of older adults in randomized clinical trials directly, with age cutoffs, or indirectly, by using medical and cognitive criteria that disproportionately affect older participants, is common. Zulman et al. [31] evaluated the inclusion of older adults in clinical trials published in major medical journals, of any medical specialty, and noted that although 20% of trials explicitly excluded older patients, nearly half used criteria that would disproportionately exclude older adults. These include exclusion criteria based on functional limitations and age-related cognitive impairment. Despite this, several trials noted a difference in the benefit of a drug by age, suggesting that there are differences in clinical effect and side effects associated with age that are not being captured in many clinical trials.
In PD, Mitchell et al. [32] studied whether older subjects were included in early trials of drugs to treat motor symptoms. They evaluated the 112 studies published between 1966 and 1996 for inclusion of participants older than 75. Overall, only 37.5% of studies clearly included subjects older than 75 (27.7% of articles did not clearly report) and only 5.5% of participants were older than 75. Earlier studies (conducted between 1966 and 1976) of immediate-release levodopa formulations, anticholinergic agents, and amantadine were more likely to include older subjects than newer studies of selegiline and sustained-release levodopa formulations.
Given the high prevalence of PD in older adults, with an increase in PD incidence with age [1, 2], restrictive age criteria pose a major barrier to trial participation. Age criteria with a cutoff of 75 years eliminate 69% of patients with PD in the USA, and up to 74% of patients in some states [33]. Globally, age criteria excluding patients over 75 years would eliminate approximately 75% of patients [2].
Age criteria also limit generalizability. Patients with early-onset PD are more likely to have slower disease progression; less likely to have early gait difficulty, cognitive impairment, or neuropsychiatric side effects; and more likely to have dystonia [34]. Older patients with PD are more likely to have dementia [35] and medical comorbidities—exclusion of these patients limits assessment of the side effect profile in more vulnerable patients. Women also tend to present at an older age than men, more commonly with tremor-predominant phenotype [36, 37], and have a lower occurrence of dementia [35] with differences in the frequencies of some nonmotor symptoms [36], so age criteria can indirectly affect the sex and clinical phenotypes represented in a study.
Based on these and other data, in 2016, Congress passed the 21st Century Cures Act [38], which required the National Institutes of Health (NIH) to collect data and publish data on the age of participants in an NIH-funded clinical research and determine whether to revise guidelines on the inclusion of participants based on age [39]. The NIH enacted the Inclusion Across the Lifespan Policy for grants in 2019, which requires rationale and justification to be submitted if participants are excluded based on age and suggests that trial eligibility criteria reflect the population with the condition being studied [40]. Participants should be excluded only if the study presents an unacceptable risk compared to the knowledge gained and therapeutic benefit.
Burdensome Participation Requirements
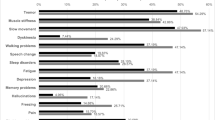
Participation in clinical trials poses unique challenges for patients and their families. A survey of 27 PD patients in a deep brain stimulation (DBS) trial asked about the experience of participating; 63% of patients reported some burden associated with participation in the trial (Table 1) [5]. The financial commitment (including travel, time off work), neuropsychological testing, and washout periods were the most common hardships. Notably, the survey was based on free-text response in a small group of relatively young (61 ± 6.4 years) patients with early disease (duration 2.1 ± 1.8 years) who completed a surgical trial (1 patient withdrew from the trial because of financial/family concerns and was not included in the survey). Thus, it may not accurately represent the concerns of patients more generally, including older participants with more advanced disease.
Financial Burden
Trial participation can have a significant financial burden on patients and families who may be also coping with other medical expenses. Financial impact can be direct because of costs of travel and lodging, or indirect as a result of missed days of work or additional medical testing. In one study, 30% of patients with PD reported financial commitments were a burden to trial participation (Table 1) [5]. Similar results have been reported in other conditions. Goel et al. [41] surveyed patients with myeloproliferative disorders participating in a clinical trial and found that 35% of patients reported spending more money during the trial than on prior treatments and 21% missed more days of work than during prior treatments [41]. Among participants in that study from the USA, more than 40% of patients spent more than $100 for trial participation and nearly 20% spent more than $1000. Nipp et al. [42] evaluated oncology patients enrolled in a program to support those with financial needs or financial impediments to trial participation, and found that these patients spent more than $600 per month on travel and lodging for trial participation.
Financial burdens can introduce disparities into clinical trial participation. Patients with more limited financial resources, including minorities and older adults who may be on fixed incomes, may be less able to participate [40].
Travel
Participating in trials can require frequent and, for some patients, lengthy travel to the study site for evaluations. An estimated 70% of potential trial participants live more than 2 h away from a study center [43]. Borno et al. [44] found that oncology patients participating in clinical trials traveled 25.8 miles on average to the study site, with a higher burden of travel for NIH-sponsored trials, phase 1 studies, and participants living in low-income areas. More than 25% of NIH-sponsored trial participants traveled more than 100 miles each way. Notably, this study evaluated patients who actually chose to participate; eligible patients with further travel distance may have elected against participation [45]. Patients who are older, with more advanced disease or impaired physical function, or with more medical comorbidities are more likely to be affected by travel requirements for in-person follow-up [40].
Significant travel requirements can result in higher financial burden to trial participation, more days of missed work, and potential loss of employment [41]. As a result, travel can also disproportionately affect patients of lower socioeconomic status.
Medication Adjustments/Washout Periods
Stopping or adjusting a stable treatment regimen, even briefly for on/off testing, can be uncomfortable for patients and disruptive to their lives. In one survey of patients with PD and their caregivers, changes to medication regimen were considered a barrier to participation in more than half of those surveyed [46]. Disruption to participants’ lives was also a concern of 37% of respondents. In a survey of participants in a DBS trial, the washout period required for participation was described as a burden for 25% of participants (Table 1) [5]. Patients with more advanced disease or a greater number of comorbidities may be more sensitive to these concerns, and so, limiting, when possible, medication adjustments may allow more of these patients to be included in clinical trials.
Access to Caregivers
Patients with PD often rely on caregivers to provide support, assist with treatment regimen and access to medical care, and perform activities of daily living. Among patients with PD, more than 80% in some studies have a regular informal or formal caregiver, most commonly a spouse [47,48,49]. Caregivers frequently accompanied patients or provided transportation to doctor’s visits [47, 49]. Given the reliance on caregivers for access to medical care, taken together with the travel requirements and frequent clinical assessments in clinical trials, the increased burden on caregivers can be an additional barrier to trial participation. Patients without a regular or paid caregiver may be less able to participate. Notably, access to caregivers is not uniform across the population. Men with PD more frequently have a regular caregiver than women and more frequently had caregivers who accompanied them to physician visits [49, 50]. Caregivers of men with PD also experience significantly more caregiver burden [49].
Additional explicit support in clinical trials for caregivers, with particular attention to the effects of trial participation, in person visits, travel, and medication changes on caregivers and caregiver burden could, in part, address this barrier to participation and reduce disparities that arise as a result of access to regular caregivers.
Limited Participating Sites
Clinical epidemiology and treatment trials are largely conducted at a limited number of academic medical centers. The limited geographic availability of trials can pose direct and indirect barriers to recruitment and trial participation. There is substantial geographic variability in the prevalence of Parkinson disease across the USA [33] and the world [2], so some patients may not be able to access clinical trials because of their distance from a clinical site. There is also significant regional variability in the healthcare usage, hospitalization rate, and the out-of-pocket cost of care [33], and so financial and travel barriers may further increase regional disparities in trial participation. The use of clinical trial networks and multisite consortiums (e.g., the Parkinson’s Progression Markers Initiative (PPMI) [51]) can increase access and the representation of subpopulations in clinical trials [40].
Recruitment for trials largely at academic centers via a neurologist or movement disorders specialist can also limit access. In one study, among Medicare beneficiaries with PD, only 58% saw a neurologist; 42% of patients did not see a specialist [52] and so presumably would not have had access to participate in treatment or other trials. Increasing primary care referrals to secondary care and increasing recruitment for trials among community physicians in PD have proven challenging [53, 54], but further efforts to connect patients, particularly women and minorities, may improve access.
Unique Challenges Related to Racial/Ethnic Diversity in Trial Recruitment and Participation
Although several studies suggest that the rate of diagnosed PD is lower among individuals of African or Hispanic descent when compared to those of European descent (or whites) [55,56,57,58], the rates of clinical trial participation for these traditionally underserved minority groups are even lower. A systematic review of published clinical trials from 1985 to 2007 demonstrated that very few studies (17%) reported participation by race/ethnicity [59]. Of the 33 distinct studies that did report race/ethnicity, less than 8% (560/7481) of participants were nonwhite. When one study that exclusively studied minorities is excluded, the number of nonwhite participants is reduced even further to 5.6% [59]. In comparison, US census data for the same time period show that the nonwhite population was at least 20%. More recent genetic studies of PD largely use data from individuals of European ancestry. These disparities in clinical trial participation are not unique to PD. A review of pivotal clinical trials, that is, studies that led to subsequent Food and Drug Administration (FDA) approval, across all therapeutic areas from 2011 to 2013 showed that African–Americans and Hispanics were under-represented relative to their numbers in the general population [60].
The lack of diversity in clinical trials has several implications. First, our understanding of PD biology and subsequent development of novel therapeutics are severely hampered when only a limited subpopulation is studied. PD is a heterogeneous disorder, and improving our knowledge of its complex etiologies, trajectories, and outcomes will require more diversity in research participation. Second, traditionally underserved minorities already receive substandard PD care when compared to whites [61,62,63]. Lack of available, generalizable data from clinical trials will limit our ability to provided high-value, evidence-based, and personalized care further exacerbating healthcare disparities.
The first step to address the problem of lack of diversity in clinical trials is to understand the underlying causes. Researchers have proposed several potential reasons for these disparities in PD [64]. One hypothesis is that delays in PD diagnosis [65] and presentation to clinical care at more advanced stages [66] prevent enrollment in early-stage, neuroprotective trials. Another very likely possibility is that the majority of clinical trials occur at the specialty movement disorders center, and most minority patients lack access to these centers [52, 67]. For example, the large observational study through the Parkinson Foundation Parkinson Outcomes Project now with over 10,000 participants recruited from Parkinson Foundation Centers of Excellence has predominantly white participants [49]. Thus, trials aiming to recruit a higher proportion of minority participants will need to first access potential participants outside of the traditional model of movement disorders clinical center-based recruitment.
There are also several barriers to clinical trial participation among minorities that are universal across diseases. Language can pose a particular barrier in recruitment of non–English speaking or illiterate/low-literacy participants. In one review of 1492 clinical trials at one major academic institution, nearly half did not include the option to enroll non–English speaking patients [68]. As a result, many non–English speaking patients are not even approached about clinical trial participation, despite high rates of enrollment when included. Many (36%) of these studies justified exclusion in part because study tools are not validated in other languages.
Among cancer prevention and therapeutic trials, actual barriers to participation that have been tested among under-represented groups included reduced opportunity to participate in trials and lack of awareness about clinical trials [69]. Another systematic review among studies of perceived barriers to clinical trial participation found mistrust, competing demands, concerns about side effects, and lack of access to information as the top 4 barriers to participation [70]. On the other hand, a common perception is that minority groups are less willing to participate in research. However, a recent study showed that when potential participants were asked whether they would participate in a proposed PD research study, there were no observed racial/ethnic differences in agreement to participate [71]. Furthermore, in a systematic review of 20 studies that reported rates of consent by race/ethnicity, there were no differences in willingness to participate in research [72]. There are also several perceived facilitators of research participation reported among minority subjects. These include benefits of participation (e.g., monetary compensation, free medical services) and altruism (i.e., helping family or community) [70].
We can learn important lessons from prior attempts to recruit a more diverse sample in PD clinical trials. One of the most successful studies, the pramipexole in levodopa-treated Parkinson’s disease patients of African, Asian, and Hispanic heritage conducted by the Parkinson Study Group over 18 months, sought to study the response to pramipexole among minorities specifically, and enrolled 144 minority subjects [73]. In this study, subjects were reimbursed for expenses such as transportation and dependent care in order to overcome financial barriers to participation. One of the first studies to test a specific recruitment methodology in order to improve minority patient participation in PD trials was an important building block for future studies. This randomized recruitment intervention tested partial funding for a recruitment coordinator, continuing medical education for physicians serving underserved populations and outreach to community-based referring physicians, but was stopped early because of lack of efficacy [53]. This study did find that the sites that were more successful in recruiting a higher proportion of minority subjects had stronger, existing relationships with community physicians. A more recent cluster-randomized trial of minority recruitment into an early stage PD trial tested a trust-based continuous quality improvement intervention that consisted of tailored interventions by site, patient navigation, and reduction of instrumental barriers (for example, cost to participate, transportation) [74]. This PD trial (STEADY-PD III) established a prespecified goal to recruit at least 10% minority subjects in the study cohort. In order to improve the efficiency of recruitment of all participants, a recruitment toolkit was created that incorporated materials for patient and referring provider engagement [75]. In addition, the study team paid particular attention to reducing the complexity of the study to limit the exclusionary criteria and reduce participant burden. In order to meet the minority subject recruitment goal, all aspects of the study design and implementation were addressed, from selecting sites based on prior record of minority enrollment and demographic data of the site, local community engagement, translated materials, and additional funding tailored to the needs of each site. More recently, Fox Insight, a large, web-based, longitudinal study of patient-reported outcomes among people with PD and healthy controls, employed targeted digital marketing through Facebook to underrepresented geographical areas within the USA and successfully recruited more participants than nontargeted recruitment [76]. These results were likely also influenced by other simultaneous recruitment efforts by the MJFF to the Fox Insight study [77].
Targeted recruitment efforts in other conditions have been successful in increasing the enrollment of traditionally underrepresented minorities. The most commonly used interventions for targeted recruitment are social marketing, community outreach, recruitment through the health system and referrals; however, community outreach appears to be the least effective [78]. Partnerships with community health workers, or trusted laypeople from under-represented communities, can help build relationships with minority patients. Community health workers have been shown to increase access to care [79]. When patient navigators or lay community health workers were used to support African–American patients through oncology clinical trials, retention was dramatically improved (75% of participants with a patient navigator completed the study compared to 38% without a navigator) [80]. Patient navigators provided help with transportation, lodging, and insurance, in addition to social and emotional support.
Although there is uncertainty as to what is the most cost-effective or efficient approach to increase diversity in clinical trial participation, there are several, established approaches that could be easily employed more broadly across PD clinical trials (Table 2). Although every approach may not be possible for every trial, investigators currently planning clinical trials should consider each of the listed measures.
In addition, we need to invest in research aimed at understanding and testing innovative methods to improve diversity in PD clinical trials. The Michael J. Fox Foundation recently launched a new initiative, Fostering Inclusivity in Research Engagement for Under-represented Population in Parkinson’s Disease (FIRE-UP PD) across 4 sites in the USA to engage more diverse communities in PD research [77]. This is an important step to build community engagement and understand specific barriers to participation in PD trials. Health policies such as the NIH guidelines on the inclusion of women and minorities in clinical research [81], and FDA regulations about required subgroup analyses prior to FDA approval, will also help motivate both academic and industry researchers to be more accountable. Finally, rethinking how we design and implement clinical trials can help improve recruitment and participation for all people with PD.
Novel Trial Designs
The barriers to trial enrollment and participation described above present opportunities for clinical researchers and aligned professions such as biostatisticians, ethicists, and clinical trial coordinators to develop novel strategies to improve clinical research. Strategies to overcome barriers to clinical trial participation in PD vary widely as do the problems that have been identified. Unfortunately, many of these strategies are without empiric, or even anecdotal, evidence. Simple and pragmatic ideas lend to their easy adoption and can be implemented without evidence of their efficacy. To address more complex barriers to participation, more research is needed. In some cases, a fundamental rethinking of our clinical research paradigm may be necessary.
Improving Recruitment
Many approaches to improve trial recruitment have been proposed, and several are formally tested. A collaborative recruitment strategy across institutions and practitioners could increase access for patients and researchers alike, despite the logistical and contractual challenges this may present [82]. This will require strong partnerships with community leaders and providers. Considering that most PD-related trials are conducted by movement disorders neurologists at specialized centers, a collaborative recruitment strategy modeled after the hub and spoke system used for stroke and trauma care could expand access dramatically. Pragmatic interventions such as using an opt-out consent format, where appropriate (e.g. observational studies), [83] enhanced patient educational material utilizing video and written patient-facing research documents, [84] more frequent communication through telephone reminders and text messages about upcoming visits and eligibility screening, [85, 86] and financial incentives [87] can increase trial recruitment [88]. Beyond these process-related interventions, the study design can also serve as an important tool in overcoming the challenge of recruitment.
Study Design
The research question will dictate the overall clinical trial design to evaluate the intervention by the most appropriate method. It is not surprising that recruitment is easier for observational trials than for randomized controlled trials, or that short-duration studies favor recruitment [82]. The possibility of receiving a placebo in a blinded study can be a deterrent to participation for many potential participants as well [89]. In pharmacological comparator studies, the use of an active comparator rather than a placebo might improve enrollment, when this is possible [90]. Another study design solution is the open trial design, in which participants know what treatment they are receiving. Although there is a greater risk of bias associated with an unblinded design, it has been associated with increased recruitment compared to a placebo-controlled study [91]. A crossover design can, similarly, address concerns about receiving a placebo, though this design requires a washout period and can lengthen the trial duration overall. Finally, the role and effects of a placebo are often not clearly communicated—more clearly discussing these effects in the informed consent process may also improve recruitment [92].
Furthermore, reducing the complexity and volume of data collection can help with trial participation. In general, the rationale for each research intervention should be scrutinized, and interventions reduced to capture the minimum set of necessary information to answer the research question. This will serve to maximize enrollment by eliminating unnecessary data collection, interventions, procedures, and burden on participants. Study design improvements aimed at improving trial efficiency may also improve recruitment and retention by requiring less from a smaller set of research participants.
Traditional, randomized clinical trials are the standard for clinical research; yet, they are expensive to conduct, require large sample sizes and long study durations, and lack power to evaluate efficacy in subgroups. Adaptive trial designs, aimed at improving the efficiency of trials, have been implemented in some cases to address these challenges. Adaptive trial designs have been used to identify safe dose ranges more efficiently, and to make prospective planned changes to the future course of ongoing trials by accounting for the results of previously collected data. Examples include seamless phase 2 to 3 designs, sample-size re-estimation, group sequential design, and population-enrichment designs [93, 94]. All of these approaches serve to improve efficiency, allow participants to focus their limited efforts on fewer trials, and benefit from interim analyses that allow for earlier identification of futility with the potential for early stopping, if appropriate. Furthermore, interim analyses may identify subgroups of participants with greater response rates, which would allow for subsequent targeted enrollment. Group sequential designs may additionally reduce the exposure to ineffective treatments, or limit participant time on placebo [95]. The overall effect of these trial design adaptations is to limit resources, costs, and waste in patients’ time and effort, and to arrive at helpful answers more quickly. In addition, traditional, randomized clinical trials often do not reflect the realities of real-world practice. Pragmatic clinical trials designed to evaluate interventions in routine practice are also gaining favor [96].
Financial Incentives
Financial incentives to participate in research are widely used, and have been shown to improve trial recruitment [87, 97]. However, there is substantial variability in the approach taken by institutional review boards towards financial incentives [98]. The size of the incentive is generally considered to influence participation, although ethical concerns of inducement remain a concern for incentives of significant value. In contrast, behavioral economic theories suggest the size of the incentive is less important than the design of the incentive, and a number of studies have examined how best to incentivize research participants [99]. Studies evaluating different models of financial incentive in smoking-cessation programs have shown that both group and individual incentives are equivalent in their effect on abstinence duration. Furthermore, reward payments, or payments for completing a task, are more effective than deposit reimbursements, in which a participant is reimbursed parts of their own deposit after increasing lengths of compliance with the outcome of interest [100]. Whereas financial incentives encourage study participation, and reward payments seem to be more effective, complex financial incentive programs do not seem to be more effective than simpler ones. Financial incentives can also be tailored based on the characteristics of the study, in collaboration with the IRB, to encourage participation and reduce attrition without undue pressure. For example, reimbursement to defray incurred costs of trial participation, including transportation, lodging, and parking, may help reduce financial burdens of trial participation and reduce some socioeconomic barriers to participation.
Technological Approaches
Technological advances can serve to improve trial participation by streamlining data collection, improving data accuracy and quality, and reducing or eliminating inefficiencies in the conduct of clinical trials. They can specifically mitigate the barriers posed by travel, and indirectly reduce financial burdens to trial participation.
Virtual visits utilizing a computer interface, or web-based data collection methods, remove travel from a participant’s decision-making process and have been shown to increase interest in participating in a clinical trial [101]. These virtual visits can be incorporated as the sole means of conducting research visits, or at interim visits based on the needs of the trial. Whenever possible, participants can also opt to have virtual visits, increasing participant autonomy.
Although telehealth can be used to increase access to trials and mitigate financial burdens, it does have limitations. Nearly 30% of households headed by a person aged 65 or older did not own or use a desktop, laptop, or handheld device; similarly, 37% of these households did not have any internet subscription [102]. Similar disparities in access to technology exist for households with limited English proficiency, of Black or Hispanic origin, and with lower household income [102]. Care must be taken to ensure technological solutions do not exacerbate disparities. Advocacy and system development to increase reliable broadband access and digital literacy are critical. Another important consideration is that simply recreating an in-person visit at a remote location would underutilize the capacity of virtual visits and web-based technologies in research studies. The opportunities to improve recruitment strategies via electronic means, collect large amounts of electronic data (including from wearable devices, smartphones and accessories, speech recognition devices, electronic questionnaires) and incorporate them into research visits, and integrate informatics platforms would dramatically increase the efficiency of data collection and safety [103]. However, to manage and make sense of the vast amounts of data, data scientists and the application of artificial intelligence and complex computer algorithms would become essential [104].
With the advent of novel technology-based objective measures (TOMs), such as wearable devices and computer interface, the method by which we collect and store data in clinical trials is undergoing a transformation. In the PD field, a 2017 survey demonstrated that only 3.2% of trials conducted use TOMs as outcome measures [105], a number that is expected to increase over time. Trials in which TOMs have been utilized have benefited from a smaller required sample size, shorter duration, and lowered costs [105,106,107,108]. Furthermore, TOMs can improve the accuracy of data collection and minimize the challenges of intra- and inter-rater variability [109]. A multitude of devices and platform are in development, although the relevance and validity of the measured variables, the complexity of the data that is obtained, costs associated with development, patient acceptance and compliance with wearing devices, and lack of standardization across devices have hampered further adoption into clinical trials [109]. Although there remains much work before TOMs can be widely deployed, they have the potential to capture real-life measures that are not captured in research office visits and reduce participant burden. More evidence is needed to determine how they can be used as primary outcome measures in future clinical trials to improve recruitment and retention, and to simplify clinical trial design.
There are additional benefits to using technology in clinical research beyond improved data collection. One of the biggest benefits to the conduct of research studies may be the opportunity to engage with diverse communities outside of the academic environment. Crowdsourcing, a term not often associated with clinical research, is the process of obtaining services, ideas, or information from an outsourced labor force, or “crowd,” by soliciting input through the internet [110]. Any tasks can be outsourced, and the labor pool tends to be diverse and not prespecified, although the “crowd” is expanding to include medical experts including physicians [111, 112]. Crowdsourcing has been used in clinical trial development to engage key stakeholders and provide solutions to improve the design and conduct of trials [113, 114]. In a phase I HIV antibody trial, crowdsourcing was used to obtain input from community members on the informed consent process, the experience of participating in a clinical trial, and fairness/reciprocity in HIV clinical trials. As a result, novel approaches to consent and participant recruitment were developed and implemented in the clinical trial [113]. Crowdsourcing has yet to be applied and tested broadly, but in PD clinical trial research, crowdsourcing may improve trial participation for several reasons. For example, this approach may encourage community members to feel invested in the research process, a metric that is associated with higher trial participation. It may also serve to engage members of the PD community traditionally underrepresented in clinical research including those outside academic centers and of different racial and ethnic backgrounds. Being involved in the design process may help to demystify the research study process and increase trust in the research system. Finally, crowdsourcing can help the research community to define the areas of highest importance and ensure that research remains patient centered.
Conclusions
As the number and breadth of clinical trials in PD grow, expanding access to clinical trials and ensuring representative enrollment are increasingly important. By addressing barriers to study participation when designing trials and when recruiting patients, we can improve access to care and research for all our patients. The use of technology, thoughtful and novel trial designs, careful attention to the burdens of trial participation, and recognition of disparities in healthcare access and delivery can help address common barriers. Increasing access and advancing community engagement can speed trial recruitment, allowing therapies to be studied thoroughly and, when effective, to reach patients more quickly. When trial design and recruitment strategies overcome these barriers to enroll a diverse group that reflects the PD population overall, we can better provide evidence-based, high-value care to all patients with PD.
References
Pringsheim T, Jette N, Frolkis A, Steeves TDL (2014) The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 29:1583–1590
Ray Dorsey E, Elbaz A, Nichols E, et al (2018) Global, regional, and national burden of Parkinson’s disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 17:939–953
Marras C, Beck JC, Bower JH, et al (2018) Prevalence of Parkinson’s disease across North America. NPJ Park Dis https://doi.org/10.1038/s41531-018-0058-0
Michael J Fox Foundation. A novel approach to clinical trial recruitment. https://www.michaeljfox.org/news/novel-approach-clinical-trialrecruitment. Accessed 5/19/2020
Cannard KG, Hacker ML, Molinari A, Heusinkveld LE, Currie AD, Charles D (2018) Recruitment and retention in clinical trials of deep brain stimulation in early-stage Parkinson’s disease: past experiences and future considerations. J Parkinsons Dis 8:421–428
Institute of Medicine (US) Forum on Drug Discovery, Development and T (2010) Transforming clinical research in the United States challenges and opportunities: workshop summary. https://doi.org/10.1177/2168479016656030
McDonald AM, Knight RC, Campbell MK, et al (2006) What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies Trials https://doi.org/10.1186/1745-6215-7-9
Charlson ME, Horwitz RI (1984) Applying results of randomised trials to clinical practice: impact of losses before randomisation. Br Med J https://doi.org/10.1136/bmj.289.6454.1281
Foy R, Parry J, Duggan A et al. (2003) How evidence based are recruitement strategies to randomized controlled trials in primary care? Experience from seven studies Fam Pract https://doi.org/10.1093/fampra/20.1.83
Chowdhury S, Meunier CC, Cappelletti L, Sherer TB (2014) Improving patient participation in Parkinson’s clinical trials: the experience of the Michael J Fox Foundation. Clin Investig (Lond) 4:185–192
Maasland L, Van Oostenbrugge RJ, Franke CF, Scholte Op Reimer WJM, Koudstaal PJ, Dippel DWJ (2009) Patients enrolled in large randomized clinical trials of antiplatelet treatment for prevention after transient ischemic attack or ischemic stroke are not representative of patients in clinical practice: The Netherlands Stroke Survey. Stroke 40:2662–2668
Patel HC, Hayward C, Dungu JN, et al. (2017) Assessing the eligibility criteria in phase III randomized controlled trials of drug therapy in heart failure with preserved ejection fraction: the critical play-off between a “pure” patient phenotype and the generalizability of trial findings. J Card Fail 23:517–524
Heiat A, Gross CP, Krumholz HM (2002) Representation of the elderly, women, and minorities in heart failure clinical trials. Arch Intern Med 162:1682–1688
Wasilewski J, Poloński L, Lekston A, et al. (2015) Who is eligible for randomized trials? A comparison between the exclusion criteria defined by the ISCHEMIA trial and 3102 real-world patients with stable coronary artery disease undergoing stent implantation in a single cardiology center. Trials 16:1–7
Kim ES, Bruinooge SS, Roberts S, et al (2017) Broadening eligibility criteria to make clinical trials more representative: American Society of Clinical Oncology and Friends of Cancer Research joint research statement. J Clin Oncol 35:3737–3744
Fehrenbacher L, Ackerson L, Somkin C (2009) Randomized clinical trial eligibility rates for chemotherapy (CT) and antiangiogenic therapy (AAT) in a population-based cohort of newly diagnosed non-small cell lung cancer (NSCLC) patients. J Clin Oncol 27:6538
Fosså SD, Skovlund E (2002) Selection of patients may limit the generalizability of results from cancer trials. Acta Oncol (Madr) 41:131–137
Reyes C, Pottegård A, Schwarz P, et al. (2016) Real-life and RCT participants: alendronate users versus FITs’ trial eligibility criterion. Calcif Tissue Int 99:243–249
Hoertel N, López S, Wang S, González-Pinto A, Limosin F, Blanco C (2015) Generalizability of pharmacological and psychotherapy clinical trial results for borderline personality disorder to community samples. Personal Disord Theory Res Treat 6:81–87
Zimmerman M, Mattia JI, Posternak MA (2014) Are subjects in pharmacological treatment trials of depression representative of patients in routine clinical practice. Am J Psychiatry 159:1
Ayaz-Shah AA, Hussain S, Knight SR (2018) Do clinical trials reflect reality? A systematic review of inclusion/exclusion criteria in trials of renal transplant immunosuppression. Transpl Int 31:353–360
Vashisht P, Sayles H, Cannella AC, Mikuls TR, Michaud K (2016) Generalizability of patients with rheumatoid arthritis in biologic agent clinical trials. Arthritis Care Res 68:1478–1488
Ivie RMJ, Vail EA, Wunsch H, Goldklang MP, Fowler R, Moitra VK (2017) Patient eligibility for randomized controlled trials in critical care medicine: an international two-center observational study. Crit Care Med 45:216–224
Storbjörk J, Garfield JBB, Larner A (2017) Implications of eligibility criteria on the generalizability of alcohol and drug treatment outcome research: a study of real-world treatment seekers in Sweden and in Australia. Subst Use Misuse 52:439–450
Reichmann H, Jost WH (2010) Efficacy and tolerability of rasagiline in daily clinical use - a post-marketing observational study in patients with Parkinson’s disease. Eur J Neurol 17:1164–1171
Parkinson Study Group (2012) A controlled trial of rasagiline in early Parkinson disease. The TEMPO Study. Arch Neurol 59:1937–1943
Kuoppamäki M, Vahteristo M, Ellmén J, Kieburtz K (2014) Pooled analysis of phase III with entacapone in Parkinson’s disease. Acta Neurol Scand 130:239–247
Kupsch A, Trottenberg T, Bremen D (2004) Levodopa therapy with entacapone in daily clinical practice: results of a post-marketing surveillance study. Curr Med Res Opin 20:115–120
Takahashi M, Fujita M, Asai N, Saki M, Mori A (2018) Safety and effectiveness of istradefylline in patients with Parkinson’s disease: interim analysis of a post-marketing surveillance study in Japan. Expert Opin Pharmacother 19:1635–1642
Mizuno Y, Kondo T (2013) Adenosine A2A receptor antagonist istradefylline reduces daily OFF time in Parkinson’s disease. Mov Disord 28:1138–1141
Zulman DM, Sussman JB, Chen X, Cigolle CT, Blaum CS, Hayward RA (2011) Examining the evidence: a systematic review of the inclusion and analysis of older adults in randomized controlled trials. J Gen Intern Med 26:783–790
Mitchell SL, Sullivan EA, Lipsitz LA (1997) Exclusion of elderly subjects from clinical trials for Parkinson disease. Arch Intern Med 157:1393–1398
Mantri S, Fullard ME, Beck J, Willis AW (2019) State-level prevalence, health service use, and spending vary widely among Medicare beneficiaries with Parkinson disease. NPJ Park Dis. https://doi.org/10.1038/s41531-019-0074-8
Wickremaratchi MM, Ben-Shlomo Y, Morris HR (2009) The effect of onset age on the clinical features of Parkinson’s disease. Eur J Neurol 16:450–456
Savica R, Grossardt BR, Rocca WA, Bower JH (2018) Parkinson disease with and without dementia: a prevalence study and future projections. Mov Disord 33:537–543
Martinez-Martin P, Pecurariu CF, Odin P, et al (2012) Gender-related differences in the burden of non-motor symptoms in Parkinson’s disease. J Neurol 259:1639–1647
Haaxma CA, Bloem BR, Borm GF, et al. (2007) Gender differences in Parkinson’s disease. J Neurol Neurosurg Psychiatry 78:819–824
Public Law 114, 21st Century Cares Act (2016) Statute 1033. pp. 1–312 . Available from: https://Congress.gov. Accessed 11/2/2020
Bernard MA, Clayton JA, Lauer MS (2018) Inclusion across the lifespan: NIH policy for clinical research. JAMA - J Am Med Assoc 320:1535–1536
Institutes of Health N Inclusion Across the Lifespan - June 1-2, 2017 Workshop Summary
Goel S, Paoli C, Iurlo A, et al. (2017) Socioeconomic burden of participation in clinical trials in patients with myeloproliferative neoplasms. Eur J Haematol 99:36–41
Nipp RD, Powell E, Chabner B, Moy B (2015) Recognizing the financial burden of cancer patients in clinical trials. Oncologist 20:572–575
Anderson A, Borfitz D, Getz K (2018) Global public attitudes about clinical research and patient experiences with clinical trials. JAMA Netw Open https://doi.org/10.1001/jamanetworkopen.2018.2969
Borno HT, Zhang L, Siegel A, Chang E, Ryan CJ (2018) At what cost to clinical trial enrollment? A retrospective study of patient travel burden in cancer clinical trials. Oncologist 23:1242–1249
Lara J, Higdon R, Lim N, et al (2001) Prospective evaluation of cancer clinical trial accrual patterns: Identifying potential barriers to enrollment. J Clin Oncol 19:1728–1733
Mathur S, Dewitte S, Robledo I, Isaacs T, Stamford J (2015) Rising to the challenges of clinical trial improvement in Parkinson’s disease. J Parkinsons Dis 5:263–268
Wong SL, Gilmour H, Ramage-Morin PL (2014) Parkinson’s disease: prevalence, diagnosis and impact. Health Rep 25:10–14
Hassan A, Wu SS, Schmidt P, et al. (2012) What are the issues facing Parkinson’s disease patients at ten years of disease and beyond?: data from the NPF-QII study. Parkinsonism Relat Disord 18:S10–S14
Dahodwala N, Shah K, He Y, et al. (2018) Sex disparities in access to caregiving in Parkinson disease. Neurology https://doi.org/10.1212/WNL.0000000000004764
Nwabuobi L, Barbosa W, Sweeney M, et al. (2019) Sex-related differences in homebound advanced Parkinson’s disease patients. Clin Interv Aging 14:1371–1377
Michael J Fox Foundation. Parkinson's progression markers initiative. Available from: https://www.ppmi-info.org/. Accessed 11/3/2020
Willis AW, Schootman M, Evanoff BA, Perlmutter JS, Racette BA (2011) Neurologist care in Parkinson disease: a utilization, outcomes, and survival study. Neurology. https://doi.org/10.1212/WNL.0b013e31822c9123
Tilley BC, Mainous AG, Elm JJ, Pickelsimer E, Soderstrom LH, Ford ME, Diaz VA, Siminoff LA, Burau K, Smith DW (2012) A randomized recruitment intervention trial in Parkinson’s disease to increase participant diversity: early stopping for lack of efficacy. Clin Trials 9:188–197
Grimshaw JM, Winkens RAG, Shirran L (2010) Interventions to improve outpatient referrals from primary care to secondary care. Chin J Evid Based Med 10:3
Van Den Eeden SK (2003) Incidence of Parkinson’s disease: variation by age, gender, and race/ethnicity. Am J Epidemiol 157:1015–1022
Dahodwala N, Siderowf A, Xie M, Noll E, Stern M, Mandell DS (2009) Racial differences in the diagnosis of Parkinson’s disease. Mov Disord https://doi.org/10.1002/mds.22557
McInerney-Leo A, Gwinn-Hardy K, Nussbaum RL (2004) Prevalence of Parkinson’s disease in populations of African ancestry: A review. J Natl Med Assoc 96:914–9
Wright Willis A, Evanoff BA, Lian M, Criswell SR, Racette BA (2010) Geographic and ethnic variation in Parkinson disease: a population-based study of us medicare beneficiaries. Neuroepidemiology https://doi.org/10.1159/000275491
Schneider MG, Swearingen CJ, Shulman LM, et al. (2009) Minority enrollment in Parkinson’s disease clinical trials. Parkinsonism Relat Disord 15:258–262
Downing NS, Shah ND, Neiman JH, Aminawung JA, Krumholz HM, Ross JS (2016) Participation of the elderly, women, and minorities in pivotal trials supporting 2011-2013 U.S. Food and Drug Administration approvals. Trials. https://doi.org/10.1186/s13063-016-1322-4
Dahodwala N, Xie M, Noll E, Siderowf A, Mandell DS (2009) Treatment disparities in Parkinson’s disease. Ann Neurol 66:142–145
Cheng EM, Siderowf AD, Swarztrauber K, et al. (2008) Disparities of care in veterans with Parkinson’s disease. Parkinsonism Relat Disord 14:8–14
Willis AW, Schootman M, Kung N, Wang XY, Perlmutter JS, Racette BA (2014) Disparities in deep brain stimulation surgery among insured elders with Parkinson disease. Neurology https://doi.org/10.1212/WNL.0000000000000017
Gilbert RM, Standaert DG (2019) Bridging the gaps: more inclusive research needed to fully understand Parkinson’s disease. Mov Disord https://doi.org/10.1002/mds.27906
Dahodwala N, Siderowf A, Xie M, Noll E, Stern M, Mandell DS (2009) Racial differences in the diagnosis of Parkinson’s disease. Mov Disord 24:1200–1205
Hemming JP, Gruber-Baldini AL, Anderson KE, et al. (2011) Racial and socioeconomic disparities in parkinsonism. Arch Neurol 68:498–503
Saadi A, Himmelstein DU, Woolhandler S, Mejia NI (2017) Racial disparities in neurologic health care access and utilization in the United States. Neurology https://doi.org/10.1212/WNL.0000000000004025
Bernier R, Halpin E, Staffa SJ, Benson L, DiNardo JA, Nasr VG (2018) Inclusion of non-English-speaking patients in research: a single institution experience. Paediatr Anaesth 28:415–420
Ford JG, Howerton MW, Lai GY, et al (2008) Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer 112:228–242
George S, Duran N, Norris K, et al. (2014) A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health 104:16–31
Nuytemans K, Manrique CP, Uhlenberg A, et al. (2019) Motivations for participation in Parkinson disease genetic research among Hispanics versus non-Hispanics. Front Genet 10:1–6
Wendler D, Kington R, Madans J, et al. (2006) Are racial and ethnic minorities less willing to participate in health research? PLoS Med 3:0201–0210
Tanner C, Comella C, Kamp C, et al (2007) Pramipexole in levodopa-treated Parkinson disease patients of African, Asian, and Hispanic heritage. Clin Neuropharmacol 30:72–85
Tilley BC, Mainous AG, Smith DW, et al (2017) Design of a cluster-randomized minority recruitment trial: RECRUIT. Clin Trials 14:286–298
Berk S, Greco BL, Biglan K, et al. (2017) Increasing efficiency of recruitment in early Parkinson’s disease trials: a case study examination of the STEADY-PD III Trial. J Parkinsons Dis 7:685–693
Dobkin RD, Amondikar N, Kopil C, et al (2020) Innovative recruitment strategies to increase diversity of participation in Parkinson’s disease research: The Fox Insight Cohort Experience. J Parkinsons Dis 10:665–675
McGuire Kuhl M (2019) New initiative will engage underrepresented populations in Parkinson’s research. https://www.michaeljfox.org/news/new-initiative-will-engage-underrepresented-populations-parkinsons-research. Accessed 4/1/2020
UyBico SJ, Pavel S, Gross CP (2007) Recruiting vulnerable populations into research: a systematic review of recruitment interventions. J Gen Intern Med 22:852–863
Andrews JO, Felton G, Wewers ME, Heath J (2004) Use of community health workers in research with ethnic minority women. J Nurs Scholarsh 36:358–365
Fouad MN, Acemgil A, Bae S, et al. (2016) Patient navigation as a model to increase participation of African Americans in cancer clinical trials. J Oncol Pract https://doi.org/10.1200/jop.2015.008946
NIH policy and guidelines on the inclusion of women and minorities as subjects in clinical research | grants.nih.gov. Accessed 4/1/2020
Newington L, Metcalfe A (2014) Factors influencing recruitment to research: qualitative study of the experiences and perceptions of research teams. BMC Med Res Methodol https://doi.org/10.1186/1471-2288-14-10
Trevena L, Irwig L, Barratt A (2006) Impact of privacy legislation on the number and characteristics of people who are recruited for research: a randomised controlled trial. J Med Ethics https://doi.org/10.1136/jme.2004.011320
Weston J, Hannah M, Downes J (1997) Evaluating the benefits of a patient information video during the informed consent process. Patient Educ Couns https://doi.org/10.1016/S0738-3991(96)00968-8
Nystuen P, Hagen KB (2004) Telephone reminders are effective in recruiting nonresponding patients to randomized controlled trials. J Clin Epidemiol https://doi.org/10.1016/j.jclinepi.2003.12.015
Free C, Hoile E, Robertson S, Knight R (2010) Three controlled trials of interventions to increase recruitment to a randomized controlled trial of mobile phone based smoking cessation support. Clin Trials https://doi.org/10.1177/1740774510367687
Halpern SD, Karlawish JHT, Casarett D, Berlin JA, Asch DA (2004) Empirical assessment of whether moderate payments are undue or unjust inducements for participation in clinical trials. Arch Intern Med https://doi.org/10.1001/archinte.164.7.801
Treweek S, Mitchell E, Pitkethly M, et al (2010) Strategies to improve recruitment to randomised controlled trials. Cochrane Database Syst Rev https://doi.org/10.1002/14651858.mr000013.pub5
Welton AJ, Vickers MR, Cooper JA, Meade TW, Marteau TM (1999) Is recruitment more difficult with a placebo arm in randomised controlled trials? A quasirandomised, interview based study. Br Med J https://doi.org/10.1136/bmj.318.7191.1114
Temple R, Ellenberg SS (2000) Placebo-controlled trials and active-control trials in the evaluation of new treatments: Part 1: ethical and scientific issues. Ann Intern Med https://doi.org/10.7326/0003-4819-133-6-200009190-00014
Avenell A, Grant A m., Mcgee M, Mcpherson G, Campbell M k., Mcgee M a. (2004) The effects of an open design on trial participant recruitment, compliance and retention – a randomized controlled trial comparison with a blinded, placebo-controlled design. Clin Trials https://doi.org/10.1191/1740774504cn053oa
Blease CR, Bishop FL, Kaptchuk TJ (2017) Informed consent and clinical trials: where is the placebo effect? BMJ 356:1–4
Bhatt DL, Mehta C (2016) Adaptive designs for clinical trials. N Engl J Med https://doi.org/10.1056/NEJMra1510061
Pallmann P, Bedding AW, Choodari-Oskooei B, et al (2018) Adaptive designs in clinical trials: why use them, and how to run and report them. BMC Med https://doi.org/10.1186/s12916-018-1017-7
van Eijk RPA, Nikolakopoulos S, Ferguson TA, Liu D, Eijkemans MJC, van den Berg LH (2018) Increasing the efficiency of clinical trials in neurodegenerative disorders using group sequential trial designs. J Clin Epidemiol https://doi.org/10.1016/j.jclinepi.2018.02.013
Gray R, Ives N, Rick C, et al (2014) Long-term effectiveness of dopamine agonists and monoamine oxidase B inhibitors compared with levodopa as initial treatment for Parkinson’s disease (PD MED): A large, open-label, pragmatic randomised trial. Lancet. https://doi.org/10.1016/S0140-6736(14)60683-8
Bentley JP, Thacker PG (2004) The influence of risk and monetary payment on the research participation decision making process. J Med Ethics https://doi.org/10.1136/jme.2002.001594
Klitzman R (2013) How IRBs view and make decisions about coercion and undue influence. J Med Ethics 39:224–229
Volpp KG, Pauly MV, Loewenstein G, Bangsberg D (2009) Market watch. P4P4P: An agenda for research on pay-for-performance for patients. Health Aff. https://doi.org/10.1377/hlthaff.28.1.206 LK - http://limo.libis.be/resolver?&sid=EMBASE&issn=02782715&id=doi:10.1377%2Fhlthaff.28.1.206&atitle=Market+watch.+P4P4P%3A+An+agenda+for+research+on+pay-for-performance+for+patients&stitle=Health+Aff.&title=Health+Affairs&volume=28&issue=1&spage=206&epage=214&aulast=Volpp&aufirst=Kevin+G.&auinit=K.G.&aufull=Volpp+K.G.&coden=HEAFD&isbn=&pages=206-214&date=2009&auinit1=K&auinitm=G. Accessed 4/1/2020
Halpern SD, French B, Small DS, Saulsgiver K, Harhay MO, Audrain-McGovern J, Loewenstein G, Brennan TA, Asch DA, Volpp KG (2015) Randomized trial of four financial-incentive programs for smoking cessation. N Engl J Med https://doi.org/10.1056/NEJMoa1414293
Shore C, Khandekar E, Alper J (eds) (2019) National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Forum on Drug Discovery, Development, and Translation; Virtual clinical trials: challenges and opportunities: proceedings of a workshop. Washington (DC): National Academies Press (US), p Jul 23. 2
Ryan C, Lewis JM (2017) Computer and Internet use in the United States:2015. Am Community Surv Rep 1–10
Doraiswamy PM, Narayan VA, Manji HK (2018) Mobile and pervasive computing technologies and the future of Alzheimer’s clinical trials. NPJ Digit Med. https://doi.org/10.1038/s41746-017-0008-y
Steinhubl SR, Wolff-Hughes DL, Nilsen W, Iturriaga E, Califf RM (2019) Digital clinical trials: creating a vision for the future. NPJ Digit Med. https://doi.org/10.1038/s41746-019-0203-0
Artusi CA, Mishra M, Latimer P, et al. (2018) Integration of technology-based outcome measures in clinical trials of Parkinson and other neurodegenerative diseases. Parkinsonism Relat Disord https://doi.org/10.1016/j.parkreldis.2017.07.022
Ozinga SJ, Machado AG, Miller Koop M, Rosenfeldt AB, Alberts JL (2015) Objective assessment of postural stability in Parkinson’s disease using mobile technology. Mov Disord https://doi.org/10.1002/mds.26214
Horak FB, Mancini M (2013) Objective biomarkers of balance and gait for Parkinson’s disease using body-worn sensors. Mov Disord https://doi.org/10.1002/mds.25684
Mariani B, Jiménez MC, Vingerhoets FJG, Aminian K (2013) On-shoe wearable sensors for gait and turning assessment of patients with parkinson’s disease. IEEE Trans Biomed Eng https://doi.org/10.1109/TBME.2012.2227317
Espay AJ, Bonato P, Nahab FB, et al (2016) Technology in Parkinson’s disease: challenges and opportunities. Mov Disord 00:1–11
Estellés-Arolas E, González-Ladrón-De-Guevara F (2012) Towards an integrated crowdsourcing definition. J Inf Sci https://doi.org/10.1177/0165551512437638
McCoy AB, Wright A, Laxmisan A, et al. (2012) Development and evaluation of a crowdsourcing methodology for knowledge base construction: Identifying relationships between clinical problems and medications. J Am Med Inform Assoc https://doi.org/10.1136/amiajnl-2012-000852
Bow HC, Dattilo JR, Jonas AM, Lehmann CU (2013) A crowdsourcing model for creating preclinical medical education study tools. Acad Med https://doi.org/10.1097/ACM.0b013e31828f86ef
Day S, Mathews A, Blumberg M, Vu T, Rennie S, Tucker JD (2020) Broadening community engagement in clinical research: designing and assessing a pilot crowdsourcing project to obtain community feedback on an HIV clinical trial. Clin Trials https://doi.org/10.1177/1740774520902741
Leiter A, Sablinski T, Diefenbach M, et al. (2014) Use of crowdsourcing for cancer clinical trial development. J Natl Cancer Inst https://doi.org/10.1093/jnci/dju258
Acknowledgments
Dr. Vaswani is supported by the Edmond J. Safra Fellowship in Movement Disorders. Dr. Tropea has received research funding from the NINDS, The Michael J. Fox Foundation, and the Parkinson Foundation. Dr. Dahodwala has received research funding from the NIA, The Michael J. Fox Foundation, the Parkinson Foundation, the Parkinson Council, Medtronic, and AbbVie and serves as a site PI for clinical trials funded by Eli Lilly and Roche.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(PDF 1225 kb)
Rights and permissions
About this article
Cite this article
Vaswani, P.A., Tropea, T.F. & Dahodwala, N. Overcoming Barriers to Parkinson Disease Trial Participation: Increasing Diversity and Novel Designs for Recruitment and Retention. Neurotherapeutics 17, 1724–1735 (2020). https://doi.org/10.1007/s13311-020-00960-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-020-00960-0